Samantha’s Adenocarcinoma Cervical Cancer Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
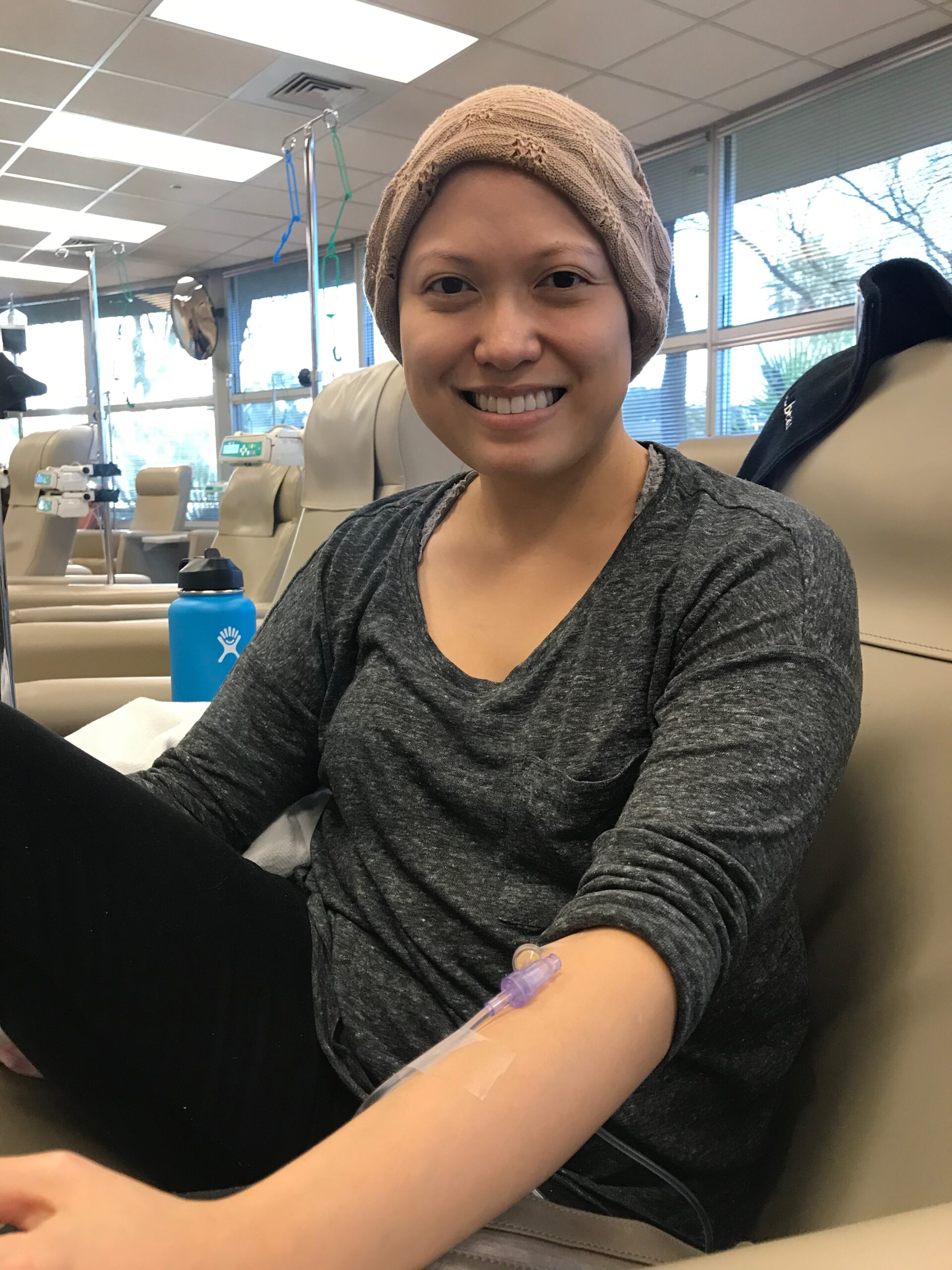
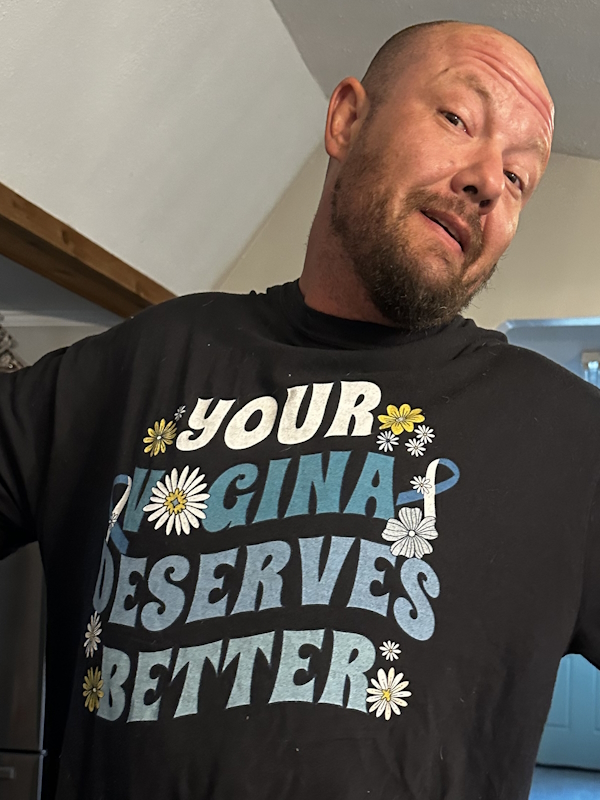
Samantha R. is a three-time cervical cancer survivor from Las Vegas, NV, who has turned her experience into a passion for health advocacy. She emphasizes the importance of listening to one’s body and advocating for oneself in the healthcare system.
Samantha’s story started in 2016 when she first experienced symptoms like irregular bleeding and pain, which led her to visit her OBGYN. After a Pap smear revealed abnormal cells, she underwent a LEEP procedure. However, she delayed follow-up appointments, which allowed her condition to worsen. Eventually, her doctors diagnosed her with cervical cancer at the age of 27, shortly after her wedding.
Samantha and her husband were devastated by her diagnosis, especially since they were eager to start a family. Her treatment involved a radical hysterectomy, which was physically and mentally challenging. The surgery altered her life significantly, affecting her identity as a woman and her future family plans.
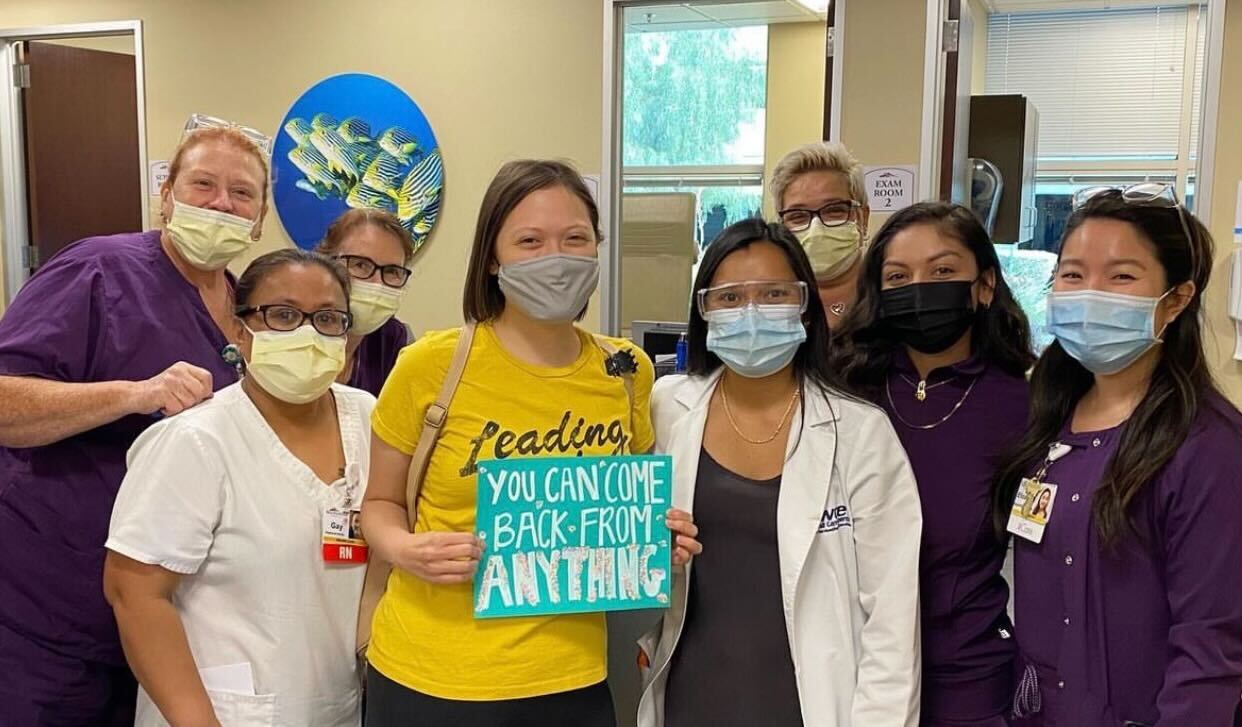
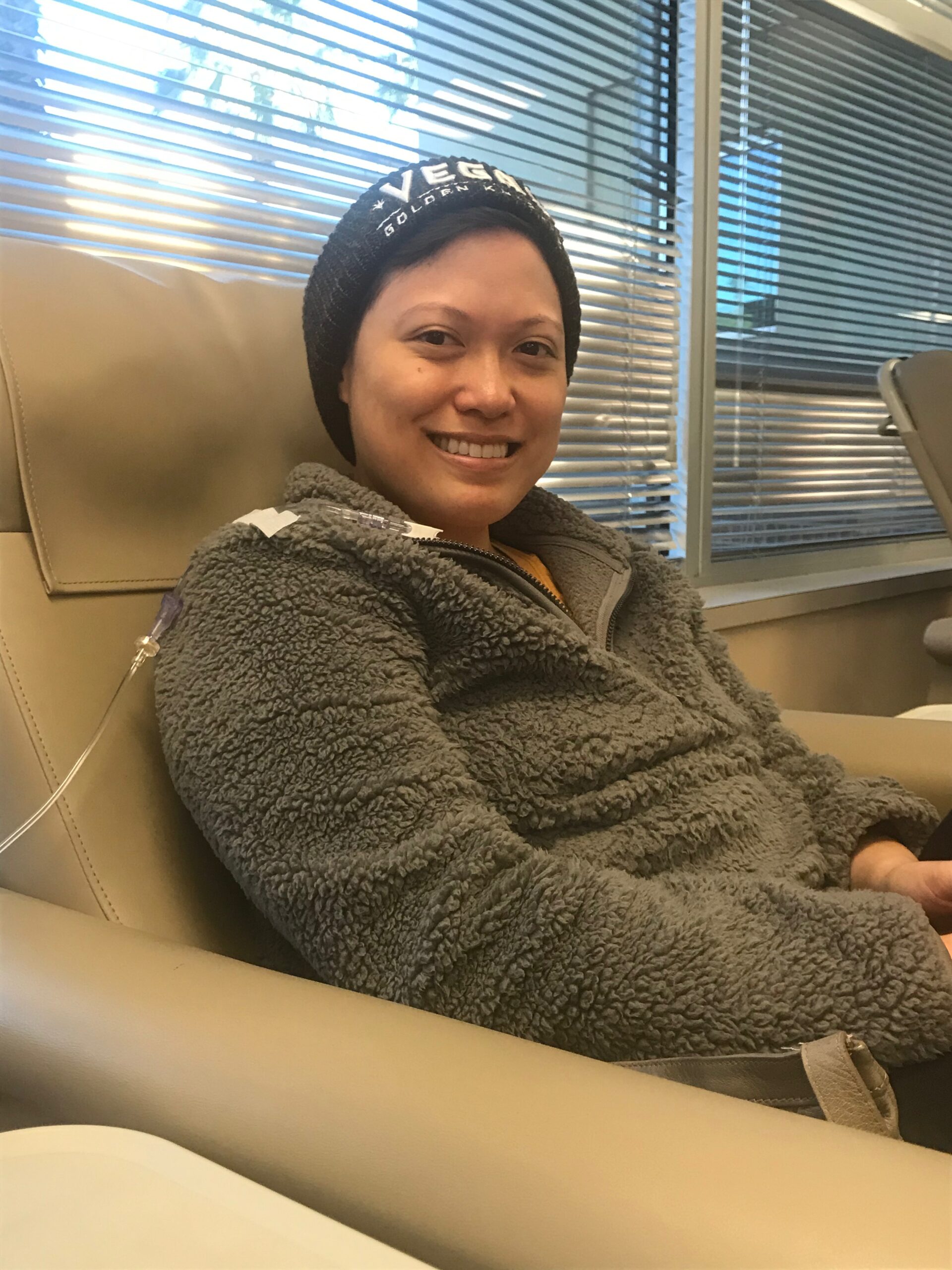
Samantha’s cancer’s recurrence, in 2018, was marked by severe symptoms that her doctors initially dismissed as stress or a UTI. After months of her pushing for answers, they finally diagnosed her with a large tumor in her cervix and intestines. This led her to find a new medical team who took her concerns seriously. She underwent surgery to remove the tumor, followed by chemotherapy, immunotherapy, and radiation throughout 2019. By the end of the year, her medical team declared her cancer-free, but her journey wasn’t over.
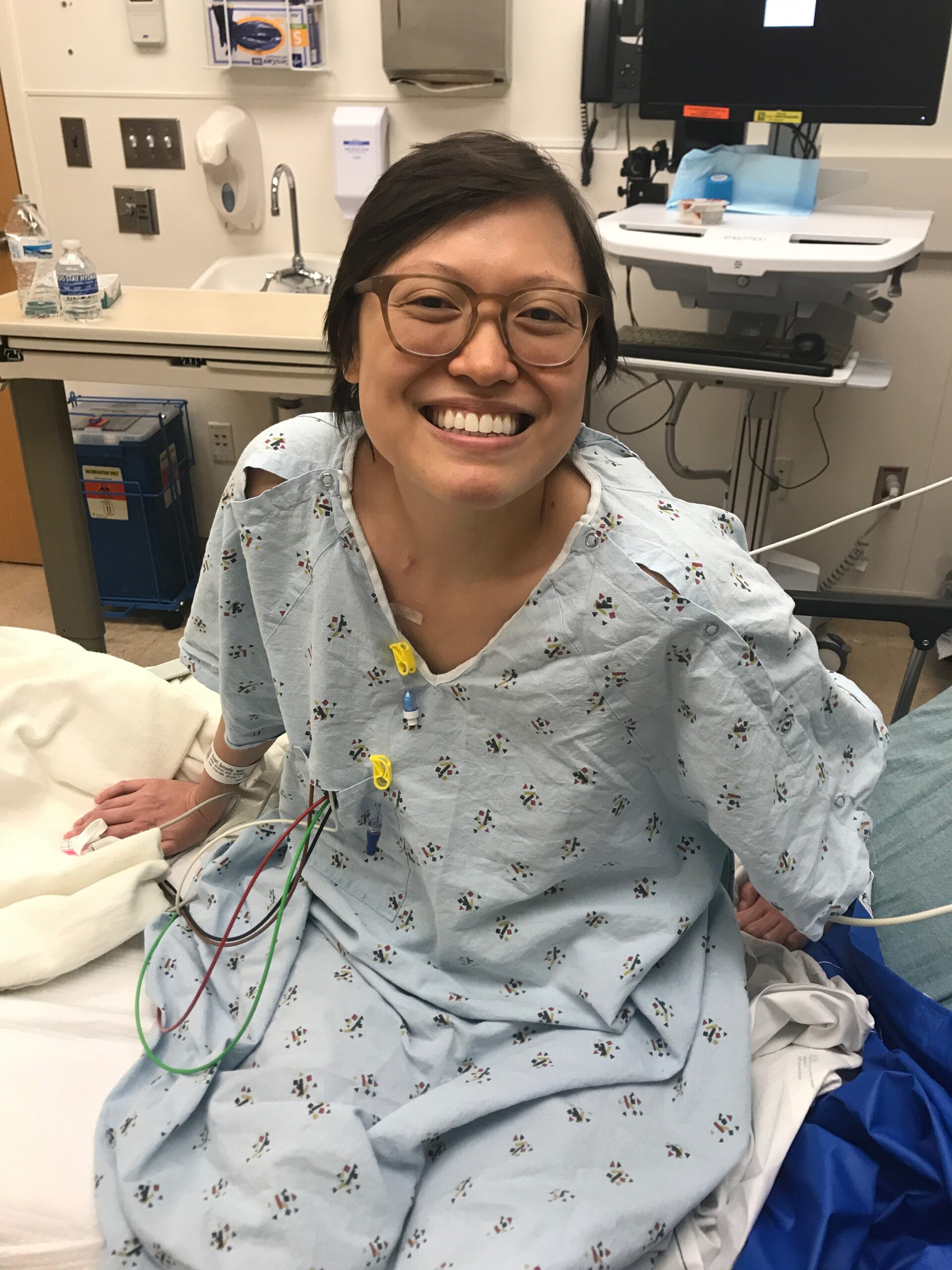
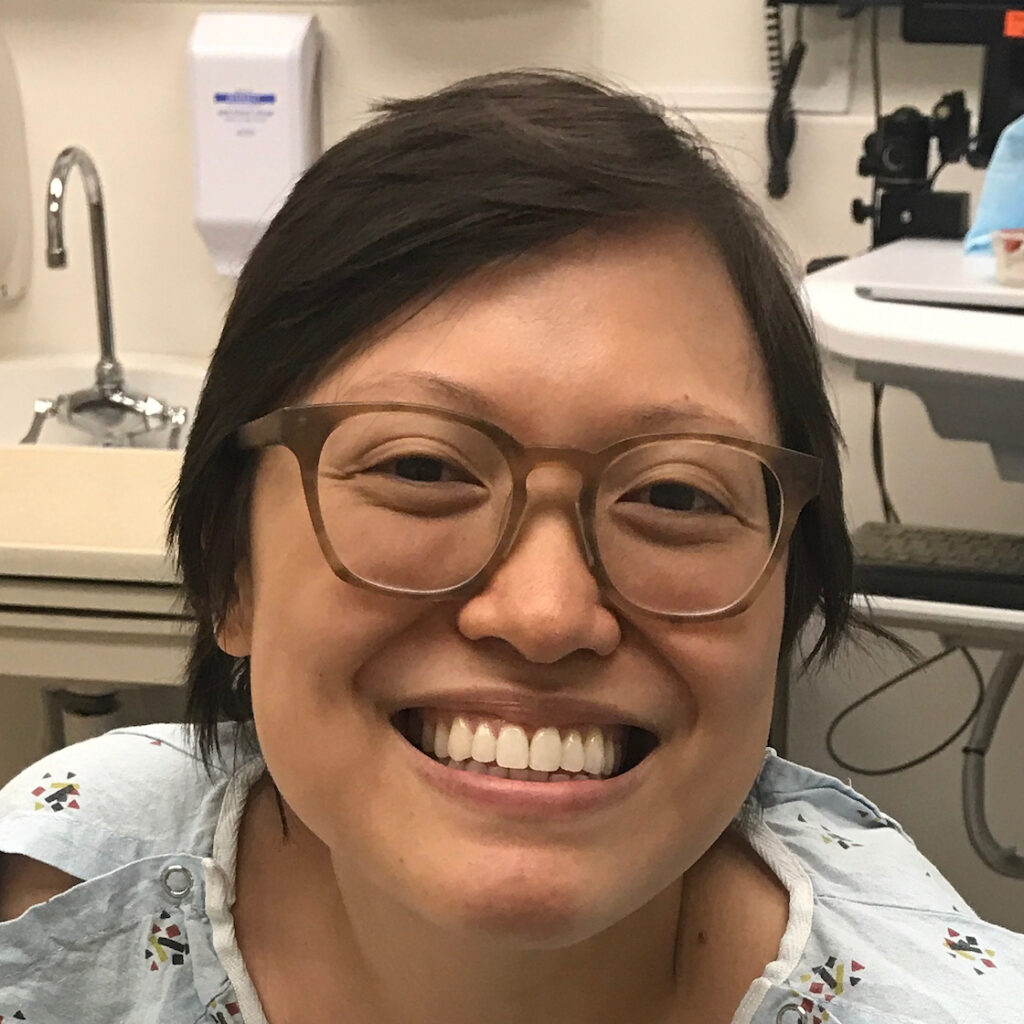
In March 2020, Samantha faced another recurrence. This time, the cancer had significantly affected her intestines and surrounding organs. Despite being told by one oncologist that nothing more could be done, she sought treatment in Los Angeles. There, she underwent a pelvic exenteration, extensive surgery that removed all organs in the pelvis. The procedure gave her a 50/50 chance of survival, and after two and a half months in LA, she finally entered remission.
Samantha emphasizes that the mental health impact of cancer is often overlooked. The trauma of her experiences left her with PTSD, anxiety, and a constant fear of recurrence. She credits her mental health recovery to therapy and self-compassion, acknowledging that healing from the emotional scars of cancer is a long and ongoing process.
Samantha advises those facing similar challenges to advocate for themselves, seek second opinions, and connect with support communities. She highlights the importance of accessing social workers and other resources available through healthcare facilities. For those without insurance, she recommends seeking help from nonprofits that offer mental health support and community-building opportunities. Above all, she encourages people to offer themselves grace and compassion, recognizing that they are doing the best they can in difficult circumstances.
Samantha’s story is one of resilience, self-advocacy, and the power of community. She has learned to navigate the complex and often frustrating healthcare system and now dedicates herself to helping others do the same.
- Name:
- Samantha R.
- Diagnosis:
- Early stage cervical cancer, adenocarcinoma
- Initial Symptoms:
- Irregular bleeding
- Pain
- Treatment:
- Surgery: radical hysterectomy, pelvic exenteration surgery
- Chemotherapy
- Immunotherapy
- Radiation therapy
- Hormone replacement therapy
- Hyperbaric oxygen therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Inspired by Samantha's story?
Share your story, too!
Related Cancer Stories
More Cervical Cancer Stories
Willow B., Pelvic Cancer, Grade 1, Stage 2.5
Symptoms: Persistent fever-like chills, scratchy throat, fatigue, post-orgasm pain, heavy bleeding, severe cramping
Treatments: Surgery (radical hysterectomy), radiation, chemotherapy, hormone replacement therapy (HRT)
...
Samantha R., Adenocarcinoma Cervical Cancer, Early Stage
Symptoms: Irregular bleeding, pain
Treatments: Surgery (radical hysterectomy, pelvic exenteration), chemotherapy, immunotherapy, radiation therapy, hormone replacement therapy, hyperbaric oxygen therapy
...
Amanda L., Cervical Cancer, Stage 3
Symptoms: Heavy periods, abnormal bleeding, large blood clots, severe cramping, severe abdominal pain, pain radiating down the left leg, loss of mobility in the left leg, loss of appetite, fatigue
Treatments: Chemotherapy, radiation therapy (external beam radiation therapy & brachytherapy)
...
Mila L., Squamous Cell Cervical Cancer, Stage 1B1
Symptoms: Abnormal lump in cervix area, bleeding after sex
Treatments: Chemotherapy (cisplatin), radiation, adjuvant chemotherapy (carboplatin & paclitaxel
...
McKenzie E., Cervical Cancer, Stage 3C2
Symptoms: Severe abdominal & back cramping, persistent & extreme pain, heavy discharge & bleeding
Treatments: Radiation, chemotherapy (cisplatin), brachytherapy, immunotherapy (Keytruda)
...
Marissa N., Squamous Cell Cervical Cancer, Stage 3B
Symptom: Excessive and prolonged vaginal bleeding
Treatments: Chemotherapy (cisplatin), radiation, brachytherapy
...
Alicia P., Bile Duct Cancer (Cholangiocarcinoma), Stage 4 (Metastatic)
Symptoms: Bleeding for a month, passing large clots of blood, severe pain in lower back
Treatments: Chemotherapy, radiation therapy
...
Leanne B., Cervical Cancer, Stage 4
Symptoms: Fatigue, irregular periods, pain after sex
Treatments: Radiotherapy, brachytherapy, chemotherapy (carboplatin & paclitaxel)/p>
...
Kristine M., Adenocarcinoma Cervical Cancer, Stage 2B
Symptom: Tumor found during postpartum pap smear
Treatments: Colposcopy with endocervical curettage, cone biopsy, total abdominal radical open hysterectomy with lymph node removal
...