Kina’s Stage 4 Colorectal Cancer Experience Highlights Fierce Self-Advocacy
Living in Canada, Kina always thought her intermittent IBS symptoms were just another part of her daily life, especially after becoming a mother. It was only when she noticed a flare-up in her IBS symptoms and, more ominously, blood in her stool that her doctor finally scheduled a colonoscopy, revealing a mass and launching her into a world she never expected as a stage 4 colorectal cancer patient. For months, doctors assumed it was an early-stage disease. But pneumonia-clouded scans hid cancer that had spread to her lungs, and only through persistence and a PET scan was the correct, advanced staging determined.
Interviewed by: Carly Knowlton
Edited by: Chris Sanchez
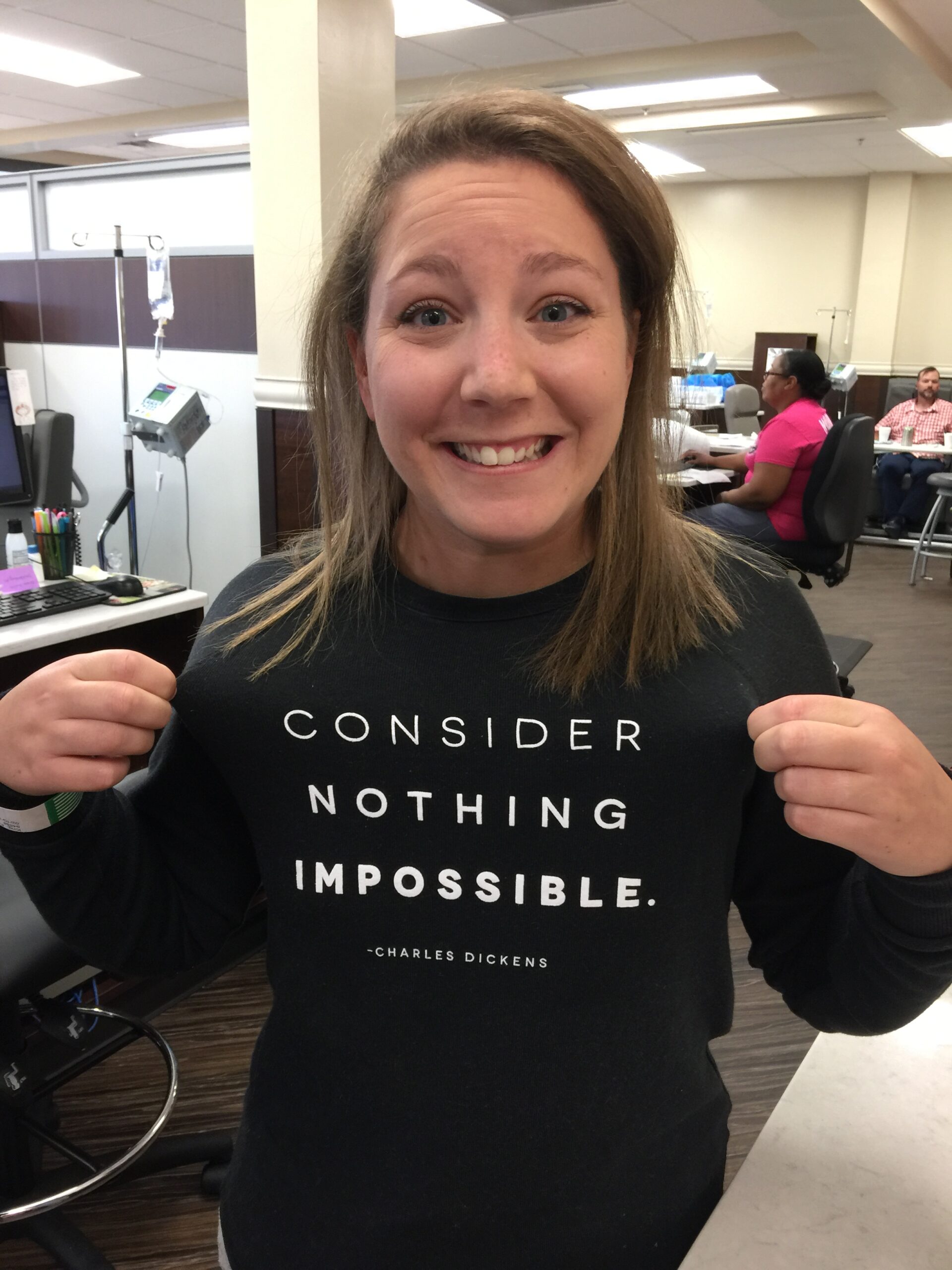
Self-advocacy became her focus. When an Ottawa surgeon offered limited surgical intervention, Kina joined patient groups, found others who also had colorectal cancer, and connected with a Toronto surgeon willing to attempt a more extensive procedure. Chemotherapy was followed by lung surgeries and a highly specialized procedure known as a chemoperfusion. Kina endured side effects like debilitating fatigue, neuropathy, and nausea, but the greatest burden was not being the present mother and partner she wanted to be. But her advocacy, networking, and relentless pursuit of the best treatment shifted her colorectal cancer experience from “incurable” to “no evidence of disease.”

Kina’s colorectal cancer experience deepened her gratitude and reshaped her worldview. Instead of regret over “Why me?” she reflected on why she deserved a second chance when others did not. She now encourages others to value every moment and says, “You just appreciate the beauty of nature, the wind in your face, the beauty of life, the little moments.” Kina’s transformation is profound: she shifted from a busy, overextended mom and professional to a fierce self-advocate and champion of preventive care. As she says, “The most difficult patients are the ones that survive: the ones that fight back, the ones that challenge the status quo.”
Watch Kina’s video and read through her interview transcript below. You’ll learn more about how:
- Early symptoms of colorectal cancer can easily be missed or mistaken for IBS. Advocate for yourself if symptoms change or worsen
- Getting a second opinion and connecting with others facing similar diagnoses can help make more treatment options available
- Peer support groups, research, and information-seeking are critical allies in complex or advanced cancer cases
- Kina’s cancer experience made her more grateful, present, and empowered to help others prioritize health and demand the best care
- The most stubborn patients are most often the ones who survive
- Name: Kina L.
- Diagnosis:
- Colorectal Cancer
- Staging:
- Stage 4
- Age at Diagnosis:
- 39
- Symptoms:
- Flare-up of IBS symptoms
- Appearance of blood in stool
- Treatments:
- Surgeries (through a clinical trial): double thoracotomy, lung resection
- Chemotherapy, including chemoperfusion (through a clinical trial)
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Kina
- My long history with IBS
- How I advocated for myself before diagnosis
- My hardest moments leading up to my diagnosis
- My initial diagnosis and staging surprises
- I researched, found better options, and had surgery
- I’m now NED
- My thoughts on clinical trials
- My mental and emotional journey
- What I want others to know
My name is Kina
I’m from Ottawa, Canada. I was diagnosed with colorectal cancer that had spread to my lungs.
I’m passionate about my family more than anything else. I love being outdoors: hiking, running, biking, camping, and just being among the trees. Reading and the written word are also big passions for me.
My long history with IBS
I’ve had IBS symptoms on and off for my whole life. They would come and go, so they became normalized, which was unfortunate because that can happen with colorectal cancer.
After I gave birth to my kids, my IBS symptoms disappeared for quite some time. I chalked it up to hormonal changes in my body, and I was no longer intolerant to some foods I had been before.
About six months before my diagnosis, my IBS symptoms started flaring up again. I cut dairy and coffee, and I saw some mild improvements. But then, at the end of summer and beginning of fall, I started having blood in my stool. That’s when I thought something was definitely wrong.
I booked an appointment with my doctor, who was already aware of my IBS symptoms. As a woman in my late 30s, I’m always dealing with symptoms and hormone stuff, so we didn’t look into it further at first. She booked me for a colonoscopy at the end of December, and that’s when they found the mass in my colon.
How I advocated for myself before diagnosis
My doctor is very good, so she booked the colonoscopy right away.
At the time, I had a new gig at work that I was excited about, so I was transitioning and initially put off the colonoscopy a bit. As a mom with two kids and two stepkids, plus a busy job, the last thing I was doing was taking care of myself. I had booked it for the end of January, but my partner pushed me to get it done sooner.
I called back and asked for the earliest appointment, so we did it on December 23rd. Christmas wasn’t fun, but at least I got the surgery at the end of January because of the quicker appointment.
My hardest moments leading up to my diagnosis
The hardest moments extend beyond just cancer for women my age; we’re very busy and overextended.
A lot of my girlfriends are dealing with different things, like one working on a PCOS diagnosis and another suspecting endometriosis. We push off getting checked because we’re constantly getting sick from our kids’ colds, and our immune systems are shot down.
I never felt healthy for maybe 6 to 10 months before diagnosis, but it was normalized. My immune system wasn’t working well, and I was getting all the illnesses, which impacted my family.
It wasn’t the cancer symptoms themselves, but my body not working right that was toughest.
My initial diagnosis and staging surprises
When I got the results back, they thought I was early-stage. The mass was pretty small, just four centimeters, and intact in the colon, not going through the wall.
My surgeon, GI doctor, and everyone had a good feeling about it. They removed 47 lymph nodes during surgery on January 31st.
But when I talked to my surgeon about the pathology afterward, he said eight of the nodes were cancerous, and I’d need preventative chemo. That was the first shock — I really thought it was early-stage and I’d go back to work.
Two weeks later, a CT scan showed the lung nodules had grown. I had a bad feeling it was cancer there too, but after the lymph nodes news, I already knew my journey would be long.
For four months, it was shifting from early stage to stage three with chemo, then to stage four and inoperable. I got diagnosed in December, and March was when they officially said stage four.
Colorectal cancer didn’t click for me
I didn’t know much about colorectal cancer at the time. The narrative is that older people get it, so even when I Googled my symptoms, it was worded as risks for people aged 50-plus.
I had a colleague, a bit older than me, who was diagnosed and unfortunately passed away, but because of how people viewed colorectal cancer, it just didn’t click that I could be facing the same situation. The early onset affecting younger people wasn’t discussed much back then. Even with a bad IBS night, googling symptoms didn’t point me to cancer.
Now I’m adamant: even if you have one symptom, get checked, because if I’d gone before the blood showed up, I might have caught it earlier. By then, it was already advanced, very focused on chemotherapy.
Initial treatment options, and my chemotherapy experience
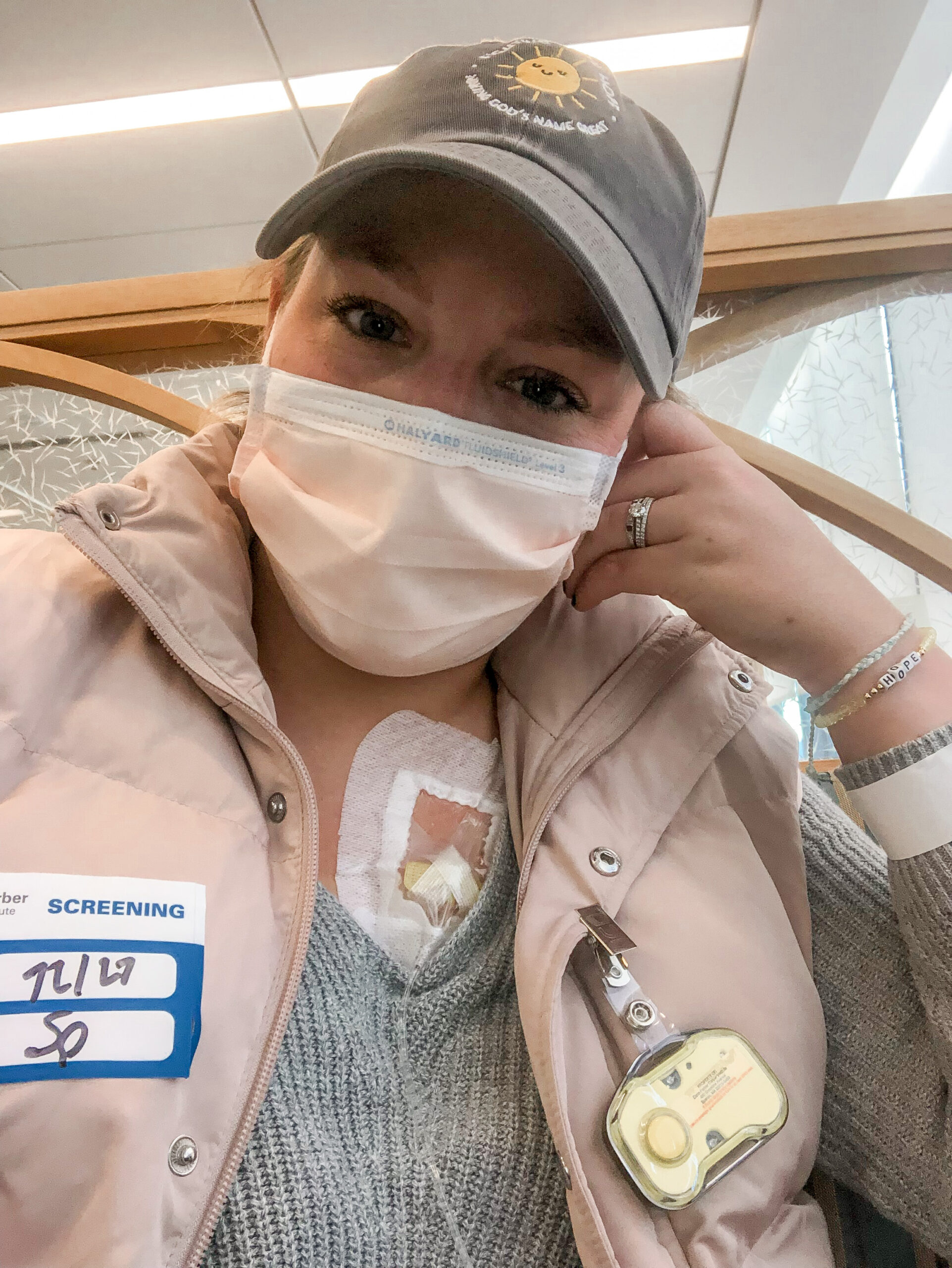
My oncologist described therapy and chemotherapy options. She referred me to the Ottawa surgeon, but she’s not a surgeon, so discussions were limited to chemo and hoping for the best.
I wasn’t eligible for immunotherapy, and clinical trials were more like something down the line. There’s a gap there; I understand standards of care and protocols, but my doctor likely didn’t know about other options like the Toronto surgeon.
If I hadn’t researched and advocated, I’d still be on chemo with the nodules grown and inoperable. They basically put me on chemotherapy for life until I found the surgical option.
The only reason we stopped chemo was for the Toronto surgery. I did six rounds in three-week cycles, about 4 or 5 months.
Chemotherapy is not fun at all. I was lucky to tolerate it well compared to others, but I had neuropathy, fatigue, a kind of metallic mouth where everything tastes like metal (it’s disgusting), and nausea. It was hard to do day-to-day stuff, especially near the end when I was on the max dose.
It was tough being the mom, partner, and friend I usually am. It impacted everything, but I have good people around me: a present partner, my mom always helping, and good co-parenting with my ex-husband. They picked up the slack when I couldn’t.
I rested the first few days after treatment, then tried to be there as much as I could. Sometimes I’d crash or overdo it and feel like garbage the next day on the couch. I forced myself to stay active; a short walk around the block helped manage symptoms. If I felt okay, we’d bike to school, go for a run, or hike to keep that outdoor connection.
I researched, found better options, and had surgery
I did a lot of research right away; I joined virtual conferences and exposed myself to everything I could. At first, it was difficult hearing tough things on a weekend, like attending two online conferences, but now it’s part of my reality.
I started researching to help myself immediately. That’s how I found the Toronto surgeon through Facebook groups.
My doctor accepted the referral, and he was removing nodules via a clinical trial.
After CT scans confirmed eligibility, we stopped chemo, and six weeks later, I had my first surgery on September 25th, a double thoracotomy on both lungs.
They then resected three nodules on my right lung and five on my left, plus a suspicious lymph node that turned out not to be cancerous, which was, of course, great news. The surgeon performed chemoperfusion on my left lung as part of the trial.
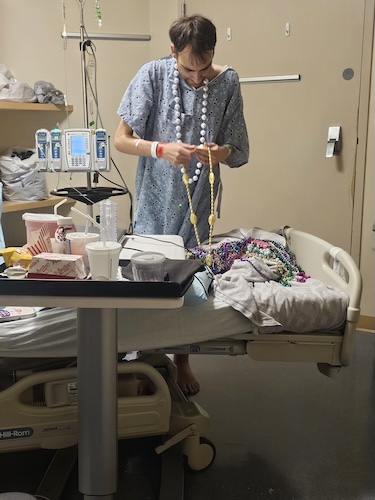
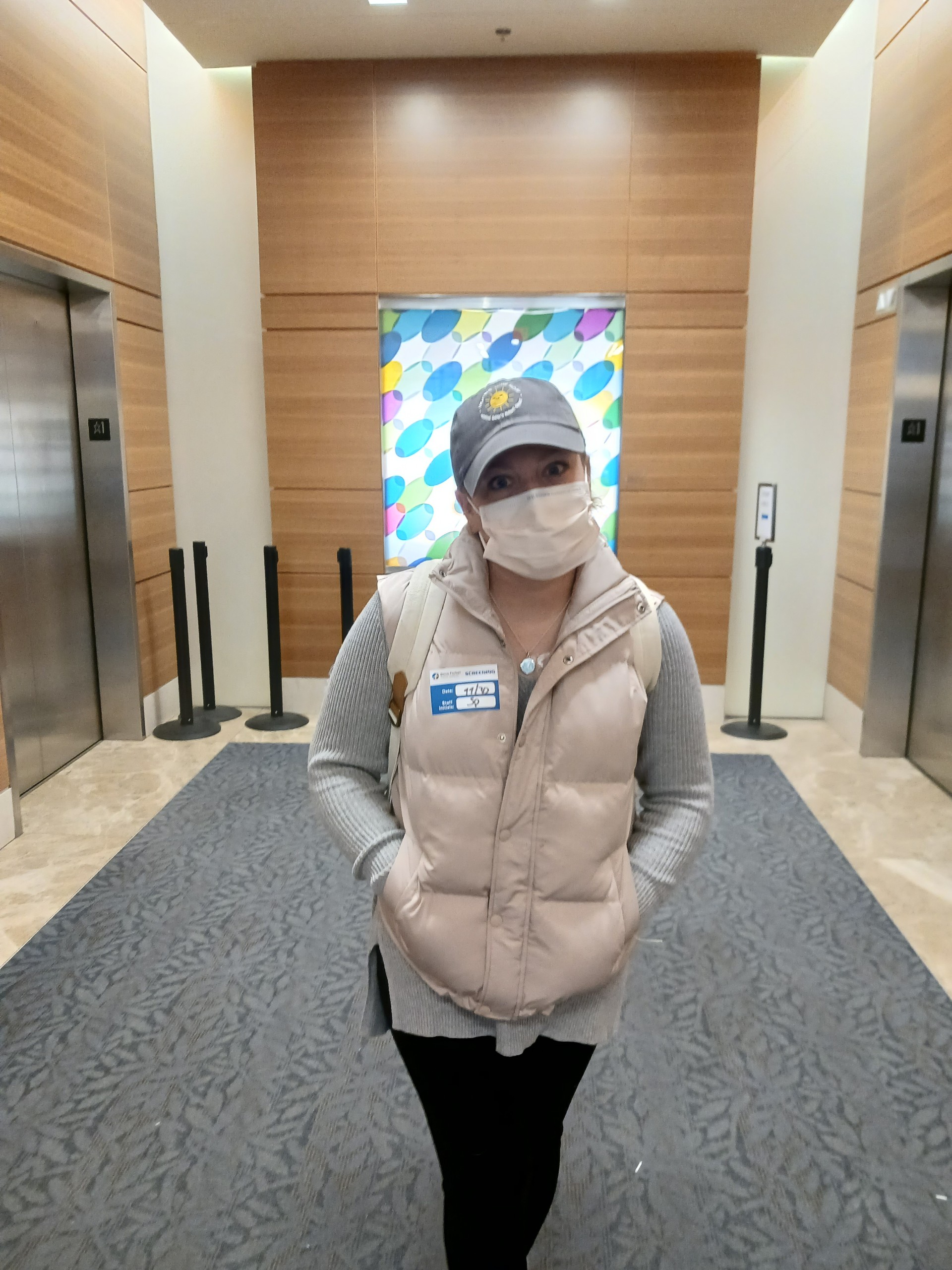
I was supposed to be in the hospital for a week, then stay in Toronto another week for a total of two weeks. But I had complications: blood transfusions, atrial fibrillation, lung collapse, and pneumonitis from the chemo inflammation. It was the highest dose they’d done, 40mg, and previous patients didn’t inflame, but I did.
Two weeks in, pneumonitis set in; I was on high oxygen, steroids, and antibiotics. I stayed a month and came home on October 22nd.
Improvements are slow, but happening. I’m still on oxygen when walking or talking; short of breath after almost two months. Recovery from that takes time.
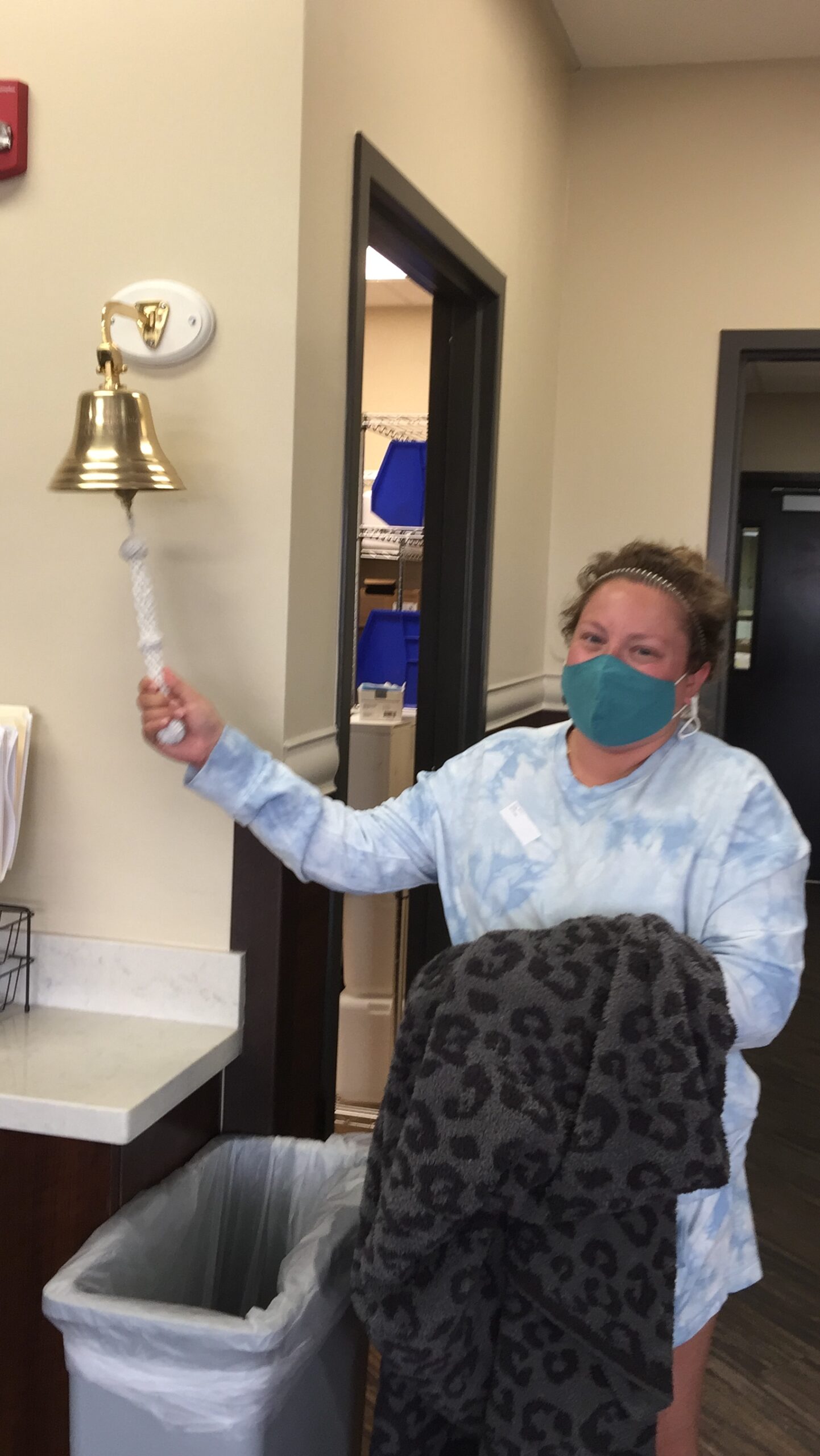
I’m now NED
Technically, I have no cancer in my body right now, and I’m hoping for the best.
We haven’t confirmed with a CT scan yet, but before surgery, the removed lung nodules were the only ones left.
I stopped chemo for the surgery, so no bell-ringing yet, but my friends and family talk about it. I think I should ring it to recognize everything I’ve been through, no matter what comes next in the next year.
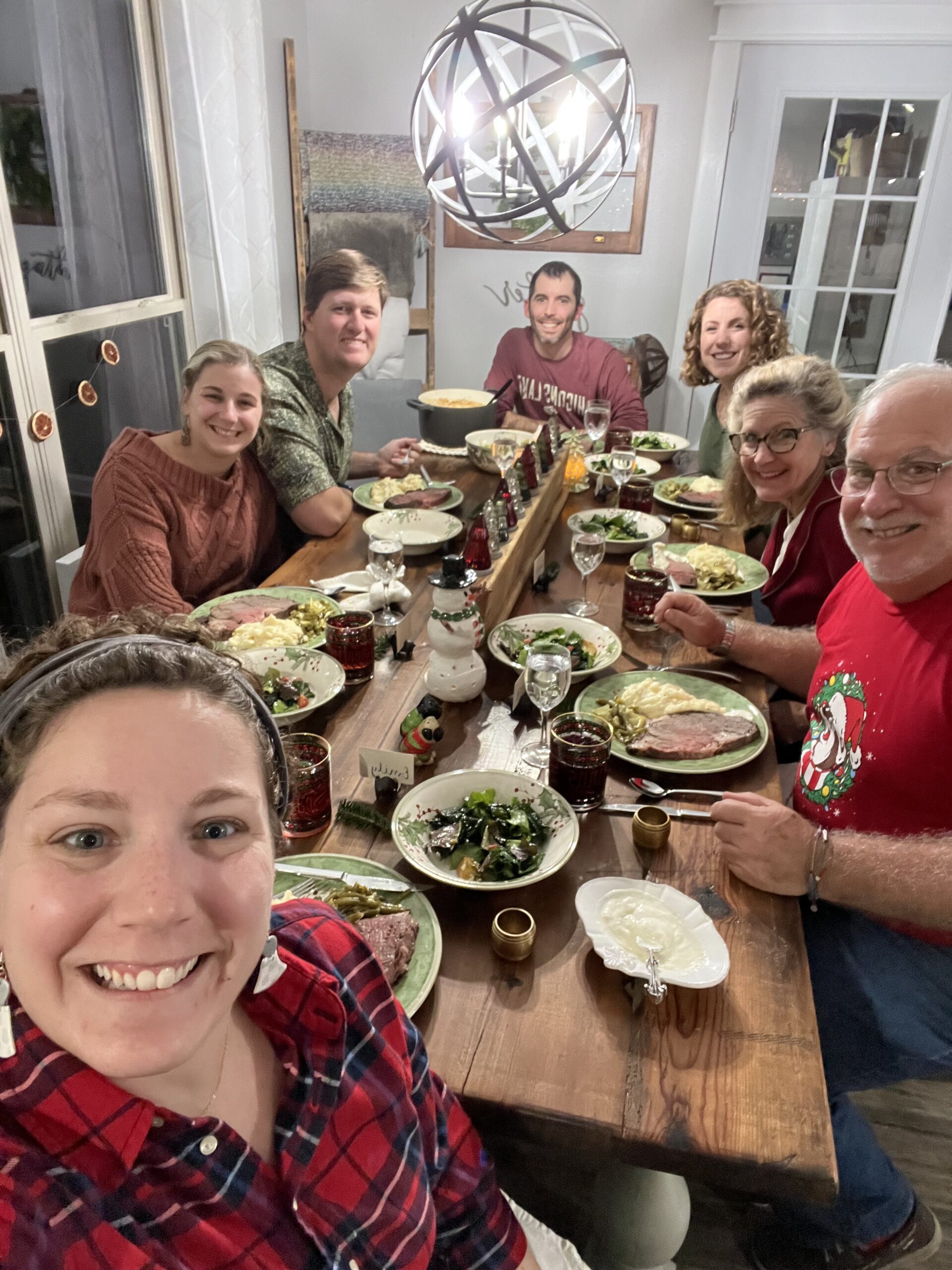
When I came home, my mom stayed for five days to help. We were lucky; people took good care of us. My girls are seven and ten, my stepkids are six and eight, so it’s busy and awesome.
Having me away for a full month was hard, but we made it through. They’re so happy to have me back emotionally.
My thoughts on clinical trials
Clinical trials are great for advancements, but they come with risks, and I’m a great example. I found a couple of people who’d gone through this trial before and spoke with them via the Facebook group.
The early-onset stage four colorectal under-50 community is small but growing. Do your research, talk to people if you can, and know the risks because side effects are real.
Sometimes it’s worth it, not just for you but for others who could benefit later. As I mentioned earlier, I’m still recovering; not at full capacity, walking slowly with oxygen.
My mental and emotional journey
I don’t think “why me?” It’s the opposite, like imposter syndrome: why would I deserve to be cured when others aren’t?
The hardest part is knowing that if I’d found it earlier, I wouldn’t be here now. There’s regret for not paying more attention.
I encourage my girlfriends: don’t delay, a colonoscopy is the gold standard for colorectal cancer. So just do it. Many around me took it seriously, got colonoscopies, and had polyps removed; that’s when you want to catch it, not too late.
If there had been more advocacy for early-onset colorectal, it would have clicked sooner, and I’d have acted differently, 100%.
It’s not a gift, but it gives perspective. Right after stage 4 diagnosis, I went for a walk and appreciated everything: the beauty of nature, wind in my face, and little moments. Before, I was busy, saying yes to everything, always on the go with work. No matter what, I won’t operate that way again—life’s too short, take care of yourself.
What I want others to know
Work as hard as you can to advocate for yourself. Make sure the option presented is the best for you.
There are so many treatments, clinical trials, and other things out there. Don’t take the first answer; challenge your doctors. Books say difficult patients, namely the ones who ask questions, fight back, and challenge the status quo, are the ones who survive. Don’t be afraid. You have to take care of yourself.
I think my self-advocacy may have saved my life. If I hadn’t, I’d be in a very different situation.
I was lucky to be positive and resilient; it carried me through. I focus on gratitude because it could be worse. I responded to treatment, found a surgeon, and have people around me.
I have so much to be grateful for. It’s ingrained in me to keep a positive mindset. Colorectal cancer in young people is rising. If you’re experiencing just one symptom, look it up, go for a colonoscopy.
Getting the appointment is tough, but don’t ignore the symptoms, and advocate for yourself.

Inspired by Kina's story?
Share your story, too!
More Colorectal Cancer Stories
Lindsay D., Colon Cancer, Stage 4
Symptoms: Lump in pelvic area, funny-smelling food, weight loss
Treatment: Chemotherapy, colectomy (surgery)