Shared Treatment Decision Making in CLL
How to Be an Empowered CLL Patient
Updated October 9, 2023. Originally broadcast September 20, 2023.
Quality of life and precision are top of mind for chronic lymphocytic leukemia (CLL) patients. Understanding the complexities of available treatments can help you optimize your CLL care and prioritize the questions to ask your doctor.
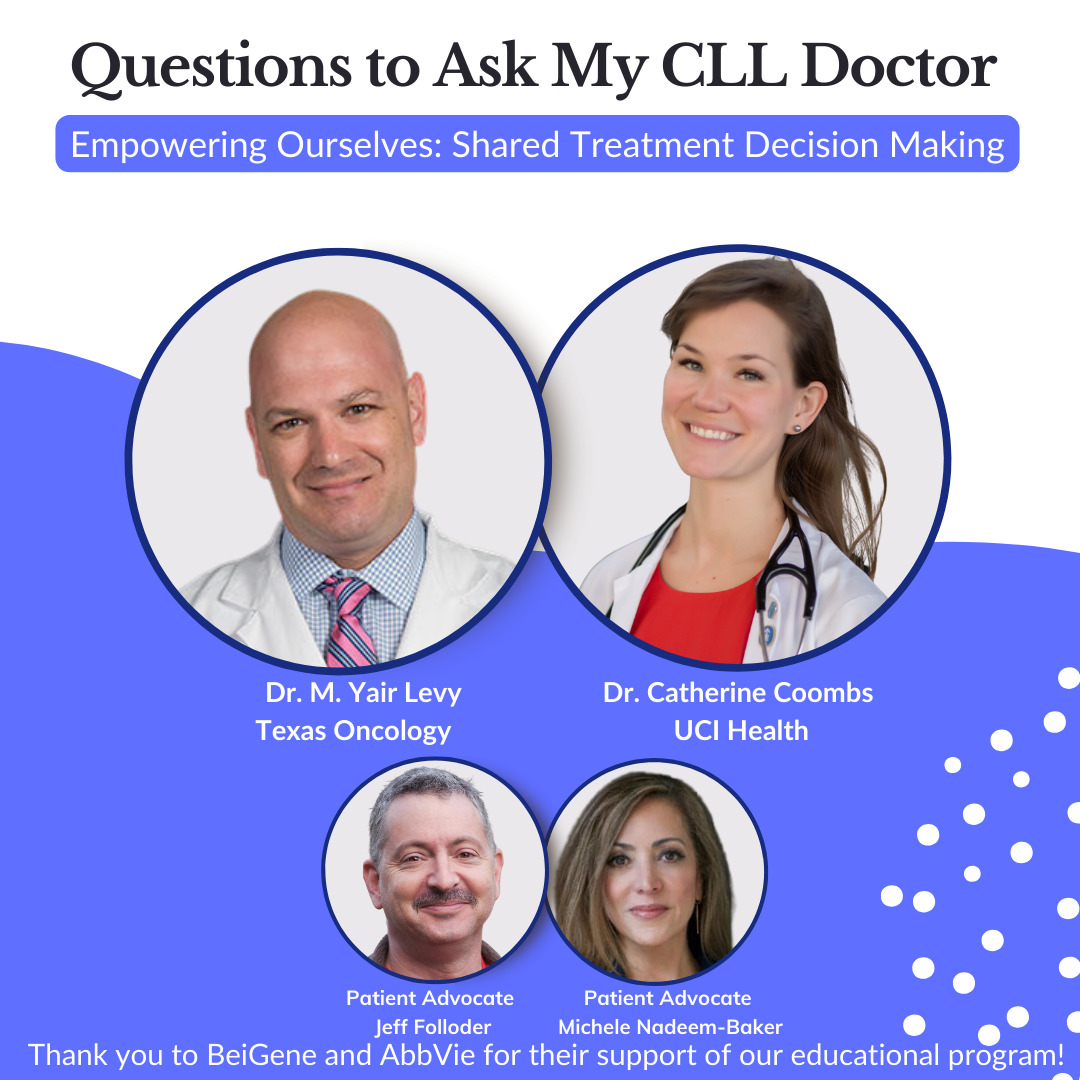
During this live conversation, panelists Dr. M. Yair Levy, director of hematologic malignancies research at Texas Oncology, and Dr. Catherine Coombs, a hematologist oncologist at UCI Health who specializes in CLL, discussed the latest in CLL care. The discussion was hosted by CLL patients, advocates, and administrators of the CLL Support Facebook group Michele-Nadeem Baker and Jeff Folloder.
This discussion covers the current landscape of CLL treatment and care options, as well as new CLL treatments awaiting FDA approval, factors doctors consider when starting or switching a patient’s treatment, encouragement for CLL patients to advocate for themselves, and each doctor’s outlook on CLL treatment and patient quality of life.
There is hope. Hope to live a normal life, and hope to see your kids and your grandkids grow up. There’s always hope on the horizon, in my opinion.
Dr. Catherine Coombs


Thank you to AbbVie and BeiGene for their support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- Changes and improvements in CLL treatment
- How CLL doctors are providing CLL patients with precision care
- The role of patient comorbidities in CLL care
- The benefits of watch and wait
- Considering the duration of treatment for CLL patients
- Factors in choosing a first-line treatment for CLL
- The benefits of monoclonal antibodies for some CLL patients
- What CLL doctors consider before ramping up treatment and dosing
- Considering the side effects of CLL treatments
- Reasons to switch a CLL patient’s inhibitor
- New CLL treatments awaiting FDA approval
- CLL doctors’ top takeaways
- Encouragement for CLL patients to advocate for themselves
- Navigating what symptoms you should share with your doctor

Introduction
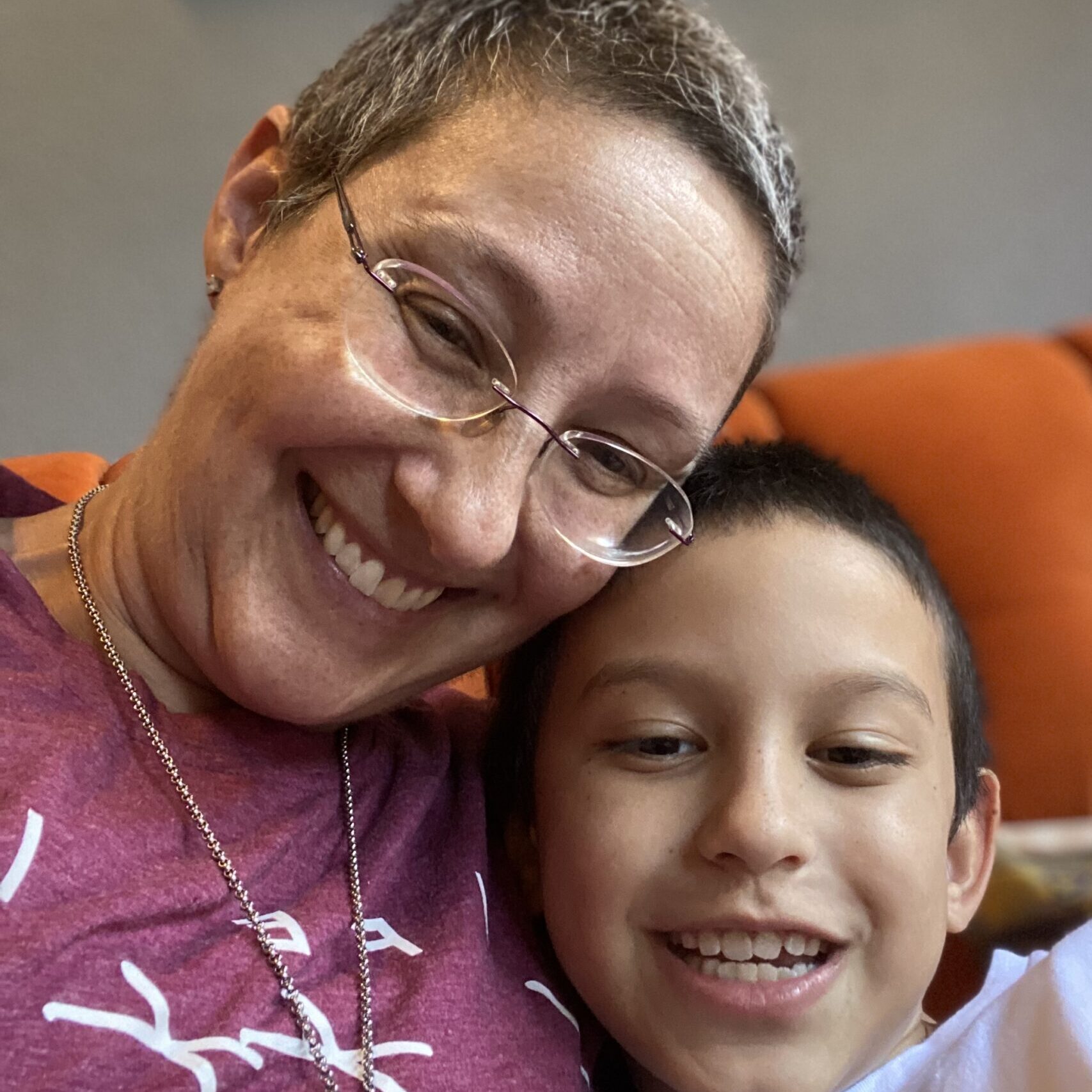
Michele-Nadeem Baker: I’m Michele-Nadeem Baker. I’m a medical and health journalist, but in addition to that, I am also a patient. I started advocating for other patients on my first day of treatment when I realized that there was so much unknown out there and to demystify things for my fellow patients and help them through their journey.
Jeff Folloder: My name is Jeff Folloder. I am a passionate patient advocate. I am now in year 14 of my little journey with CLL and I am living a great life. That’s why I became a patient advocate because I want to make sure that everyone knows that it is possible to live a great life with CLL.
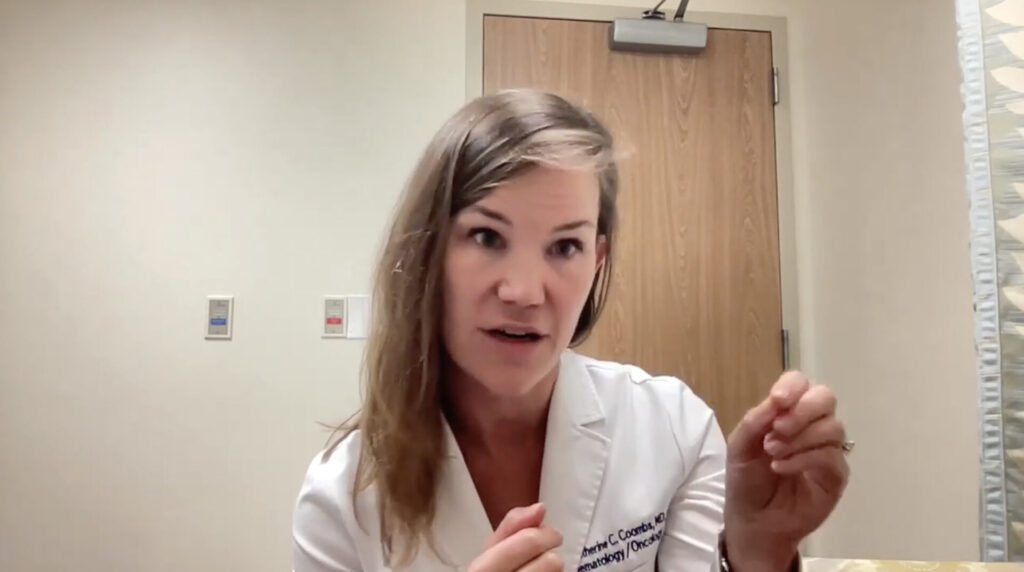
First up, I get to introduce Dr. Catherine Coombs. She is a hematologist oncologist with UCI Health and she specializes in chronic lymphocytic leukemia. She also helps lead clinical trials, trying to find better ways to treat CLL. Dr. Coombs, tell me what drew you to specializing in CLL. We don’t hear that a lot.
Dr. Catherine Coombs: It was a long road. I went into medical school knowing I wanted to be a cancer doctor. I didn’t have any doctors in my family, but I do have a lot of family members with cancer. It always inspired me to be on the patient end of the oncologic relationship. That’s always what I thought I would do.
Now, I didn’t decide on CLL until my residency years. I looked for a research project right away, because that’s the only way to get into a good fellowship program is by doing research. It always was something I wanted to do regardless. I found a wonderful mentor in my time at Duke University as a resident, Mark Llaneza, where I focused on the underlying genetic risk of CLL as my residency project. That drew me to the field right away.
Then I saw all these other benefits of being a CLL-focused clinician, which is that the patients do really well and they live a long time. I love having that long-term relationship with my patients. I love blood cancers in general, but I would say the acute leukemias, which I had focused on a bit earlier on in my time as a faculty when I was doing a bit of both were hard because there are a lot of patients that we lose and I really admire the docs that do it. But I think for my long-term well-being, I know that it’s just so much more gratifying and less emotionally traumatic to be able to have patients that thrive for so many years and be able to really enjoy those relationships as the added benefit.
The therapeutics have just continued to improve over the 13 years since I first graduated medical school and started doing research.
Michele: We need more doctors like you. Dr. Coombs, thank you so much. I’d also like to introduce Dr. Levy, who is a hematologist oncologist at Texas Oncology. He is the director of Hematologic Malignancies Research and specializes in CLL. He’s also helped lead clinical trials in CLL. Dr. Levy, what drew you to CLL?
Dr. Yair Levy: Before moving to Texas, I actually did mostly chronic lymphocytic leukemia, but I’m a little older than Dr. Coombs. So back when I was doing it, it was still a relatively better outcome for this cancer, but we still lost some folks to chronic lymphocytic leukemia. However, if I reflect on my current experience, I don’t believe that I have lost a patient to chronic lymphocytic leukemia in the past decade. This is not because I have a shortage of patients. I’ve probably accumulated about 150. I’m not saying that the patients don’t die, but they don’t die of CLL.
So to live a normal life is the goal. Even though we still think of CLL as a treatable but incurable malignancy, for the most part, people are doing relatively well. Not to mention, not only are our treatments better in terms of efficacy, but they’re so much better tolerated.
If I reflect on my current experience, I don’t believe that I have lost a patient to chronic lymphocytic leukemia in the past decade. This is not because I have a shortage of patients. I’ve probably accumulated about 150. I’m not saying that the patients don’t die, but they don’t die of CLL.
Dr. Yair Levy
Jeff: We have an interesting topic for today’s program, Shared Treatment Decision Making: How To Be An Empowered Patient. This is something that strikes me right in my heart. I am a firm believer that patients who take an active role in their own care tend to have better outcomes, and this is actually borne out of clinical research.
I took an active role in my own care. I chose not to go in the specific direction that my first doctor wanted to go in, and I wound up at a large research hospital participating in a clinical trial. I’ve been living a great life as a result.
Changes and improvements in CLL treatment
Michele: For me, treatment decision-making also came down to becoming an empowered patient and becoming health literate in CLL. The more I could learn from credible sources, for me, was better. I realized all patients are different and doctors, you can probably relate to this more than anyone but the world has changed quickly and pretty drastically for clinicians, researchers, and those of us who are patients.
I was diagnosed 11 years ago, not quite as long ago as Jeff, but still a long time ago. My frontline treatment started in 2015 and things were even different back then. I was on a trial that combined ibrutinib, which at the time was not approved yet for frontline treatment. It had been for relapsed and refractory but not frontline treatment. It was combined with FCR, the standard at the time, fludarabine, cyclophosphamide, and rituximab. Things have changed so quickly even since then. In my frontline treatment, I’m now on a different treatment. I had relapsed in between.
Dr. Coombs, could you tell us how the landscape of treatments for patients has vastly changed over the last couple of years?
BTK Inhibitors
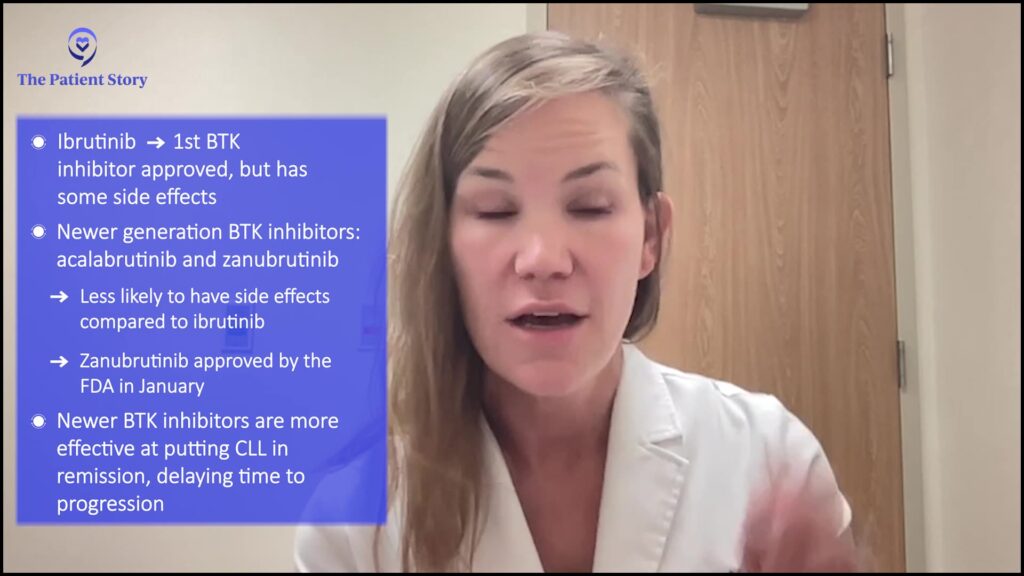
Dr. Catherine Coombs: Over the past decade, but even over the past few years, we’re seeing advances. When I first got into the field, yes, it was chemoimmunotherapy for patients fit enough to receive it like FCR and BR. With the introduction of targeted agents, largely chemoimmunotherapy is not widely used. However, we still do see about a third of uptake looking at these large-scale studies across the country.
I’d say that doctors who are focused on CLL realize that chemoimmunotherapy is not worth the toxicity. Its efficacy is also inferior to these novel drugs that are more efficacious, so more likely to put the CLL at bay, in remission, and delay time until ultimate progression, but also hugely safer. That was first ibrutinib, as you wisely know from your own personal experience and your knowledge over the time of your journey as a patient. But now we have a lot of newer and better drugs. Ibrutinib has been amazing and revolutionary, but it does have some side effects. Fortunately, they’re not so common, but they still can be clinically significant.
The first category of drugs that have really changed in the past few years is newer generation BTK inhibitors. Ibrutinib was the first in class. It inhibits this critical protein that’s part of CLL cell machinery, BTK, but it’s not totally selective for its target. We now have 2 additional drugs that inhibit BTK – acalabrutinib and the most recent addition, zanubrutinib which was FDA-approved in January.
The advantage of both of these drugs is that they’re more selective for their target, BTK. That, fortunately, has translated to improved safety, where both drugs have been compared head to head with ibrutinib and they demonstrate improved tolerability, specifically lower rates of atrial fibrillation for both drugs. Acalabrutinib also has the advantage of lower rates of hypertension.
What we don’t know is whether zanubrutinib is better than acalabrutinib or acalabrutinib is better than zanubrutinib, because we don’t have that comparison. But I think they’re both excellent options and both offer advantages over the ibrutinib days when we were dealing with a lot of atrial fibrillation. There’s a lot less in the way of that.
The other huge class of drugs that I haven’t mentioned is a completely different way of treating CLL, so I’ll mention it briefly. I don’t know if we’re going to get more into the nitty gritty on this, but these BTK inhibitors work wonderfully at controlling CLL, but they’re considered as treat-to-progression regimens, meaning that patients go on and stay on as long as they’re, number one, tolerating it and their CLL is responding favorably.
Some patients don’t like the idea of being on a drug indefinitely, so the other huge therapeutic advance over the past few years that’s been widely available is the drug venetoclax. This is typically combined with another drug called obinutuzumab when used in the frontline setting. Because it can so effectively kill off the CLL to very deep levels, patients are able to completely stop treatment after one year and then eventually relapse, but it can take a long time. That’s one of the other major, major changes in CLL just over these past 5 years or so.
I’d say that doctors who are focused on CLL realize that chemoimmunotherapy is not worth the toxicity. Its efficacy is also inferior to these novel drugs that are more efficacious, so more likely to put the CLL at bay, in remission, and delay time until ultimate progression, but also hugely safer.
Dr. Catherine Coombs
Michele: Dr. Levy, what else would you add?
Dr. Yair Levy: Dr. Coombs, you hit the nail on the head. It’s a dramatic change from chemoimmunotherapy. In the chemoimmunotherapy era, our high unmet need was what we considered high risk which were ones that harbor a 17p deletion, or a mutation in this TP53 tumor suppressor protein, or these cells of origin that are called pre-germinal cells of origin. So a more immature cell that had gone bad, and we’ve known that they have done historically quite poorly with chemoimmunotherapy.
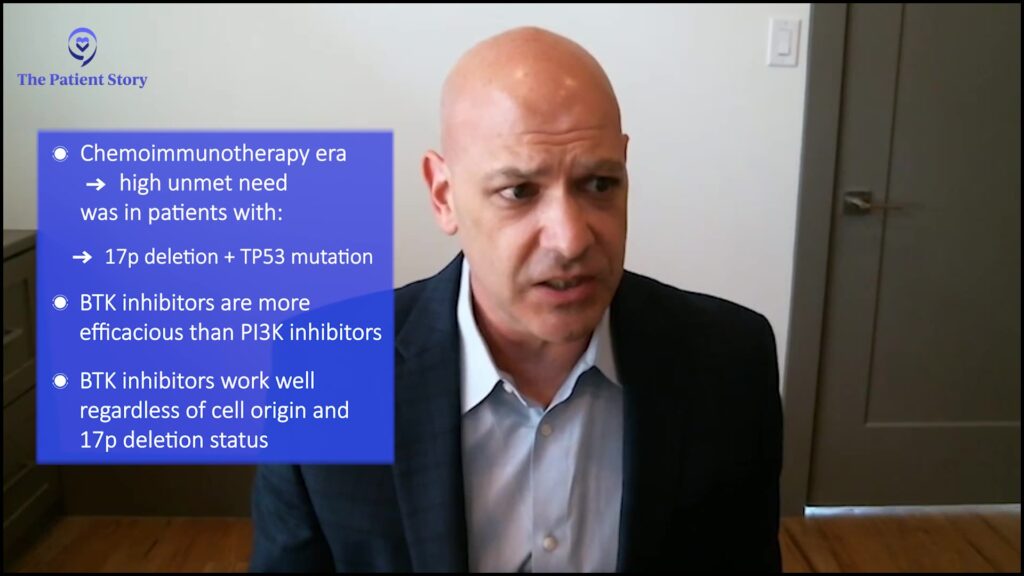
As Dr. Coombs mentioned, the biggest improvement that we saw was when we actually recognized druggable targets within the B-cell receptor pathway. The first such drugs were actually not Bruton’s tyrosine kinase (BTK) inhibitors, and they are largely relegated to the history of the B-cell receptor pathway now. But these were the PI3K delta inhibitors. Those worked irrespective of cell of origin, and they also worked in the 17p deletion. So again, they did certainly have some tolerability issues and the efficacy was not comparable to those of Bruton’s tyrosine kinase inhibitors, which is one of the big reasons that those have really fallen out of favor.
As Dr. Coombs mentioned, the BCL2 inhibitor venetoclax has also been a game changer. We’ve been utilizing these agents, either alone or in combination with CD20 monoclonal antibodies. Now, the European Medical Association has even approved the combination of a BCL2 and a BTKi. This is something that we’re doing further studies on within the United States as well because we’re seeing that people achieve very impressively high rates of response. More importantly, very deep responses can allow, hopefully, a very long treatment-free interval, and perhaps even in some cases, a functional cure.
So, in the beginning, we were saying that CLL is largely treatable but incurable, but we put an asterisk on that. Even with chemoimmunotherapy, there was a subset of CLL that may have been cured by chemoimmunotherapy, or at least a functional cure. I think we’re going to see the same thing with these other combinations as well.
We’re seeing that people achieve very impressively high rates of response. More importantly, very deep responses that can allow, hopefully, a very long treatment-free interval, and perhaps even in some cases, a functional cure.
Dr. Yair Levy
How CLL doctors are providing CLL patients with precision care
Jeff: This is exciting stuff. We’re talking about an awful lot of options for patients, but before we can get to those options, we need to figure out how we get to that point. So let’s chat a little bit about the tests that are needed to diagnose and then accurately inform those potential treatments.
A lot of us in the support groups and on social media love tossing around the cute names, the FISH test, the flow test. Not a lot of people truly understand what’s going on with those tests. They don’t understand the concept of chromosomal abnormalities that may be going on with a patient at the time of diagnosis. Dr. Coombs, can you briefly give us a top line as to what these tests are doing and more importantly, what they’re telling you in terms of prognostics?
Dr. Catherine Coombs: Absolutely. Before the advent of all these, let’s call them sophisticated tests, we would stage patients. That’s always what I think cancer patients think of, what stage am I? We do have a staging system called the Rai Staging System that we use in the US. In Europe, they use this Binet Staging System. But the idea is, how much is this really affecting me? Rai stage 0 is when it’s just a high white count to Rai stage 4 when you have low platelets from the CLL.
I’m taking a step back because there were, for decades, ways of saying this a good or a bad CLL. However, what we’ve learned over the years is that there are some patients with really early-stage disease that would follow very aggressive clinical courses and then some that may have been technically a Rai stage 4 that were totally stable for decades. The goal with all these more sophisticated tests was to better predict, how is this person’s CLL going to behave, which then helps us as clinicians know what to expect. It helps the patient as far as what he or she should expect.
So taking a step back, we now have a lot of advanced testing that we can send. The good news is that these can be sent on the peripheral blood so it’s not necessary to get a bone marrow biopsy early on. Of course, we do consider these at the time of therapy, but we can send these tests in the blood because the CLL, by its nature, is circulating in the blood. So we can pick up different abnormalities that can tell us, this is a good or a bad CLL or maybe somewhere in the middle to help us, number one, know if we should follow this person more closely. Number two, is this someone that perhaps it’s less likely to cause more trouble than not?
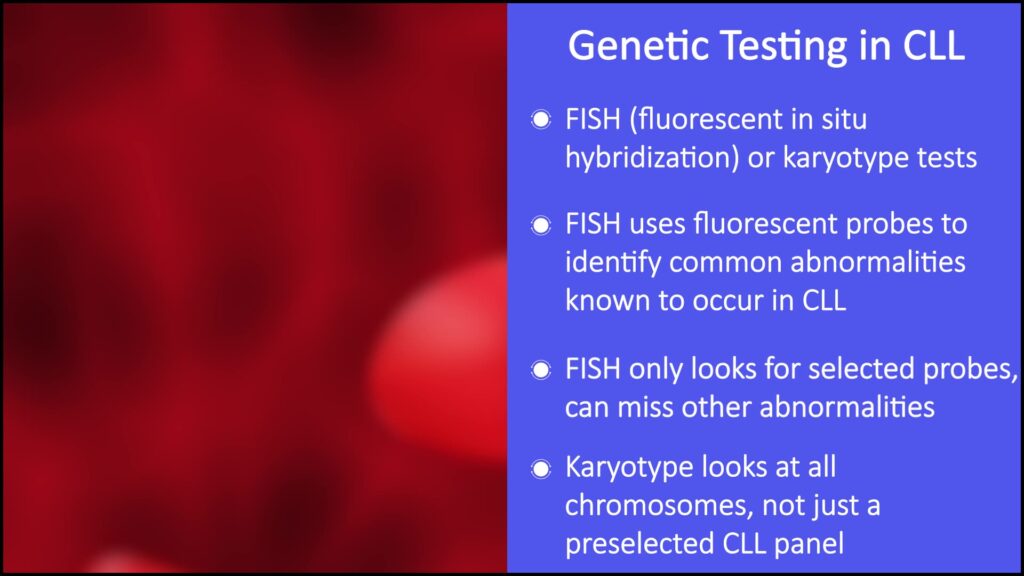
The categories of tests are looking at the DNA, which is either via a FISH test which uses fluorescent probes to find common abnormalities that are known to be seen in CLL. The most adverse is the 17p deletion. On the other spectrum, the most favorable is an isolated 13a deletion.
However, what we’ve learned is that this is only looking at certain probes. Sometimes you can have other abnormalities that aren’t present as part of the FISH panel. In my own practice, I also send a karyotype test which looks for the same thing, abnormal chromosomes. Instead of using a preselected panel of common abnormalities in CLL, it just looks at all the chromosomes. The chromosomes, just for the patient’s knowledge, are just the big chunks of DNA that live inside every one of our cells. We’re focusing on what these abnormalities are in the cells because there are common patterns. There are good patterns and bad patterns.
It’s also bad to have a complex karyotype, meaning 3 or more abnormalities in any given cell, so that’s one category. The 17p deletion I mentioned is known to behave more aggressively. It’s still a chronic disease, but those are often the bad actors, especially back in the chemo days when chemo doesn’t work well at all. It does do better with our new drugs, but that is a particular problem because it deletes a copy of this very important gene called TP53.
We used to think the only way of losing that gene was by completely deleting the part of the chromosome where it’s contained. What has been learned over the past 10 to 15 years now in CLL, is that it may not be deleted, but it could be mutated. That’s another test that I think is very wise to send, especially in patients who are going to need treatment because a TP53 mutation is largely the same as a 17p deletion. There are a little bit of nuances there, but these are 2 separate tests. They both give similar information because those 2 abnormalities are treated as one and the same as far as their impact on prognosis.
The next category of testing is looking at the immunoglobulin heavy chain status, so a normal B-cell over its life. CLL is a cancer of B-cells that undergoes a process of somatic hypermutation where it just acquires mutations. It’s actually good to have a mutated, immunoglobulin-heavy chain. The bad finding is for that to be unmutated, which suggests this is a bit more primitive of a cell. And what’s been borne out through a lot of studies is that patients with unmutated are the ones who need therapy quicker and they don’t respond as well to certain therapies. Now, again, the negative predictive impact of some of these abnormalities is somewhat outdated. Sometimes they do just as well with our new treatments, but they definitely don’t do as well with the old treatments.
The other test I always send is the beta-2 microglobulin (B2M), mainly because that goes into our scoring system for CLL, the CLL International Prognostic Index, but it’s an adverse finding to have that elevated. I think that wraps up the bulk of all the prognostic tests that I send at the time of meeting a new patient and trying to help understand what is our future going to be like.
The goal with all these more sophisticated tests was to better predict, how is this person’s CLL going to behave, which then helps us as clinicians know what to expect. It helps the patient as far as what he or she should expect.
Dr. Catherine Coombs
Jeff: Let me play that back for just a second and put it in terms that are not quite so technical. You have a toolbox, and that toolbox has a lot of really nifty tools in it, where instead of saying you have leukemia or you have chronic lymphocytic leukemia or you have one of these genetic abnormalities, you’re able to hone down to a very precise level of differentiation. That’s where the term personal and precision care comes in. Correct?
Dr. Catherine Coombs: Excellent explanation. Yes.
Michele-Nadeem Baker: I love this term and how that is happening more and more for patients. Dr. Levy, before planning treatment, what do you like to understand from your patients so that you can learn more about them when it comes to prescribing their treatment?
We need to speak with the patient and find out what is most important to them and explain everything about the treatment, including side effects, logistics, expected outcomes if you choose one route versus another, and the cost of travel. There are a lot of things that go into everything.
Dr. Yair Levy
Dr. Yair Levy: We’re all different and everybody’s cancer is also different. The reason that we have jobs as oncologists is because, I’m not sure that’s true here, but hopefully we know more about CLL and the treatment options than the patients. It’s our job to explain to them all their various options and then help them arrive at a choice that makes the most sense for them.
I think Dr. Coombs mentioned that we have a lot of options, but they haven’t necessarily been compared head to head. So we can’t tell you prospectively how treatment A compares to treatment B or treatment C. There are certain guidelines of what’s called preferred therapies and other alternative therapies that are also acceptable. We need to speak with the patient and find out what is most important to them and explain everything about the treatment, including side effects, logistics, expected outcomes if you choose one route versus another, and the cost of travel. There are a lot of things that go into everything. This is our job to get them to ask the right questions and then answer those questions.
The role of patient comorbidities in CLL care
Michele: And what about comorbidities? Is it important for patients to discuss their other health issues with you, such as cardiac issues? There’s a myriad of so many other types.
Dr. Yair Levy: Absolutely. This is what we were saying is, we’re all different, we all have different things that matter, and we are all in a different place in our lives. We take all of that into consideration, there’s no question about it.
The comorbidities are incredibly important, but we certainly advanced past where we were 15 or 20 years ago when we were looking at whether patients are fit enough to take therapy versus not because right now we’re not necessarily looking at fitness for therapy as much as we’re looking at what is the optimal therapy for them.
Many of the therapies that we have, if you take a look at what’s called the Preferred Category 1 recommendations from the NCCN Panel, were all studied in what we would have technically called a non-fit population before. It’s wonderful that we have all these highly effective therapies that we can give to people, even if their fitness is not optimal.
The benefits of watch and wait

Jeff: We’ve been talking about a whole bunch of novel therapies, stuff that has really impressive outcomes these days. Michele and I will both be able to tell you without hesitation, that the first thing that most patients encounter is not treatment. It’s this thing that we call watch and worry. You guys call it watch and wait. CLL does not always need to be treated right away. Your medical team is going to work with you to decide when it’s best to start treatment. In the meantime, the patient’s worry. Did I sum that up correctly, Michele?
Michele: We sure do, even though we tell everyone not to and to take a breath when they’re first diagnosed. Jeff, you and I both know that we still go through that when we’re back in that time period. It’s just so counterintuitive to not be treated right away when the disease has not progressed where it ends up going when you do get treated.
Dr. Coombs, what are you looking for when it’s time to treat? You go through years, hopefully, during watch and wait. Worry and wait, as patients call it. But what is it that you’re looking for and is there any benefit to treating it sooner as with some of the other cancers out there?
Dr. Catherine Coombs: I’m coming straight from my clinic. I’m in a clinic room. I just had this conversation with a patient who is newly diagnosed about watchful waiting, which I totally understand why it’s watchful worrying for many. I always see it as my duty to help them understand why this is our approach. I acknowledge this is not what we do for many other cancers where you hear, find it early, treat it early. I wish our treatments were so good that treating it early would knock it out and you’d never have to worry about it again. In 2023, we haven’t been smart enough to come up with something that will do that for CLL.
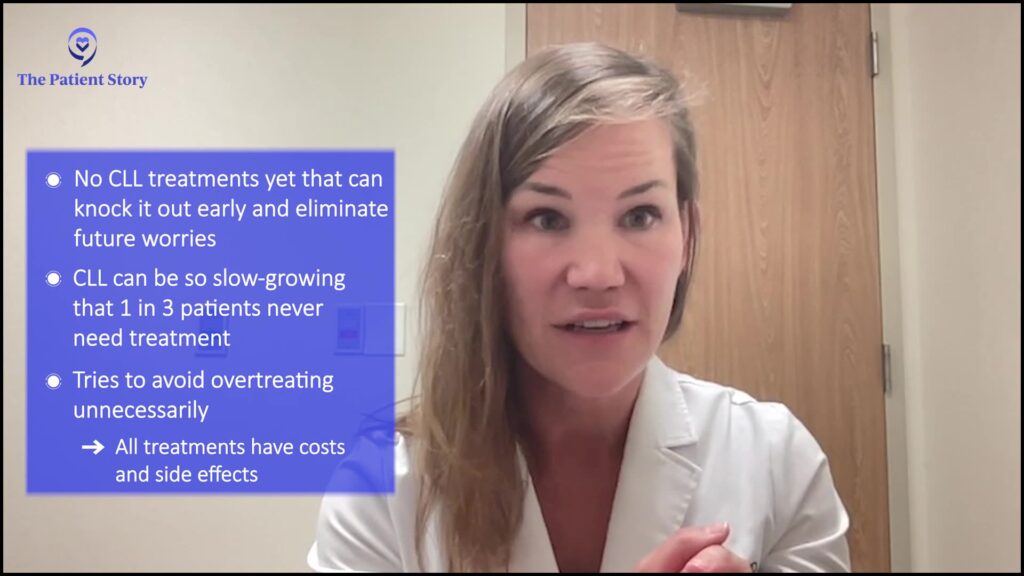
The way that I help put that in context for my patients is this disease can be so indolent that maybe up to 1 in 3 patients never need treatment in their lifetime. So if we treated everyone, inherently we’re over-treating people. I hate giving people things they don’t need because every treatment comes with a cost, whether it’s financial or side effects. That’s my one very strong argument for not over-treating. But also, none of the early treatments that we have tried and done clinical trials on have been shown to make patients live any longer. That is just where we are.
I definitely could understand the frustration on the part of patients because that leaves you with these worries. I do see those getting better in patients as time goes on. There’s this initial period of uncertainty, but then as you see what your pattern is, that either tells us, maybe we are approaching the time for therapy or nothing’s really changing, I feel fine, and this is something I can accept.
Now, obviously, we never know which camp a patient is going to fall into in these prognostic tests. They help us have a general sense of, maybe this will be a super slow CLL versus one that progresses more rapidly, but nothing is certain. I do personally have enthusiasm for making this change.
There is an ongoing countrywide clinical trial looking at early intervention for patients with high risk. That is open at my own institution and across many, many institutions in the country. I really hope things will change so we can improve patients with early disease. I don’t think it’s going to be every patient because of this third that never needs treatment. I don’t ever see a reason to just treat everyone, but the trial specifically is focusing on high-risk patients. Maybe there will be some movement there. It’ll probably take about 10 years to find the results of the study because you have to follow patients for a really long time.
For now, my job is to not over-treat and not make people who are feeling good feel worse. If you’re asymptomatic, then the best I can do is leave you alone, but hopefully calm some of whatever natural anxieties come about with what is a life-changing diagnosis.
This disease can be so indolent that maybe up to 1 in 3 patients never need treatment in their lifetime. So if we treated everyone, inherently we’re over-treating people.
Dr. Catherine Coombs
Michele: We have some questions coming in from our audience. Dr. Levy, here’s one of the questions for those of us with liver enlargement. Should we watch and wait?
Dr. Yair Levy: I completely understand the anxiety that comes along with this. I’ve been treating indolent lymphomas for a couple of decades now, and I’ve got the same experience. You talk with patients, you tell them they have cancer, and then they’re saying, “You tell me I have cancer, but you’re not going to treat me now. Are you sure you went to medical school?” I had that come up several times.
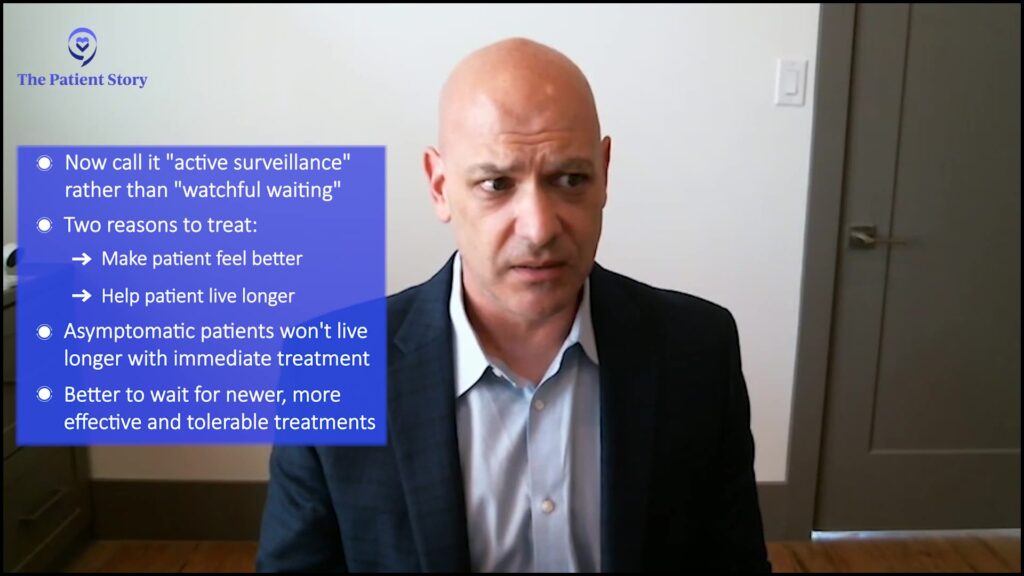
By the way, we don’t do watchful waiting anymore. We call it active surveillance. Nobody likes watchful waiting, but if we’re saying we’re actively surveilling you, that sounds certainly a lot better.
The way that I explain it is, that there are really only two good reasons to treat you for anything. This isn’t just an oncologist, it’s in all of medicine. My wife is a real doctor, she’s an internist. She has the same parameters for treatment. So, number one, if you can make somebody feel better, that’s absolutely a great reason to treat them. Number two, if you can make them live longer.
What we’ve seen, as Dr. Coombs was saying in chronic lymphocytic leukemia, as well as a variety of other indolent non-Hodgkin’s lymphomas is that early treatment does not confer a benefit in survival. In other words, if we treat you when you’re asymptomatic, you’re not going to live any longer than if we wait to treat you when you are symptomatic. This is important because as we were talking before, our treatments are changing and changing for the better.
The treatments are becoming more effective and better tolerated. And remember, something is only incurable until we’re able to cure it. So there are a lot of good reasons to wait. Dr. Coombs mentioned this as well. If I can’t make you live longer by treating you earlier with our current therapeutics, the question is, can I make you feel better? If you’re asymptomatic, I can’t make you feel better. I can make you feel worse. I can spend a lot of your money, but I’m not helping you. You are the most important part of that equation.
If somebody has liver enlargement, the question is, are they symptomatic? Are they having pain? Are they having any other symptoms from their liver involvement? If they’re asymptomatic, I would not necessarily treat them just for liver enlargement. The same thing is true with spleen enlargement as well, which is a far more common finding in chronic lymphocytic leukemia.
If we treat you when you’re asymptomatic, you’re not going to live any longer than if we wait to treat you when you are symptomatic.
Dr. Yair Levy
Michele: I experienced that when I relapsed, but along with other things as well, which led to my going back into treatment. Dr. Levy, thank you. You brought up a lot of great reasons why people are not rushed into treatment which also hints at all the things that you do look at when it is time for treatment, which we’ll continue to talk about as we go through with our program today. Thank you very much.
Considering the duration of treatment for CLL patients
Jeff: We spoke earlier about a bunch of the newer options that are available. We know that the treatment landscape is changing by the minute. I’m going to tee this up in terms that forum participants and our support group participants, they all had the same questions.
Yeah, the drugs are great. Am I going to have to take them for the rest of my life, or is there a chance that I can do it for a fixed duration? Dr. Levy, let’s break down what those current treatments are, what baskets they fall into and is this a lifetime activity or could we end it in 6 months? Could we end it in one year? You’ve got a lot of stuff that ends in -ibs, and -tas, and -mabs, and all that. Explain to us what’s going on.
Dr. Yair Levy: Again, this treatment progression model is a relatively new phenomenon for us in the treatment of malignancies. We used to treat with a fixed duration of therapy when all we had was chemoimmunotherapy. You can understand why. Once we give chemo, we can’t take it back. Certainly, the effects of cytotoxic chemotherapy are not something that you want in a cumulative manner.
Because of the logistics of how cytotoxic chemotherapy works, we could not give that till progression because that would be a very difficult life. Everybody thinks that the worst thing in the world is dying, and no, the worst thing in the world is not dying. The worst thing is a long, crappy life. That’s what we would assure we would do to people if we continued them on chemoimmunotherapy.

If you take a look at our approved therapies right now, basically it’s two categories. Bruton’s tyrosine kinase inhibition, BCL2 inhibitors, and monoclonal antibodies, can be sprinkled on any of these regimens. In terms of approved fixed durations of therapy, it’s only with the BCL2 inhibitors. The reason for that is that’s the most ideal drug that we have seen in the treatment of chronic lymphocytic leukemia. What I mean by that is it is a killing machine. It kills so well that we had to attenuate the dose because if you kill things too quickly, that can also become a problem.
We’re able to get those very, very deep responses. These deep responses, even if they’re what’s called MRD, which stands for minimal residual disease, really should be measurable residual disease. Even if people achieve a level of disease below where we can measure it, we know that in many cases it still returns. We really need to get that logarithmic killing. We really need to reduce their tumor burden by many zeroes in order to give them that long treatment-free interval. Currently, that’s possibly more likely with a BCL2 inhibitor venetoclax.
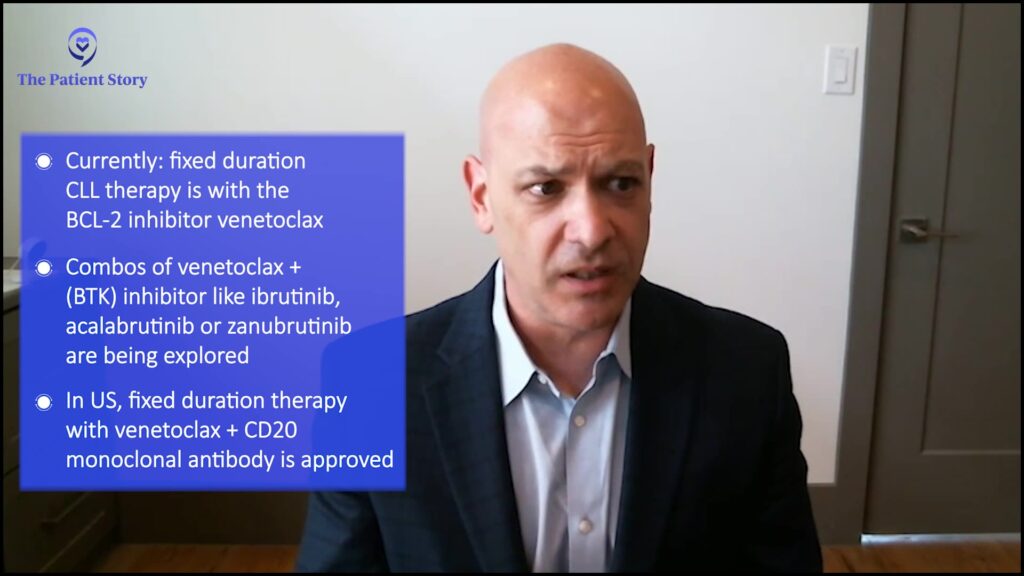
As we were alluding to before, we are seeing combinations of Bruton’s tyrosine kinase inhibitors like ibrutinib, acalabrutinib, or zanubrutinib in combination with venetoclax. Again, this was based on these laboratory models in which they actually saw whether or not these cells were primed for death with this combination. They actually saw synergy, meaning that the drugs worked better together than the sum of their parts.
As we mentioned, this is a fixed duration of therapy that’s actually approved in Europe right now, but not here in the United States. In the United States, we certainly can give a fixed duration of therapy with venetoclax and a CD20 monoclonal antibody. I can tell you that anecdotally, I’ve also done that with Bruton’s tyrosine kinase inhibitor and a monoclonal antibody if I can achieve that very deep response.
In terms of approved fixed durations of therapy, it’s only with the BCL2 inhibitors. The reason for that is that’s the most cidal drug that we have seen in the treatment of chronic lymphocytic leukemia.
Dr. Yair Levy
Factors in choosing a first-line treatment for CLL
Jeff: Excellent. Lonnie’s got a great question. Since we’re now considering treatments, he wants to know what are the primary factors to consider in choosing a first-line treatment. Dr. Coombs How do doctors and patients make that call? How do you choose which drugs are up on deck first?
Dr. Catherine Coombs: I think there are disease-related factors and patient-specific factors. We tackle those one at a time. I think there is an important role in knowing what an individual’s CLL risk findings are because those can help inform how likely a treatment is to lead to prolonged remission. Specific to a venetoclax-based approach in the front line, what we do know is that there are shorter remissions in patients with the 17p deletion or TP53 mutation and also shorter remissions for individuals with unmutated IGHV.
I tend to be an optimist and so my view is that these therapies, venetoclax-based, work way better than chemotherapy ever did for patients with these high-risk features. We can still see lengthy remissions on the order of a little over 4 years for the 17p patients for progression-free survival or around 5 some years for the unmutated IGHV. That is shorter than if you don’t have those markers.
I do think it helps weigh expectations on what to expect from a time-limited regimen. If you have high-risk markers, if you have all favorable markers, venetoclax also works really well and it just works longer than if you had negative markers.
Now, Bruton’s tyrosine kinase inhibitors as a class that have really leveled the playing field. If we divvy up patients with the unmutated and the mutated IGHV and the chemo days, the unmutated would relapse years faster than the mutated. There’s not much of a difference, and so those drugs work really for everyone. Now, they’re just so different conceptually and side effect-wise, which is why it is so important to weigh the patient’s comorbidities.
In addition to these disease-related factors that could help gauge the relative success of any given therapeutic approach, there are patient-specific factors. That’s why it’s so important for me to know, not only the details of the CLL but also the details of your specific comorbidities. Do you have a high degree of cardiac comorbidities where maybe we might be a little bit nervous about the BTK inhibitors, which can have cardiac side effects?
I will say the newer drugs are much better than ibrutinib, but it is something I weigh whether you have significant kidney disease, which might be a little bit risky. When we think of a drug like venetoclax that causes tumor lysis syndrome – none of these are complete no-goes, but they help tip the scale of which one are we favoring a bit more.
Then, of course, I want to know what other medications you’re taking, because a lot of medications can interact. That’s something we have to make sure of. Often that’s not a big deal, we just switch one out, but we have to know.
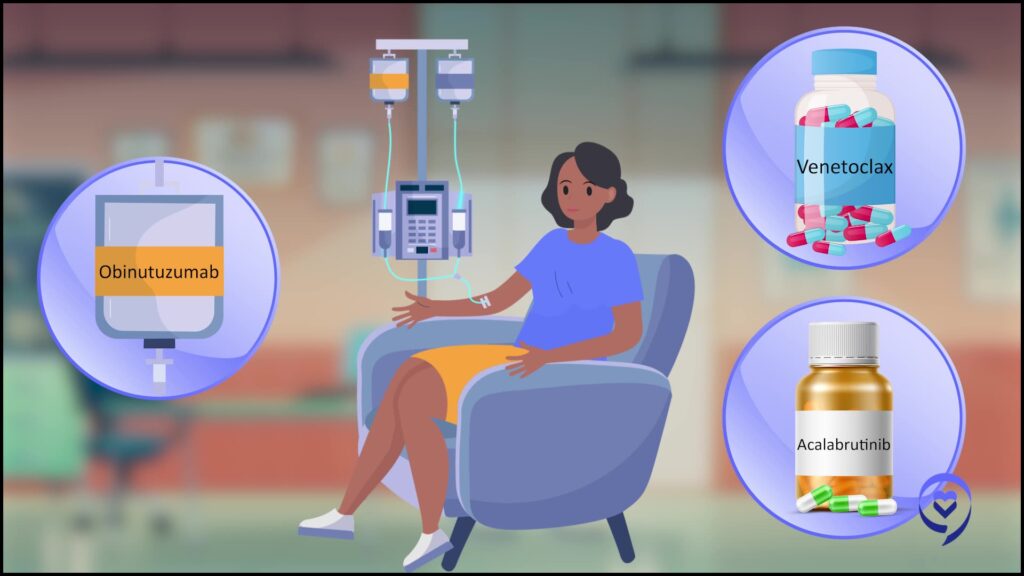
Lastly is social factors. What are your preferences? Are you the type of person who wants to do everything and doesn’t mind a frequent schedule, but wants that payoff of then being done with treatment in a year, where we might lean more towards venetoclax-obinutuzumab? Or are you someone who wants to spend as little time at a doctor’s office as possible and is okay with indefinite treatment where we may lean more towards BTKi? Those are the 3 major categories I think of – disease factors, patient comorbidity, specific factors, and then social and preference.
My view is that these therapies, venetoclax-based, work way better than chemotherapy ever did for patients with these high-risk features.
Dr. Catherine Coombs
The benefits of monoclonal antibodies for some CLL patients
Michele: Dr. Coombs, thank you for talking about the biomarkers that might indicate someone is a high risk, such as 17p or TP53. I am high-risk, but I don’t have either of those. I have the other that you had discussed being unmutated IGHV, and that actually impacted my treatment decision when I relapsed. I just finished. I am on acalabrutinib and was on a blinatumomab until a couple of weeks ago. It was obinutuzumab for 6 months along with the acalabrutinib.
Now, I will be staying on acalabrutinib indefinitely because I am considered high-risk. I had originally stated before that I started on ibrutinib. BTK inhibitors work for me and I just had adverse events initially and that’s why I went off. I had a couple of years of a drug holiday and then my doctor decided that while BTK inhibitors were still working, let’s go for it. I would still have another option with venetoclax.
Dr. Levy, why does a monoclonal antibody help? What does it add to the one-two punch? I know you talked about the different things that they’re addressing and being a killing machine, but why is it only for some patients? For example, what I’m on, acalabrutinib and obinutuzumab trials have shown that it specifically works the best. One trial was presented at ASH this past year for people like me who were unmutated. So, why only for some patients is it a benefit?
Dr. Yair Levy: Well, that’s a great question. The CD20 monoclonals were our first immunotherapy in the treatment of many B-cell malignancies. When we combined them with some of the targeted therapies, we didn’t necessarily see what we were expecting. In all of the trials with chemoimmunotherapy, adding a CD20 monoclonal improved progression-free survival. But interestingly, when we took a look at some of the studies that had arms that contained both ibrutinib, our first, covalent Bruton’s tyrosine kinase inhibitor in combination with a CD20 monoclonal or without those progression-free survival curves were superimposable. I think we were really surprised by that.
By the way, I need a button that says “I agree with Dr. Coombs.” Dr. Coombs was actually mentioning the fact that there are differences among these covalent Bruton’s tyrosine kinase inhibitors, and our first one had a less focused kinase profile. In other words, it hit other kinases, not just Bruton’s tyrosine kinase that we were trying to inhibit. One of the other kinases that it inhibited was something called ITK or IL-2-inducible tyrosine kinase. This led to antagonism of the CD20 monoclonal, which is why we got no benefit from the addition of the CD20 monoclonal.
This is not true for the other covalent BTKi, zanubrutinib and acalabrutinib. However, you’re seeing the combination with acala because that is FDA-approved and zanubrutinib does not have an FDA label in combination with a CD20 monoclonal. Do I have any reason to think that it wouldn’t work as well? I do not. There’s certainly data that supports that as well, that there are differences in terms of PFS for folks receiving the combination of zanubrutinib with a CD20 as well as without.
Now you can say, so why doesn’t everybody get a CD20 monoclonal? The answer is that there are trade-offs. Everything in life is a risk-benefit ratio. We know that, for example, there is this virus here in Texas, I don’t know if you guys have it too, called COVID. We know that for COVID, the CD20 monoclonal certainly antagonized an immune response to vaccination, as do the BCL2s and Bruton’s tyrosine kinase inhibitors.
Certainly, you are at more risk for adverse events and complications when you add additional drugs, so everything is a trade-off. We’re getting additional efficacy but at a cost. Our job is not to tell patients what to do. Our job is to have a discussion and come up with a solution that works best for them after we have a discussion and they are fully informed.
Now you can say, so why doesn’t everybody get a CD20 monoclonal? The answer is that there are trade-offs. Everything in life is a risk-benefit ratio.
Dr. Yair Levy
What CLL doctors consider before ramping up treatment and dosing
Michele: Thank you. Dr. Coombs, let’s talk about ramping up treatment. When you start treatments such as with venetoclax or even obinutuzumab, you start with smaller amounts and then ramp up to full dosing. Why is that?
Dr. Catherine Coombs: It’s different based on the drug. Let’s tackle obinutuzumab first. Obinutuzumab is the monoclonal antibody that can be paired with either venetoclax or acalabrutinib. It can also be used by itself less often. It’s a hugely effective drug, and it doesn’t really have that many side effects except for one that’s almost universal, which is these infusion-related reactions. Of course, it has other side effects such as impaired vaccine efficacy infections. It can cause low blood counts, but the one that’s universal is infusion-related reactions.
Instead of just giving patients their full dose of 400 mg daily, we…slowly introduce it so we’re more slowly killing off the cells in a way that’s friendly to the kidney and friendly to the rest of the body to minimize any potential risks from all this dead cancer cell debris.
Dr. Catherine Coombs
What they’ve learned over the course of developing this drug in clinical trials is that, instead of blasting patients with the full dose on the first day, the reaction seemed to be more manageable if you split the dose. The traditional way of administering obinutuzumab, the full dose is 1000 mg.
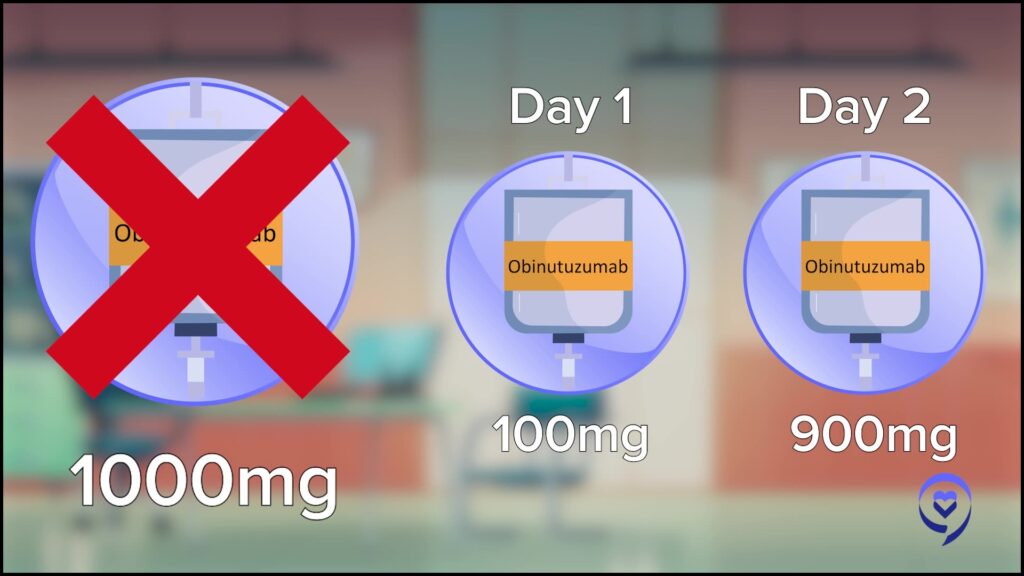
Instead of doing that all at once, which would make for a very colorful reaction in the infusion suite that no one nurse nor patient wants to be involved with is giving 100 mg on day one and then the other 900 mg on day two. Then of course you follow along with the rest of the schedule. The reactions, fortunately, are almost always on the first 1 or 2 days and then not long-lasting except for rare exceptions. That’s the reason for ramping up obinutuzumab, to make the reactions more manageable.
Venetoclax is a different story. As Dr. Levy mentioned, this drug is remarkably effective at annihilating CLL cells. But it’s not a good idea to kill any cancer just too quickly, because when you kill a cancer cell, all this dead cancer cell debris gets released into our bloodstream and our kidneys can’t handle that, even the best kidney in the world.
Instead of killing cancer rapidly by administering the full dose, it’s been learned through very well thought out and designed clinical trials that patients tolerate it better with less chance for dangerous tumor lysis syndrome, which is the term for complications from cancer dying too quickly, is to ramp it up. Instead of just giving patients their full dose of 400 mg daily, we give them a little whiff of venetoclax in week one, 20 mg, a little whiff the next week, 50 mg, and slowly introduce it so we’re more slowly killing off the cells in a way that’s friendly to the kidney and friendly to the rest of the body to minimize any potential risks from all this dead cancer cell debris.
Considering the side effects of CLL treatments
Jeff: Dr. Levy, I love the fact that you used the term risk management because that’s pretty much how I approached my entire journey, with risk management. We know that for most people there are going to be some side effects. There’s going to be some challenges when they start treatment. Can you give us a minute on, are they all going to happen upfront? And how do you manage them?
Dr. Yair Levy: That’s a great question. As Dr. Coombs mentioned, for the CD20 monoclonals, most of the reactions occur early and typically improve as you receive more of the drug. This is also true for the oral medications that we have. Most of the side effects, if you look at what’s called adjusted incidence, meaning how likely is it to happen per amount of time, it’s more likely to happen in the beginning. However, as we talked about, some of these therapies are indefinite progression or intolerance.
If you take a look at the cumulative incidence of events that continue to go up, there are certainly some events that are much more difficult to come back from. One that we worry about in particular is what’s called ventricular tachyarrhythmias, so getting a funny heart rhythm can actually lead to sudden death. It’s tough to come back from sudden death, isn’t it? One person’s done it right. They wrote a book about Him. One Person came back from the dead. A very popular book, but nobody else has done it since so we want to make sure that we give patients the safest possible therapeutics that we can.
Reasons to switch a CLL patient’s inhibitor
Jeff: Sometimes patients are told that they need to switch out their BTK inhibitor. There are a lot of reasons why this could be done. Dr. Coombs, can you tell us what’s going on with this?
Dr. Catherine Coombs: That is a common question, and that’s something that’s evolved over the years from having one option, just ibrutinib, to now having multiple options. In my own practice, I actually have switched patients for a number of reasons. I would say the reason that I consider switching a patient off of a BTK inhibitor to a different BTK inhibitor is if they’re having some side effect that’s negatively impacting their quality of life. I have switched patients from ibrutinib to acalabrutinib with very good success. I’ve also switched patients from ibrutinib to zanubrutinib, and I’ve even switched patients from acalabrutinib to zanubrutinib.
There have been studies looking at switching for side effects. About 70% of the time, the patients have improved tolerability on one of the newer drugs. There have been studies looking at switching to both acalabrutinib from ibrutinib and then switching to zanubrutinib from both ibrutinib and acalabrutinib and it seems to be a pretty uniform result where more often than not, the newer drugs are better tolerated than our oldest drug, specifically ibrutinib. I think that’s a very valid reason to switch.
The education point is, I would not switch in the setting of progression. That just is not a strategy that works more than a month or two and it isn’t really worth it. If you’re progressing on a BTK inhibitor of these FDA-approved ones, again, not speaking to switching from any of the approved ones, ibrutinib, acalabrutinib, or zanubrutinib, that is not recommended.
Now, I’ve heard of some occasional doctors just switching everyone off of ibrutinib. I’d say I talk to a lot of the community. I think most of us don’t do that because the side effects that occur most of the time are early on. I don’t use ibrutinib for my new starts, but I definitely have patients in my clinic who have been on it for years and they’re doing well. The old expression is if it ain’t broke, don’t fix it. Some people think, well, let’s just switch everyone. I don’t think that’s wrong, but it’s just not something that I’ve done for the reason I mentioned.
Jeff: Thank you for that. Makes complete sense.
I would not switch in the setting of progression. That just is not a strategy that works more than a month or two and it isn’t really worth it.
Dr. Catherine Coombs
New CLL treatments awaiting FDA approval

Michele: Doctors, there are so many types of treatment and clinical trials. Dr. Coombs, which ones are you most excited about that are getting closer to FDA approval?
Dr. Catherine Coombs: There are two that I’m going to mention. I’m excited about a lot of things, but the ones that I think are the closest to being approved potentially, I have no window into when the FDA actually approves things. One is a drug called pirtobrutinib. This is a drug that inhibits the same target as ibrutinib, acalabrutinib, zanubrutinib, and BTK, but instead of inhibiting it irreversibly, it is a reversible inhibitor.
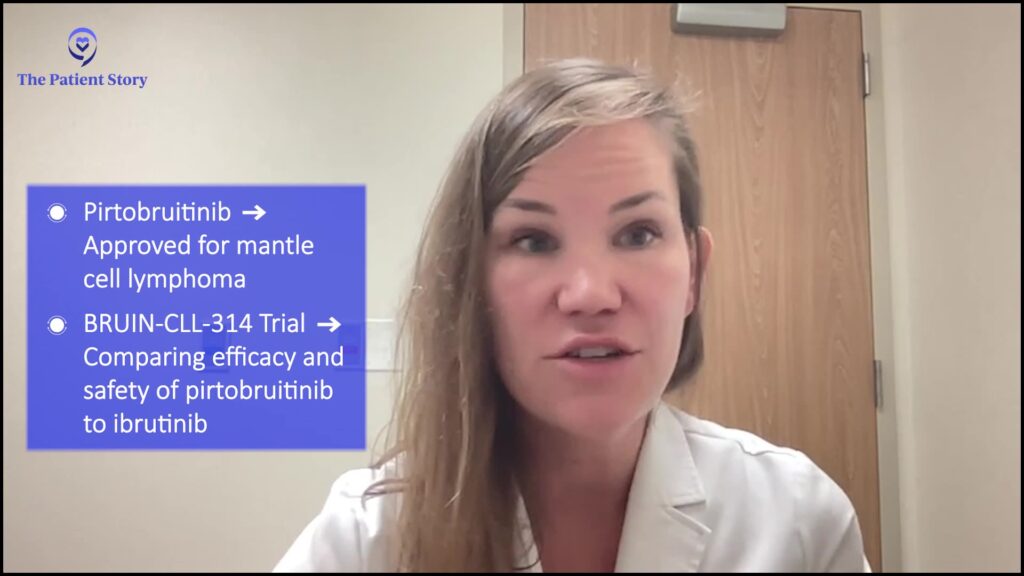
The reason that that’s important is that when patients develop resistance to ibrutinib, acalabrutinib, and zanubrutinib, the resistance is shared by all of these drugs. So you can’t switch from acalabrutinib to zanubrutinib or ibrutinib to zanubrutinib, etc., if your patient is resistant because they develop most commonly mutations where the drugs bind. Pirtobrutinib binds at a different mechanism. It’s in a different part of the BTK molecule protein and it has shown very excellent efficacy in a very large study. I do think that that may attain FDA approval for CLL in the coming days.
It’s already FDA-approved for mantle cell lymphoma as of January, so there are ways to get it off-label, but I would much rather see it get full FDA approval to help with insurance paying for the drug when it’s needed. It fills a huge unmet need for patients who have progressed on covalent BTKis, especially after patients who have progressed following venetoclax where we don’t really have good options.
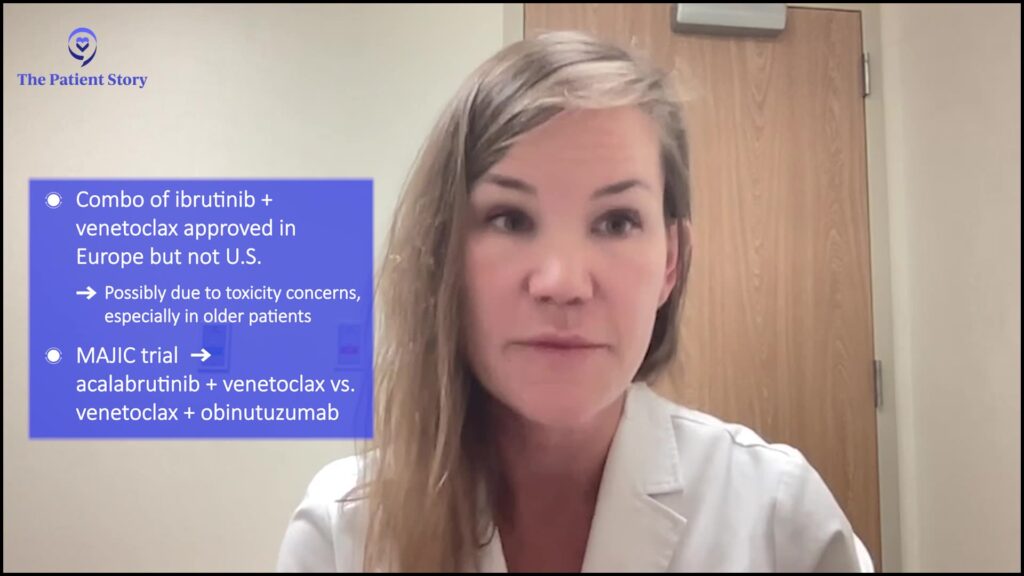
The other big category that Dr. Levy has alluded to is the combination of a BTKi plus venetoclax. Europe approved the combination of ibrutinib with venetoclax, which did not get approved in the United States. I can’t really speak about the reasons because I’m not involved with those discussions. I do wonder if some of it may be the toxicity of that regimen, which can be somewhat hard to tolerate, especially for older adults.
But what we know is that we have better BTK inhibitors with respect to tolerability. So there are a couple of trials that are looking at the combination of acalabrutinib and venetoclax that I do think hopefully will be positive trials that lead to FDA approval. That’s the other major category that I’m looking forward to. Those would be frontline treatment. You would use that combination as your first treatment. Whereas pirtobrutinib, if it gets approved, would be a relapsed treatment, at least for now. Things obviously change as time goes on.
It fills a huge unmet need for patients who have progressed on covalent BTKis, especially after patients who have progressed following venetoclax where we don’t really have good options.
Dr. Catherine Coombs
Michele: So your top two are pirtobrutinib and the combination of–.
Dr. Catherine Coombs: A BTKi plus venetoclax.
Michele-Nadeem Baker: Dr. Levy?
Dr. Yair Levy: I agree once again. There are other small molecule inhibitors, again, targeting that B-cell receptor pathway, which has really revolutionized the way that we treat a lot of these B-cell NHLs. In addition, the bispecifics, are certainly working their way into our armamentarium for non-Hodgkin’s lymphomas as well as CAR Ts.
Interestingly, one of the first articles that came out about CAR T was in chronic lymphocytic leukemia, despite the fact that our current constructs, these current autologous derived products are certainly not showing the same level of efficacy in chronic lymphocytic leukemia as they are in diffuse large B-cell lymphoma, for example. Nevertheless, I think that we are going to see some tremendous improvements in terms of the CAR Ts in chronic lymphocytic leukemia as well as the Bispecifics.
CLL doctors’ top takeaways
Jeff: So, Dr. Levy, I’m going to put you on the spot. What is the number one takeaway that patients should be grabbing from this discussion that we’re having today? What’s the top of the list?
Dr. Yair Levy: We’re doing so much better. As I mentioned at the beginning of the conversation, I have not had a patient die of CLL in the past decade. When we take a look at the high unmet need and again, Dr. Coombs was alluding to that. Folks who have progressed on a Bruton’s tyrosine kinase inhibitor and a BCL2 inhibitor are certainly the unmet need. We have a tough time finding those folks.
We’ve had some studies that have been languishing for accrual because it required folks to become double refractory. Again, we have a tough time finding those patients, which is wonderful. I don’t want to find those patients. I’ve put 2 people on in the past 5 years, and one of them was actually not even really refractory. He just wasn’t taking his medication. With CAR T, once I give it to him, he can’t take it, so this was more of me being paternalistic.
We’re doing so much better. As I mentioned at the beginning of the conversation, I have not had a patient die of CCL in the past decade.
Dr. Yair Levy
Jeff: Dr. Coombs, what is the single most important thing that you want patients and their caregivers to take away from this discussion?
Dr. Catherine Coombs: Jeff, we are friends now. It’s going to be hard to narrow down one thing, but I think if I have to say one thing, it’s there is hope. Leukemia is a horrifically scary word to hear for the first time, or maybe even after years of knowing that this is what you have. But all the treatments work extremely well and they work for an extremely long time. There is hope. Hope to live a normal life, and hope to see your kids and your grandkids grow up. There’s always hope on the horizon, in my opinion.
Encouragement for CLL patients to advocate for themselves
Jeff: What can patients and their caregivers do or ask if their local hematologist-oncologist isn’t quite looking at this new wonderful stuff that’s on the plate right now? What if they’re just going with the old stuff?

Dr. Catherine Coombs: That’s such an important question. And, you know, I think it’s tricky. I think it depends on what your personality type is. My personality is that I want to make everyone happy. I never want to offend anyone. I certainly understand the hesitation to question your doctor. But I think in the end, you just have to realize this is your life. If your doctor is not sounding up to date or if you’re just not getting your questions answered, then you deserve more than that.
I just think it’s so important to advocate for yourself or advocate for your loved ones if things aren’t adding up. I think our community docs are amazing. The ones that I interact with, I have no idea how they keep up with everything they keep up with. To put things into context, there are around 20,000 cases of CLL diagnosed a year.
When you think about the common cancers that have a majority of patients, they’re seeing lung cancer, breast cancer – those are like 200,000 plus cases. CLL ends up just being a much smaller slice of what they’re seeing every day, and it’s just very hard to keep up. I would say most community docs I work with very much welcome the second opinion because I can teach them something and then we now have a relationship where they’ll ask me questions and we can work together.
So, number one, don’t be worried about offending your doctor. Number two, most doctors aren’t going to be offended. Number three, if they are, well, I don’t know what to say about that, but I don’t get offended. Back when I was at UNC, I had patients go to Duke and the Duke patients would come to me. Sometimes it’s just good to hear things twice. I think if your doctor is offended, that’s a red flag on their own ego. I think all that we should want as your doctors is for you to get the information you need. That is your job to advocate for yourself, and almost all doctors are going to be totally happy with it. We can learn something from each other as we share in your care journey going forward.
There is hope. Hope to live a normal life, and hope to see your kids and your grandkids grow up. There’s always hope on the horizon.
Dr. Catherine Coombs
Jeff: Thank you for that and I love the way you put it. Patients should not be concerned about asking questions. They shouldn’t be concerned about saying, why not? If they’re having trouble getting along with their doctor, like you said, that’s a red flag.
Navigating what symptoms you should share with your doctor
Michele: We have some more patient questions, so here’s one of them. Sara N. asks, “How do I know when I should contact my doctor between visits? Do they need to know about every infection or just about CLL symptoms?”
Dr. Catherine Coombs: Sara, that’s a great question. I think in the digital age, we certainly can let doctors know about every single detail, but I think it’s good to set up expectations. I try to do this on my first visit or maybe my second visit if we don’t have time to cover it.
But what things do I always want to know about, and then what goes into the other category? I always educate my patients on red-flag symptoms. Things that for my patients on watch and wait, watch and worry, active surveillance, things that make me think, we need to get you in right away. Unintentional weight loss, drenching night sweats, fevers. I go through the list of the things I always want to know about – a rapidly enlarging lymph node, etcetera.
Then there may be other symptoms, and the ones I want to know about are the ones that are worrying you. I don’t want you to go to bed freaking out about something that may be nothing. Just send me a message and I’ll tell you, that’s nothing or I need more information. Maybe let’s have you come in. I’d say, it’s never wrong if it’s something worrying you. But of course, we all have to acknowledge it could get to be a lot of messages if it’s every single thing. I think you just learn that over time as you establish with a doctor, but I think it’s good to go through what things should I let you know about right away, and what things can wait. Then obviously there’s some gray zone where it doesn’t hurt to just pass the info along and then you can get back a message and not worry about that.
Michele: In looking at a patient holistically, so to speak, regarding these little things that we may not think are important, such as all these various infections – I keep getting sinus infections. I’m trying to think of some other types of infections. Maybe you could list those for patients, some of the ones that they might be seeing that you want to know about.
Dr. Catherine Coombs: We do see an increase in infections in our patients with CLL. I do like to get a general sense of how often patients are getting infections. If they have a primary care doctor who’s very responsive, I’m okay with them treating these infections. I’m also okay taking the lead, whatever works best.
But when they become really frequent, especially if it ends up with the patient landing in the hospital, I absolutely do want to know about that. There are some strategies we have to lessen the incidence of these infections.
Patients with CLL, a proportion of them, don’t make enough immunoglobulins. If you’re landing in a situation where you’re having a lot of severe infections, meaning pneumonia that you’re in the hospital for, or terrible sinus infections, etc., that may be a reason to consider this intervention called immunoglobulin infusions.
I definitely like to know about things that I can fix. I’m okay knowing about things I can’t fix too. The ones where it’s like, this would change what we do, those are especially important. The patients may not know that before messaging me, and that’s okay. It’s okay to just message because you don’t know and then I’ll tell you there’s nothing to do or let’s bring you in and talk about X, Y, Z.
I always educate my patients on red-flag symptoms…Unintentional weight loss, drenching night sweats, fevers.
Dr. Catherine Coombs

Jeff: Fantastic. I’m going to make this a little bit personal as far as what I hope people are taking away from this discussion. When I was first diagnosed with CLL, my doctor told me straight up that I was going to die in about 6 years, and that doctor got fired. My next doctor told me, “Don’t worry, we’ve got this. You might die with this, but you’re not going to die from this.”
Listening to both of you fantastic doctors talk about the landscape of CLL and even use the 4 letter word “cure,” I am convinced that I am going to be able to continue doing everything that I want to do, and I want to do an awful lot of things at some point. If my daughters’ are cooperative, maybe I’ll become a grandfather, but I’m going to continue knocking out half-marathons. I’m going to continue knocking out full marathons. I’m going to drink good wine and good whiskey. I’m going to eat well. I’m going to laugh a lot. I’m going to smile a lot and I’m going to share my story so that patients and their caregivers know that that can be their life, too. Michele, how about you?
Michele: I agree some of my key takeaways are that there are so many things in research and we have the potential of being approved in the somewhat near future, which is yet another option for us. As you had explained, it does work in a different way than the traditional types of BTK inhibitors we now have. I think this is fabulous to have yet another option for patients.
Also, I love what you said about what you really need to look for in your own doctor and not be worried about offending your doctor. This is so vital for patients. I ask a million questions and I encourage patients to do so so that they can become more empowered for their own care and self-advocate for themselves.
It’s been so great hearing you and Dr. Levy both talk about patients asking questions and encouraging them so that patients are not afraid of this. This is again, one of the things I had started doing to try to get rid of the mystique around care and treatment with people’s doctors. I continue to do that.
In addition with Jeff – and we’ll be toasting soon, hopefully in person about this with something more than water, which we’ve been drinking during the program – and that is to live life to its fullest and to live a normal expected life span thanks to doctors like you, Dr. Coombs and Dr. Levy. I thank you so much for joining us, both of you and I thank all of our audience members watching us.
Dr. Catherine Coombs: And thank you both for all the work you do in patient advocacy. Like 10, 15 years ago when the Internet wasn’t available, I think there’s so much more fear. To be able to bring light in a way that patients can understand is so hugely important. So thanks for what you do as well and for having me.


Special thanks again to AbbVie and BeiGene for their support of our patient education program all about building shared treatment decision-making! The Patient Story retains full editorial control.