Evan’s Acute Lymphoblastic Leukemia Story
Evan was 32 years old when he was suddenly diagnosed with acute lymphoblastic leukemia (ALL) and forced to undergo chemotherapy (infusions and pills) and radiation.
In his story, Evan shares how he navigated life with cancer, including mentally and emotionally coping through a longer treatment and how he approached work during that time. Thanks for sharing your story, Evan!

- Name: Evan L.
- Diagnosis:
- Acute lymphoblastic leukemia (ALL)
- Age at Diagnosis: 32
- 1st Symptoms:
- Extreme fatigue
- Easily bruised
- Treatment:
- Chemotherapy infusions
- Chemotherapy pills
- Spinal taps
- Cranial radiation
- Diagnosis
- What were your first symptoms?
- What was your overall treatment plan?
- Describe the bone marrow biopsies
- How did you feel after the bone marrow biopsies?
- Describe the wait time after the biopsies
- Advice on how to deal with the wait time
- How did you decide where to go for treatment?
- Did you get a second opinion?
- Researching your diagnosis
- How many oncologists did you see?
- What was your experience at a larger hospital?
- Treatment and Side Effects
- Describe your first hospital stay
- Describe the PICC line
- What were the chemotherapy side effects?
- Describe the hair loss
- You chose to be outpatient after the first hospitalization
- How often did you have to get infusions after the hospital?
- When you switched to chemo pills, how many did you need to take?
- What were the side effects of chemo pills?
- Describe the spinal tap procedure
- Why did doctors decide to remove spinal fluid?
- Describe the cranial radiation
- Describe the process of the cranial radiation
- How often do you need follow-up appointments?
- Quality of Life
- What was the worst part of treatment?
- Coping with a longer cancer treatment
- How did you deal with the emotional and mental stress?
- Could you work through treatment?
- Paying for cancer treatment
- Did anyone help you navigate the decision-making?
- Did you have to advocate for yourself during treatment?
- Message to other patients
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
You will get through it. If you have friends and family around you, definitely lean on them. They will be there for you no matter what the case may be.
Just keep your head up. Stay positive. I think it’s very important that you know you will get through it. It’s just time. It’s just patience and protocol.
There are many great doctors and nurses out there that are on your side, and they’re going to get you through it. It does get better.
Evan L.
Diagnosis
What were your first symptoms?
I have a clothing business. At the end of the year, we were in the process of moving out of a local mall here in the Bay Area. We were going through the process of moving.
There was a lot of manual labor. I was feeling very fatigued and getting bruises here and there. I attributed that to the move.
I was feeling very weak. A couple weeks had passed. It had been the new year, and I was feeling very, very weak. My aunt actually saw me and suggested I go to the doctor and get some blood labs to see what was going on, because I looked very unwell.
I went through the process and didn’t think much of it. I figured this must be some type of illness, possibly mono, or something like that. We did the labs.
The very next day, they called me in the morning and pretty much said, ‘You have cancer, and we think it’s leukemia.’ At that point, freaking out, wasn’t quite sure what any of that was.
I had people around me that have gone through different cancers and things, but I didn’t really have a good understanding of what the different ones were and what this one was in particular.
What was your overall treatment plan?
That started this whole process of talking to my parents. We went in that morning to the hospital. I was pretty much there for the next month or so. Never left.
Went through bone marrow biopsies, chemo treatments, various different stages. We went through the different phases of addressing the cancer. Within that month, I believed when I left the hospital that the cancer was supposedly gone.
Pretty much from that point on, it’s been a remission and maintenance situation.
Theoretically, the cancer is no longer here, but it’s all part of the protocol in the sense of this is based on prior use cases.
Describe the bone marrow biopsies
I did 2 because there was the initial one, and then there was another one [to test for something] called the Philadelphia chromosome, which was some offshoot of what I had. If I were to have that, then my survival rate percentage would have been way lower.
It was pretty traumatic. I recall they take you in this room, and there’s this huge needle. They give you a numbing medication. It’ll feel like bee stings or something briefly. That numbs the area. Then they go in with a needle.

The purpose of it is to draw out material from your bone marrow. In my case, they went in my side, and it’s very painful. Not an enjoyable experience.
You feel a pressure. It’s not really a sharpness like you’re being cut. It’s more like a deep pressure because it’s deep inside. They administered morphine or some type of agent to make me feel better.
The process, which I went through twice, was about 20 minutes each time. They do what they had to do. Not a comfortable experience, but definitely something that needs to be done. [I’m] glad that worked out okay.
For me, I had some internal bleeding after. They really had to apply a lot more pressure because my bones were a little bit stronger than normal, [while] it’s easier to get in sometimes for some people. I think that was the reason for that, so there was a little bit of bruising that I experienced after.
How did you feel after the bone marrow biopsies?
It was an aching pain. It was a little tough because I was pretty much bedridden during that time, so I was experiencing other issues. Really being able to parse out that one specific discomfort, I don’t remember that well.
I think it was a soreness or aching. I get spinal taps once a quarter now, so it’s a similar feeling. It’s not as painful, but it’s a similar ache after. I would imagine that’s what it felt like after for the next week or 2.
Describe the wait time after the biopsies
The first bone marrow biopsy, I don’t remember a particular amount of stress for that waiting. I don’t think they told me what results they were looking for.
The second one we did was for the potential Philadelphia chromosome, which is an offshoot of acute lymphoblastic leukemia (ALL). If you have that variation, then it changes your whole treatment and whole situation.
That was a little more nerve-wracking because they had informed me what they were testing for this time, and it’ll determine the path you take moving forward.
That waiting period — a week or so, or maybe a few days — was a little bit more stressful because I knew specifically what they were looking for.
Advice on how to deal with the wait time
A huge takeaway for me with this whole situation is [that] stressing about the waiting is understandable, because you don’t know what’s going to happen [or] what the next stage is. There’s so many variables and so many unknowns.
A lot of it is about just letting go and not being as stressed about it because there’s literally nothing you can do.
The only thing you can do wrong is not take your medicine properly or not do what the nurses and doctors tell you. As long as you do what you’re supposed to do, there’s really nothing else that I can do.
I think in a way, that almost made me more comfortable because if this is going to happen, it’s going to happen anyways. There’s really nothing I can do.
Don’t stress yourself out. From what I understand, if you’re always super stressed, super nervous all the time, that can’t be good for your recovery.
I was fairly relaxed through the whole thing because of that fact that I knew that there’s nothing really I could do. I felt bad, but you’re in that situation. You have to get through that till you get to the next part of it.
It’s completely understandable for people to be stressed out and people to be nervous about their results, particularly if it’s like in the case of the Philadelphia chromosome situation, where you’re waiting for a specific thing to come back. It’s one of those things I would say the more relaxed you are, the better the outcome will be.
»More: Coping with scanxiety →
How did you decide where to go for treatment?
My primary care doctor is at Kaiser. I believe when they asked me to come in, they asked me to go to the South San Francisco Kaiser, probably because it was the closest center to where my primary care physician was, and [it was] somewhere that had the oncology department.
I met my doctor. She was awesome. I had no reason to go anywhere else. She’s been great ever since. I didn’t think twice about where I might be going. I was already within the Kaiser community.
That does come up. I want to make sure I’m going to the best treatment center.
I have a family member that’s a doctor at Kaiser, so by default I’m comfortable with that hospital. There’s different medical professionals in my family that I lean on for information regarding that stuff. I think if they had anything pertinent to say about that, they would probably let me know. I had that, thankfully. I know other people don’t necessarily have the resource.

I just felt comfortable with the people. The nurses were very attentive, very good. My doctor was really great and has been really great. I had no reason to question the treatment that I was getting. But I can definitely understand how people might want to look at the different options and see what different stuff is out there.
Did you get a second opinion?
The only time a second opinion came up was during one part of my treatment, cranial radiation. I had to get a certain amount of sessions of cranial radiation to potentially kill off any cancer cells that had grown within my brain stem area. I believe that was optional. I didn’t necessarily have to get the radiation if I didn’t want it.
There were disclaimers about, “You could lose some of your memory, short-term memory. You could have other issues, headaches, things of that nature.” It was something that was not required but highly recommended.
I did get some second opinions from different doctors on what they thought about it. Risk versus reward, what percentages of different things.
That was probably the only part of the treatment I remember particularly getting varying opinions separate from what the options were that were laid out for me.
Researching your diagnosis
In this day and age of Google, everyone should do their due diligence for whatever they’re doing.
You want to have more information rather than less. If you have people around you that can help you with that, it’s very helpful. I was not going to sit from my hospital bed Googling all this stuff.
I’m sick. I feel horrible. I’m weak. I’m tired. I don’t want to be going through this stuff. Thankfully, there are people that can help me with this.
If you do have people like that available to you, definitely take advantage. Lean on those people to help you make the best decisions for your treatment.
Other than that, as much as you’re able to do, you could do it on your own and talk to other people that might have other ideas. There are so many people out there.
I learned this through having gone through this. Naturally, people will start messaging you on Facebook or whatever, “Hey I have a friend that has cancer. This person just went through this.”
Everybody knows people that are either going through some type of cancer or have been through something. There’s a lot of good advice just from talking to different people that might be in your life that you don’t even know have been through something similar, so they might have different advice as well.
How many oncologists did you see?
I’ve only used one oncologist. I would only be seen by anyone else if she was not available or if she was gone or something. Other than that, my treatment would be through the oncology nurses.
I would get chemo infusions. Specialists like in radiology and in different areas, like an MRI. There are special technicians and things.
In terms of the day-to-day protocol, the treatment as it pertains to the cancer, it was all through the one doctor.

What was your experience at a larger hospital?
There’s nothing that I really disliked about it. It’s hard because I have nothing to compare it to. I had nothing to really complain about.
I think because there’s a certain understanding [that] this is a large company, [so there are] probably many similar patients dealing with many similar things to me. When you keep that in mind, you have an understanding of, “I’m probably going to get this level of attention or this level of care.”
Bearing that in mind, nothing stood out as I’m being neglected or I’m being overly cared for or anything. I think it was a good balance of the attention I was getting while I was in the hospital for different things.
I was very satisfied and [am] currently satisfied with the treatment that’s been going on. With a smaller group, I don’t know if the protocols are different or anything. Because you’re dealing with [fewer] people, maybe there are fewer nurses or different places you need to go for things.
I didn’t feel lost in the shuffle. I go back to how I had a really good support system. I had my mom, who was keeping my calendar updated [to] say, ‘Hey, you need to go in this week and do this, and you have a pill schedule all set out.’ That’s very helpful.
When you’re in the hospital, you don’t have to worry about anything like that. There’s going to be nurses that are going to be coming in. They’ll tell you you need to do this, this, and this. You pretty much do whatever they tell you to do.
From that standpoint, the more help you have, the better. They’ll make sure that you’re doing what you’re supposed to do.
Treatment and Side Effects
Describe your first hospital stay
It was about a month off the bat, maybe 30 to 35 days. During that time was intense chemo. I had the 2 bone marrow biopsies. They were maybe a couple weeks apart from each other. There were daily chemo IV infusions.
There were probably 3 to 4 different chemos that were going on. It was some cocktail based on whatever the protocols are. I was on the youth protocol, as opposed to the older people protocol.
I think that’s what they were going off of. It was various, different, brightly colored medicines in bags.
I would also get blood plasma infusion, platelets. Your platelets will go down when you’re going through the treatments. That was pretty much that first month.
Describe the PICC line
I had a PICC line, a way to administer the medicine through my arm. That became a port in my chest, which was put in later after I’d left the hospital. Those were the 2 main vehicles that I’d get treatment through.
There would be pills as well. As I recall, daily they were doing different tests and checking levels of everything. I was neutropenic for most, if not all, of the time, so there were limited food options I could eat. Your taste buds are very damaged throughout the whole process.
What were the chemotherapy side effects?
Summary: Neuropathy, muscle cramps, heartburn, fatigue, nausea, mouth sores (mucositis)
There was numbness and tingling, which I’m sure a lot of people will speak on. You get a strange numbness or tingling in your toes and fingers. I would get spasms, which I still get sometimes. I’m pretty sure that’s related to some of the chemo.
I think it’s really important to be really hydrated as well. They always tell you that in the hospital.
Spasms. They’re like muscle cramps or spasms. They manifested after I started getting treatment, so the assumption is that it’s from the chemo. There was this one crazy instance where I got this spasm in my arm, and it started twisting in a clockwise manner. It was almost like it was possessed.
The nerves just took over or did something crazy related to the medicine that I was taking. That was the craziest nerve issue, but there are certainly nerve issues.
There’s heartburn associated with chemo, so they give you omeprazole to help mitigate that to some extent. That’s all part of the protocol. Chemo in general is a poisonous agent, so it damages the lining of the chest area. Things like that. That’s definitely an effect that I experienced fairly regularly throughout the treatment, and I still will occasionally have that.
General fatigue is another one. Chemo makes you tired in general.
Of course, the nausea is a big one. I take Zofran. I would take that for that, which is a pretty common nausea medication. They have stronger stuff if it really starts to affect you. Nausea’s a big one related to typically the level of chemo that you’re getting. If they lower the dose, you’ll probably not be nearly as nauseous.
I think it’s important to eat, too. When I wasn’t eating enough, I would start to get nauseous. Even if it doesn’t taste good, it’s good to eat food and just have food in your body.

There was a time when I got this thing called mucositis. That was this horrible mouth sore where you get a canker sore in your mouth, but it’s your entire mouth. I could barely drink water. I definitely couldn’t eat any food.
Because of that, I was not eating. Actually, it was over the course of a week, and I hadn’t eaten any food in 4 days. I became what they call delirious. I didn’t know where I was. I didn’t know what was going on for 6 hours.
I was finally able to eat after that, but it was a pretty crazy time. It’s good to eat. Don’t get mucositis — that’s not fun — but if you get it, there are mouthwashes and things you can take.
That was a rough one, though. The taste buds was tough for me because I love food, so I was very sad. You have to have strong, heavily salted or heavily sweet, just to get the taste.
There were headaches. I had spinal taps as well. The purpose of the spinal tap is to administer the chemo into the spinal column and brain stem.
Due to that, there was some pressure buildup. I would have some headaches related to receiving treatment through the spinal taps.
Describe the hair loss
I didn’t actually lose it until much, much later. I was expecting that to happen within that first month, but it was probably 9 or 10 months after.
»MORE: Dealing with hair loss during cancer treatment
Within 2 weeks, it all fell out. It was really weird. Then it sort of came back about a month after that. It was strange. I think my body finally just called it quits and said, “Okay, we can’t hold out any more.”
It wasn’t so bad. I know a lot of people have different experiences with the hair loss, but for me personally, it was kind of weird.
You chose to be outpatient after the first hospitalization
After I left the hospital, it was pretty much like a maintenance thing at that point, so I would go in weekly in the beginning to get IV infusions. It was a situation where I could’ve stayed in the hospital, but I just wanted to be a little more independent and do things on my own.
They said as long as you can stick to your regimen, take the pills you’re supposed to do, follow the rules, and come back in when you’re supposed to get treatments, you can stay at home.
I much preferred that. I didn’t want to stay at the hospital any longer than I had to. It was a weekly come in, get a treatment, get a checkup.
They were probably doing blood labs once a week to make sure [I was okay] because it’s pretty volatile when you’re getting the higher levels of chemo. You can drop to [low blood counts] very quickly. Different things can happen.
There was a point when I got very weak because my white blood cells were really low, so I was just walking up and down the stairs. I was staying at my parents’ house, and going up and down the stairs was the hardest thing ever. I pretty much collapsed, so we ended up going in. I had to get a bunch of blood to re-energize myself.
»MORE: Mental and emotional support when leaving the hospital
How often did you have to get infusions after the hospital?
Once a month. The longest wait is when they order the medicine. They hook up to my port, pretty much just hang out, and chat with the nurses and when they bring in the medicine.
The process itself might be 8 minutes or so. From start to finish, it could be an hour or longer just because of all the setup and stuff.

When you switched to chemo pills, how many did you need to take?
I alternate between 1 and 2 mercaptopurine pills, and those are just a chemo pill I’ve been taking for years now. That’s the only daily one.
There’s methotrexate. That’s a more common one that I take weekly, unless it’s a treatment week. Then I’m not taking it because I get it through the IV.
What were the side effects of chemo pills?
I think now the dose is pretty manageable for me. After the first 6 months, after the first year, after the first year and a half, the doses will gradually diminish for me. Now it’s pretty manageable.
I typically don’t take any anti-nausea pills or anything like that. It definitely varies for everyone because it’s based on the amount of treatment you’re getting. That’s going to affect the nausea and different side effects. I don’t experience many.
I would say the main one is probably being a little bit more low energy than I would normally be. Next May when I’m done, I’m imagining I’ll have more energy in general, but it’s not super quantifiable. It’s not something where I feel super weak. It could be different for different people.
But for me, it’s nothing discernible. It’s not inhibiting in any way. I try to play sports, and I run and do different things. It’s not really inhibiting in that sense, but I would imagine when the medicine is no longer there, I’ll have a little bit more energy
Describe the spinal tap procedure
Spinal taps are in the radiology department of the hospital. They’ll lay you down on the table. It’s similar to the bone marrow biopsy process, but much less invasive I would say.
They give you a numbing medication, which feels like little stings to numb from the main needle that goes in. Then they put that in, and they get to the right area. In my case, they extract spinal fluid and then replace a similar amount with the chemo.
That will leave you with some of the pressure issues. That’s the process. You feel a little bit of a pressure, but not a sharp pain really.
There can be nerve issues. They’re in your spinal column area, so if it hits a nerve for example, you might feel a shooting pain down your leg or something. There are those things that can happen.
Other than that, it’s a pressure. I have no ill effects afterwards. There may be occasionally a little bit of achiness after for a couple hours, but typically there’s no aftereffect at all. Once they’re done, they’re just done.
It’s the lower spine area, near the lower vertebrae. It’s more of a pressure feeling because they are numbing it, so you don’t actually feel like, “Oh, there’s a needle going in me!” It’s kind of like a deep pressure.
Not to say it’s comfortable, It’s not comfortable at all, but it’s just a different kind of pain I’d never experienced before. I’ve never had anything like that. It’s more like someone’s really pushing on your back.
The time it takes is between 20 and 40 minutes. If they were only administering the chemo, it would be half the time. Because they’re removing spinal fluid and they have to find the area, it takes a little bit longer.
Why did doctors decide to remove spinal fluid?
Originally, we weren’t removing spinal fluid, but I was getting these headaches. We were thinking, “Let’s try this, because it could be a pressure-related thing with the fluid.” As soon as we started doing that, it helped a lot.
Not to say that works for everyone, but certainly for me. That’s what we ended up finding out. That’s not always the case with people, but for me it was the case. Before we were doing that, I could hardly lift my head. I’d be lying down all day and have these really bad headaches from that. That helped a whole lot.
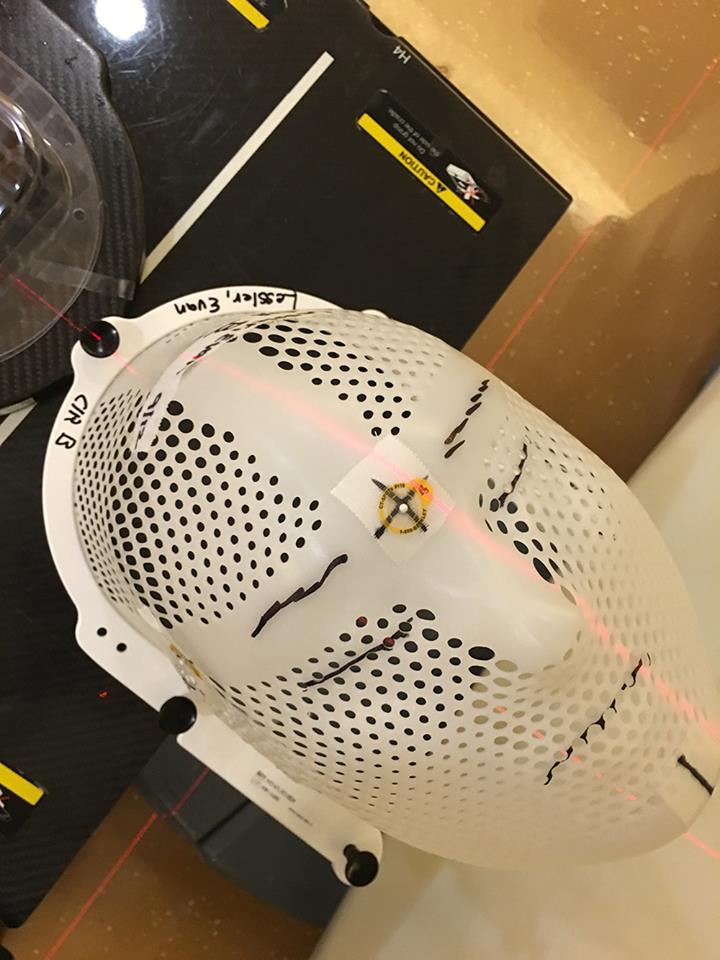
Describe the cranial radiation
It was preventative in the event there was some type of cancer that developed in the brain area. It pretty much wipes it out if it’s there. I think that was the idea.
That was at the end of the first year, so maybe about 11 months in. That was 10 to 12 sessions. It was low-dose radiation. It wasn’t anything too extreme, but it’s a weird feeling.
They lay you down. They make this mold of your face, this mask to protect your facial area from the radiation beams they’re shooting. It’s a really quick process. It takes 5 seconds every session. For me, it’s a blue light, and then it’s a weird smell.
Other people have described no smell or some other type of light or something. I think it’s some weird sensory thing that everyone experiences differently. To me it was a funky smell. Really nothing else associated with it.
There may have been headaches related to it, but because of the other treatments I was getting, you can’t really tell if that’s related to that or related to something else.
They did give me some pill that would potentially alleviate memory loss issues that could be associated with radiation. I have no idea of their effectiveness.
My memory could be worse now. I have no idea! I can’t remember, surprisingly enough. That process wasn’t too bad at all.
Describe the process of the cranial radiation
You go in. They would give you the mask, and you’d wear it. You’d lay facing up on a bed, and they would put this device above your head. They would shoot the beam or whatever, and 5 seconds later, it was done and you’d leave.
They would try to get the machine in the exact area, because they don’t want to shoot you in some other area that you’re not supposed to be shot in. It was a quick, painless procedure.
How often do you need follow-up appointments?
Since I left the hospital 2 years ago, it’s been pretty much just varying degrees of whatever they’re telling me to do now. I go in every month. I get IV treatment for chemo. I take pills every day from home.
Every quarter at this point, I do the spinal taps for the spinal chemo. That’s been my schedule for maybe the past 6 months or so. Before my spinal tap was quarterly, it was alternating every other month. Everything else has been pretty consistent.
Quality of Life
What was the worst part of treatment?
The worst part of the treatment that was administered to me was probably the bone marrow biopsy, simply because it’s very painful. I would say between that and the headaches due to the initial spinal taps, those were the most uncomfortable, painful things.
The mucositis was another really painful one. That’s a side effect of just receiving chemo. I don’t know that I’d call that part of the treatment, but that was something that happened.
A lot of it, too, is just the frustration associated with the amount of time that it takes. My plan is all told 3.5 years. Compared to a lot of people, that’s very long.
It gets a little bit frustrating, and it’s kind of tiring to have to deal with this stuff over this large amount of time. All things considered, I’m just glad I’m still here. Those are the different challenges that I experienced, but I would say if I really had to pick one, it’d be the mucositis. It was the worst one.
Coping with a longer cancer treatment
Honestly, the biggest thing is just having an understanding that there’s nothing you can do about it. There’s no purpose in lamenting your life or lamenting your situation if there’s zero you can do about it.
The best thing you can do is just do what you’re supposed to do. Make sure things are going as they should be. When that 3.5 year hits, I’m done. I think that’s the way that I looked at it. Keeping positive in most situations in the best way you can.
Thankfully, I had my business, so I can stay busy with that and not just sit and brood and lament things. If I’m busy shipping orders or working the store, it’s going to take me away from that situation.
Staying busy, not idling is important. Having a positive attitude.
How did you deal with the emotional and mental stress?
That’s the craziest part. There’s a couple phases that happen. First is the shock part. What is cancer? I don’t know. I’m a relatively young person. This is a relatively unusual type of cancer for someone of my age.
It’s usually typically with very young or old people. The shock part, not knowing what’s going on. Then you get a little bit fatalistic with the whole thing. Does this mean I’m dying? How much time do I have?
As you go through the process and start to get the treatment and people start to tell you things, you have an understanding of what’s going on and what the process is.
Emotionally, it’s very up and down a lot. Having a good base of friends and family to keep you grounded is really important. One of the most important things I was told was to just keep your spirits up.
Keep positive. Don’t think dark thoughts and think bad things, because that will manifest itself. I personally think it could, if you get too down on yourself.
Positivity is super important. Always was the biggest part of the whole thing, having gratitude for everyone around me and the people that supported me through the whole process. No matter what, you’re going to feel bad because you have cancer and you’re in this really bad situation, but it’s certainly no reason to go into some sort of dark depression.
It’s about staying positive. Going through all the range of emotions. I had family members who passed away while I was sick, so there were other emotions that were playing in. The drugs themselves make you feel certain ways, so there are a lot of weird things that happened in your brain chemistry and everything.
It was a big up and down time, but once the initial craziness was over and I was able to go home and live a somewhat normal life, things sort of even out.
It’s important to not get too down during the really tough times. Of course, there’s no knowing which direction your treatments are going to go or if chemo is working, chemo’s not working. You have to do different types of treatments, but just the best thing is to be as positive as you can within reason.
Just to go through it in that sense. That was probably the biggest takeaway for me.
Could you work through treatment?
I think it varied. There’s be times where I wouldn’t even notice. I’m just working and doing what I used to do — doing clothing events, working the store, talking to customers — but there were other times where it was like I can’t do anything.
The first year, I wasn’t really able to function much. My warehouse manager pretty much handled everything. I maybe answered a couple emails here and there. That type of stuff with the computer is okay, but there were just a lot of times where you’re fatigued, you have a headache, you can’t concentrate, you’re just tired, [or] you’re not in the mental state to be able to work.
I think that’s something that’s different with everyone. It all depends on how you feel, how intense your treatment is, and how much motivation you have to want to work.
There were certainly times where I probably could have worked, but I’m like, “I’m just going to rest. I don’t want to work.” It was a good combination of you work when you can work, take off time when you can take off time.
More: Working during cancer treatment →
Paying for cancer treatment
I was very fortunate. My mom has always told me growing up, some of the best advice is, “Don’t ever go a day without medical insurance.” I know a lot of people do go without medical insurance, and there’s certain programs and things in place for that, but if I didn’t have insurance, I would be in a much different situation than I’m in now financially.
Having insurance is incredibly important because insurance exists because of situations like this. It’s not what you anticipate happening; it’s what you don’t anticipate happening. I never thought in a million years it would happen.
Then it happened. It’s really expensive, so the fact that a huge amount of that is covered by my insurance was a huge boon for my situation in the sense of not having to pay for it myself.
You make the monthly payments for whatever — the copay. Obviously, the amount of the copay and amount of the monthly payment is related to the plan that you have.
I would recommend a younger person get something middle of the road that’s going to cover you in catastrophic-type situations, where it’s hundreds of thousands of dollars worth of treatment. I imagine I was high in the hundreds of thousands, so I definitely recommend getting health insurance.
Did anyone help you navigate the decision-making?
I remember when I was in the hospital, they would have people come in that would say, ‘Hey we want to make sure you understand your plan, how everything works, if you have any questions.’
But I had my mom. She was handling the bills and all that, so she had an understanding of how some of that would probably work. I didn’t have to deal with much of that. There are certainly advisors for that.
Did you have to advocate for yourself during treatment?
My doctor’s really great. She didn’t tell me to do anything that was particularly weird or not doing right by me. I didn’t get that feeling. Then having my uncle [be] a doctor and mom a nurse — they’re pretty smart people, and I’m pretty sure my mom’s not going to let these things slip by.
If you feel like that’s happening, absolutely leave got o a different hospital. It’s your own life. It sounds bad but, it’s not their life. It’s your life. They don’t necessarily care as much, because it’s not their life.
They’re just following whatever they think they’re supposed to do. You always have to take care of yourself first. If you don’t feel like they’re doing it, find somebody that’s going to do that.
» MORE: How to Be Your Own Advocate
Message to other patients
The first one would be to meter your expectations for what is going to happen to you in the future, at least in the immediate future, because you just have no idea.
Unless you’re a doctor or you know how this works, they could tell you something a week from now that’s completely different from what they said before based on some other information that’s come up or based on the way you’re reacting to your initial treatment.
Just don’t get too caught up in, ‘This is the way it’s supposed to be, or ‘This is what I want to happen in this situation,’ because you don’t have control over the situation.
I think the best thing you can do is roll with the punches, follow the protocols they tell you to do, [and] don’t get overly stressed out about the situation, even though you’d be understandably pretty scared and confused.
Trying to be as calm and level-headed as possible is important for your general health and well-being. That’s what helped me a lot going through the process — and having people around me that could help me work through those issues as well if I was starting to feel down.
Just understanding your expectations and realizing the next year of my life is not going to be [what I expected]. I had these trips planned, or I had this thing I was going to do with my business, or get this job or something — you just can’t expect any of that to necessarily pan out the way you think it will.
Just take things literally day by day, step at a time. Just keep your expectations in check of what you think might be happening in the near future. I think that’s really important.
Also, eating healthy is also important. You have to take care of yourself in aspects that you can control because you can’t control the treatment. You can’t control the different medicines you have to take, but you can control if you are physically able to stay fit and work out. Do that. Try to eat as health as you can.
Try to do the normal things that you normally do. Don’t be bedridden all day if you don’t have to be. Positivity, huge. Positivity is like the running theme for me — to just have a positive outlook.
Inspired by Evan's story?
Share your story, too!
Acute Lymphoblastic Leukemia (ALL) Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)



