How a Mom with Stage 4 Colon Cancer Turned Pain Into Purpose
When Lauren began feeling off in early 2025, she figured it was just constipation, since she was usually irregular. But when she found herself running to the bathroom up to 27 times a day, she knew something wasn’t right. Despite her persistence, early appointments with her primary care provider and even an ER visit didn’t give her the answers she needed. Her path to a stage 4 colon cancer diagnosis would take perseverance.
Interviewed by: Nikki Murphy
Edited by: Katrina Villareal
Eventually, her gut instincts led her to push for a GI consult, and that’s when her life changed. After a colonoscopy couldn’t even get past the blockage, a CT scan finally revealed the unthinkable: stage 4 colon cancer, specifically a rare and aggressive type called signet ring cell carcinoma (SRCC).

Lauren’s diagnosis came fast, and with it, a whirlwind of decisions. Within hours of her arrival at the ER, doctors were talking about cancer and prepping for emergency surgery. Lauren underwent a colon resection and came home with a colostomy bag. At just 41 years old, she found herself facing a diagnosis most people associate with much older adults. And while the shock was overwhelming, Lauren chose to face it with openness, strength, and grace.
Navigating treatment has been tough. Chemotherapy brought on intense neuropathy, nausea, and deep fatigue, but Lauren focuses on what keeps her going: her two young children, her incredibly supportive husband and family, and her inner fire. Talking to her kids about the changes in her body, including the colostomy bag and the port in her chest, wasn’t easy, but she handled it with honesty and love. Her children quickly adapted. Their curiosity turned into acceptance, and their resilience reminded Lauren that life, even now, is still full of beauty.
Since being diagnosed with stage 4 colon cancer, Lauren’s perspective has shifted in powerful ways. She’s slowed down, learned to cherish simple joys like reading in the backyard, and poured her heart into writing children’s books, stories inspired by her daughter’s autism diagnosis. Cancer pushed her to finally do what she loved.
Lauren now advocates fiercely for early screenings, especially since her cancer type often doesn’t show symptoms until it’s advanced. She also urges others to trust themselves. If something feels off, speak up. Her story is a moving reminder that you don’t need to look sick to be facing something serious, and that even in the hardest moments, it’s possible to find love, purpose, and joy.
Watch Lauren’s full interview to find out more about her story:
- Discover how a bathroom log helped lead to a life-saving diagnosis.
- Learn how Lauren explained stage 4 colon cancer to her young children in the most beautiful way.
- Find out why her daughter’s autism diagnosis gave even deeper meaning to her children’s books.
- Hear how Lauren’s life shifted from corporate chaos to creative purpose.
- See how love, laughter, and support lifted her through one of life’s hardest moments.
- Name: Lauren G.
- Age at Diagnosis:
- 41
- Diagnosis:
- Colon Cancer (Signet Ring Cell Carcinoma)
- Symptoms:
- Frequent urges to have bowel movements (up to 27x/day)
- Incomplete evacuation
- Abdominal bloating
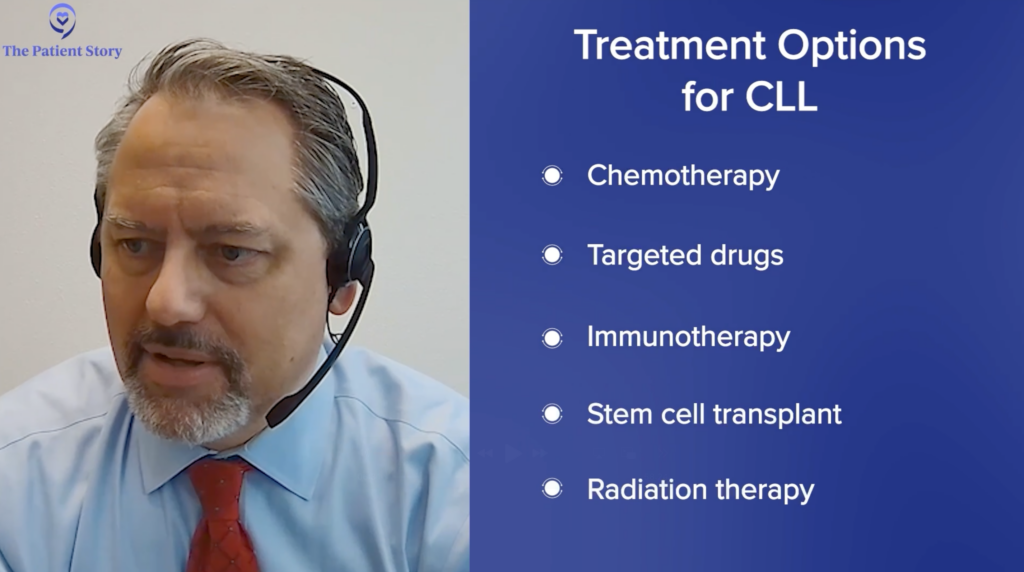
- Treatments:
- Surgeries: colectomy (colon resection), colostomy bag placement
- Chemotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.

Inspired by Lauren's story?
Share your story, too!
More Metastatic Colon Cancer Stories
Raquel A., Colorectal Cancer, Stage 4
Symptoms: Frequent bowel movements, pin-thin stools, mild red blood in stool
Treatment: Chemotherapy
Steve S., Colorectal Cancer, Stage 4
Symptoms: Blood in stool, changes in bowel habits, feeling gassy and bloated
Treatments: Surgery, chemotherapy, monoclonal antibody, liver transplant
Jessica T., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach cramps, diarrhea, vomiting, anemia (discovered later)
Treatments: Surgery (hemicolectomy), chemotherapy
Jennifer T., Colon Cancer, Stage 4
Symptoms: Weight loss, coughing, vomiting, sciatica pain, fatigue
Treatments: Surgeries (colectomy, lung wedge resection on both lungs), chemotherapy, immunotherapy
Kasey S., Colon Cancer, Stage 4
Symptoms: Extreme abdominal cramping, mucus in stool, rectal bleeding, black stool, fatigue, weight fluctuations, skin issues (guttate psoriasis)
Treatments: Surgeries (colectomy & salpingectomy), chemotherapy