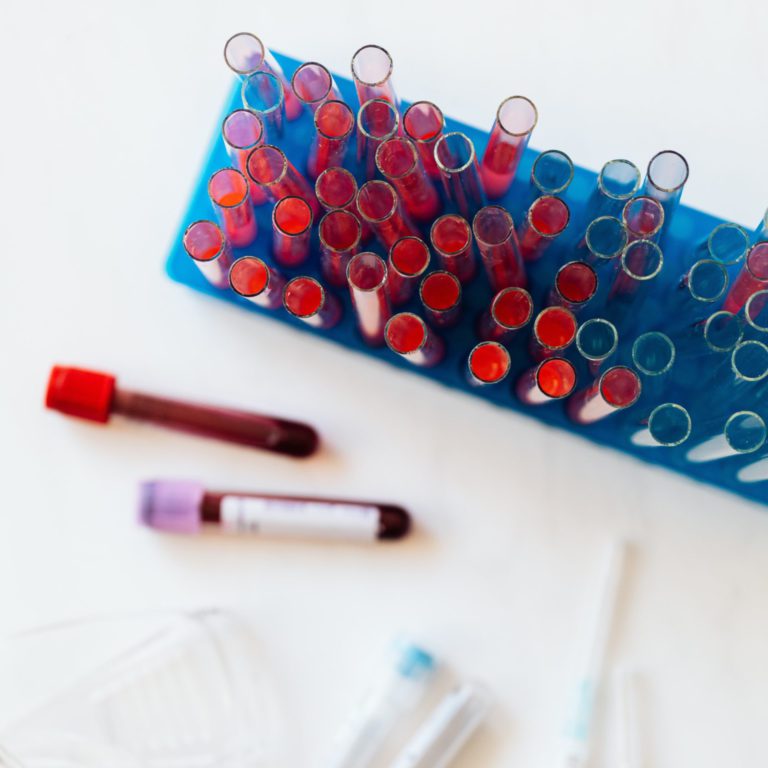
“For the most part, it’s found by doing a routine blood check by an internist. Usually, they first notice that the white blood cell count is a little high, so they send the patient for a referral,” Barrientos says.
“Sometimes, people might be shaving or washing their face and notice they have an enlarged lymph node. In that case, we’d do a biopsy, and the biopsy would show leukemia.“
This means that CLL can present in your blood, your lymph nodes, or both.
Dr. Barrientos explains that there are three major categories of patients.
One-third won’t develop symptoms, but they will be affected in the sense that they will be at a high risk for infections and malignancies.
Another third won’t need treatment right away, but they usually start up to three years after diagnosis.
The last third of patients will be showing problematic symptoms like anemia, low platelets, or painful, enlarged lymph nodes. They will require treatment immediately. In these cases, not only is their age and medical history taken into account, but also things like their lifestyle and how the patient will tolerate the prescribed treatment.