New Motherhood and Stomach Cancer: Dawn’s Story
Dawn’s experience with Stage 4 CDH1+ Hereditary Diffuse Gastric Cancer
Dawn is a mom from northwest Indiana who thought her family was complete. She and her husband already had a ten-year-old and a nine-year-old when they learned they were expecting a surprise baby boy in her early forties. At 41, she approached this pregnancy much like her first two, expecting another normal experience and focusing on caring for her growing baby while juggling life with two older kids, unaware that stomach cancer was already developing.
Interviewed by: Keshia Rice
Edited by: Chris Sanchez
Dawn’s health began rapidly declining during her third trimester. Despite thankfully having a healthy baby, she endured symptoms like intense fullness, daily vomiting, dehydration, and ultimately, blood in her vomit, a warning sign that demanded urgent attention. Dawn’s persistence led to big changes in her medical care: hospitalizations, an emergency C-section, and a cascade of tests, including biomarker testing, that finally uncovered her stage 4 CDH1-positive stomach cancer (Hereditary Diffuse Gastric Cancer or HDGC).
The genetic testing that revealed the CDH1 hereditary mutation, impacted not just her future but her children and extended family. As she navigated complex treatments, from chemotherapy and immunotherapy to HIPEC procedures and a swath of surgeries that included a gastrectomy, she became an empowered self-advocate. She challenged healthcare roadblocks, appealed insurance denials, and leaned on online patient communities for support and knowledge.
Through physical recovery, emotional uncertainty, and relentless self-advocacy, Dawn experienced profound transformation. She credits her faith and her family for sustaining her through exhausting treatment cycles and recovery, celebrating the small victories and moments of connection. She emphasizes that patient experience is not a solo effort: self-advocacy, family partnership, and compassionate care networks are essential for navigating stomach cancer.
Watch Dawn’s video above and scroll down for the edited transcript of her interview. You’ll learn how:
- Symptoms in pregnancy, like fullness and vomiting, deserve careful monitoring and should not be automatically attributed to standard pregnancy issues
- Self-advocacy is a life-saving skill; researching, appealing insurance denials, and seeking multiple medical opinions directly impacted Dawn’s experience
- Family, faith, and community are crucial sources of resilience during prolonged medical treatment
- Every patient’s experience is unique; personalized treatment decisions and persistence shape outcomes, not assumptions
- Dawn transformed from a struggling patient to an empowered advocate for herself and her family
- Name: Dawn C.
- Age at Diagnosis:
- 41
- Diagnosis:
- Stomach Cancer (Gastric Adenocarcinoma, Hereditary Diffuse Gastric Cancer)
- Staging:
- Stage 4
- Mutation:
- CDH1
- Symptoms:
- Persistent bloating
- Feeling of discomfort in the stomach area
- Weight loss
- Dehydration
- Feeling very full, leading to vomiting
- High blood pressure
- Treatments:
- Chemotherapy: HIPEC, including through a clinical trial
- Surgeries: Gastrectomy, splenectomy, cholecystectomy, oophorectomy, appendectomy, omentectomy, peritonectomy, lymphadenectomy
- Immunotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Hi. My name is Dawn
- My initial symptoms
- I had an emergency c-section and got admitted
- When I first heard the words “gastric adenocarcinoma”
- Parenting through cancer: feelings of loss
- Hereditary Diffuse Gastric Cancer: Learning about genetics
- My treatment: chemotherapy, HIPEC, and surgery
- The importance of self-advocacy in cancer care
- I had to find a new normal after surgery
- My family has really supported me
- Messages for my kids, and for myself
- My advice for other patients
Hi. My name is Dawn
I am from Northwest Indiana. I was diagnosed with gastric adenocarcinoma, also known as gastric cancer, in September 2024. At that time, I was 41 years old.
My husband and I were blessed with a surprise baby boy. We also have a ten-year-old and a nine-year-old, so we thought we were done. But God had other plans. I was pregnant and due in October 2024. All my pregnancies had been normal, and I felt okay for most of this one, even though I was older at 41. Everything was fine until about the third trimester. Around August, or maybe June or July, I started to feel unwell.
My initial symptoms
I tried to keep pushing through, make sure I drank enough water and ate well, but the baby seemed fine, and I just couldn’t come around; I just was not feeling well.
I’d eat and drink throughout the day, but at the end of the day, I couldn’t take any more. I’d be so full that I’d get sick. I told my OB doctor overseeing my pregnancy, and since the baby seemed fine and there were no other alarms, we chalked it up to morning sickness. But it progressively, slowly got worse.
I got dehydrated and went to a local IV drip bar for hydration a few times. I ended up in the ER twice for dehydration. The doctor said, “You’ve been complaining about this for a while. We can’t do much, but if you go to the ER, maybe they’ll give you a scan.”
They didn’t want to scan me in the ER because I was pregnant, so they did an ultrasound of my gallbladder, and that was fine. No bowel obstruction or other issues.
We still just didn’t know what was going on. All I knew was that I just wasn’t feeling well, and I had never had morning sickness with my other pregnancies. I didn’t feel comfortable taking the Zofran because I was pregnant and wasn’t really nauseous, just full every day. This continued with the baby still growing fine, but I started losing weight, even though I was in my third trimester and should be at my biggest.
I tried to eat as much as I could to help the baby grow, but I was still throwing up. At one point, I threw up blood. There wasn’t much we could do since the baby seemed fine and was measuring okay.
Eventually, I went in for a checkup, and my blood pressure was high. That raised alarms, and I told the nurse I’d been getting sick nearly every day for the last two months of the pregnancy.
I had an emergency c-section and got admitted
The nurse told me, “I don’t think you’re going to be leaving here today.” They drew blood work, and I was critically low on electrolytes, especially potassium. The high-risk doctor said, “We’re going to have a baby today.”
We had a C‑section, and everything was good, though I was nervous because I hadn’t been feeling well. But the baby was healthy. We just missed the NICU by a few pounds; he was born at 5 pounds and a month early, but all was well.
Later that night in the hospital, I ordered a meal, ate a few bites, and felt full; again, something wasn’t right. I got sick, and there was blood, so that prompted more action.
Now that I was in the hospital, we wanted to find out what was going on. The GI doctor ordered a CT scan; next, they wanted to do an endoscopy.
When I first heard the words “gastric adenocarcinoma”
The next day, I had the endoscopy. I had never had one before. You’re sedated for it, and I went down, it was done, and next thing I knew, I was in recovery.
The GI doctor came in and told me they found something. This was the first time I’d ever heard the words “gastric adenocarcinoma.”
To me, it seemed like a foreign language. I didn’t know what it meant. He said “stomach cancer,” and when you hear those words, that just wasn’t on my radar whatsoever.
To my knowledge, I didn’t have any history or family history of stomach cancer. I was just trying to process it. He was quite certain about what he saw, but they did a biopsy anyway.
I got the phone call a few days later. It was confirmed, I had stomach cancer.
Looking back, yes, I had symptoms. It wasn’t true that it came out of nowhere. I didn’t have debilitating signs, but I had bloating for years, discomfort, and sensitivity in my stomach area, though I couldn’t pinpoint what it was. I didn’t have acid reflux or GERD or nausea, or vomiting until the pregnancy. I’d seen a few doctors, even a GI, searching for answers about my stomach. I had been told different things: constipated, try a different diet, or do autoimmune or genetic testing. I did a lot of chasing from 2020 to 2023, looking for why I didn’t feel well. I chalked it up to prior pregnancies and C-sections, or just lifestyle.
There were signs, but nothing super alarming, and pregnancy definitely masked it.
Parenting through cancer: feelings of loss
So my son was born on September 26th, and I was officially diagnosed on September 30th.
This entire past year has been a blur, a lot of lows. My mind hasn’t always been present and focused on my son, when so much of it has been about treatment, diagnosis, and surgeries.
Thank God for my family, who helped care for him, especially since we traveled a lot for doctors, treatments, and surgeries, and the days when I just needed sleep.
I feel robbed, almost like a shell of myself. I feel like I’ve missed the first year of his life because I’ve been here, but I haven’t really been here.
With the cancer diagnosis, there’s so much that comes with it. It’s humbling and puts things into perspective. You think about what matters and what’s frivolous.
All of our relationships, especially with my husband, have strengthened. There are moments of weakness, and sometimes I feel it’s unfair for him to deal with this right now. But he’s been a rock and allowed me to heal, research, and be comfortable with my care team.
We’ve grown in faith, hope, and love, with our beautiful children. We are determined not to take a second for granted.
Hereditary Diffuse Gastric Cancer: Learning about genetics
I had never heard of CDH1 or hereditary diffuse gastric cancer before my diagnosis.
When the genetic counselor called to say I was CDH1 positive, I had no idea what that meant. That’s when the research began: what does this mean for my family, children, sisters, and mom? Everything changed.
There are different types of stomach cancer, and statistics, survival rates, and understanding the disease have become important. The lack of research and funding is scary, but I’ve learned so much from online communities advocating and sharing stories. That’s helped me gain strength and keep fighting.
Once I found I was CDH1-positive and that it was inherited, it was another blow. Now not only I but my family was affected too; my children, who’ll explore options for surveillance or surgery when they’re older, and my mom and sisters.
My dad passed away from colon cancer in 2014, and we hoped the gene was from him, but my half-sister on my dad’s side (who recently passed from cancer) did not have the gene. My mom got tested and, unfortunately, is a carrier, prompting more family members to get tested. It set off a domino effect. Now, cancer is affecting everyone close to us.
My treatment: chemotherapy, HIPEC, and surgery
Meeting with the oncologist, I had no idea what to expect, even though my dad had gone through cancer. I started treatment and also saw a surgeon who wanted to remove part of my stomach due to the blockage and inability to eat.
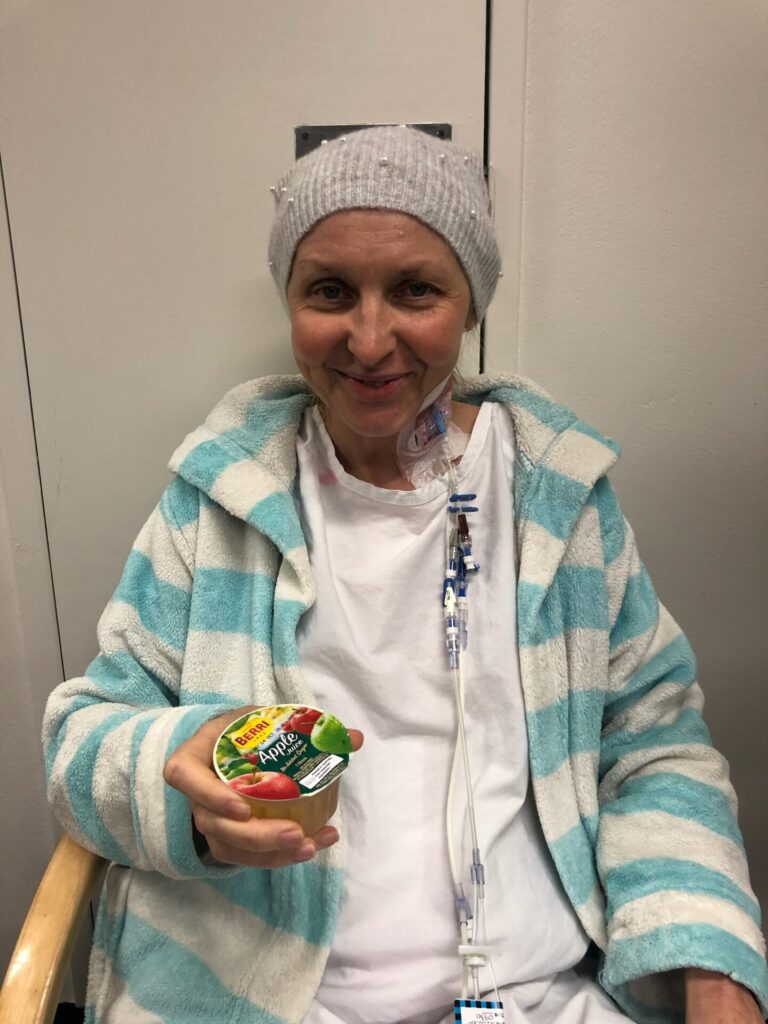
I was down to 98 pounds, very ill, and had little energy. I tried to eat and drink, but I kept getting sick. The lesson: with cancer, you want things done right now, but you have to have patience; it’s a wait-and-see process.
I had to wait for treatments, scans, and not rush into surgery, especially when I learned about the CDH1 gene. I started chemotherapy at our local university hospital. I had side effects like neuropathy, cold sensitivity, and nausea.
In November, I also had a laparoscopic washing to check for spread, learning that with hereditary diffuse gastric cancer, tumors aren’t easily visible on scans. A lot of how the treatment goes depends on how I feel.
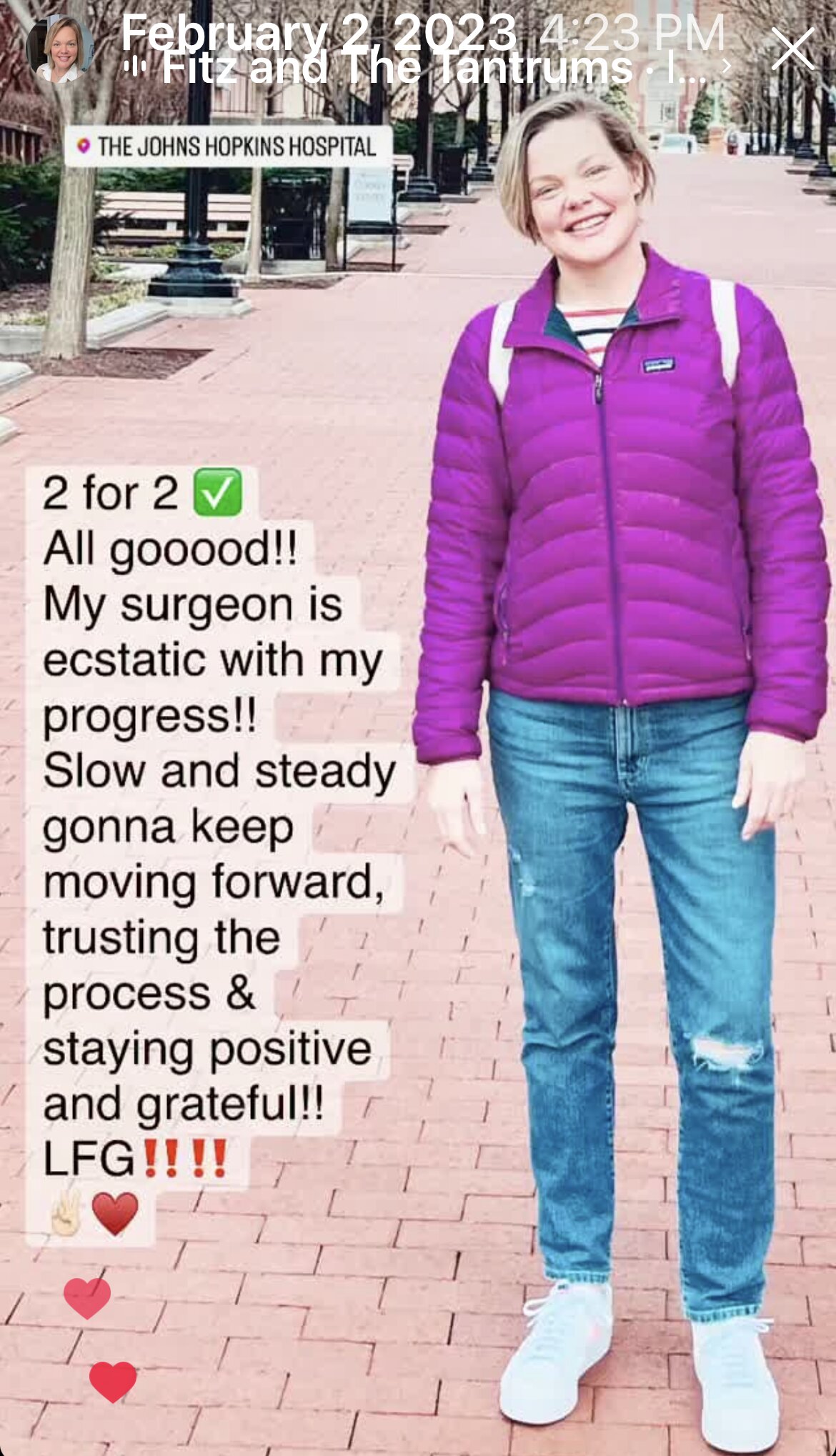
I responded well to chemo, added immunotherapy, and by December, I was eating again. Even if scans didn’t show clear shrinkage, I felt the difference.
The hospital had a clinical trial for HIPEC (hyperthermic intraperitoneal chemotherapy)—important because traditional chemo doesn’t always reach peritoneal spread. My insurance denied the trial as experimental, but my surgeon fought for it; I appealed and sought other clinical trials elsewhere. While off chemo waiting for HIPEC, symptoms worsened, and I had to get back on chemo. Insurance eventually reversed the denial, and I was able to receive HIPEC and, later, gastrectomy.
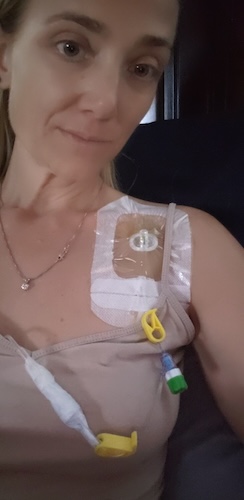
In June, I had my first HIPEC; the procedure was tough but successful. In July, I had a second HIPEC combined with gastrectomy. The 12-hour surgery removed my stomach, spleen, gallbladder, ovaries, appendix, omentum, part of the peritoneum, and 45 lymph nodes. Three of the lymph nodes were cancerous. Since then, I’ve been recovering, resumed chemotherapy on a reduced dose, and continue immunotherapy.
A feeding tube was placed but removed after a week; I’ve been able to maintain my weight since and eat mostly normally again.
The importance of self-advocacy in cancer care
Some doctors say, especially for stage 4 patients, “It’s only palliative care, and surgery isn’t an option.” Others follow strict guidelines without options. I knew that kind of doctor wasn’t right for me.
My persistence and advocacy were crucial. If I hadn’t advocated for myself, done research, or looked at every option, things could be different. I may not be here had my stomach been partly removed earlier. I had to fight for TPN nutrition when I dropped to 98 pounds, and it saved my life.
It’s vital to know your options; if you don’t know, you might miss a lifesaving opportunity. Take charge. Every case is different, and you have to do the work.
I had to find a new normal after surgery
Post-surgery, life is still settling. There’s a lot of anxiety with upcoming scans and uncertainty. It’s not back to normal; it’s a new normal. I try to live each day as best I can, taking the good with the bad, one step at a time, not thinking too far ahead.
I’m feeling well now between treatments and hope to go to Washington to advocate for stomach cancer; to be a body in the room, a voice, or a shoulder to cry on.
I thank God for leading me and for my children. I’m taking it one day at a time, cherishing moments with my boys, getting outside, and eating well. I want to share the love I’ve received and help others; not focus on disease, but health. For work, I’ll probably go back soon, but not very soon.
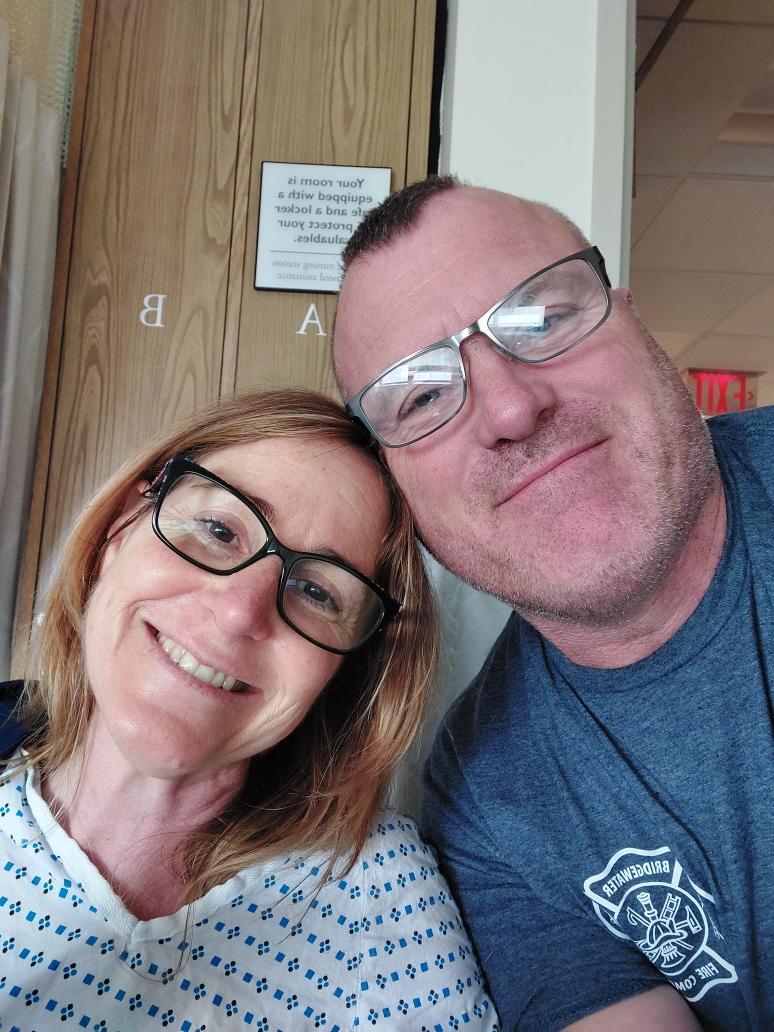
My family has really supported me
No questions asked. If I need anything: my mom to watch the baby, my husband to help, my mother-in-law or sister-in-law, they’re here.
We wouldn’t be where we are without family and friends, even our church family.
The kids keep me moving; I can’t wallow too long because I need to get up for them. For as tired as I am, they need me. I’m determined to be here for them, and I’ve needed them more than they know. They’ve been my rock.
Messages for my kids, and for myself
I wish my boys had never had to watch me go through this. I want them to know how proud I am, how they’ve been the light of my life. They give me the strength to keep fighting, to get up each day with energy, hope, and love. Their light gives me mine.
I thank them for being strong, but also want them to know they don’t always have to be; their feelings are okay. We must enjoy today’s moments. Nobody knows what tomorrow brings.
To myself last year, I’d say: It’s all going to be okay. God’s got me and will show me the way. I have angels, my dad, sister, nephew, and grandparents, watching over us.
Cancer’s an awful, awful disease. It robs us of joy and love, and it’s not fair. But there’s hope, and everything will be okay.
My advice for other patients
To other patients going through treatment or facing a diagnosis: God bless you, I pray for your strength, and want you to know there’s hope. Do for yourself what you would for someone else. Fight!
Don’t give up. Do research, talk to your doctor, and listen to yourself. Ask for help. There are amazing communities that will advocate, help, and show up for you. Lean in; you don’t have to fight alone.
Take each day as it comes. No one is promised tomorrow, and every day is beautiful.
Inspired by Dawn's story?
Share your story, too!
More Stomach Cancer Stories
Andy G., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Stomach pain, back pain, chest pain, extreme exhaustion, shortness of breath after short walks
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...
Brittany D., Stomach Cancer, Stage T1b
Symptoms: Choking suddenly while eating and attempting to speak, neck and right shoulder pain, neck tightness, trouble swallowing certain food items
Treatments: Surgeries (subtotal gastrectomy, D1 lymphadenectomy, gastric bypass)
...
Camilla C., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Issues swallowing, swollen gland in the neck
Treatments: Palliative chemotherapy was offered but declined, nutritional changes to support her comfort and energy, meditation and mindfulness practices, self-directed healing methods
...
Emily D., Stomach Cancer (Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Persistent postpartum stomachache, early satiety, difficulty swallowing, vomiting
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic) (Hospice Update)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...