Expand to read the AI-generated YouTube Video Transcript
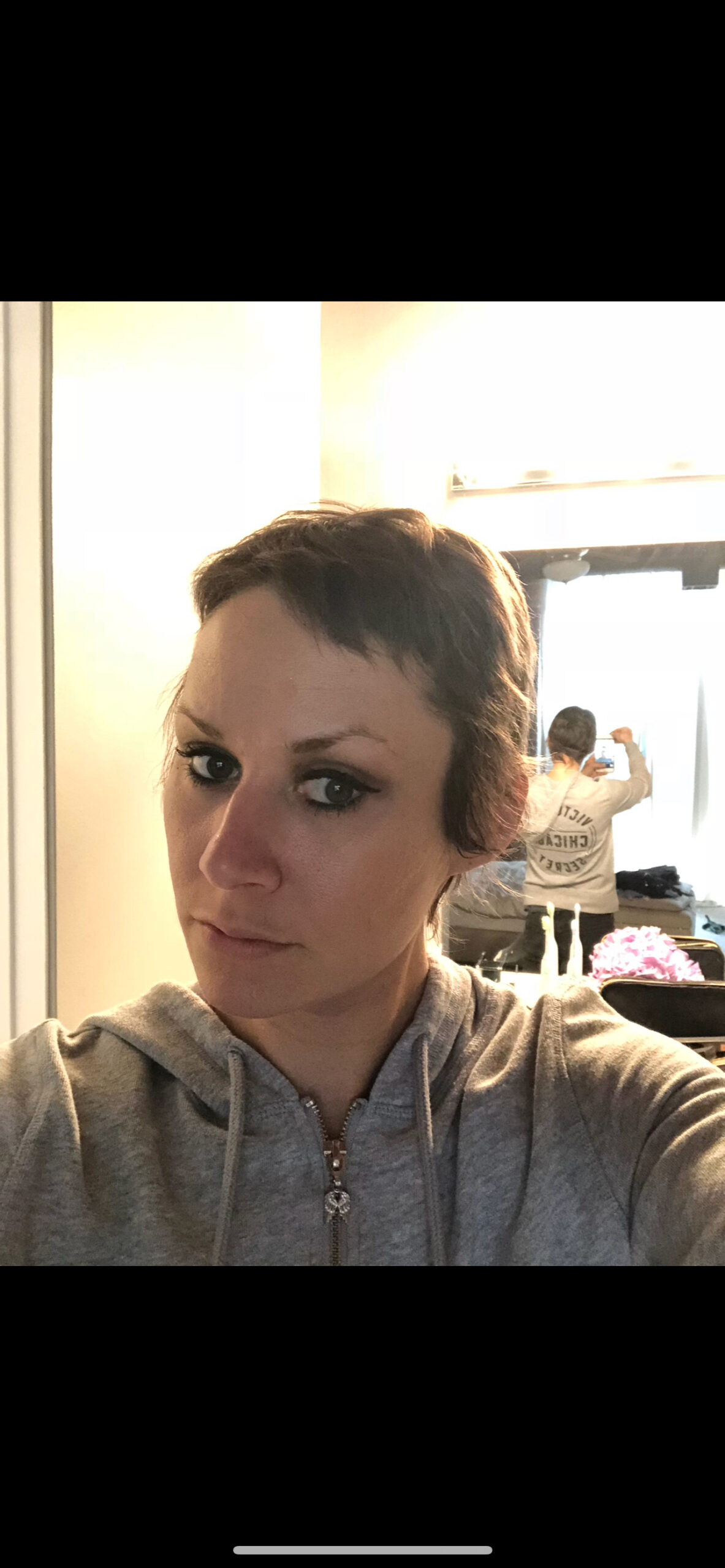
[00:01] Hi, I’m Krista, and I am a nurse and a patient advocate and a breast cancer survivor. My story really begins with my mom’s cancer diagnosis. She was diagnosed at age 48 with stage 3 breast cancer. At that time, she was only tested for two gene mutations linked to breast cancer, which were the BRCA1 and BRCA2 mutations. She was negative.
[00:36] Fast forward, she did every type of treatment—chemo, radiation, hormone therapy, everything. She put up a strong fight for about 12 years. Shortly before she passed away, she was unfortunately offered expanded genetic testing for other genes linked to breast cancer. She did test positive for a mutation in her ATM gene, which was a pathogenic mutation and higher risk than the average ATM gene.
[01:15] She shared that with all of her children because we then had a 50% chance of inheriting that from her, so we had the option to also test for that mutation. A few months after she passed away, I decided to move forward with my own genetic testing and found out I was also a carrier of the same mutation. So, I had a 69% risk of breast cancer, a 5 to 10% risk of pancreatic cancer, and also a 2 to 3% risk of ovarian cancer.
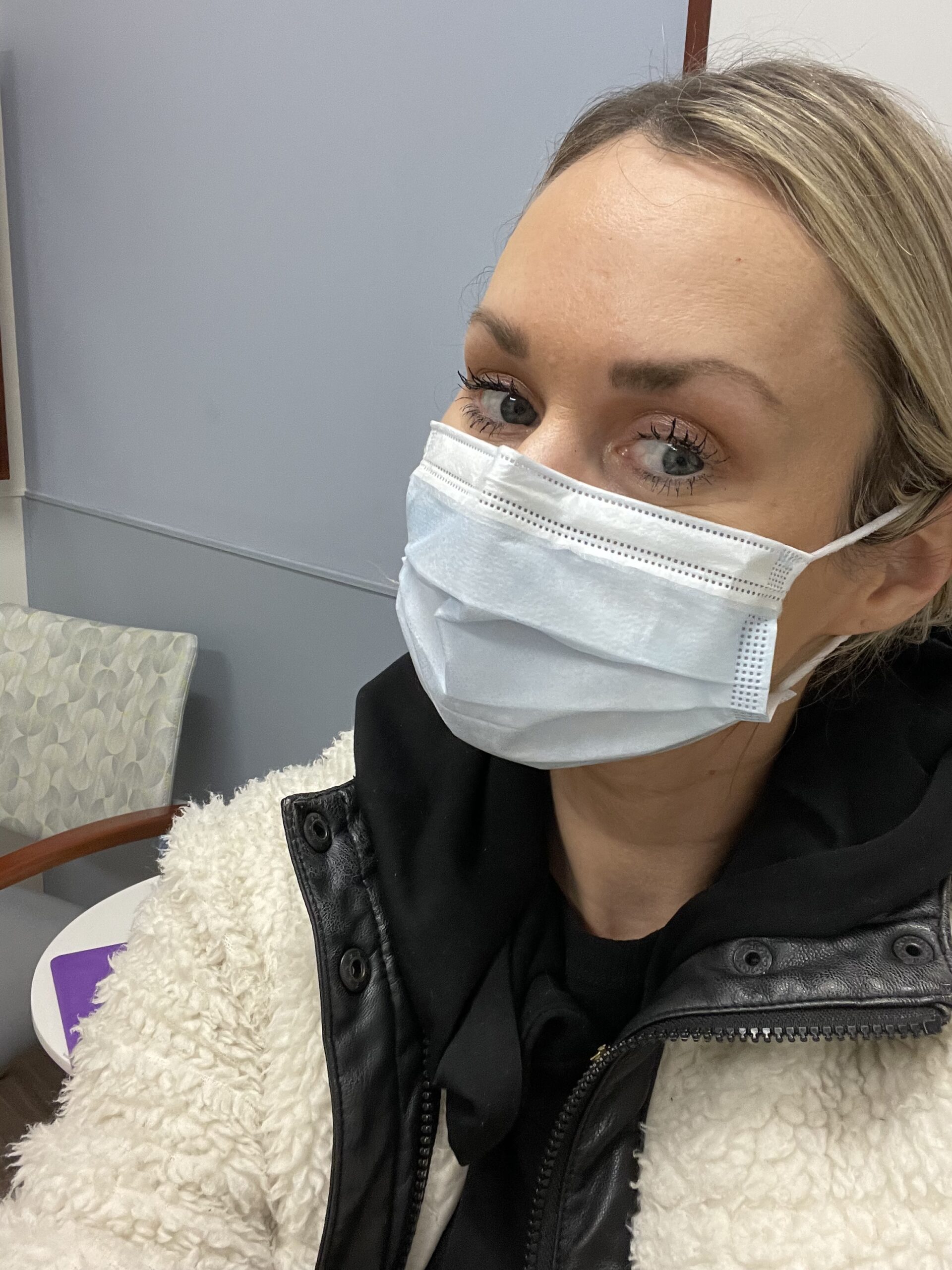
[01:56] Because I was at high risk for these cancers, I started to follow the recommendations for more thorough and frequent screenings, which meant on top of mammograms, I was also doing breast MRI, alternating every six months. I started that process and also began considering different surgical options for preventative surgeries.
[02:20] During this time, my mammogram was normal, but my breast MRI showed an abnormality. We did some follow-up testing—ultrasound and diagnostic mammogram. At that time, they said that it did not look like cancer. I was nervous about that with my risk, so I followed up and had three specialists tell me that it was not cancer. They advised me to take my time, make my decisions, and move forward with the surgical plan that I had in place.
[03:01] So, I did that, but because it started to have a possibility of affecting the process of my surgery, I requested a biopsy. It came back two weeks before my preventative surgery and showed a diagnosis of breast cancer. It was a little bit of a shock. I went into my biopsy thinking, “Oh, I’m good. This is just a routine check to make sure it’s okay to move forward with my surgery in the order we had planned.” So, I was really surprised at the diagnosis, but I was grateful to have that plan in place already and that I wasn’t scrambling to make decisions.
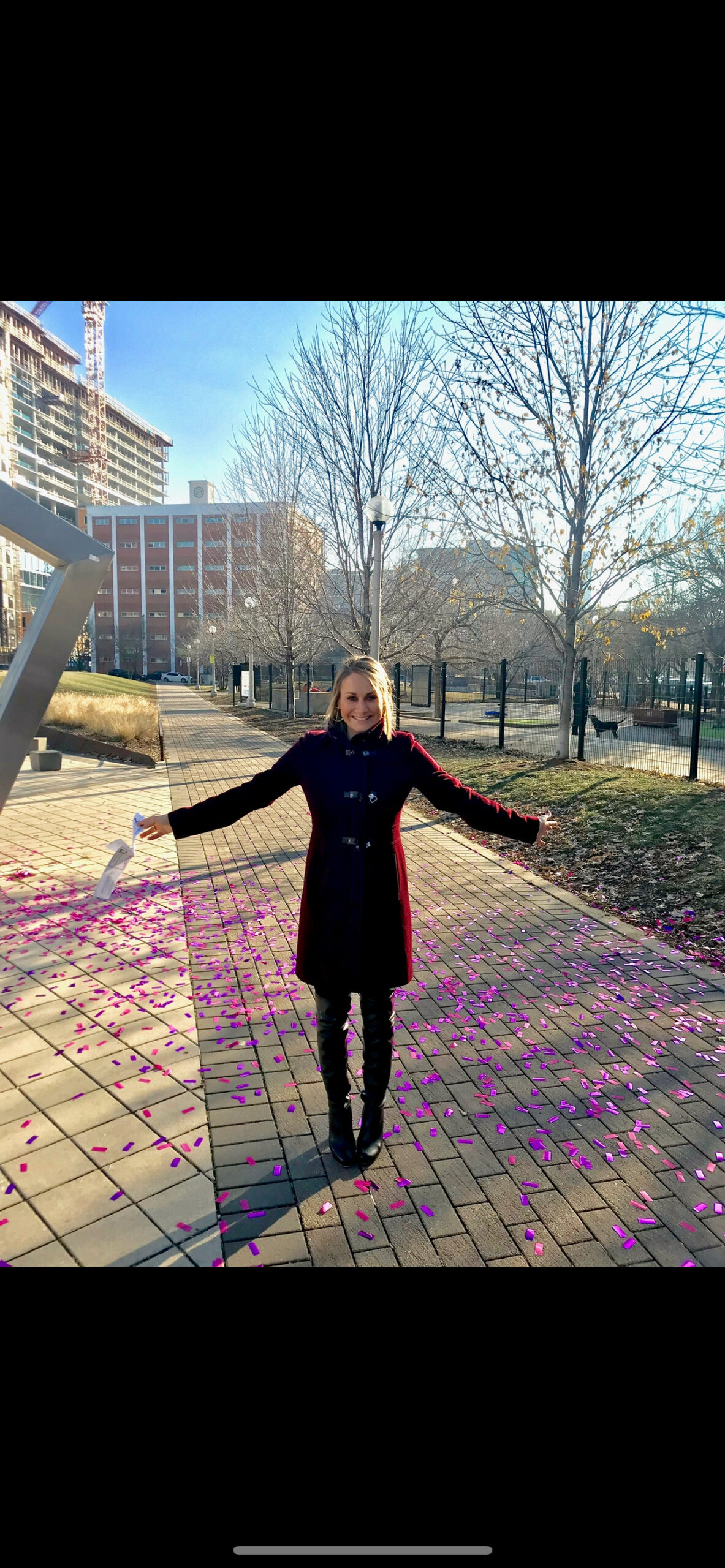
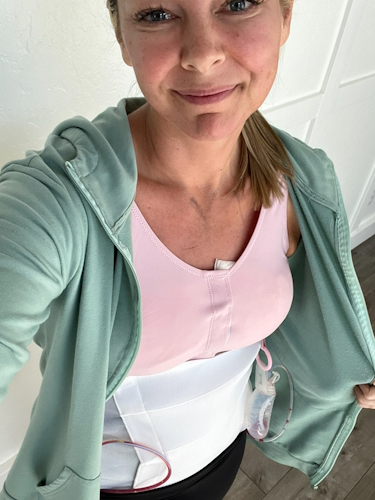
[03:42] I had my first surgery, a double mastectomy with flap reconstruction, on January 30th of this year, followed by a second surgery in April. Luckily, I really believe that I owe this all to my mom and advances in genetics. I’m grateful every day for the fact that she did genetic testing because, to this day, at this point in time, I don’t think I would still have a diagnosis based on my screening schedule. I’m very grateful I was able to avoid chemotherapy and a lot of the other things that I watched her go through. I’m grateful for that every day. It saved my life.
[04:36] If you’re interested in doing genetic testing, the first step would be to talk to your medical provider. This can sometimes be your primary care provider, an OB-GYN, or any specialist in the field of cancer that you may or may not have a family history with. You’re going to want to request a hereditary cancer panel, which screens for somewhere around 79 different genes that are now linked to cancer. The first step would be to request that from your provider, and most of the time, they’ll recommend that you see a genetic counselor, which is a great idea in my opinion. They’re amazing and have the most up-to-date information on the different genes and the risks associated with each. They do a deep dive into your family history and then make recommendations for different testing.
[05:31] From that point, it has really changed my life. I have three little girls, and I just think how different it’s going to be for them and how much they can avoid. But when it comes down to choices for reconstruction, there are typically three main choices that are offered to patients or should be offered to patients. One of them is esthetic flat closure, the second one is breast implants, and the third is flat base reconstruction. Flat base reconstruction is one that’s a little less known. It was my choice, and rather than having an implant, they take tissue from a part of your body and basically transplant it with all the vessels and use that in place of the implant for your reconstruction.
[06:26] It’s pretty amazing the way that they do it, and there are different places that they can take the tissue from. One of the most common is the one that I chose called deep flap reconstruction. They take tissue from your abdomen and use that for the reconstruction. It’s a little bit of a longer surgery upfront, and it was a two-phase surgery for me. That’s very common for patients who choose this reconstruction option. It is around an eight-hour surgery usually, so a little longer.
[07:06] My advice to anyone who is facing these choices is that they’re very hard choices, right? They’re life-changing decisions that you have to make. Sometimes you aren’t given a lot of time, but the thing that I hope everyone understands is that there are different options out there. Regardless of what anyone else thinks—whether it’s your provider, your family members, or someone who has been through it—ultimately, it’s your decision, and it’s what you have to live with. It should be the choice that makes you feel the most at peace moving forward.
[07:50] I have a lot of patients who I talk to who get very frustrated because they were not offered all the options. That’s one of the reasons I like to share my story because even for me as a nurse, in the beginning, I did not have a clue that this was an option. My biggest advice would be to take your time. Even with a cancer diagnosis, you have time to make an informed decision. Consider all of your options and choose the one that makes you feel the most at peace moving forward.
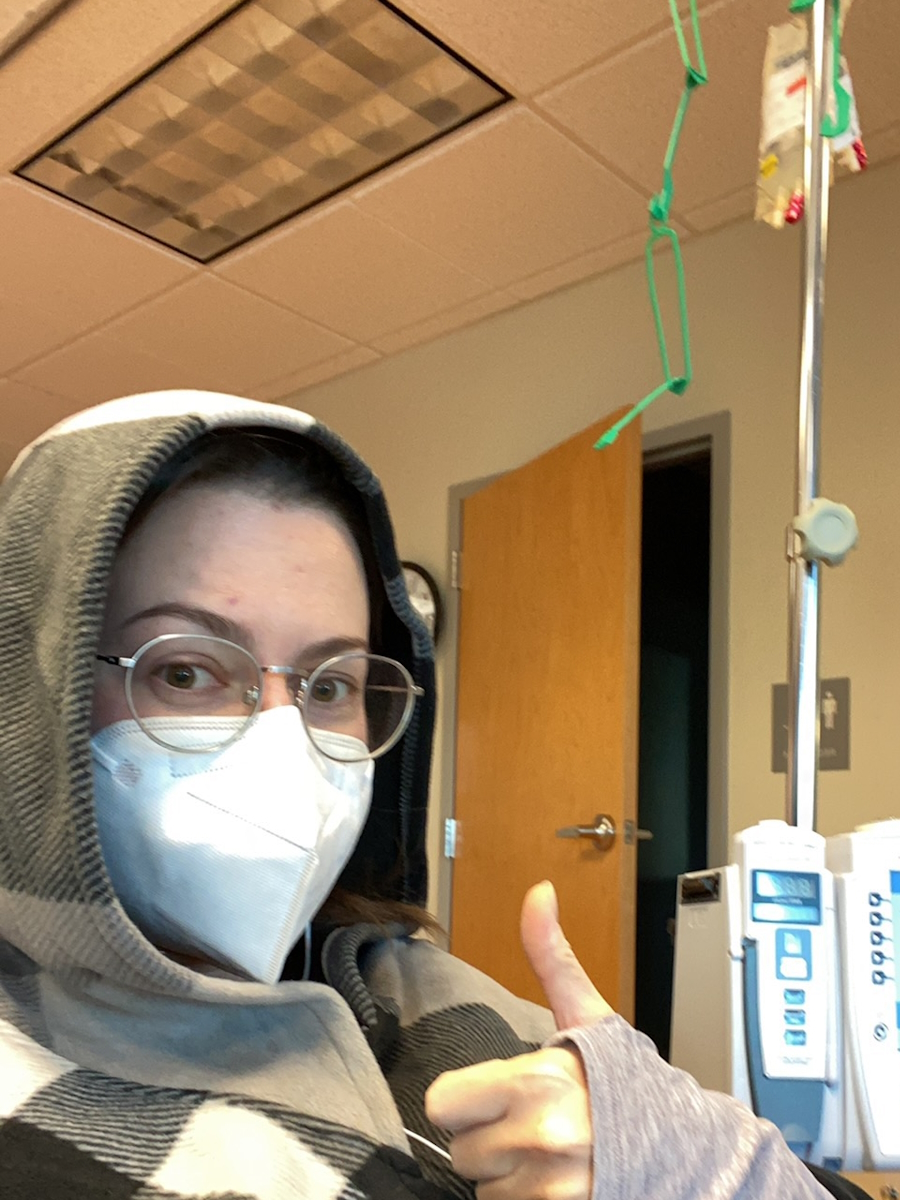
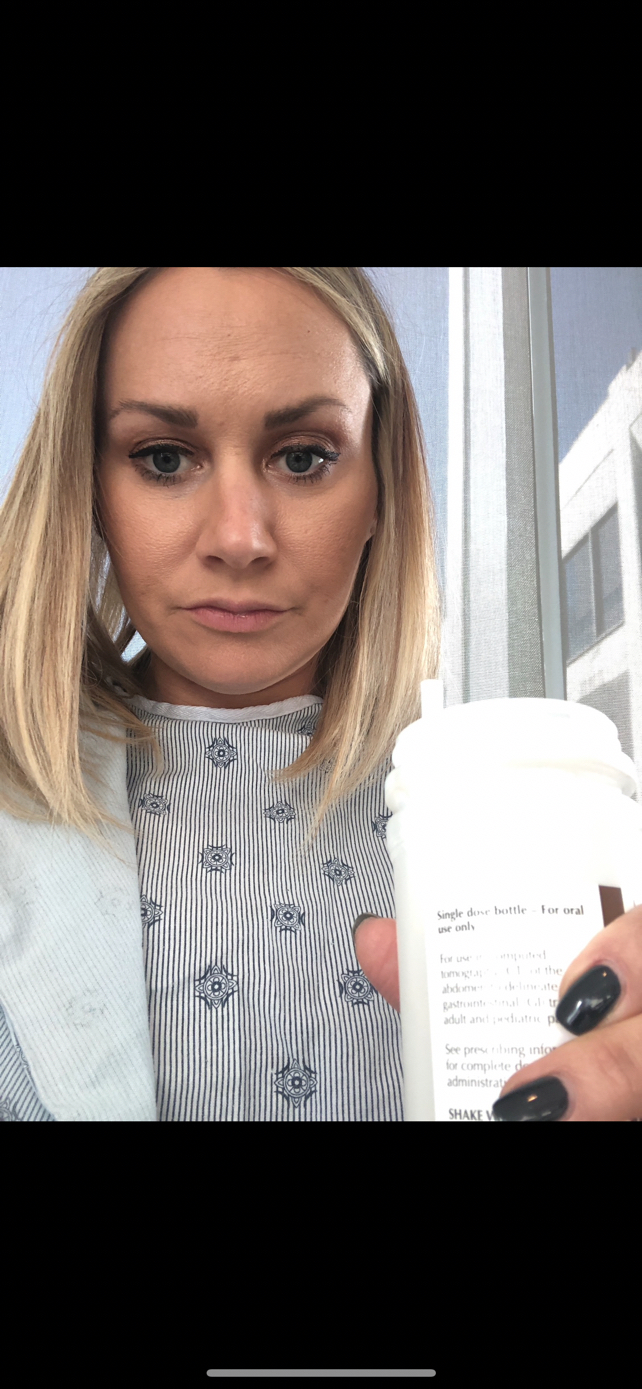
[08:25] The recommendation for me, treatment-wise moving forward, was that I had a very low risk of recurrence. My Oncotype score was one out of 100, so no chemo was recommended. But I was hormone receptor-positive, HER2-negative. The recommendation for me was tamoxifen, and that would be over a five-year period. I am at this point only three months in, but very happy to say that my side effects have been very minimal so far. I know that can change, but so far, not bad—just a little bit of sleep disturbance and fatigue, but nothing that is not manageable.
[09:10] One of the things that my oncologist, who I love, recommended was making sure you exercise every day. That was going to make the biggest difference in my side effects on that medication, so he said, “Don’t stop.” So I increased it, and I’m going to keep doing that and hope for the best moving forward. I know that side effects can be really hard sometimes, and it’s always a hard choice. It was something that I never wanted to do, which is why I chose the preventative surgery. But here we are. Just try to make the best of it and take it day by day.
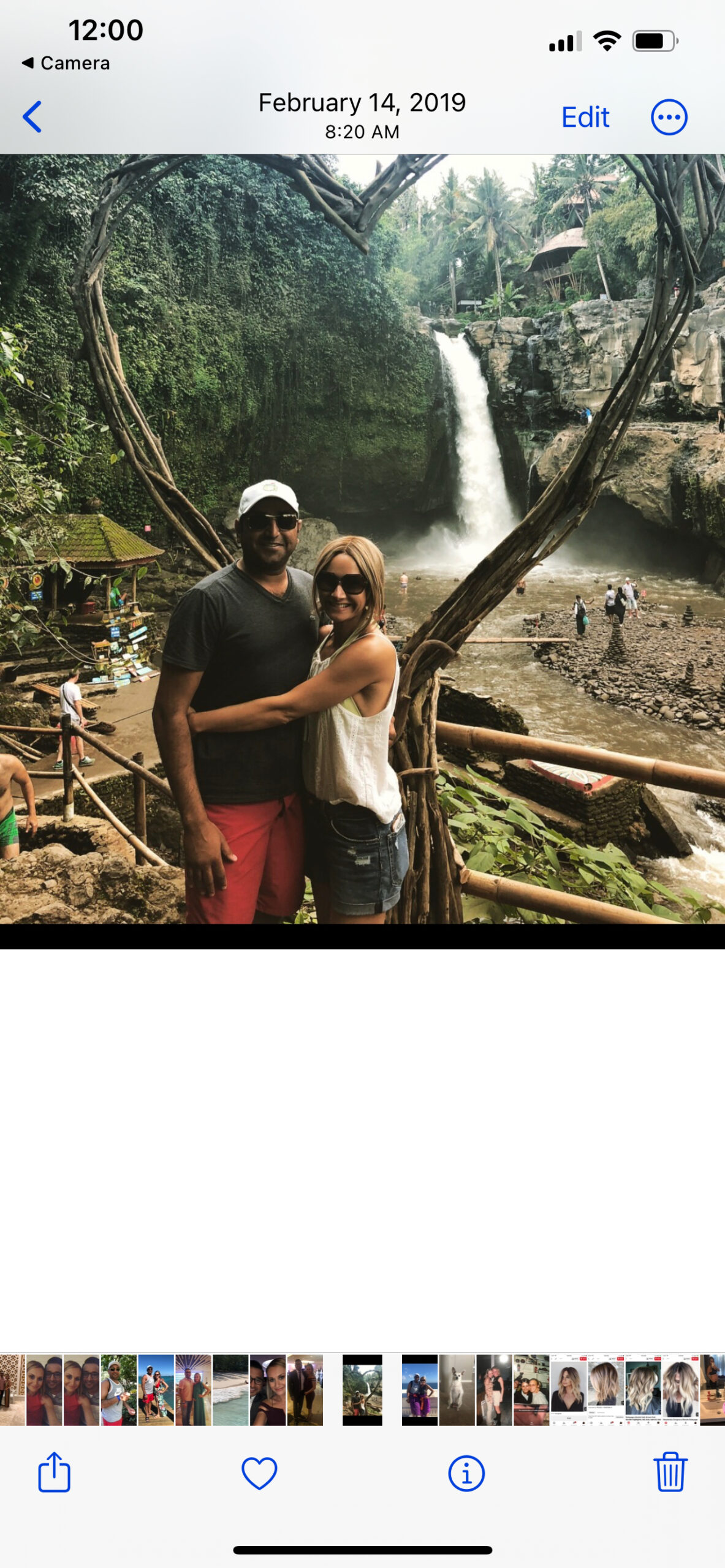
[09:52] I think I tend to carry stress well somehow, but after everything was finished, I felt this huge weight lifted off my shoulders. I remember saying to my husband, “I didn’t even realize how much I was carrying until I was done with the surgery part.” It’s a huge stressor, but I did try to do a few things during the last year as I was going through all of this that helped a lot.
[10:31] For me, I’m not necessarily a meditation person, but that is very helpful for a lot of people. For me, I have a swing on my back porch, and that’s kind of my space where I spend a lot of time. I guess it could be similar to meditation, but that was very helpful to me. I would just go out and have quiet—turn off the phone, have time to just kind of process things, and swing on my swing. Grounding is also really good.
[11:10] Having somebody to talk to is important. I’m very lucky. My husband is very supportive, and he listened to me. I’m an out-loud processor, so he listened as I made all these hard decisions and changed my mind 500 times. Just the back-and-forth, talking about all the things I’m learning about food—you have to have a person who is willing to listen and not necessarily give advice. That was very helpful.
[11:42] I’m also back to the exercise, but running is a huge stress relief for me. That was one of the things I also tried to focus on—making sure I was getting in running and doing some deep breathing.
[11:55] One of the biggest things that feels overwhelming to a lot of people who have just been diagnosed with cancer or are at high risk is, “What do I eat?” That was one of the first things that I said to my doctor, “What should I eat? Is there a specific diet that I should be on?” I talk to women every day who are asking the same questions. It is one of the most impactful things that we can do, but also one of the most overwhelming, especially if you’re trying to navigate all of these things being thrown at you with a new diagnosis and high-risk genes.
[12:34] I am in a Master’s of Medical Nutrition program right now, which I love. I get to focus a lot on the research with cancer prevention and all of the new studies that are coming out. I love it. I’m very passionate about it, but I will also say that there is no perfect plan. There’s no perfect diet that we can all do to prevent cancer, right? There’s no 100% guarantee with anything when it comes to cancer. It does what it wants.
[13:10] Some of the best recommendations I can give are to eat a lot of plants. One of the best things you can do is eat lots of fruits and vegetables. I think the recommendation is 5 or 6 servings. I try to go for 8 to 10 every day, which sounds like a lot, but once you start incorporating them and finding different ways to do it, there are so many things—fruits, vegetables, nuts, legumes, whole grains—that have so many benefits for cancer and trying to prevent cancer and reduce your risk as much as possible.
[13:47] The reason that I like to share this kind of information is because, for me personally, moving from this place of overwhelm and trying to navigate everything into a space where I felt more empowered was huge for me. I remember thinking, “I’m a nurse, and how much of this did I not know from the start, and how much have I had to learn?” I felt very fortunate to have access to a lot of courses and certifications that not everyone has.
[14:26] I feel like I owe my life to my mom and genetic testing, and I would be in a very different place without that. After I went through all of this, I felt this huge responsibility to share with others because I know there are so many people who could benefit from this information. Even if it makes a difference for one person or helps one person feel more empowered in their decision-making and informed about the options that are available, even genetic testing—if it helps one person or prevents one cancer diagnosis—it’s totally worth it.
[15:12] No matter what phase you’re going through, it’s scary, and it’s overwhelming. Whether you have been diagnosed with cancer already or are a provider who is just starting out on your journey, just know that it’s not always going to feel like it feels right now.