Live with Hope for Yourself: Deb’s Multiple Breast Cancer Diagnoses
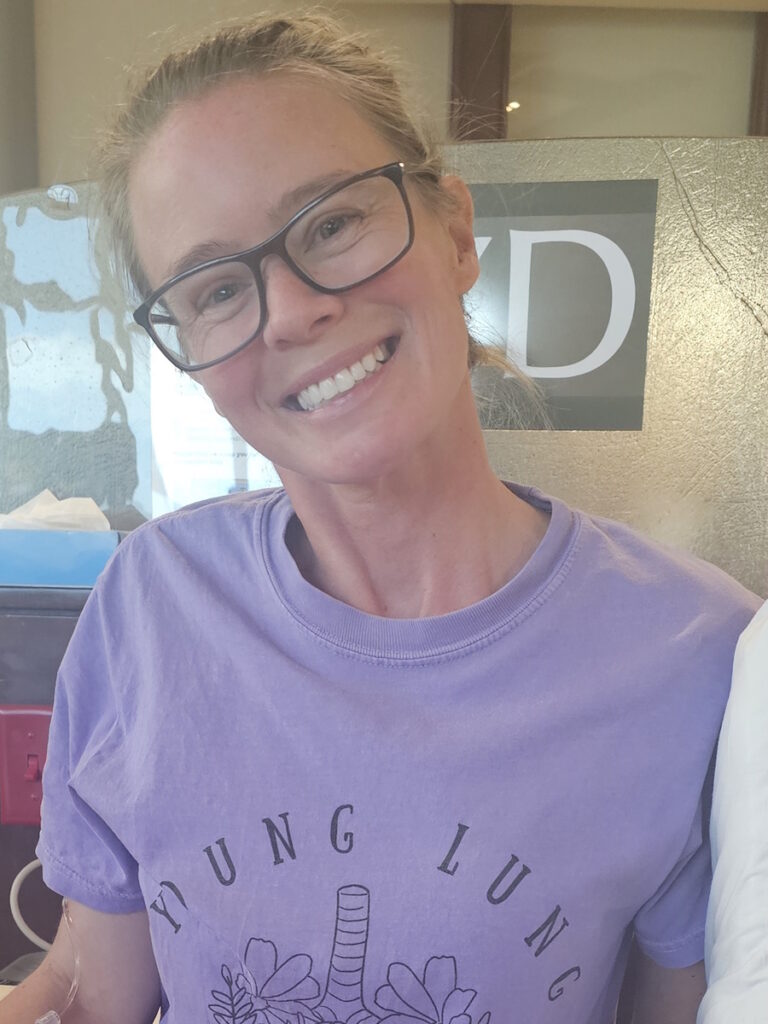
Deb has lived with metastatic breast cancer for seven years, originally diagnosed stage 4 triple-positive breast cancer in 2018 while raising her young daughter. Five years later, in 2023, she discovered a new lump and learned she had developed a second, unrelated breast cancer that was early stage and had a different profile.
Her life today is a blend of motherhood, advocacy, and strength. A longtime activist and English–Spanish interpreter, Deb has used her voice to push for understanding, empathy, and better support for people living with breast cancer. What began as two life-altering diagnoses has become a commitment to helping others feel seen, supported, and less alone.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
Deb’s story began in 2016, when she found a lump while she was breastfeeding her daughter, but it was dismissed as a clogged milk duct. Two years later, the lump had not only persisted but had also grown, leading to a de novo metastatic breast cancer diagnosis. The “de novo” distinction means the initial diagnosis was already at stage 4 or metastatic. “I didn’t know what metastatic meant,” Deb recalls. Once biomarker testing was complete, she learned it was HER2-positive, hormone receptor-positive breast cancer, or “triple positive breast cancer.” The early months were filled with fear, tests, and treatments, but also immense love from her community, who helped her care for her young daughter. When she reached no evidence of disease in 2018, her optimism clashed with the reality that metastatic breast cancer is often managed, not cured.

Living with both bipolar disorder and cancer, Deb describes her reality as one of constant adjustment. “Some days, the mental illness is harder on me than the breast cancer,” she says. Her transparent advocacy helps others balance emotional health with ongoing treatment.
In 2023, Deb faced a new, separate early-stage breast cancer diagnosis. Treating both simultaneously tested her physically and emotionally, but her resilience remained unshaken.
Deb’s breast cancer experience continues to evolve. Today, her scans again show no evidence of active disease, yet she acknowledges the uncertainty that remains including being on active treatment. What keeps her grounded, she says, is hope: hope for herself, for her daughter, and for a better understanding of metastatic disease. “Do it for you,” she tells others living with this diagnosis. “You deserve to have hope for yourself.”
Watch Deb’s video above and scroll down to read the edited transcript of her interview for more on how:
- Metastatic breast cancer is lifelong and demands ongoing adaptation
- Hope can evolve, from doing it for others to valuing one’s own life and wellbeing
- Mental health challenges can be as significant as physical ones
- Support networks and advocacy communities provide essential strength
- Parenthood can coexist with cancer care when boundaries and love guide the balance
- Name: Deb O.
- First Diagnosis:
- First Diagnosis: De Novo Triple-Positive Breast Cancer
- Second Diagnosis: ER-Positive, HER-Negative Breast Cancer
- Staging:
- First Diagnosis: Stage 4
- Second Diagnosis: Early-stage
- Age at Diagnosis:
- First Diagnosis: 37
- Second Diagnosis: 42
- Symptoms:
- First Diagnosis: Appearance of lump that later on increased in size, orange peel-like skin around inverted nipple, persistent ache under right arm
- Second Diagnosis: appearance of lump
- Treatments:
- First Diagnosis: Chemotherapy, targeted therapy, hormone therapy
- Second Diagnosis: Surgery (mastectomy), chemotherapy, radiation therapy, CDK 4/6 inhibitor
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Hi, I’m Deb
I live with metastatic breast cancer, HER2-positive, hormone receptor-positive. I’ve been living with it for seven years. I also have an early-stage breast cancer diagnosis from 2023. I’m living in southern Utah right now.
I’m a mom to a beautiful 11-year-old daughter. Before motherhood, I was an activist for over 20 years. I’m also an English–Spanish translator and interpreter, with much of my time spent volunteering.
Originally from California, when I moved to Salt Lake City, I found activist groups that interested me and poured my heart into community involvement. Everything changed when I had my daughter, but I continue to do advocacy now, with my focus shifting towards breast cancer.
Advocacy is incredibly important to me; I’ve moved my background in mental health advocacy into the breast cancer world, because it’s the life I’m living now.
My daughter Estelar—her name means “stellar”—is the biggest-hearted, kindest kid you’d ever meet. She’s in sixth grade and was only four when I was diagnosed, so this is all she’s ever known: mom living with cancer. She’s very mature about it, and I take her to therapy so she has ways to cope. Estelar is a creative kid; she loves Roblox and graphic art, and she’s an artist, though she didn’t get that from me. She’s always trying to bring a smile to everyone she knows and is very protective of me. Sometimes, she takes on a caregiver role, and I have to remind her that I’m the mom and she’s the daughter. She’s incredibly sweet. Sometimes she offers, “Mom, you don’t have to walk me this morning if you’re not feeling well.” But I cherish our walks to school and always try to be there, unless I really can’t. Estelar has adjusted remarkably, though I do worry about her falling into caregiver habits. “I don’t want her to think that’s her job in any way”.
Therapy has helped a lot. When I was diagnosed, a hospital social worker took Estelar around the hospital and explained things in child-friendly terms, even using a doll. She’s always been aware that things are changing. She struggles sometimes, feels sad, but overall has been processing it very well. She’s able to talk to me about her worries, and she calls my infusion days “port medicine day.” It’s super cute. She knows I’ll feel a little worse the next day, but she’s so supportive.
My diagnosis and how my family and I handled it
The story of my diagnosis actually begins before 2018. In 2016, while breastfeeding, I felt a lump in my right breast. At an appointment, my provider told me it was probably just a clogged milk duct, saying I was too young for breast cancer and had no family history, so I let it go.
Life got busy as a single mom of a two-year-old, and, as is common in Latino families, mothers often put their medical needs aside. But two years later, the lump had grown. In 2018, after encouragement from a new partner, I scheduled an appointment, and things moved quickly.
I was seen at a clinic; the second provider, a female physician, took things seriously. Within a day, I was scheduled for a mammogram and a biopsy at the Huntsman Cancer Institute. I was alone during the biopsy, which was incredibly painful and frightening.
Soon after, I received the diagnosis call while boarding a train with my four-year-old daughter en route to preschool. I shared the news matter-of-factly with a friend on the train, holding back emotion for my daughter’s sake: “I’m a mom, and the day still had to go on. I would deal with this later.”
Later that day, reality hit as I was walking home, tears streaming down my face, carrying my daughter. It was a slow realization that everything would change. Nothing was ever going to be the same again.
Navigating urgency and my first treatments
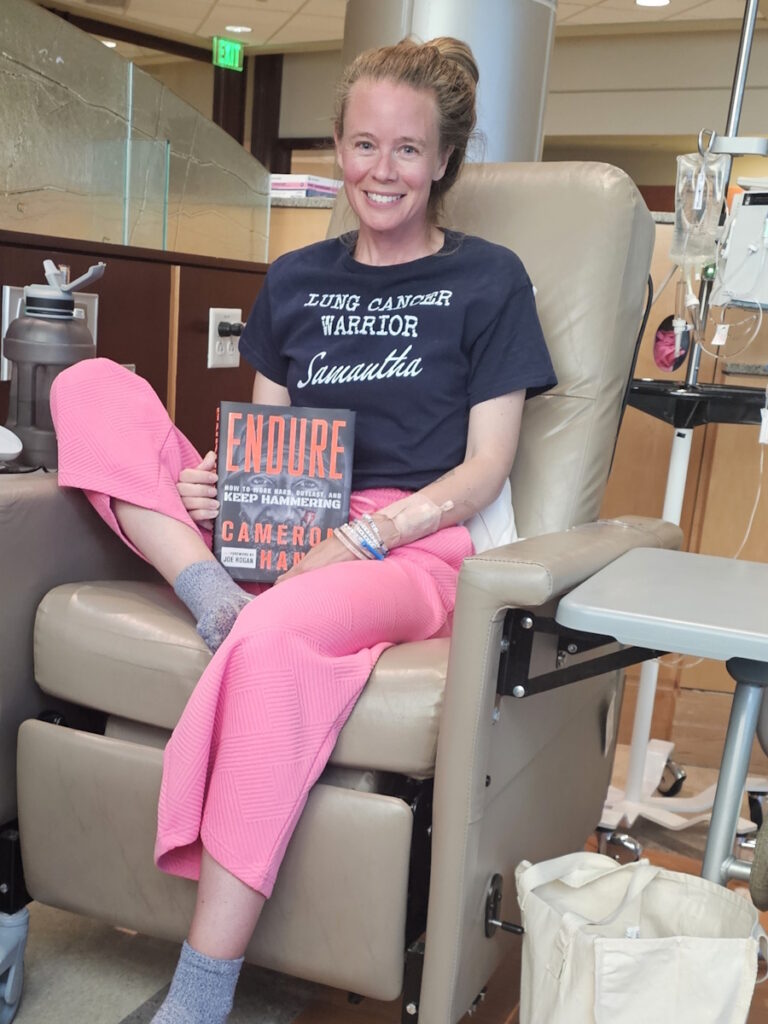
That first month after diagnosis was a whirlwind. The hospital scheduled endless tests: PET/CT scans, a bronchoscopy, and port placement for chemotherapy.
I hadn’t even decided what I wanted to do yet, but there was a sense of urgency. My oncologist reminded me, “You have a four-year-old, and this is aggressive cancer.” Therapy helped, and my top priority was doing whatever it took to be there for my daughter. Three weeks later, I was told my cancer was stage 4, metastatic, throughout the mediastinum and lymph nodes.
It was a lot of uncomfortable first-time experiences, and honestly, I’m not really sure how I got through that, but I do know that I had a lot of community with me. Community support was invaluable; friends and community members helped with my child, appointments, and rides.
By June 1st, I started my first chemo. My sister-in-law Jenny left her job to help, especially with my daughter. That summer, despite treatment and illness, we tried to have fun: concerts, dating, and staying active in the community. Through it all, I didn’t know what “metastatic” truly meant and thought I might beat cancer.
After chemo, my first PET scan showed “No Evidence of Disease” (NED). I celebrated, believing I had beaten cancer, but my doctor explained I’d need treatment indefinitely.
I didn’t have time to feel angry because everyone was so excited by the clear PET scan news. The word ‘indefinitely’ just weighed on me.
Advocating, community, and mental health
Reaching NED was both joyous and sobering.
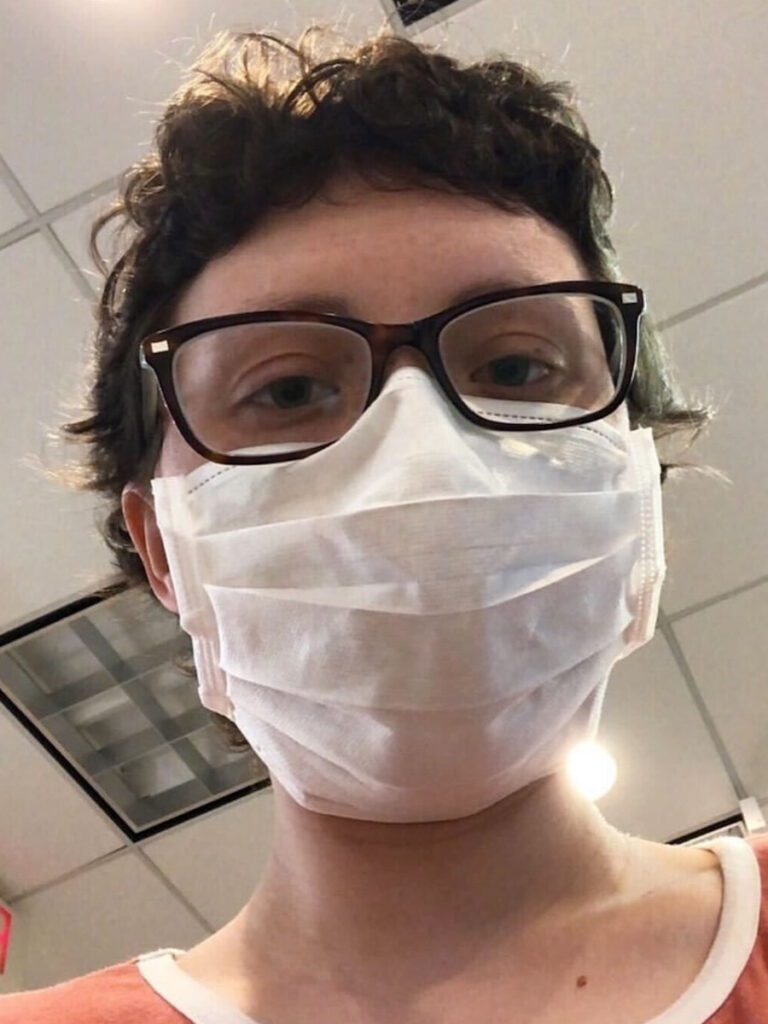
For two years, I didn’t seek out other women with metastatic breast cancer; I didn’t want to know. But the pandemic changed things, and I found a strong online community. Treatment, scans, and appointments have become normal over the past seven and a half years.
I also live with bipolar disorder, which complicates everything. Some days, mental illness is harder than cancer. Abigail, an advocate friend, helps lift my spirits, shares memes, and trains me as a mentor for other patients.
My second diagnosis: finding out I had a new cancer
In 2023, I was ready to celebrate five years of living “NED” with metastatic breast cancer. But a month before my scheduled scans, I found a new lump while doing a monthly self-check.
Scan day came just as Metastatic Breast Cancer Awareness Day arrived. I was hopeful, but my scan wasn’t clear. The whirlwind began again.
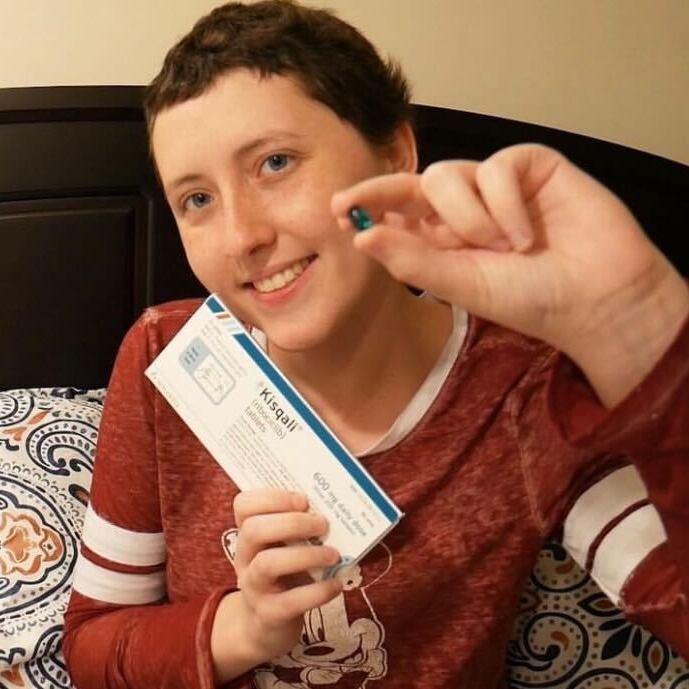
This time, I was older, without my in-person community, and faced a changing body from years of medication. After a painful biopsy, my partner by my side, the results showed it was a completely different breast cancer: hormone receptor-positive, HER2-negative. I got a second opinion from my first oncologist, who confirmed that it was a new cancer, not progression.
Treatment required chemo again, a pause in my metastatic regimen, and surgery, which I hadn’t been eligible for during my initial stage IV diagnosis. I had a mastectomy, another course of chemo, and suffered through radiation and new side effects like lung scarring. This time, my daughter had more questions, and could see I wasn’t as strong as the first time. You have to keep adapting, keep adjusting. That’s what it is like, living with multiple breast cancer diagnoses.
Months later, a clear scan brought relief. I could return to my regular treatment schedule for metastatic disease.
Living with metastatic breast cancer
Metastatic breast cancer never really goes away.
There’s worry; will the earlier-stage cancer come back and metastasize? Will progression happen?
Doctor appointments and scans consume my time, and sometimes it’s hard to find the fun I used to have.
Advocacy and support organizations
Any type of community you have is so beneficial when you’re going through a diagnosis.
Three organizations have been especially supportive. The first is Project Life, an online wellness house for women with metastatic breast cancer, with programs like journaling, yoga, and support sessions.
The second, Living Beyond Breast Cancer, holds advocacy training and mentorship programs, especially for young women diagnosed under 45.
The third organization, For the Rest of Us, is an online empowering community for women of color, focused on community education and fundraising.
Meeting others with breast cancer, in-person and online, brings joy and helps fight isolation, even though it’s tough losing friends to this disease.
My advice for others
There are many misconceptions about metastatic breast cancer. People need to know it is lifelong and incurable, and we need research for a cure.
More people are living longer, thanks to medication advances, but also remember we are more than our diagnosis. We are mothers, daughters, partners, and community members.
Hope can be elusive, especially at low moments, even before cancer. But it’s vital. Don’t just have hope for your children or family. Have hope for you, because you matter, exactly as you are.
You’re not alone. Educate yourself, take care of your mental health, and seek counseling or support groups. Don’t wait too long to meet other people who get it.
Don’t just exist with this illness. Live.

Inspired by Deb's story?
Share your story, too!
More Breast Cancer Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy
Callie M., IDC, Stage 2B, Grade 2, ER+
Cancer Details: ER positive = estrogen receptor positive
1st Symptoms: Dimpling/lump found on breast
Treatment: Mastectomy, AC/T chemotherapy, hysterectomy, reconstruction
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Symptoms: Tightness and lump in left breast
Treatments: Chemotherapy, radiation, surgery
Stefanie H., IDC, Stage 3, Triple-Positive
Symptom: Lump in the breast
Treatments: Chemotherapy, surgery (lumpectomy), radiation