Madeleine’s Stage 2 Hodgkin Lymphoma Story
Madeleine was in her early 20s when she first noticed symptoms such as itching that kept her up at night. She visited the dermatologist several times who couldn’t pinpoint her issues and gave anxiety as a possible explanation for her itching. A year later, she visited her primary care doctor after developing a bad cough and lump on her neck. After multiple scans, Madeleine was diagnosed with stage 2 Hodgkin lymphoma at 22 years old.
Her oncologist was hopeful about treating her with ABVD chemo, but when the ABVD proved minimally responsive, she was given a 5-year life expectancy. This led Madeleine to change doctors and begin additional treatments. Other treatments also showed little progress, but salvage chemotherapy turned things around and opened the door for her to have a bone marrow transplant.
Today, she is cancer-free and shares her journey with us including her experience with different types of cancer treatments, why she encourages championing your mental health, how she dealt with recurrence, and her advice to others on their own cancer journeys.

- Name: Madeleine S.
- Diagnosis:
- Staging
- Stage 2
- Symptoms
- Itching on the feet, legs, and torso
- Sleeplessness
- Bad cough
- Lump on neck
- Treatment:
- Chemotherapy
- ABVD
- GVD
- ICE
- Brentuximab
- Immunotherapy
- Nivolumab
- Bone marrow transplant
- Allogeneic
- Chemotherapy
My story is still ongoing. I guess you could say the curse of cancer is the fact that it’s always going to be in the back of my mind, but the further away you are from that moment of actually getting the declaration of remission, the easier it gets.
Madeleine S.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms & Diagnosis
Tell us about yourself
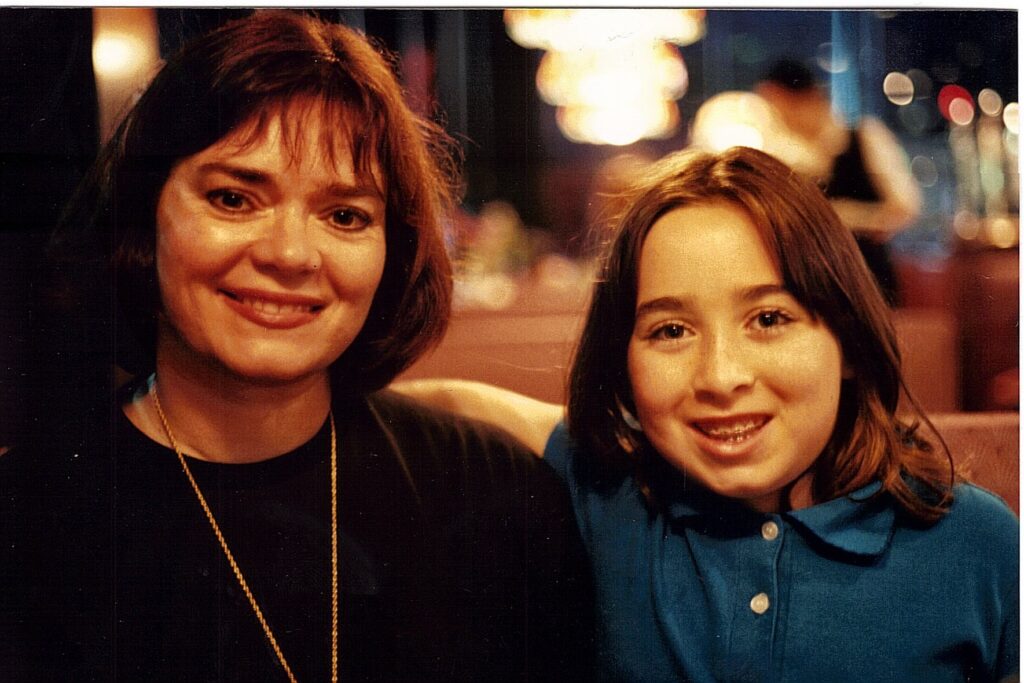
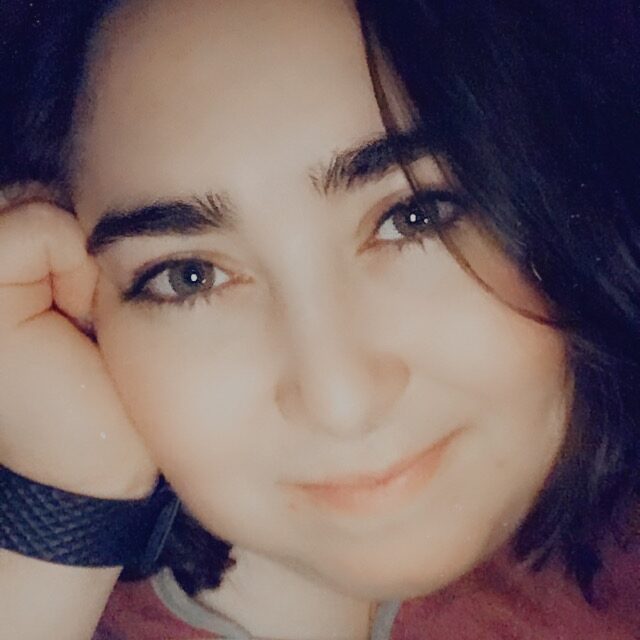
I am Maddie. I am 30 years old. I am a senior at the University of Maryland, I’m a history major, and I also work full-time as an accountant.
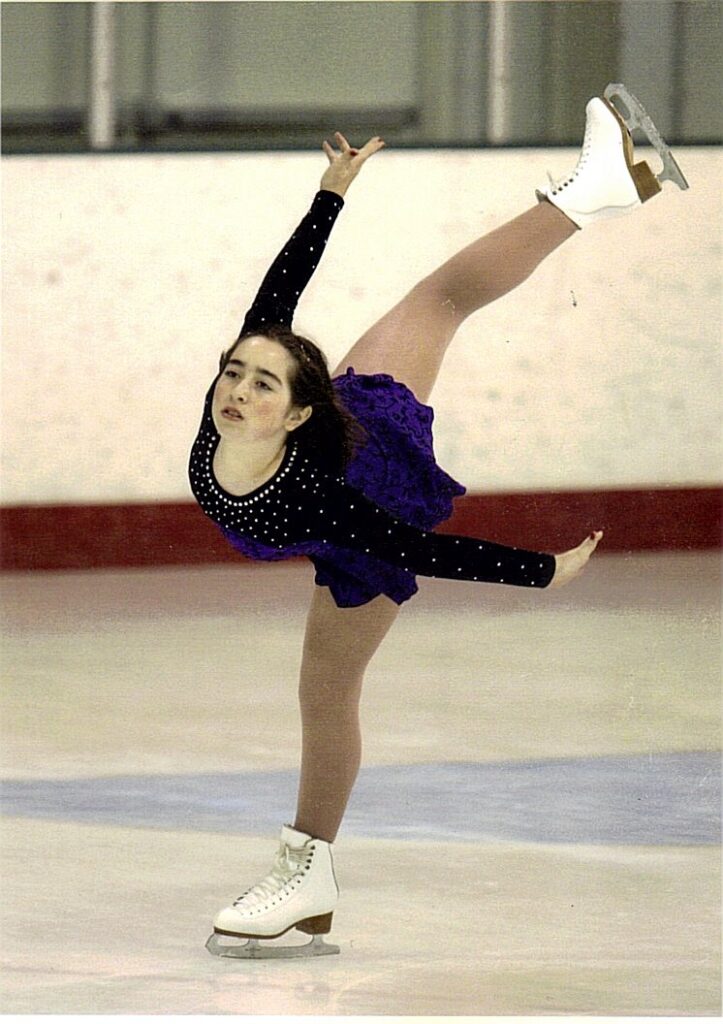
I used to be a competitive figure skater, so I do like doing that on the side. Not competitively anymore, but whenever I have the time. I’m a big fan of theater and singing. Before I was a history major, I was a theater major. That’s an active hobby of mine. I like watching movies. My friends have told me that I’m a walking IMDb.


What were your first symptoms?
Everything started a year before I was diagnosed with stage 2 Hodgkin lymphoma. I had insanely itchy skin on my feet, my legs, and my torso. For a year, I went from dermatologist to dermatologist trying to figure out what the heck was going on because it was getting to the point where I was breaking skin in the middle of the night.
That was when we knew that we were dealing with some kind of cancer.
None of the specialists could figure out what exactly was wrong. They said it was everything from eczema to it’s just in your head, it’s anxiety. It was incredibly frustrating because, after a year of no sleep, I was starting to accept the fact that this was just what I had to deal with for the rest of my life.

In April 2015, I scheduled an appointment with my primary care doctor because I had a really bad cough. The day before that appointment, I happened to be running my hand down my neck and I noticed a lump on the side, and I didn’t really think much of it.
I thought it was probably just a swollen lymph node from an infection. That would explain the coughing. I went into the appointment and that was in the back of my mind. At the very end of the appointment, I casually brought it up and my doctor said, “Yeah, that’s not normal.” Immediately she scheduled an ultrasound appointment and the ultrasound led to an MRI. The MRI led to a PET scan, and that was when we knew that we were dealing with some kind of cancer.
What did the scans show?
I got that call 2 weeks into a new job that I had just started. That was rough to take because I finally felt like things were getting back on track in my life and I had plans to go back to school that fall. But everything had to go on hold.
Did you suspect that you had cancer?
No, not at all. I don’t think I started thinking about the worst-case scenario until a family member of mine said, “My daughter had something similar.” She was worried that it was going to be a type of lymphoma, but it turned out not to be. That was the only time prior to getting my diagnosis that cancer was even on the radar at all.
I thought the odds of it were probably very slim. Come to find out, Hodgkin lymphoma is actually pretty common between ages 20 to 25, and I was 22 when I was diagnosed.
How did you process your diagnosis?
That’s when I put two and two together, that the itchiness was actually related to the cancer because it never came back after that day. It was really frustrating to know that it could have been caught a year before.
I knew I was dealing with cancer before actually finding out that it was stage 2 Hodgkin lymphoma. And that was the hardest moment. Finding out what exactly it was actually a little uplifting because I knew what I was dealing with and we had a plan to go forward.
The oncologist that I had at the time said something along the lines of, “Out of all the cancers to have, this is one of the more easily treatable ones,” which no oncologist should ever say. I think because there are so many variables, everyone’s cancer is different. Regardless of what the diagnosis is, anything could happen and my case is a perfect example of that. I didn’t last with that oncologist for very long.
I was still very upset getting the news that I had cancer. No 22-year-old really wants to hear that kind of news. That’s supposed to be when you’re in your prime. I was upset in my appointment, and my oncologist said, “You have to be strong. You have to buck up and stop crying, you’re going to get through this. It’s just 1 chemotherapy and then you’re done.” I’m like, okay, cool.
»MORE: Reacting to a Cancer Diagnosis
Chemotherapy
What were the first steps in your cancer treatment?
It was a bit of a rush getting into chemo, because before I knew it, I was doing a bone marrow transplant, a bone marrow biopsy, I was getting my port put in, and all of this was happening all at once. It was really overwhelming.
It wasn’t until that first infusion that I actually slept through the night for the first time in over a year. That’s when I put two and two together, that the itchiness was actually related to the cancer because it never came back after that day. It was really frustrating to know that it could have been caught a year before.
How did your body respond to chemotherapy?
I’m sorry to say, but it looks like you have less than a 5-year life expectancy.

After doing ABVD chemo, at the end of the year, my oncologist gave me the impression that I was basically in the clear and I could go back to normal life. I was ready to do that. I celebrated with friends. I went back to work because I had taken disability halfway through chemo. I thought it was just a really bad chapter in my life. I’m going to move on. It didn’t even take over a year so it’s okay.
Then I found out that it didn’t respond perfectly well to the ABVD. It responded, but not enough. After finding that out, the oncologist that I had at the time said, “I’m sorry to say, but it looks like you have less than a 5-year life expectancy. We’re looking at having to do ICE chemo, we have to do a transplant, and your odds aren’t really looking too good.” She recommended that I resign from my job that I had just resumed. At that point, I was like, “I need a second opinion here. I don’t feel comfortable with this.”
Were you originally given options for treatment?

There weren’t really any options. It was just the standard protocol at that time, and this was in 2015. I don’t know what it is now, but the standard protocol was ABVD for 6 months and I can’t remember how frequently I went in for infusions. I think it was every other week. I did that diligently and made every appointment on time. My mom accompanied me to every single one of those appointments.
So, no, there wasn’t really any wavering. I didn’t even ask any questions about other options because I figured that was the best case for me. Especially being told that it’s so easily treatable. So why question it if I’m getting the best care?
Did you have any side effects from chemotherapy?
Oh, yeah. There’s the usual hair thinning and the nausea, but the worst side effect for ABVD was by far mouth sores. It just really aggravated my mouth to the point where I had to eat ice chips while I was getting the infusion, which was so miserable. I had no appetite at all, so I didn’t really want to eat. All I wanted to do was sleep.
Did anything else help with the mouth sores?

Not really. It was just the ice chips. That was all they could really offer. But out of most other patients who have had chemotherapy, they thought I tolerated it really well and I think I did.
A lot of my friends, I could have fooled easily with how I was going about my day-to-day. I felt exhausted, all I wanted to do was sleep and I was depressed given everything that had been blown up in my face over the course of a few months. But I tried to give the outward appearance that everything was fine. I think I did a pretty good job of that for a while.
»MORE: Chemotherapy FAQs & Patient Stories
Recurrence
How soon after your treatment did you get scans?
We originally planned on having the last PET scan in January, which was a couple of weeks after my last infusion of ABVD. When that came back, there was a little tiny residue that was in my chest so I couldn’t feel lumps or anything.

They said that there was a little tiny speck in the middle of my chest, and I was given an option. We can assume that this is a recurrence, or there’s the possibility that it’s just scar tissue. If that’s the case, then we can just do a repeat PET scan and see what happens. I went with that option thinking it was behind me still. When that repeat PET scan came back, it came back aggressive.
How did you react to having cancer recurrence?
At the time, it was just a complete shock. I didn’t really know what to make of the future anymore. I was distressed, but I look back on it and actually, there’s a lot of pent-up anger around that because it’s like there are so many things that could have been done differently. There’s the possibility that it could have been avoided altogether if I had gotten diagnosed sooner or if I had actually just treated it as a recurrence. Maybe my cancer journey would have been shortened by a half.
But at the time, I was in a lot of distress, and the only thing I could think of at the time was, “I’m not going to just give up.” I wanted to get a second opinion. I wanted to find out if there were other options besides ICE chemo because I was told, that out of all the chemo options out there, it’s one of the more toxic ones. At the time, I was only 23 and I still had so many things I wanted to do with my life. One of them was to eventually have a family of my own and to be able to have a kid of my own.
Did you discuss preserving fertility with your doctor?

I don’t really remember what the conversations were like with my oncologist, but I do remember having the conversations with my family. My immediate family was very supportive of whatever I wanted to do in terms of preserving whatever I could after having 6 months of chemo.
Then there were some family members and also friends of mine who had just learned about the incident. They weren’t as supportive. They were like, “This is God’s plan. There are so many kids out there who need to be adopted.” I know that, and my original dream was to have my own kid plus adopt. But to have cancer rob me of one more thing, I didn’t really want to let that stand. So I went through the fertility treatment prior to doing the next chemotherapy.
Do you feel your medical team encouraged you to preserve fertility?
When I asked for a second opinion, they sent me directly to Johns Hopkins and I saw one of the best specialists specifically for lymphomas there. He strongly recommended that if I want to have my kid, don’t jeopardize it. I should definitely consider it. Especially because I was looking at potentially doing a transplant at that time if I ever made it to remission. He said, “If you do a transplant, the odds of you having your own kid without any kind of assistance is pretty much impossible.”
[With my first oncologist], I do remember it being brought up, but it was kind of dismissed because they were like, “You’re young and a lot of people bounce back.” At the time, it wasn’t covered under any kind of insurance. It would have been paid completely out of pocket and I didn’t have the funds for it. Neither did my family. So I was like, I’ll take the risk.
It wasn’t until afterward when I was facing a transplant, I was like, this is something that I really want and I want to invest in. I held a GoFundMe and the people who were supportive of me supported it.
What did you discover after receiving a second opinion?

When I asked for a second opinion, they sent me to Johns Hopkins. That was where I found out there are a ton of options. There are clinical trials, there’s immunotherapy that’s just come out for Hodgkin lymphoma. Besides that, there were other chemo options out there that weren’t as toxic as ICE chemo.
He said, “Since you’re familiar with chemotherapies, brentuximab has some of the better results and it’s not as toxic.” He recommended doing that. After discussing it in thorough detail with him, and I had my parents with me in the room, we all decided that that was the better course. When I went back to my main oncologist, I immediately sought a different one. The second oncologist that I went with ended up being the one who saved my life ultimately.
Switching Treatment
How did your body respond to brentuximab?
I did brentuximab after doing all the fertility treatment and all it really did was stabilize the cancer. It didn’t do a whole lot, unfortunately. When it became apparent after a couple of months of it not doing anything, it was like, okay, we need to look at another option.
Exploring clinical trials
That was when my new oncologist said there were some clinical trials going on at NIH. He assembled a team of doctors from both Johns Hopkins and NIH to find out what everyone’s opinions were on the situation. He sent me over to NIH to get every scan and test done under the sun. Then I finally met with the team over there, and I had never felt like a lab rat more in my life because they were all talking about statistics and everything. It was a lot to take in.

They presented all these different options. They presented the clinical trial which was the CAR-T cell project, but it was in its beta phase so it had only just come out with recent results. They said, “Before we even think about doing that, there’s one more option that we want you to try, which is an immunotherapy called nivolumab.” I said, “Okay, sure, let’s do that.” It was basically like chemotherapy, but again, less toxic. I went with that and that one almost killed me actually.
Describe your experience with nivolumab
I went in for my first infusion thinking nothing of it. It’s like any other infusion that I’ve had. I was seeing the same crew of nurses that I’d seen for a year now, and I remember them hooking it up and maybe 2 minutes into the infusion, I couldn’t breathe. I felt like something in my chest was cut off. I was really struggling to take another breath and immediately hit the emergency button.
I was in a panic and they said, “It sometimes happens. Maybe it’s because we were putting the drugs into your system too quickly.” They slowed it down in the next infusion and it worked out a little easier for me. I still had a little bit of chest pain, but it was something I could put up with. I figured it was going to do its job. Why not just put up with it?
Is breathlessness a common side effect of nivolumab?
For that drug in particular, it’s not exactly a common side effect to have. I think it was just an error with how quickly it was being administered to me. But I mean, after having an incident like that, that kind of changes your perspective on future infusions. You’re very, very cautious going forward after that. Beforehand I had really no major issues. I tolerated the treatments rather well, so this took me by surprise a bit.
It honestly had no benefit at all. It actually gave me lasting problems to this day. I’ve had thyroid problems ever since. Prior to that drug, I never had any issues. It was actually very upsetting being told that I would have to be on medication for life when I didn’t have to deal with that beforehand. Mind you, prior to cancer, I was healthy, I was active, so this was very upsetting.
That’s when I started to see a decline in my mental health because I was starting to feel very hopeless. It was after the nivolumab that I was told, “We’re looking at something that’s incurable here,” which was very hard to take.
They said that the clinical trial was still an option, but because of how early on in the phase it was, it basically would just buy me time. I was like, okay, well, it’s better than nothing.

Did you have a cancer support group?
I had an amazing support group that I had been attending and they all lifted me up. When I was told that news that we’re basically facing something that’s incurable, the first thing that they all wanted to do was take me out and treat me to dinner. We all partied up.



They also asked if there was anything that I would want to do before the end and what would it be. At that time, I was like, “All I want to do right now is go and see family that I haven’t seen in a decade in France.” They set up my second GoFundMe, which I didn’t really feel comfortable with, but they set it up so that I would be able to go and see my family. The intention was basically to say goodbye to them.
Clinical Trial
Preparing to go on a clinical trial
With that in place, I started preparing for the clinical trial at NIH. I had done all the tests and everything, but my lab work came back and showed that I had increased levels of estrogen despite all the chemo that I had undergone. They said, “Because your estrogen levels are too high, you’re technically not able to go through with the clinical trial just yet. We have to put you on hormone therapy. In the meantime, while you’re doing the hormone therapy, we’re going to have you go on salvage chemotherapy,” which was GVD.

Salvage chemo leads to a breakthrough
It was just supposed to hold me over until my levels were at the right place so that I could do the clinical trial. However, 2 months into doing the salvage chemo, which was not supposed to have really any effect, I started bouncing back. I noticed a significant decrease in the lumps that had recently formed after the nivolumab, and no one saw it coming. It was like, okay, clinical trial is no longer at the forefront. We’re looking at another opportunity for a bone marrow transplant.
I was thrilled and ecstatic. I saw hope in the future. But when having the discussion about the transplant, given everything that had happened, my team of doctors broke it up into thirds. “There’s a third possibility that you accept the transplant and it goes great and you’re in remission. Awesome. There’s a third chance that there are complications during the transplant and cancer doesn’t go away in the end and we have to take it from there. There’s also the potential third percentage that you don’t even make it at all. That you don’t respond at all to the transplant.”
Two months into doing the salvage chemo, which was not supposed to have really any effect, I started bouncing back.

Delaying the transplant
After having that conversation, I was still determined to go to France and see family, because nothing is guaranteed. At the time, when we had made travel plans, I was reaching a state of temporary remission, and my doctor was like, “You should really think about dropping your plans and going into transplant.” I was like, “Yes, I have every intention of doing that. But my mental health right now is at an all-time low. I am under the impression that you have to go forward with a positive outlook here.”
I knew that if there was the potential that I wasn’t going to pull through and I wasn’t going to get into remission after the transplant, I would regret not being able to see my family. Because at that point, I probably would have been too weak to even do that. After talking to my doctor for several minutes, I was like, “Okay, this is what I want.” That was the first time in a while that I really called the shots. Come to look back on it, I actually regret doing it because when I came back from my travels, there was a regrowth happening.



What treatment options did you have at this point?
At first, my oncologist was sort of optimistic. He said, “You know, the GVD worked before. Let’s have you go back on it for another 2 infusions and see what happens.” It became apparent that I was no longer responding to it so I was right back where I was at the start having to face a decision. It was the final decision at that point. Either I’m going to go into the clinical trial or I’m going to do the last option available to me, which was the chemotherapy, which my first oncologist was the one who recommended from the start.

I had a really strong gut feeling that doing chemo was the right thing to do.
I remember having that conversation with my oncologist over the phone. Surprisingly, I wasn’t really upset anymore. I think it was because I had actually taken the initiative of going to see family and doing what I wanted to do in my life that made me content with whatever outcome was going to happen.
I asked my oncologist, “Can I have a day to think about which option I want to go with?” Because both had major risks involved. He said okay. The next day, I basically spent the entire time contemplating and thinking and weighing the pros and cons and deciding what I felt most comfortable with.
When my oncologist finally called over the phone, I just had a very, very strong gut feeling. I can’t even really describe it. I had a really strong gut feeling that doing chemo was the right thing to do. When I told him that specifically, he said, “If you have a good feeling about it, then I’m all for it.” So we went with the chemotherapy and that ended up actually being the miracle.
Bone Marrow Transplant
Preparing to go on ICE chemotherapy

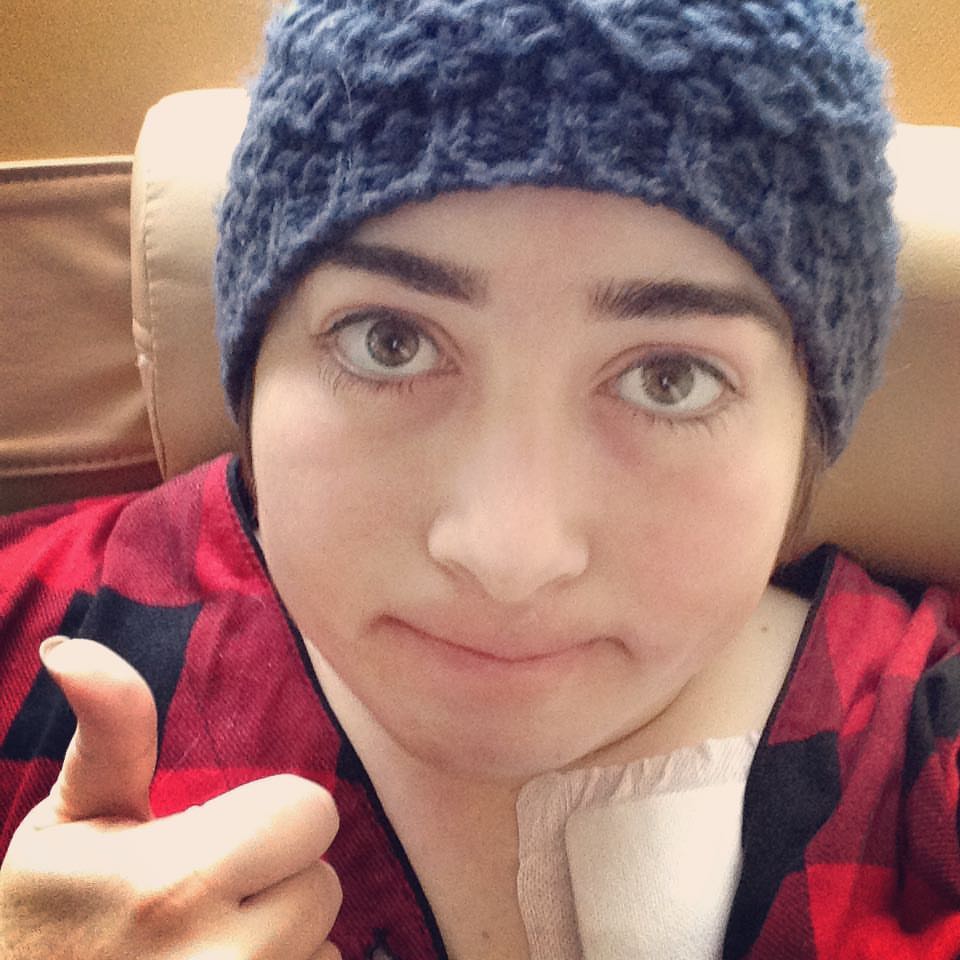
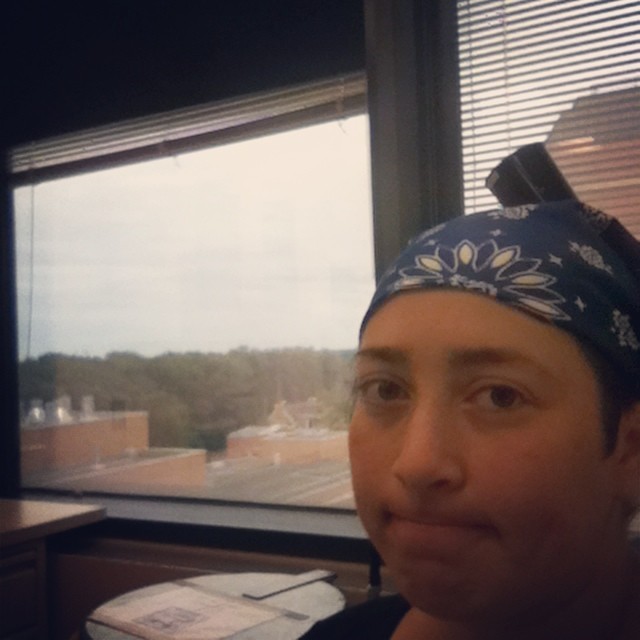
ICE was a whole different game because, unlike the previous infusions where I just went to my doctor’s office and sat in the infusion center for a couple of hours, I actually had to be hospitalized this time. That was the first time I ever had to be hospitalized through the whole cancer situation. It was right after the holidays, too. There was trouble trying to book things because everyone didn’t want to be in the hospital over the holidays. Finding a bed was rather difficult, but they managed to squeeze me in at the start of January.
Describe your side effects on ICE chemotherapy

The side effects were pretty brutal. I was very nauseous and very fatigued. I know I had friends visit me in the hospital, but my recollection of it is very limited. When I was looking back at photos, I found a photo of a friend who had come by, and I’m like, I don’t even remember them swinging by at all. That’s how completely out of it I was.
But at the end of every infusion, I was re-energized. I was like, yeah, let’s get out of here. One of my good friends from my support group was the one to come and pick me up and take me home. But before going home, she took me to support group, and she treated it like bailing me out of prison. That was memorable. But getting the infusion, it’s kind of a blur.
How soon after beginning ICE did you get scans?
Originally, I had been getting PET scans, I want to say, once every 3 months because they don’t want to put them too close back to back. There’s a lot of radiation involved, which is already a phobia of mine. But after the second infusion of ICE – there were only 3 that were given – I didn’t feel any lumps anymore. I had a very strange feeling that this had actually worked.
My oncologist said, “You know what? Let’s schedule a PET scan first thing tomorrow.” The PET scan showed almost complete remission, and no one expected that. It shocked not only my oncologist but also the whole team of doctors that had been in communication. They were like, “Oh my God, we need to fast-track her into a transplant immediately. No waiting.” My oncologist was even like, “Don’t go traveling anywhere.” I said, “I have no intention of doing so. This is a golden opportunity here.”
Preparing for a bone marrow transplant
By that time, we already knew that if I did make it to transplant, my sister was going to be my donor. They got her into all of her tests and labs and everything. It was a whirlwind over a month’s time of getting all those tests and everything done because we were trying to erase the clock. They decided to bypass the third infusion just to get into transplant. If at any point during those tests and scans, there was any kind of recurrence, then it’s off the table. It was a race against the clock.
Finally, on March 15th or 14th I ended up moving out to Baltimore and I started the transplant. I had an allogeneic bone marrow transplant. Originally, the idea was to get autologous, which is a lot easier. You’re not dealing with a donor, you’re dealing with your own cells. But because of all the recurrences I had, that was off the table.
So we were dealing with a donor, and that poses more complications or the potential of more complications, specifically graft versus host disease. Because of that, they have you stay at the hospital for whatever length of time they recommend. For me, they recommended 3 months of being in and out of constant care.
Describe your experience with getting a bone marrow transplant
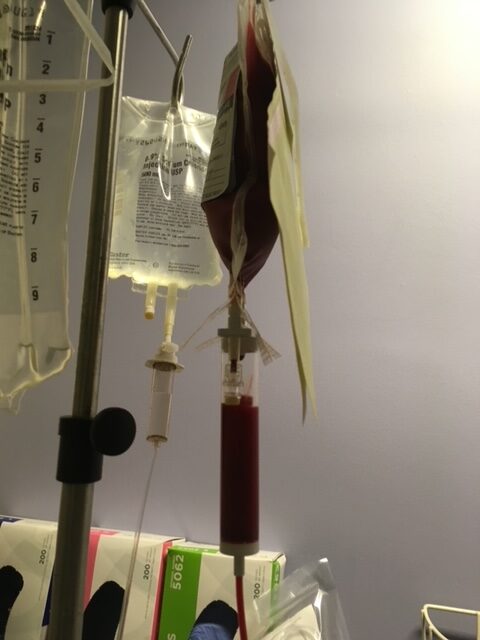
They had me stay in housing right across the street from the cancer center at Johns Hopkins. I would just walk across the street every other day almost to get looked at, and take my vitals. Every once in a while I had to do blood transfusions because when you go through the process of a bone marrow transplant, you’re immunity is shot. You undergo 5 days of really, really aggressive chemotherapy followed by total body radiation and I did that for 20 minutes.
Then you do the transplant. The funny part is that they say that the transplant is supposed to be the most boring day out of the whole duration that you’re out there. But for me, my odds have never been great. That ended up being the scariest day of my life. Even though my sister and I were pretty much a perfect match, we had different blood types. When they collected her bone marrow, some of her blood cells got in, and it triggered a horrible reaction to the point where I had to stay under observation for over 24 hours, and I was in and out of consciousness.

I was absolutely sick. Every time I would get back into consciousness, the thoughts going through my head were, “Oh, this is it. This is what they were talking about, that third possibility.” After that, they just monitor you and you’re taking antifungal and antibacterial medication to try to watch as your levels slowly climb back up from ground 0.
»MORE: Managing Nausea and Vomiting from Chemotherapy
What was the follow-up to your transplant like?
After the transplant is one giant blur. I take that back, the first couple of days. The first couple of days were pretty traumatic. Not just because of the transplant day occurrence, but shortly after that, my very good friend Needa, the girl who used to bail me out of the hospital, passed away. She had been in remission up until the point where I went in for ICE chemo. As I was slowly getting better, she was steadily getting worse.
That was very, very difficult for me to take because it really felt like, even though it really makes no sense, it really felt like something in the universe swapped. It felt like I was swapping places with her. It felt wrong because she had so much to live for. She was amazing. After that day, it became a blur. When Needa passed away, that was pretty much where I shut down. All I wanted to do was wake up, have a little something to eat, walk across the street, get monitored, walk back across the street, and go to sleep. I did that for 3 months.
Quality of Life
A second lease on life

When you’re out there for a transplant, you have to have a caregiver with you at all times just in case. I had a whole calendar of friends and family members who would take shifts and be with me. Half of half of those shifts, I don’t even really remember. I don’t remember half of the friends who came by and spent time with me because I was so out of it.
As I steadily approached the end of the whole transplant ordeal, and I was getting catheters taken out, I was like, I’ve been standing on the sidelines for so long watching all my friends move on with their lives. I’ve been given a second lease on life, so I want to get back out there. I want to go and do the things that I want to do, which was first, go back to school and get my degree.
After speaking with the nurses, I managed to sign myself up and register for classes that summer. It was a way to distract me from all of the horrible stuff that had happened over the last 3 years. I put all of that in a closet in the back of my mind, locked it away, and was like, I’m going to focus on my studies. I’m going to get straight As. I made the Dean’s list every semester. But that stuff catches up with you after some time.
Describe the transition back to normal life post-cancer

At first, it was really uncomfortable because I was going back to school and my head was shaved. I didn’t recognize my body anymore. From all of the stuff that had happened with the thyroid problems, I ballooned and I hated my appearance. I just felt very uncomfortable.
I was still so determined to try to reclaim whatever normal part of my life I could that I just kept my head down, and focused on my studies. The following year, I also got a job part-time working at a grocery store just to get myself through school. It was an interesting transition, to say the least.
I was still attending the support group, but as time went on, it felt very strange being in a support group where people were either actively in treatment or they were facing a recurrence. There was a seed of guilt that was growing because it was like, I’m okay right now. So how do you make sense of that? You can’t really.
Dating after a cancer diagnosis

I kept off for a while after the transplant. In my support group, everyone was basically already married and already had kids. That was never really an issue that was brought up despite it being a young adult support group. The only other young adult who was single was Needa. When she passed away, it was just me there. That was another thing that made it uncomfortable still being in that group setting because it felt like my needs weren’t really being addressed anymore.
It’s hard to introduce yourself to someone who doesn’t know you, who’s wondering why you’re wearing headscarves every day. Even after treatment, it’s like, how do you explain the last 3 years of your life? When they ask you, “What do you like to do for fun?” It’s like, “Well, right now I’m too tired to really do anything.” I used to have this ongoing joke that I’m a full-time cancer survivor to try to find a little humor in anything I could.
Dating was very, very difficult for a while there. It wasn’t until probably 2021 when I started really putting myself back out there. That was in the middle of the pandemic so it was horrible timing.
Describe the fertility preservation process
I went to Shady Grove Fertility here in Gaithersburg, Maryland. Out of all of the doctors – outside of my oncologist – that I interacted with, the doctors and nurses there were out of this world amazing. It was all out-of-pocket costs to do any kind of fertility preservation. It’s not just withdrawing eggs, it’s also like the lead-up to that. Having to go in for ultrasounds, having to get the medication to actually produce those eggs, and they’re not cheap.
When I mentioned to the doctor in my first consultation that the only reason I was doing this was because this is where I’m at. I’m facing a bone marrow transplant in the near future. He felt really sorry for me. He said, “I’m going to discuss things with the finances department and we’ll see what we can do for you.”
At my first appointment, when I showed up for an ultrasound, they were trying to teach people how to give themselves self-injections for medication. Which, at the time, I was not really fond of needles. Finding out that was something that I would have to do twice a day, that was something. But when I went to that teaching class, they gave me a giant bag full of all the meds that I would need. They said, “Don’t worry about it. It’s covered. The nurses all pitched in.” I remember crying when I left the place. They covered basically everything except for the actual retrieval date. Without their help, I probably wouldn’t have been able to do any of that. It was a mind-blowing experience, to say the least.
»MORE: Fertility After Cancer Diagnosis
Reflections
What advice would you give someone on their own cancer journey?
First, don’t ever make the mistake that I made by just assuming standard protocol is the thing for you because it might not be. I strongly recommend getting a second opinion, even if your oncologist is one that you really like. Always get a second opinion from a specialist, another oncologist, or someone. Because there might be treatment options that they aren’t even aware of that another person might be.
When it comes to picking a treatment option, if you have more than one option available, look at not just the statistics, but also the side effects. You have to weigh the pros and cons and figure out what you think your body is going to be able to tolerate. The reason I went with ICE chemo over the clinical trial was because it was something that I was more familiar with, and that I knew that my body would probably be able to tolerate, even if it was the more toxic out of the 2. That’s on top of the fact that, statistically, there was a better outcome than through the clinical trial. I’m sure you know, that statistics constantly change.



I strongly recommend getting a second opinion, even if your oncologist is one that you really like.
Don’t let my my story prevent you from actually looking into clinical trial options, because I know quite a few people who had success come from their clinical trials. That’s always something you want to weigh as an option.
It’s always good to communicate with not just your oncologist or your team of doctors, but also family members, your significant other, or your friends because those are your caregivers. If there’s one thing that I noticed over the 3 years of undergoing treatment after treatment is, that it’s not just you who’s having to cope with the the potential of a bad outcome. It’s also the people around you and it plays a huge role in the way that you look at your treatment. If they’re going into it with a positive attitude, that rubs off on you and vice versa. Definitely something to discuss with them.
Recognizing that everyone’s cancer journey is unique
If there’s one thing that my support group constantly mentioned was, don’t always buy into the statistics because they’re not always right. Half the time they’re not even really up to date. Like I said at the beginning, everyone’s cancer is different. Everyone’s cancer is unique. If you look at statistics, I wasn’t supposed to have pulled through this, and yet, I’m still here. My friend Needa was supposed to have her whole life ahead of her. You can’t just look at cancer at face value and say, “Oh, yeah, that one’s more easily treatable in comparison to this other cancer.” It doesn’t work like that. Doctors really need to consider that because you’re giving your patients false hope that way, and it only bites them in the end.
The other thing I would say is definitely prioritize your mental health because that’s something that, even after your chemo treatments and everything, is going to play a huge role in your recovery process. That was something that I didn’t address immediately, and I wish I had. The more you put that off, the more you think, “Oh, yeah, I’m fine now that life is going to go back to normal.” The harder it’s going to be to move past all of the trauma that you went through. Even if it’s 6 months or 3 years of chemo, it’s still a huge, huge impact on your life. Your whole world gets flipped upside down and that’s something that you need to address with, a professional. I strongly recommend you prioritize your mental health just as much as you value your physical health.
»MORE: Cancer and Mental Health

My story is still ongoing. I guess you could say the curse of cancer is the fact that it’s always going to be in the back of my mind, but the further away you are from that moment of actually getting the declaration of remission, the easier it gets. I probably wouldn’t even be here right now if it wasn’t for the support system that I have in place, not just with the therapist, but with family, my very close friends, and the support group that got me through it. I have so many people to thank for just being here. The only way I can really give that back is just to be there for others and give as much support as I possibly can to the cancer community.
More Hodgkin Lymphoma Stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta






