Jim’s Myelodysplastic Syndrome Story
Interviewed by: Nikki Murphy
Edited by: Katrina Villareal
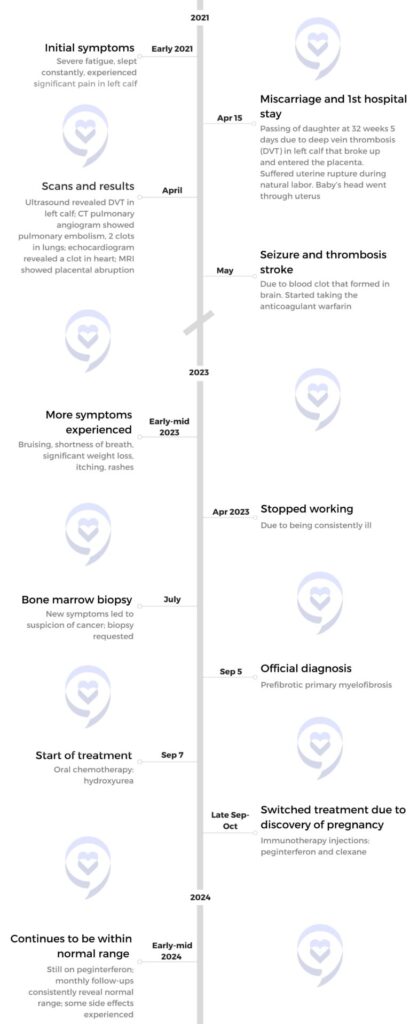
In 2014, Jim was diagnosed with myelofibrosis after an X-ray for kidney stones revealed an enlarged spleen. Follow-up tests showed elevated white blood cell counts, leading to a bone marrow biopsy and confirmation of the disease. Initially asymptomatic, he monitored his condition through regular blood work.
Four years later, in 2018, he began experiencing severe fatigue and breathlessness. These symptoms led to a diagnosis of myelodysplastic syndrome (MDS), a serious condition that could progress to leukemia. His prognosis was grim without a stem cell transplant, giving him potentially only months to live. Despite his age of 70, a medical committee deemed him a suitable candidate for the transplant due to his overall health. He underwent chemotherapy and numerous blood transfusions to prepare for the procedure.
A matching stem cell donor was found in Germany, and the transplant occurred in October 2018. The process involved intensive chemotherapy and total body radiation, followed by a stem cell transplant. Post-transplant recovery was challenging, with prolonged hospitalization, physical weakness, and isolation to protect his immature immune system. However, he avoided severe complications such as graft-versus-host disease, experiencing only a manageable rash.
This experience reshaped his outlook on life. Gratitude became a central theme, as he embraced moments with family, trips to the beach, and future travel plans, including a visit to meet his donor. He credits his recovery to the unwavering support of his wife, who served as his full-time caregiver, and his confidence in his medical team.
Looking ahead, he hopes for advancements in treatments to eliminate the need for stem cell transplants and alleviate complications. He encourages others facing similar challenges to maintain faith in themselves, their medical teams, and support systems.
- Name: Jim C.
- Age at Diagnosis:
- 70
- Diagnoses:
- Myelodysplastic syndrome (2018)
- Myelofibrosis (2014)
- Symptoms:
- Enlarged spleen
- Fatigue
- Shortness of breath upon exertion
- Treatments:
- Chemotherapy
- Blood transfusions
- Allogeneic stem cell transplant





Thank you to Sobi, Karyohpharm, GSK, and Novartis for supporting our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make treatment decisions.
My myelofibrosis was discovered accidentally. I didn’t experience symptoms.
Introduction
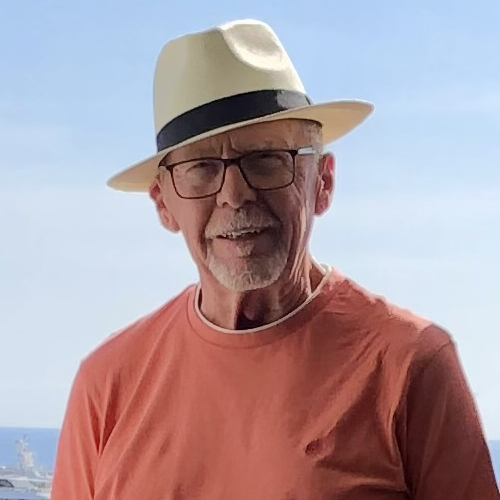
I’m a retired lawyer. I was a prosecuting attorney for 10 years and then a corporate litigator for about 20 years. Nearing the mid-2010s, we moved west of downtown St. Louis. We live with our daughter and her three children, so they help us and we help them. We have horses, donkeys, and chickens. Most of the time, I’m the pool boy, the stable boy, the groundskeeper, and the handyman, but most importantly, I’m grandpa.
I was diagnosed with myelofibrosis in 2014 and myelodysplastic syndrome in 2018.


Pre-diagnosis
Initial Symptoms
My myelofibrosis was discovered accidentally. I didn’t experience symptoms. I had kidney stones, so I would get an X-ray every year. In late 2013 when the X-ray results came back, I also had a slightly enlarged spleen, which I didn’t think was important.
Luckily, my wife’s a nurse and our doctors thought it was important. They started doing some follow-up and more blood work. My white count was too high, which was suggestive of a problem.
I had no symptoms, no discomfort, and no treatment. We kept track of it by doing blood work fairly often.
Getting a Blood Cancer Diagnosis
My family doctor recommended that I see an oncologist, who my wife and I knew well. He ordered a bone marrow biopsy. I still remember the day he came in and said, “We’ve got a diagnosis. You have blood cancer.” He indicated that it was not his area of expertise, so he recommended either Saint Louis University or Washington University. Since WashU’s where I’d gone to law school, I figured their medical school was probably good too, so I chose Washington U.
I met a doctor there who is a leader in that area of cancer. He told me about myelofibrosis, where you had 7 to 10 years on average before you run into trouble, and at that point, it might morph into leukemia or something. I had no symptoms, no discomfort, and no treatment. We kept track of it by doing blood work fairly often.


In the spring of 2018, I began to get very short of breath at the slightest exertion. I was 70 years old at the time and I thought that maybe it was my age, but it was worse than that. Fatigue set in, so we did more tests.
We had a conversation with the doctor and he said, “Jim, this is serious. You have myelodysplastic syndrome. With your situation, you might go six months, a year, or a little longer if you’re lucky unless we can find a donor and get a transplant.”
We walked down the hall to the transplant doctor to begin the process. When we first talked, she used the word cure, that stem cell transplant is a possible cure. It was encouraging. She also said, “When I saw your picture, I knew that you were a good candidate for this,” so that gave me comfort and hope.
Because I was 70, a special committee had to meet to determine my eligibility. I was otherwise a healthy person, so her acknowledging that and saying I was going to be okay for the transplant made me feel good.
I was very confident in the medical treatment that I was getting and the support I had from my wife and my family.
Reaction to the Diagnosis
I don’t remember panicking or getting too distressed. When the doctor from Washington said 7 to 10 years, I thought, well, I’m already 70. When you tell a 70-year-old that he’s got 7 to 10 years, he’s probably going to say that’s not too bad and so that didn’t upset me too much.
What it did do is that instead of my wife and I talking about doing something someday, we scheduled it for the following month or year. We started to travel a lot and did a variety of other things that kept getting pushed back. You say that you’ll do something someday and so we did.

When the doctor came in and gave me three months, that was a little more unsettling. The worst moment was being told you’ve potentially got a few months to live. It was a combination of being an optimistic person and a person of faith. I was very confident in the medical treatment that I was getting and the support I had from my wife and my family.
The other possibility is I’m oblivious to it. What am I going to do? I can shout and throw things; that’s not going to help. I don’t ever remember feeling down.
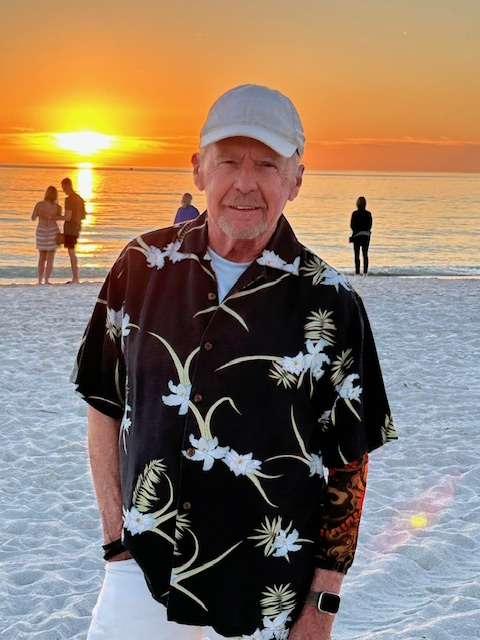
Shortly before I went into the hospital, I said I’ve got to get to the beach again. Living in St. Louis, there are no beaches nearby, so we took a quick trip down to Destin. It was still warm enough where you could walk along the beach and that was relaxing.
There was one time when I thought this might be the last time I was going to be at the beach. I guess it’s part of my faith. I thought if I was going to die six months from now, after that, I probably wouldn’t miss the beach. I hope where I’ll be is a lot better than the beach anyway, so that’s not an issue.
They found a donor and it was a perfect match… My donor is from Germany.
Getting a Stem Cell Transplant
For the myelofibrosis, we watched and waited. Once the myelodysplastic came in, we immediately started a pretty serious regimen of chemotherapy and blood transfusions. In June 2018, I had a week of chemo every day, probably one or two transfusions during that week, a couple of weeks off, and then repeat. I don’t know how much chemo I had, but I counted 15 or 16 blood transfusions during that time. Thankfully, I did not react poorly to the chemo. I don’t remember being sick at all. I usually felt better after getting blood.
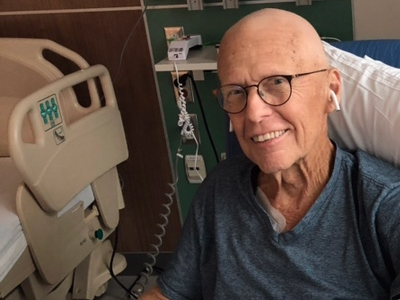
In late September, I was told that they found a donor and it was a perfect match. Before the scheduled transplant, I went to the hospital and received heavier chemo for about a week and then I had total body radiation, which I referred to as being microwaved. You sit on a table, clutch your knees, they measure your body, you stay in one position for about 10 minutes, you turn around, and do it again. That was the only time I felt sick after.


I was weak. It’s do-or-die at this point. They scheduled the transplant for the evening of October 11, which was cool because that’s my oldest granddaughter’s birthday and I’ll get my new birthday on the same day. My donor is from Germany. We discovered later that the courier missed the train, so it was delayed. The transplant finally happened a little after midnight on the next day, October 12.
The doctor came in and it was in a small bag, smaller than a typical blood bag. I already had a port in my chest. I suspect the doctor was there in case I had an immediate bad reaction for some reason, which I did not. It’s pretty anticlimactic. You wait for the stem cells to drain out of that bag. After a while, I went to sleep and that was it.
I don’t know how I would’ve felt if this hit me at 29… I’ve had a good life already. If something happens, it’s unfortunate, but at 70, it’s not terrible.
Post-Transplant
I was in the hospital for a month. My wife was with me 24/7. Thank goodness she’s also a nurse, so that helped. Fairly soon, I started taking antibiotics, antifungals, and antivirals. I didn’t have graft versus host disease, except for a rash that we treated and went away.
I was very weak. When I came home, I very slowly got my strength back. I had physical therapy and occupational therapy. I stayed away from other people for a good bit because I had a very immature immune system. I’m still taking various medications.

Renewed Appreciation for Life
I didn’t and don’t wake up every morning saying thank you to God for another day; my wife does. Other times, it will hit me, like when I’m watching my grandson do something, being able to go to a baseball game, or going back to the beach, I would think, “I almost missed this,” and that makes me feel good.
I don’t know how I would’ve felt if this hit me at 29. One of the first times that I felt sorry for myself was when I was getting chemo and a kid next to me learned that he had leukemia a week before. He was around 20 and you know how different and how difficult that must be. I’ve had a good life already. If something happens, it’s unfortunate, but at 70, it’s not terrible.
If you’ve got a caregiver who’s impatient or gets tired easily, that can be a problem. It requires dedication and love. Having a caregiver makes a difference.
I have a renewed appreciation for life. It comes at the weirdest times, but almost every day, something comes to mind and I say to myself, “Oh, I almost missed this.”
We’re planning a vacation for the summer. We already planned a trip to Scotland with our church group. I’ve been in contact with my donor, who was 24 at the time. He recently turned 30 and said that we would have to find each other if I were ever in Europe. We decided to spend a few extra days to go to Germany to meet him and his girlfriend.


The Importance of Having a Care Partner
I hit the jackpot with my caregiver. My wife’s an RN and a retired hospital administrator, so she knew who to call if there was an issue and who to talk to, and was not shy about doing it. There weren’t that many issues, but she also literally stayed in the hospital room with me 24/7, except for one time, but my sister substituted for her.
At home, I couldn’t do much for myself. If you’ve got a caregiver who’s impatient or gets tired easily, that can be a problem. It requires dedication and love. Having a caregiver makes a difference. I don’t know how you could do it without someone, even if they can’t stay 24/7. It’s hard to describe how important it is.
Connect and look for help. Don’t give up.
The Future of the MPN Landscape
It would be great if there could be some treatment that would be as good as a transplant but didn’t require a transplant. White Caucasians have a pretty good chance of finding a good match. If you’re Black or Latin American, there aren’t that many donors. I don’t know if it’s a lack of education or effort to spread the word or how important it is. If there could be something other than a transplant that would work, that would be great.
A lot of work still needs to be done on graft versus host disease. One of the doctors in the team had 2 or 3 transplants himself and had terrible graft versus host disease. A gentleman down the hall from us had terrible mouth sores that made it almost impossible for him to eat or drink. Now, I think that eventually cleared up, but it’s still a difficult time to have to go through. Work needs to be done and an alternative to transplants would be great.


Words of Advice
Have faith. Have faith in yourself, in God, and in your medical team. If you don’t have faith in your medical team, find another one. It’s easy for me to say being in St. Louis because we have a variety of excellent medical facilities around, but there’s help out there.
Finding organizations that will help you find the help you need would be worth looking into. If you’re not happy with your doctor, find another one. Luckily, that’s not been my experience at all. It’s important to connect and look for help. Don’t give up.




Special thanks again to Sobi, Karyohpharm, GSK, and Novartis for their support of our independent patient education content. The Patient Story retains full editorial control.
Inspired by Jim's story?
Share your story, too!
More Myelodysplastic Syndrome Stories
Jim C., Myelodysplastic Syndrome
Symptoms: Enlarged spleen, fatigue, shortness of breath upon exertion
Treatments: Chemotherapy, blood transfusions, allogeneic stem cell transplant
Nicole T., Acute Myeloid Leukemia (AML)
Symptoms: Severe itchiness, night sweats, fatigue
Treatments: Chemotherapy, bone marrow transplant