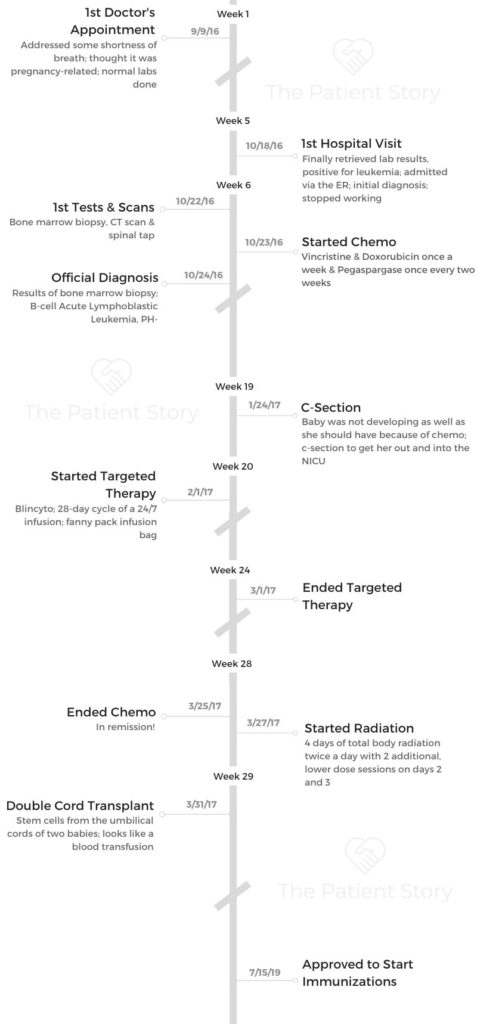
Veronica’s Refractory Ph- B-Cell Acute Lymphoblastic Leukemia Story
Veronica was diagnosed with B-cell acute lymphoblastic leukemia (ALL), Philadelphia chromosome-negative, all while pregnant with her baby. Thankfully, she was able to deliver a healthy baby girl!
In her story, she shares the experience of navigating chemo, surgery, and a double cord transplant. She also highlights quality of life issues like being her own advocate, dealing with financial toxicity, and how the leukemia diagnosis impacted her relationships, including marriage. Thanks for sharing your story, Veronica!

- Name: Veronica B.
- Diagnosis:
- Acute lymphoblastic leukemia (ALL)
- B-cell
- Ph- (Philadelphia chromosome-negative)
- Refractory
- Staging: N/A
- 1st Symptoms:
- Mild shortness of breath
- Palpitations
- Treatment:
- Chemotherapy:
- Vincristine & doxorubicin
- Infused once a week for 18 weeks
- Pegaspargase
- Infused once every other week for 9 weeks
- Intrathecal (spinal) cytarabine
- Vincristine & doxorubicin
- Targeted agent:
- Blincyto (blinatumomab)
- 28-day cycle infused 24/7 for the duration
- Blincyto (blinatumomab)
- Surgery:
- C-section
- Double cord transplant
- Chemotherapy:
It’s okay to not be okay. Take each day one day at a time. You’re going to have good and bad days.
It’s okay to experience emotions. Just don’t let those negative feelings consume you.
Take the time to accept and grieve your diagnosis, but at the same time, try to keep moving.
Veronica B.
- Diagnosis
- What were your first symptoms?
- How did you find out about the cancer?
- Waiting for answers
- Processing the diagnosis
- How did you tell your loved ones about the diagnosis?
- What happened when you got to the ER?
- What was the bone marrow biopsy like?
- Figuring out treatment around the pregnancy
- How were you feeling when they said you had to terminate your pregnancy?
- Chemotherapy and C-Section
- Transplant
- What was the process of getting into remission and preparing for transplant?
- Why was an autologous stem cell transplant not an option?
- Learning more about the double cord transplant
- Radiation before the transplant
- Describe the actual double cord transplant
- How was the recovery from the transplant?
- Describe the side effects after transplant
- Quality of Life
- Mental and Physical Support
- What was the lowest point for you mentally and emotionally?
- What got you through the lowest points?
- How important was it for you to have caregivers and a support system?
- What were some ways family and friends supported you?
- It can be hard to ask for help. How did you do it?
- Being your own advocate
- Can you talk more about the housing program?
- Dealing with the financial toxicity of cancer treatment
- Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Diagnosis
What were your first symptoms?
I didn’t really have any. The only symptoms that started to present themselves after I found out I was pregnant was a little shortness of breath and some palpitations. I addressed that during my first prenatal appointment, and they told me that was completely normal with pregnancy.
How did you find out about the cancer?
I went to the doctor for that first visit, did my normal labs, and went back to work. I work in the medical field, so when I didn’t hear back from them for 3 weeks, I thought for sure everything was normal.
I thought no news was good news.
At just about that 3-week mark, I got a call from the doctor’s office stating that they wanted me to repeat my labs. I asked them if I should be concerned about anything, and they said no. They just wanted me to repeat them.
I went in and repeated the labs. I noticed that they were slightly different than the labs I had originally done, but they said it was nothing to worry about.
Waiting for answers
I didn’t hear from them again for another few weeks. I figured nothing was wrong. About 3 weeks later, I got another call asking me to repeat one more set of labs again.
At that point, I was starting to get really concerned. I asked her if I should be, and she said no. I left work, and I went to go pick up the lab slip at the office. I demanded to speak to somebody because no one was telling me anything.
The front desk lady went to talk to someone, came back, and said I just needed to do the labs and hopefully I’d hear something the next day. The lab tech who was back there with me told me I wouldn’t actually get my results for another 3 to 4 days. I went back to work super nervous.
I called human resources to get my own labs back so I could see what was going on. A couple of days went by, and I followed up with them again. They kept telling me that my labs weren’t in yet. I kept calling and calling.
Finally, I was in the middle of a midterm when I checked my email and saw my lab results. It was a leukemia test that I had tested positive for.
I was in tears, and I left class. I called my doctor’s office, and they said they still didn’t have my results. I said, ‘No, I have my lab results. I need to speak to somebody right now.’
The girl asked me how I had my results, and I told her since nobody was telling me anything, I got my own medical records. She put me on hold, and about 20 minutes later, a nurse practitioner got on the line.
She said they had been reviewing my labs over the last month and hadn’t wanted to scare if there was nothing to worry about.
She also said she had forwarded my medical records to Stanford, and I needed to wait for them to call me back. Then my OB called me a few days later and said she spoke with the director of oncology at Stanford, and they wanted me to go to the ER to be admitted.
»MORE: How to be a self-advocate as a patient
Processing the diagnosis
I was afraid. I was pregnant with my first baby. I was so scared. My mom passed away from stage 4 colon cancer in 2011, so I was just really afraid. I didn’t know what to do.
»MORE: Patients share how they processed a cancer diagnosis
How did you tell your loved ones about the diagnosis?
I immediately called my husband. I had not felt well that day, so I had my husband drive me to class. When I saw the email, I called him. He came and picked me up. We sat in the car, and I told him what I found out.
He read it himself, and we both cried. He’s a nurse in the emergency department where we live, so he knew right away what was going on.
We drove home, and I talked to my employer. We told them the news, and we took care of all of that. We went to HR and told them I was going to be on leave.
While I was at home waiting to hear from Stanford, I went ahead and made those phone calls to friends and family.
That was really hard because just a few weeks earlier, we had been trying to figure out ways to tell them I was pregnant. She’s the first grandchild on both sides, so we were trying to come up with a creative way to tell everyone.
Now, we were trying to figure out how to not only tell them I was pregnant but also that I had cancer. It was hard. We were breaking it to them easy.
We started with the good news, ‘You’re gonna be an aunt,’ or ‘You’re gonna be an uncle, but I also have cancer, so this is what’s going on.’
We called close family and friends first. Then, after I started treatment, my husband sent out a long post on Facebook to other friends and family who don’t live here or who we aren’t as close to.

»MORE: Breaking the news of a diagnosis to loved ones
What happened when you got to the ER?
Upon getting there, they asked me what my symptoms were and how I knew my diagnosis. Apparently, my records hadn’t been sent over to them yet. Thankfully, I had my own medical records on my email and could forward them to them from my cell phone while there in the hospital.
They were really crowded when I got there, so I spent the night in the ER. The next morning, they transferred me to a different unit with a bed before finally transferring me to the oncology unit a few hours later.

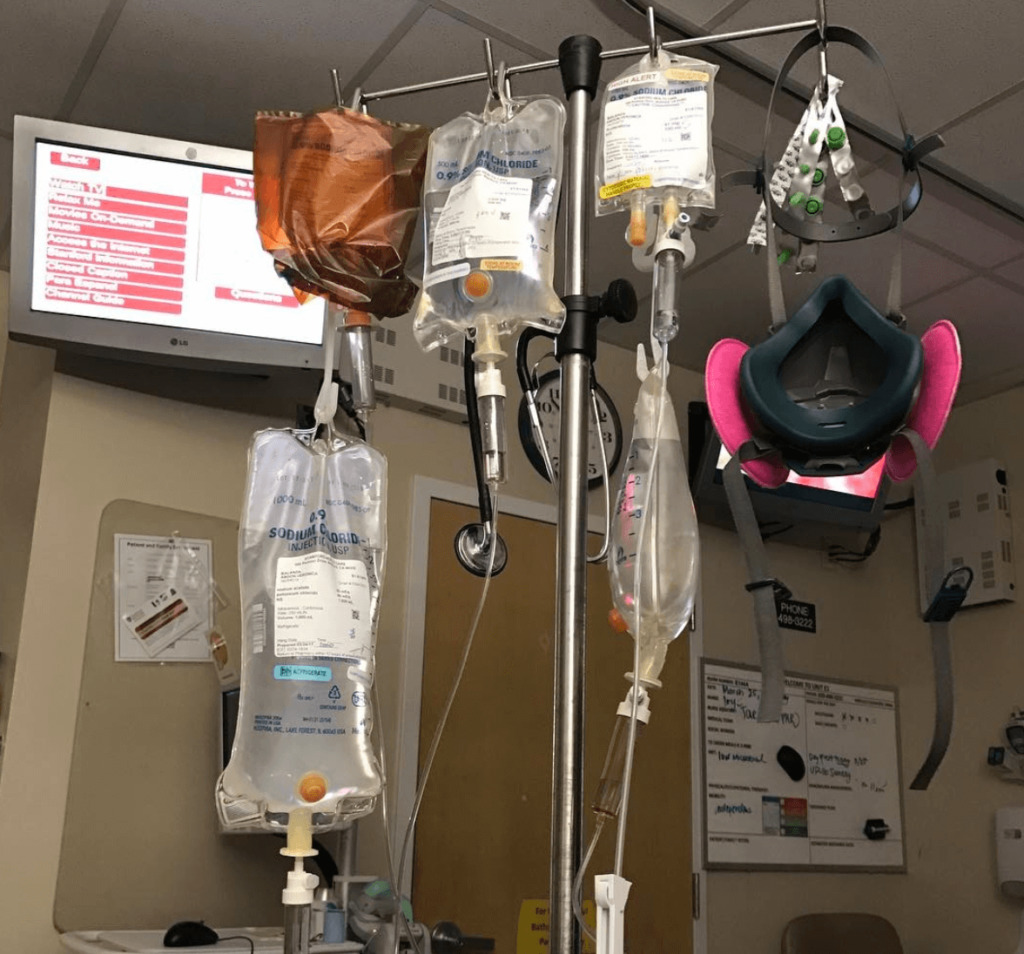
Once I was admitted, they had all kinds of specialists come and meet with me and discuss next steps with me. From that point, I had a bone marrow biopsy, a bunch of labs, a PICC line, and started chemotherapy.
What was the bone marrow biopsy like?
It’s a little intimidating. I was just more or less glad that they were getting the ball rolling, though. One of the oncology residents came in with a group of interns.
They numbed the area with lidocaine. They drilled a small hole in my lower back bone to get some bone marrow. It’s not super painful, but it’s hard to describe exactly what it feels like.
It’s pressure when they’re drilling the hole to obtain the sample. It’s feels really weird when they’re aspirating and taking the bone marrow out. I felt like they [opening a] wine bottle or something. I wouldn’t look forward to it, but it had to be done.
Figuring out treatment around the pregnancy
After the bone marrow biopsy, I was scheduled to have my PICC line put in. After that, they brought in all my teams. Not only did I have leukemia, but I was also pregnant, so I spoke with my high-risk OB team.
Originally, they had told me I needed to terminate to better my options, but I didn’t want to do that.
My oncology and OB team worked together to come up with a plan. They discussed everything with me, and then we started treatment the next day.
How were you feeling when they said you had to terminate your pregnancy?
That was scarier than finding out I had cancer. We had tried and planned for her. They told me in the ER upon arrival that that was going to be necessary in order to start treatment.
Right after that conversation, they wheeled me up to get an ultrasound and look at the baby. They weren’t really giving me answers. I guess they wanted to see how far along I was.
The technician told me she couldn’t give me my results and read the scan for me, but she said she could see that I was scared. She said that what she could tell me was that everything looked good from what she could see. She told me she just couldn’t give me an official reading.

Knowing that, it’s hard to think that they wanted me to terminate. I told my oncologist that I wanted to keep the baby, and she talked to my OB team. They assessed the risk, and the main things to watch for were small birth weight and stillbirth.
We already knew that she would be born small because they planned on inducing me at 33 weeks to prepare for my transplant, and the risks were worth it to us to have her.
We just went ahead and did it, and once that’s what we decided, my medical team was fully supportive.
Chemotherapy and C-Section
Getting a PICC line
That was actually not that bad. It’s very intimidating. It’s like a glorified IV. It was less painful than getting an IV, I think. It was really fast and efficient.
»MORE: Read patient PICC line experiences
What was your chemo regimen like?
I was on vincristine, doxorubicin, and pegaspargase. It was not too bad. Every other Sunday, I had pegaspargase. Vincristine and doxorubicin were every Sunday.
Describe the chemo side effects
From what I remember, it wasn’t too bad. I expected so many side effects. I watched my mom go through chemo, and everything that could’ve gone wrong in her situation did.
That’s what I was expecting for me, but it really wasn’t that bad. I didn’t experience that many side effects.
When I started getting intrathecal cytarabine every so often, I would get nauseous. I did experience neuropathy with vincristine, but for the most part, I was okay. I tried to stay proactive and active. I would go for walks around the hospital floor when I was allowed.
I would wake up every morning before rounds started at 6 a.m. to take a shower and make sure I was presentable for everybody.
As far as the chemo itself, it wasn’t too bad. The prednisone was actually worse. I got swelling, insomnia, achy joints, and I had a hunchback.
You had to be induced mid-chemotherapy
My counts were going down but not fast enough. They started calling my cancer refractory. What they did was they had me repeat the induction period. I was halfway done with that when they noticed my baby wasn’t growing like she should’ve been.
They told me that it was probably due to placental insufficiency due to the illness. I stopped the induction phase midway through, and that’s when they induced me at 26 weeks.
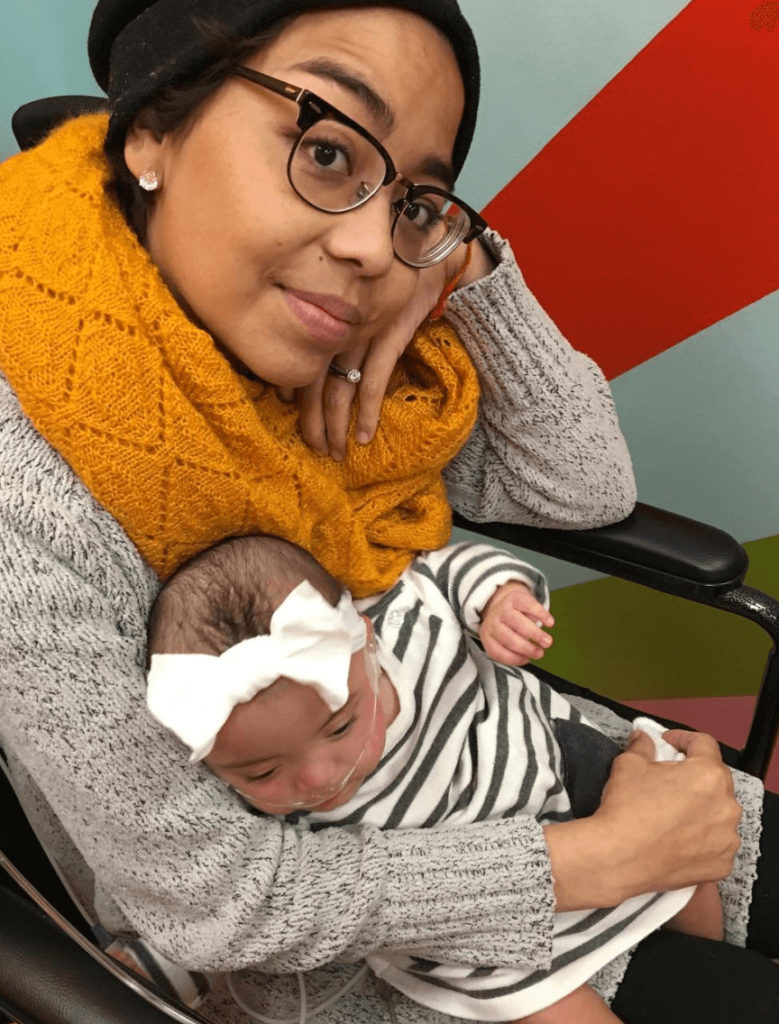
I had mentally prepared myself for that when we had all these conversations at the beginning. I felt like if she was meant not to be here, she wouldn’t be here. I tried to keep a positive mindset, though, and I was happy that she was here. It wasn’t easy to see her all hooked up like that, but I loved seeing her.

It was horrible that she was born so early, of course, but it turned out to be a good thing. I had met with my hematologist beforehand.
Since my blasts were not decreasing as fast as I wanted, the next plan was going to be Blincyto, which had never been tested on a pregnant person before.
She thought the drug would ultimately get me in remission, and so a week later, they gave me a C-section. I had a week to recover, and we started chemo again.
What was the Blincyto like?
It’s a 28-day cycle, and it’s a continuous thing. I had a fanny pack that was connected to me for 24 hours a day. When the bags would run out, I changed them.
I did that for 28 days, and that’s what ultimately got me into remission.

Recovering after the chemo
I had to stay in the hospital for 4 to 5 days to be monitored, but then I got to go home and continue the regimen on my own. My daughter was still in the NICU, but I was there with my fanny pack all the time.
Transplant
What was the process of getting into remission and preparing for transplant?
They did a bone marrow biopsy right after I finished the Blincyto. After that, I did a CT scan, and they made sure there was nothing else in my body before I could move forward with the transplant.
I did more intrathecal chemo, spinal taps, lots of labs, and everything. My biopsy came back with no residual disease. I was in remission at that point.
I was excited, but I was also nervous. They were testing all my siblings for a match because I didn’t have any matches in the registry.
None of my siblings were a match, so they decided on a double cord transplant for me. It’s where they take the stem cells from the umbilical cords from 2 babies. They were a better match for me than my 50% match sibling.
Why was an autologous stem cell transplant not an option?
They didn’t want to risk waiting on the retrieval process and the precautions I would have to take beforehand.
They figured the best option to keep me in remission would be a transplant, so they wanted to get it going quickly.
Learning more about the double cord transplant
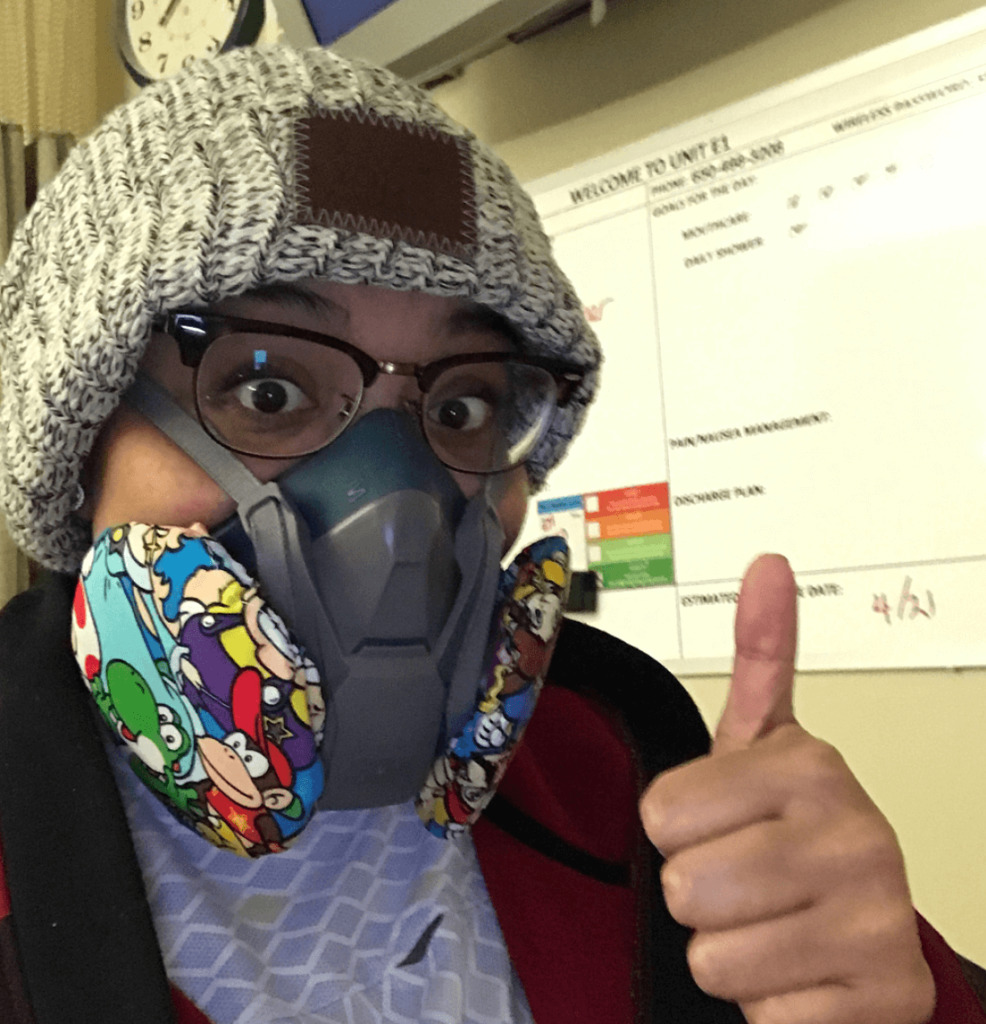
I was admitted on day 7 into the hospital. I had 3 days of intense chemotherapy, followed by a break for one day, and then I had full body radiation twice a day for 4 days.
I had reached out to a girl on Instagram when I was first diagnosed. She had her transplant at Stanford, too. We immediately became good friends. She was my resource when I was going through the process. Google isn’t really your best friend, so it was nice to talk to her.
Radiation before the transplant
She had one day of radiation therapy, and she told me it was the worst part for her. I had 4 days, so hearing that was kind of scary for me. I was afraid. I didn’t know what to expect, but it really wasn’t that bad.
I didn’t feel anything during the radiation. I was tired afterwards, but during the actual event, I didn’t have any pain or anything. My anxiety did spike up a little while it was happening just because it was a dark room, and I couldn’t move.
Reality slapped me in the face. That was an emotional part for me, but the radiation itself wasn’t bad.
Describe the actual double cord transplant
The actual transplant was actually very uneventful. It was a big deal going into it because when you read the pamphlet, you’re ingesting all this information, but the transplant itself was very anticlimactic.
It felt like just another blood transfusion. It looked like one, too. It didn’t take very long. It was a very very uneventful day.
How was the recovery from the transplant?
With cord cells, the time it takes to engraft is longer than with a standard bone marrow transplant. I was in the hospital for 2 months before I started to engraft.
Describe the side effects after transplant
I experienced some mucositis about a week after the transplant. I’m not sure if it was from the chemo or what. I had nausea and fatigue. I also broke out in a full body rash.
It wasn’t itchy or uncomfortable at all, but it looked horrible. It was from head to toe and even in my eyes. They weren’t sure if it was graft vs. host (GVHD) or an allergic reaction.
»MORE: Explore more on GvHD and what to expect from a medical expert
I met with a dermatology team and did skin biopsies. Those were inconclusive. They changed the antibiotics I was on, and they gave me lotions just in case it was graft vs. host. They weren’t really sure what caused it. It was a pretty wicked rash.
After I started engrafting, I continued to have minor skin issues. I had some itching, or I’d get a rash every once in a while. To this day, I still get them sometimes on my ankles or inner arms.
I had a cough for several months after the transplant. They did a bunch of tests, and they said it might have been allergies or asthma that I developed as a result of the transplant.
After that, I had some loss of appetite. They said it was normal, but I couldn’t eat anything for almost 4 months. My starting weight pre-pregnancy was 130. I went up to 168 on steroids while pregnant.
After that period of time where I couldn’t eat, I dropped to about 80 pounds. I had to go into the clinic every week or so for hydration.
They had prescribed me Marinol and other anti-nausea drugs. None of it helped. I was living on sips of water.
That was the worst part, and it went on for a few months. Eventually, my appetite came back, but it was a big issue.

Quality of Life
What is your monitoring schedule like now?
It went from daily to a couple of times a week, and so on. Now we’ve trickled down to once every 3 months. Once every 3 months, I go in and get labs to ensure that I’m still in remission. They do regular labs, and then they do some special labs that come in a kit. It’s a test that detects small amounts of cancer in your blood.
Do you ever experience “scanxiety“?
I don’t think you ever get used to getting scans or tests or anything. Any and every day sometimes, I’m nervous about it. If I’m not feeling well or if I have an ache, I freak out.
If I have a bruise, I drive myself crazy trying to figure out where it might’ve come from. The anxiety is something that has never gone away.
Anything can trigger the fear of relapse. Every single day. I can’t let it consume me, but I definitely have my fears.
»MORE: Dealing with scanxiety and waiting for results
Was there talk about fertility after chemotherapy?
I’ve talked to 2 gynecologists since because my last period was after my transplant. I had one period right on time, but I haven’t had one since.
They’re saying I’m probably post-menopause by now. More than likely, I won’t be able to have more children because of all the chemo and radiation I went through.

They have said that they’re not 100% sure because I’m so young. They said there’s a chance it could come back, but more than likely, it won’t.
They told me to wait at least 2 years. If everything stays the same after that and I still want more kids, meeting with the fertility specialist would be my next step. They want to give my body time to heal first, though.
»MORE: Fertility preservation and cancer treatment
Did you lose your hair?
I did lose a lot of my hair during chemo. It fell out a lot, but I didn’t lose all of it. It was really thin. You could see patches of my scalp.
I looked like a character from “Lord of the Rings.” Knowing I was about to start radiation, I knew it was all going to come out.
The day before my transplant, I had my husband go ahead and do it in the hospital. I was ready to do it. It was the one thing I felt like I could control, so we did it.
I’m glad I did because within 4 days after the transplant, the follicles of every other hair I had anywhere on my body fell out.
It was liberating to shave it. I wasn’t as attached to it as some people might be. Hair can be a huge thing, but for me, the most important thing at that point was and still is my daughter.
If hair loss was part of the cycle, I was ready for it. I wasn’t as emotional about my hair as I thought I would be.
I used to cry when I asked for a trim and got more off than I expected. This time around, it wasn’t as big of a deal.
It was more liberating than anything.
It was more depressing for me to wake up with hair on my pillow than for me to just go ahead and get rid of it.
»MORE: Dealing with hair loss during cancer treatment
Do you have any advice for someone who’s about to lose their hair?
If anything, I would say if you can handle it, go ahead and shave it. It’s the one thing you can control. When you’re thrown into the cancer world, you usually just have to go through with what the doctors tell you is best, but you can decide when and how to lose your hair.
Knowing that hair loss is a potential circumstance, if you want some control, go ahead and shave it.
Mental and Physical Support
What was the lowest point for you mentally and emotionally?
When my daughter was finally home and I couldn’t eat after the transplant. I felt like I was fading away. I couldn’t even take care of her. I was doing my best to get better. When she was finally allowed to be home, I felt like I didn’t get to enjoy it.
I was robbed of so many moments. I didn’t get the baby shower. I didn’t get a maternity shoot. I didn’t get to spend time with her as a newborn.
She was in the NICU a lot for that first year, and when she was home, I didn’t get to spend much time with her. I had to stay with family a lot. I was pretty much just walking bones. I had to spend a large amount of time in bed or with my head in a bucket. There was a point where it all felt never-ending.
I didn’t think I was ever going to get better. I couldn’t eat. I couldn’t sleep. Lying in bed was uncomfortable. I really didn’t think I was gonna get better, and that was really low, but I had to keep on trying for my kid.

What got you through the lowest points?
As hard as it was, my daughter kept me going. I was there physically, but I couldn’t spend real time with her other than lying on the floor with her. She was still such a good kid.
Kids cry, and kids do all these things, but surprisingly she just laid there with me happily even though she had her own little issues. She kept me going through it all.
How important was it for you to have caregivers and a support system?
It’s so incredibly important. I couldn’t have done this without them. You definitely need someone there to support you. There was a point where I could barely get up.
They had to help me get in and out of the shower, which is something I never thought I would get help with. I’m a very independent person.
They played a very important role for me. I know some people might not have a situation like mine. Thankfully, I have a very supportive family.
Between my family and my husband’s family, they helped me through a lot. There were some days where my in-laws were the ones watching my daughter while I was unable to do anything.
It would’ve been impossible to do this without them.
What were some ways family and friends supported you?
In addition to being there to physically help us, they were also very understanding and reassuring. They understood the situation. I would apologize for not being able to help, and they would tell me not to apologize and that they would always be there to help.
We had a ton of people come over and prepare food for us, bring us food, or give us a Doordash card or something. Even if they couldn’t physically be there, someone would call or message daily. Those that were nearby would ask if they could come spend time with us, take care of my daughter, or cook a meal.
They went above and beyond for us. I had people offering to take me to and from doctor visits if I needed them to. People would drive down just to go sit with our daughter while she was in the NICU, and I would get to FaceTime and see her.
Our employer started a GoFundMe for us. That was helpful because it wasn’t just my stuff but her medical bills, too.
»MORE: What kind of support cancer patients say helped the most
It can be hard to ask for help. How did you do it?
I just had to accept that I needed the help. Having to do that was something that I never thought I was going to need to do. With how sick I was, though, there’s just no way I could’ve done it on my own, and I just had to accept that.
I couldn’t even stand or shower by myself for more than minutes. You just have to push pride aside and ask for help because it’s something you need.
Being your own advocate
Nobody knows your body like you do. You have to speak up when something doesn’t feel right or you’re uncomfortable. You just have to learn how to speak up.
Doctors are human. They’re not always right. If you feel like there’s something else that could be done or something isn’t right, say something. A good doctor will listen.
Jot things down before an appointment so you don’t have to wonder if you’ll remember them in the moment. Bring a friend or family member who is more bold and willing to ask questions on your behalf. One way or another, you or someone you love needs to stand up for you.
Social workers are a great resource, too. They always were helpful for us. They’re good at coordinating things for you. They helped arrange our housing situation, too. I didn’t know that was covered for us through insurance, and they were the ones that told us about that.
They are so resourceful. They can help you better understand and navigate the medical system, especially in terms of insurance and support and things like that.
»MORE: How to be a self-advocate as a patient

Can you talk more about the housing program?
I didn’t know that there was a Ronald McDonald house and other facilities for my daughter’s situation so I didn’t have to go home and then drive back every day to see her. They had units at the hospital that were available, and you just had to talk to a social worker about it.
If you have a family member in the hospital, they have a unit that might be available for you. The Ronald McDonald house was free to stay near the hospital as well.
With my transplant, they required that I stayed within 30 minutes of the hospital while I recovered just in case I had any complications. I didn’t have anyone in that area to stay with, so they put me up in an apartment complex that worked with the hospital. It was income-based, but most insurance companies cover that, too.
We paid daily to stay there for 3 months, but we got all of it back once we submitted the invoices to the insurance company.
Dealing with the financial toxicity of cancer treatment
It’s been hard with me not working especially. There is always a way, though. You can qualify for disability after being diagnosed with leukemia and being out of work. That would definitely help.
It’s an automatic qualification. That helped. The deductible is still ridiculous every year, but there are ways to alleviate it. We’re here, so we just deal with the financial stuff as we can.

Reflections
How did cancer affect the relationship with your husband?
It made us stronger.
We’ve been through some tough stuff, but this was really hard. The hospital I was going to was 4 hours away from our home. When I was diagnosed, he took his leave and stayed with me for the first few weeks of treatment, but then he had to come back.
It was kind of wonderful because he and I both work for the same hospital, and a lot of people donated their own vacation time to extend our leave. Our job has been wonderful throughout this.
It was hard on him, and they really helped us because he had mixed feelings. He wanted to be there for me, but he also wanted to save some time for when our daughter was born because she was going to need him, too.
The majority of the time I was in treatment, he would have to travel 4 hours each way, either taking Amtrak or driving just to go back. There were days he would leave right after work, come see me for a day or 2, and then drive right back.
We spent a lot of time on the phone with one another, too. It really did make our relationship stronger, though.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
Advice for other couples going through cancer
You just have to learn to get through things together. It’s hard. You need each other. You just have to work together and work one day at a time. Don’t get overwhelmed, and always lean on each other. It’s hard, but it easier together.
How has cancer affected your relationship with your daughter?
It just makes each moment with her special, regardless of whether I could take care of her or not physically. I didn’t feel like I could take care of her, but I was there for her. Like I said, I laid on the floor with her and tried to soak up as much time with her as I could.
I never take a day for granted. Every day is a reminder of how lucky we are to both be here. When I see pictures or have flashbacks, it’s just crazy to think of how far we’ve come. It makes me truly value each and every day.
How has cancer changed your life perspective?
I accept the way that things are now. There are things I used to be able to do that I can’t do now. I want to say that I never took life for granted, but it’s weird how much more you appreciate life after cancer.
I’m grateful for every single day that I wake up. Things could have been so much worse. This new normal may not be perfect, but I’ll take it all over death any day.

Advice for someone who has just been diagnosed
Being your own advocate is the most important thing.
When they told me that termination was my best option, I told them I wasn’t okay with that. They worked with me, and now she’s okay.
During that time, there were so many things I was told about my pregnancy, but I went with my gut. Sometimes, you just have to trust your instincts.
It’s okay to not be okay. Take each day one day at a time. You’re going to have good and bad days. It’s okay to experience emotions. Just don’t let those negative feelings consume you.
Take the time to accept and grieve your diagnosis, but at the same time, try to keep moving. Positivity is hard when you’ve just been diagnosed, especially if things aren’t going well or looking too good.
Things do get better, though, so try to take one day at a time and not get stuck in that sad, angry place.

Inspired by Veronica's story?
Share your story, too!
Acute Lymphoblastic Leukemia (ALL) Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)



