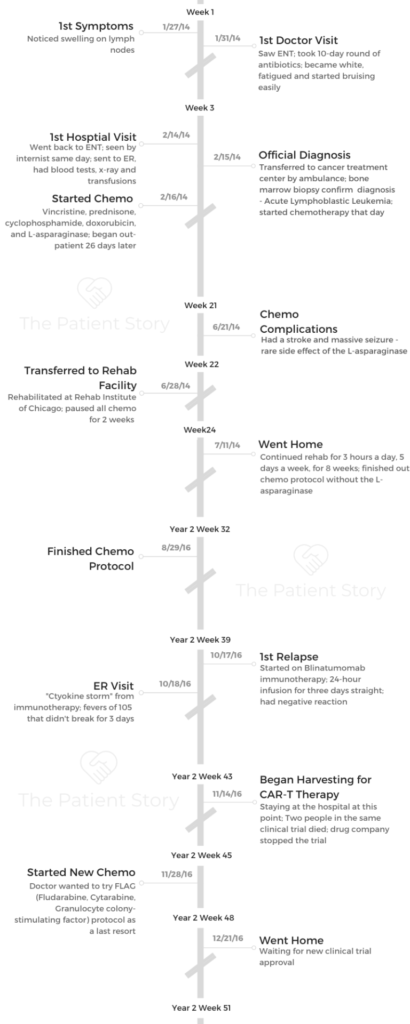
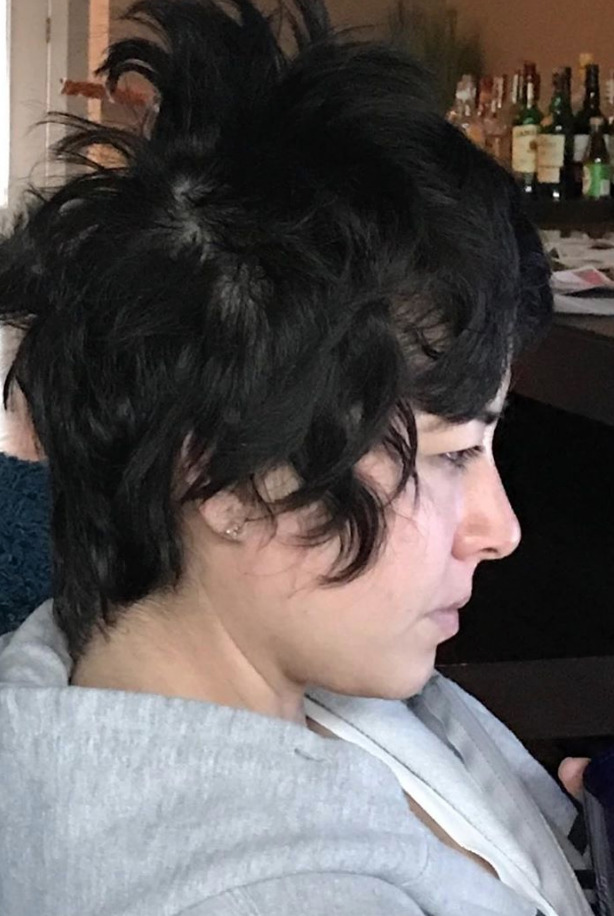
Casey’s Relapsed Acute Lymphoblastic Leukemia Story
Casey’s life changed after her acute lymphoblastic leukemia (ALL) diagnosis, 2 relapses, and undergoing many treatments: chemotherapy, immunotherapy, radiation, and a stem cell transplant.
In her story, the survivorship coach shares how she navigated life with and after cancer, from losing her hair twice, advocating for herself as a patient, and the support that helped her the most. Thanks for sharing your story, Casey!

- Name: Casey H.
- Diagnosis:
- Adult acute lymphoblastic leukemia
- Staging: N/A
- 1st Symptoms:
- Lump on throat
- Extreme fatigue
- Shortness of breath
- Bruising easily
- Treatment:
- Chemotherapy
- Vincristine, prednisone, cyclophosphamide, doxorubicin, and L-asparaginase for 8 weeks
- Immunotherapy
- Blinatumomab
- “fanny pack” infusion
- Izotunomab
- Clinical trial
- Blinatumomab
- Radiation
- Total body in preparation for the stem cell transplant
- Stem cell transplant
- Chemotherapy
- Diagnosis
- Chemotherapy & CAR T-Cell Therapy
- You had some complications with the chemo. What happened?
- What were the next steps after learning you were chemo-resistant?
- What happened after chemo and CAR T therapy both failed?
- How did you handle the time between failed treatments and waiting for the new one to start?
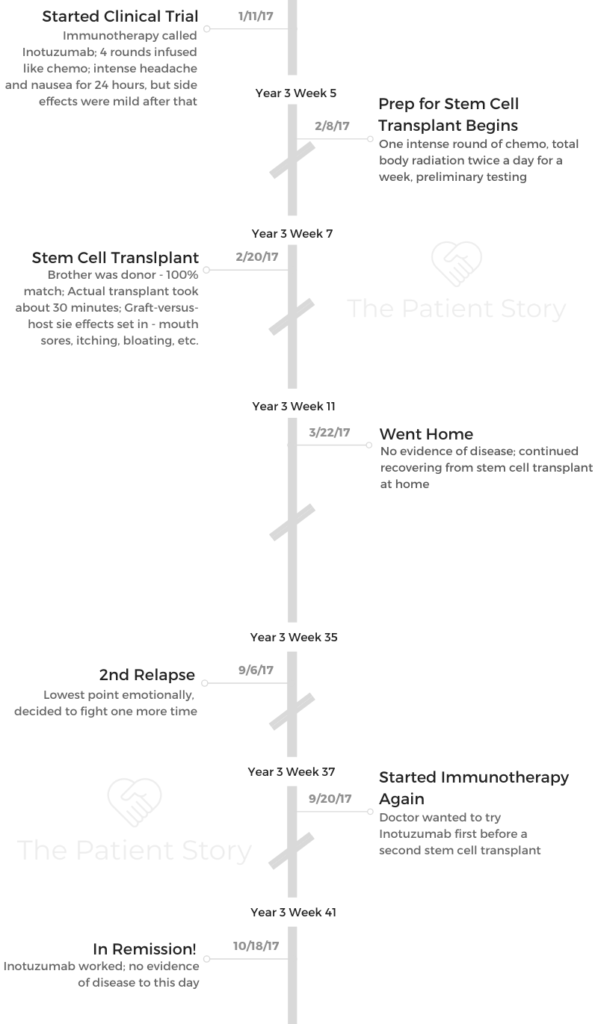
- What was your clinical trial like?
- What happens after the clinical trial?
- What was the total body radiation like?
- Stem Cell Transplant
- Hair Loss
- Quality of Life
- What was the lowest point you had during all of this?
- Preserving fertility
- How did the cancer affect your relationship with your spouse?
- What helped you process your emotions after cancer?
- Paying for cancer treatment
- Be your own advocate
- Do you have any advice for someone who’s nervous about standing up for themselves?
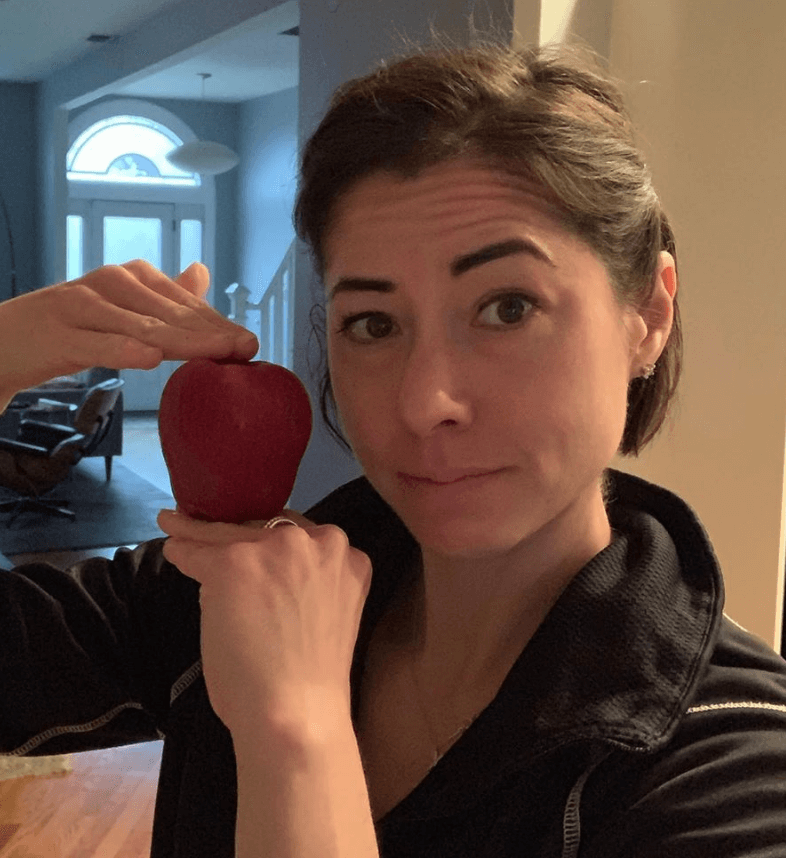
- Support & Survivorship
- Do you remember the last time you went into remission? How did you feel?
- How important was it for you and your husband to have outside support?
- Did you feel like you could ask for help when you needed it?
- Was there any gift or service anyone gave to you or did for you that really stood out?
- The “new normal” after cancer
- What is your advice for someone who has just been diagnosed?
- Do you have a message for anyone reading this?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Just breathe. It’s going to be okay. You and your body are so much more resilient and strong than you think. Your body can withstand so much and recover.
There is a whole other level. You can dig deep and find that can get you through anything. You just have to be open to it.
You cannot get through it without digging really deep sometimes and knowing that you can get through it.
Casey H.
Diagnosis
What were your first symptoms?
I found a lump on the side of my neck. I thought I was getting sick, so I didn’t really think much about it. I went to an ENT, and he gave me 10 days of antibiotics and told me to come back in 2 weeks.
I took the antibiotics, but they didn’t go away. There were about 3 nodules on each side.
From the time that I stopped taking the antibiotics to my doctor’s appointment on that Friday was about 5 days. During that time, I started to get really short of breath.
I normally go to work, walk up 3 flights of stairs, and start working. I couldn’t hardly get up 1. It took me 10 minutes to walk up the stairs.
I became really white and started bruising really easily. I would touch my hand to a counter and have a bruise. Then I started getting petechiae all over my body. They’re little clusters of red dots. I didn’t know what that was.
On that Friday I had my doctor’s appointment, my boss had pulled me into her office. She was like, “Are you okay? What is going on?” She thought my husband was beating me or I was hungover or something. I was telling everyone I was tired and had a doctor’s appointment.
How did you get diagnosed?
When I got to the ENT, I could tell he knew something was wrong. He sent me over to an internist. He immediately took me in, and I knew that meant something was going on.
He had me walk around the office, and he couldn’t get a pulse [oximeter] reading. He didn’t understand what was going on. From that appointment, they sent me straight to the ER.
They told me I needed blood work and that was the fastest way to get it. They were concerned since it was Friday and might have had to wait over the weekend, so I went straight there.
They took my blood, and in the meantime, they gave me an X-ray because I was complaining about lower back pain. I was getting an X-ray, and in that time, they said I needed a blood transfusion right then.
They didn’t explain anything to me, so my husband and I asked them what was going on.
After they started ordering everything, the emergency room doctor came in and said, ‘We are 90% sure you have leukemia, but you need to get a bone marrow biopsy to confirm it.’
They said they couldn’t transfer me to the cancer treatment center I wound up getting my treatment from until I had another pint of blood and more platelets.

What happened when you heard the diagnosis?
I looked at my husband kind of confused and said, “Wait a minute, what?” My brain could not grasp that concept. They handed my husband a pamphlet about acute lymphoblastic leukemia. He showed it to me, and my brain was just not computing what was happening.
It was so uncomfortable that I couldn’t really process what was happening. I was running on such little hemoglobin, so I wasn’t really functioning properly anyway.
Add in the shock, and it was very confusing.
You’re told what you’re going to be doing. You’re in such a deteriorated state, so you’re pretty much just like, “Okay. Is it gonna make me feel better?” You don’t think about what you’re about to do because you don’t really have much context for it.
The only time I had heard the words “cancer” were with older people. I just wasn’t familiar. It was never a thing I thought would be a possibility, so I hadn’t given it much thought. There was more shock than anything else.
»MORE: Patients share how they processed a cancer diagnosis
What were the next steps?
When they did the bone marrow biopsy, they actually wound up doing 3. When they pulled the first one out, it was so compacted that it looked like a white strip of plastic.
The attending physician looked and said it didn’t look right. He said, “Maybe I got bone instead of your marrow. I have to go again.”
They did another one, and it looked the same. He said the odds of him missing twice were super slim, and he wanted to do one more. I was so high on the drugs they gave me that it didn’t matter. The third one came out the same.
He came in later that day and said, ‘I’m so sorry we had to do that. It was your bone marrow. It was so far off from what it’s supposed to look like. It was compacted bone from the leukemia taking over.’
He apologized for having to do the biopsy 3 times but said it confirmed the diagnosis, and he told me how we would proceed.

He pulled out this 5-page protocol they were going to put me on and went through it. [The protocol] was over a year and a half, so you just go into survival mode and say, ‘Okay, what am I doing today?’
What was the bone marrow biopsy like?
I’ve had more than 20 now. The first time, though, they gave me Dilaudid. I’d never been on anything that strong before, and I barely take Advil. I was high as a kite. I looked at my husband and said, “I completely understand why people do drugs now.”
After they give you the drugs, they also numb the actual area of extraction. People often say it’s the most painful part of the process, but for me it wasn’t.
It is painful, but it wasn’t as bad because I was so drugged up. It’s more painful the next day because there are no meds and there’s bruising on your back.
You’re so heavily medicated that you don’t really feel a whole lot of pain, but it literally feels like they’re drilling into your back with a giant screwdriver.
The amount of pressure it puts on your lower back is suffocating to the point where you have to remember to breathe.
I had mine lying flat on my stomach. The doctors were sweating when they were doing it, so you know it’s a lot of pressure. If they don’t pull out the bone marrow the right way, it can get stuck in your bone, and that is probably the worst part.
How did you break the news to loved ones?
My husband was with me, and I had him tell my dad. I couldn’t say the words because I was scared and honestly a little ashamed at that time. I didn’t know where it was coming from. Especially as a female, you tend to blame yourself.
I kept thinking, ‘What did I do wrong? Is there anything I could’ve done differently?’
I took on the responsibility that I created it, which isn’t how it works at all. During that time, I just couldn’t say the words to people. I had my husband do it for me.
»MORE: Breaking the news of a diagnosis to loved ones
Did you get a second opinion?
I was in a weird spot where I trusted the hospital and the plan they came up with. Northwestern and the University of Chicago work really closely with each other. They share a lot of information and consult with each other on tough cases.
I was so degenerated that I don’t think I had time to get a second opinion, but the 2 hospitals were already talking to one another about it. Looking back, would I have gotten one? I don’t know.
Chemotherapy & CAR T-Cell Therapy
You had some complications with the chemo. What happened?
My regimen was 6 doses of doxorubicin, 5 doses of daunorubicin, 7 of cytarabine, 3 of cyclophosphamide, 13 of thioguanine, and 7 PEG-L-asparaginase.
Unfortunately, I had a stroke and massive seizure as a complication of the PEG-L-asparaginase.
I remember looking at the side effects of the chemo and going, ‘Who has a stroke?’
Then I signed the paperwork and kept going.
That left me temporarily paralyzed on my left side. I’d spent 2 weeks in the hospital at the Rehab Institute of Chicago to basically learn how to use my left side again enough [until] they could discharge me.
In that 2- or 3-week time period, they did stop chemo for a little while, but then they put me back on. I was rehabbing and on chemo, and I did that for 8 weeks.
It was a good thing because it really pushed me to see how resilient the body is and what it can come back from. It was very interesting in that regard.
I finished out the protocol in 2015, and 7 weeks later, I relapsed. I went right back into the hospital for 60 days. During this time, they decided I was chemo-resistant.
What were the next steps after learning you were chemo-resistant?
They had one immunotherapy drug at the time called blinatumomab. They wanted to give it a try. You get a fanny pack. It’s a 24-hour infusion for 3 days straight.
You go back to the hospital, and they change it out. Then you normally would do that again, but within 24 hours of me starting that, I was right back in the hospital again.
It caused a cytokine storm. I basically had the flu but way worse. I was spiking fevers of 105, and they couldn’t break it for 3 days straight. Immunotherapy works different ways for different people because it’s about the way it interacts with your body.
A lot of people have different experiences than I did, but that was the negative side effect I had from that.
The initial side effect was extreme fatigue. I went home and had to bring a chair in our shower because I couldn’t stand long enough to bathe myself. That was what made us go to the hospital. We knew something wasn’t okay because I was way too fatigued. Then I started spiking the fevers.
I had to beg them not to send me to the ICU. I had to get the immunotherapy out of my system, and then I started to feel better.
What happened after chemo and CAR T therapy both failed?
At the time, Northwestern was working on CAR T-cell therapy. It was a clinical trial, and that’s what we went for next.
To be on a clinical trial, you get tested for everything under the sun. They take your own immune system and engineer it to fight the cancer.
I started to do all the testing required for the trial, along with having my own stem cells harvested. I had just had my stem cells harvested and was going to start my clinical trial the next week.
Unfortunately, during that week while my cells were at the lab, 2 people in the same clinical trial passed away. The drug manufacturer shut down the clinical trial, so at this point I had nothing. They said the University of Chicago had a different clinical trial, but it was full.
I stayed in the hospital for 60 days total this time, mostly doing maintenance chemo with a side of steroids to keep the leukemia at bay.
Then after an oncology conference, my doctors suggested that another immunotherapy may work. There wasn’t very much information.
Basically, there were 2 pages of research, and only 11 people on it had acute lymphoblastic leukemia. I had no other options.
Worst case, they would have possibly transferred me to another hospital for a different clinical trial, which happened to be full at the time. So I waited.
Over the 60 days in the hospital, I was starting to go a little stir crazy, but the doctors suggested I try the FLAG protocol of chemotherapy just in case it might work. It’ a combination of fludarabine, high-dose cytarabine and filgrastim. It’s normally for relapsed AML patients. Unfortunately, it didn’t work.
Just before Christmas and after 62 days, they sent me home and sent letters of compassion to Pfizer and the FDA for approval to use this new immunotherapy.

How did you handle the time between failed treatments and waiting for the new one to start?
I was out of the hospital for about 2 months, waiting for this treatment to be approved for me.
I really thought I was going to die. I didn’t really see another outcome happening.
I started cleaning out closets, because that’s what you do apparently. I threw a lot of stuff away. My husband asked me what I was doing, and I said, “I’m just trying to make things easier for you because I’m not going to be here, and I don’t want you to have to do this.”
He told me to stop and told me I didn’t know that. I said, “Well, but don’t I?” I was telling him what I wanted him to do if I died.
I also had some really hard conversations with my dad. I told him I was scared I might not be here, and he looked at me quite frankly and said, “You know, sometimes we all don’t make it until the end.” I was like, “What? Who says that?”
Looking back, I know that was his way of processing and preparing himself for the worst. It was just one of those weird conversations you have when you’re watching Law & Order in the middle of the day with your dad.
What was your clinical trial like?
I eventually got approved, and we didn’t know what to expect because there wasn’t a lot of information, but it actually wasn’t that bad. I had 4 rounds of this immunotherapy called inotuzumab.
Honestly, the side effects — compared directly to chemotherapy — aren’t that bad.
I had a headache for 24 hours and was nauseous for about 12. After that, it was pretty much nothing. I did 4 rounds, and I got into remission a second time from that.
What happens after the clinical trial?
After I went into remission, it was immediately stem cell time. I needed to get my transplant really quickly after that.
I was in the hospital for another 32 days. I had another intense round of chemo before the transplant because that’s just what they do, I guess. I had total body radiation, and then I got my brother’s stem cells.
My brother is my donor, and he’s a 100% match. On February 20th, I was ‘rebirthed.’
What was the total body radiation like?
I had total body radiation twice a day for 7 days straight. I got fitted with lung plates to protect my lungs. They put you in a position where you have to lay as still as you can for 30 minutes.
You don’t really feel anything in that moment. It just feels like you’re laying in a room.
You just wear the clothes you’re already wearing, which is usually just sweatpants and a loose shirt. That’s it. They wheel you in, they position, and they flip you over like a pancake once.
I didn’t actually feel the side effects of the radiation therapy until after my stem cell transplant. We finished the radiation and did the transplant the next day. There wasn’t really a lag time.
The actual radiation itself is not painful, but the side effects are like getting hit with a truck. I don’t know if it was because I had the stem cell transplant and the side effects compounded or what, but it was intense.
Stem Cell Transplant
What happens with a stem cell transplant?
They warn you that you’re going to be in there for about 30 days. The first week, I did the chemo and radiation. Then they set the date for the stem cell transplant.
It’s kind of uneventful. They come in with a cold container and pull the stem cells out. They’re a salmon-y color, and they’re in this big tube.
They hook that up to your infusion thing and start pressing down. It goes into your body, and honestly the worst part is the smell. It smells like creamed corn and vomit. It’s so distinct.
Any time anybody on the floor was getting a stem cell transplant, I could smell it. I would have to hold my breath when I walked past the room. I’ve never smelled anything like it.
Before the transplant, they gave me Advil or Tylenol and Benadryl. The entire time they were doing the transplant, I was trying to stay awake. It was a good thing that was happening, and I wanted to be awake for it, but I was pretty out of it.
My throat started to close up a little. It felt like I had something caught in it. Their solution to that is popsicles. I’m sitting there half out of it from Benadryl, eating a popsicle, smelling like creamed corn and vomit. It was the weirdest thing.

Describe the stem cell infusion
The actual infusion takes no more than 30 minutes. After that, they just wait to see what happens because graft-versus-host side effects are different for everyone. They wait for the side effects, and when they happen, they deal with each one as they come.
That’s why they keep you in the hospital after the transplant. The worst potential side effect I remember them telling me was my body could reject the transplant completely, and that can potentially kill you if your body doesn’t react to it the right way.
They just want to make sure the side effects you do get aren’t life-threatening. The ones I got were pretty bad. They were pretty standard, but they were pretty terrible. It really takes its toll.
What side effects did you experience from the stem cell transplant?
You get what are called graft-versus-host disease (GVHD) side effects. Those are brutal and aggressive and uncomfortable. My graft-versus-host side effects were mouth sores, itching, bloating, and eye sensitivity.
I couldn’t eat solid foods or ingest liquids. It was super painful. I had a full body rash happening. It looked like I rolled in poison ivy.
It was super uncomfortable and itchy. I couldn’t pee. They have these pills they give you that are supposed to help you pee immediately, but they didn’t work.
»MORE: Explore more on GVHD and what to expect from a medical expert
I left the hospital and couldn’t buckle my bra because I was so bloated from the water retention. I had gained more than 30 pounds of just water weight.
I started having panic attacks about leaving the hospital. I was like, ‘Oh my god, my team’s not going to be here. What if something happens?’
Everything starts going through your head, and you start freaking out.
They were like, “You have to leave. It’s time to go home,” but I just kept asking if they were sure. My mind kept going to worst-case scenarios.
I went home. Within a week, the water weight was gone, but I still had the side effects. I still had the mouth sores and weird rashes. That eventually went away.
I still get mouth sores occasionally, but they only show up if I eat certain foods. They aren’t nearly as bad as they were, though. Also, my eyes are really sensitive to the light, which is apparently pretty normal for transplant patients.
The mouth sores were by far the worst side effect. They’re so uncomfortable because you can’t eat. I had one in the middle of my throat. I could feel it, but I couldn’t pop it. They say you’re not even supposed to run your tongue over it. They told me not to mess with them. It’s just very uncomfortable.
»More: Leaving the Hospital: Emotions & Support
They gave me a steroid rinse to help with them. They were so aggressive in the beginning that it didn’t really do anything for the first 2 weeks. Then they start to just pop on their own, which sounds so gross because it is. When they pop, pus runs out.
It’s by far the grossest side effect. You could see it. You could feel and know what’s happening, so it’s disgusting. I spit up blood because they were in my mouth, and it’s just really really bad.
What helped you with side effects from treatment?
Continue to move every day in some capacity. You need every ounce of strength you can get. Even if it’s just walking for a second, get out of your bed.
It’s so important physically, but mentally and emotionally as well. Keep working out for as long as you can and as much as you can every day.
The movement helps you get out of your own head and helps alleviate the side effects.
I did a lot of walking just because it was summertime. Body weighted exercises are also good, or any strength training. You can slow it down or modify anything based on how you’re feeling that day. If you’re doing cardio, it’s more high impact. No matter what you’re doing, it’s so essential to have as much strength as you can get.

You relapsed a second time
Then 7 months after I was recovering slowly from my stem cell transplant, I relapsed again. I had been doing regular blood work, so we caught it early on.
I was so mentally, physically, and emotionally exhausted from the process that I looked at my husband and said, ‘I don’t think I can do this again.’
I was sobbing uncontrollably and got it all out, and I looked at him again and said, ‘Okay. I’ll do this one more time, but that’s it. I can’t do it anymore.’
It was mostly because I didn’t want to disappoint my family. It was hard to dig really deep in that moment and do it again.
Immunotherapy leads to remission
They ended up deciding to go back to the immunotherapy. The immunotherapy worked. It was the inotuzumab.
I went through 4 rounds of that, and it worked like a freaking lucky charm. I’ve been in remission ever since.
Were there any other surprises during treatment?
The stroke was the worst of what I had. I didn’t expect that to happen. Having a stroke is really rare. I don’t know if there’s a percentage, but if there is, it’s really low. That sent me down a whole other rabbit hole of care.
On top of everything else I was doing, I had to then go see a neurologist and have neurological testing done regularly.
Doing all the added tests on top of what I was going through already wasn’t only annoying, but it was exhausting.

Hair Loss
Did you lose your hair?
I lost my hair twice. The first time was the initial hospitalization and chemotherapy. They had told me I would lose it. I was showering one day in the hospital, and a giant clump came out in my hand.
My whole body started shaking, and I was staring at the hair in my hand. I completely broke down bawling. My husband knocked on the door and asked if I was okay, and I said, “I’m fine. My hair is just falling out.”
It was more the reality setting in of what was happening than anything else. I had been putting these toxic poisons in my body, but nothing was really happening. Then that hit me like a ton of bricks. I was like, ‘Holy crap, this is happening. This is real.’
My hair was below my shoulders at that point, and it started knotting up in a terrible ball in the back of my head. There was no fixing it at that point, so I had to cut it out. I had my husband’s sister cut it off my head.
It was pulling at other hairs that were still in my head, and it was terrible. Then it started all coming out, so I just shaved it. I found out I have a really round head, which is a good thing, I guess.
The second time was from the stem cell transplant. They did total body radiation and chemotherapy at the same time. That time, I knew it was going to fall out. Before it did, I shaved it. I wanted to be proactive about it.
How did you emotionally process the hair loss?
In that moment, I realized what was happening. It was super depressing at that point. I wasn’t really getting out of bed. I wasn’t doing anything other than showering or eating.
What helped you through the hair loss and all the emotions?
My dad and husband were telling me I needed to get out of the room. My husband ran into this man we would see from my window. He was always walking around the floor.
He was flying by. The man explained he was trying to make his body stronger by walking. He said 17 laps around the nurses station was a mile.
We came up with a plan for me to do laps. The first time I did it, it took me 5 minutes to go one lap around the nurses station. This 60-something-year-old man is flying by me. I realized there was something to it, and I decided to get out of bed every day.
There was a whiteboard in my room that no one was using, so we started tracking my progress. My husband knew that if I couldn’t get well enough to walk and get up stairs, they weren’t going to send me home.
»MORE: Dealing with hair loss during cancer treatment
That was what started me on setting daily goals and getting out of my own head. That really changed my mindset.
Advice for someone who might be facing the possibility of hair loss
Definitely take control. Shave it yourself. Shave it off preemptively. It can be really painful when it comes out.
There’s also something very cathartic in knowing that you did it, rather than it being a side effect happening to you.
The mind shift is so empowering. I’ve said that to other people who have gone through it, and they agree. It’s empowering to take control of it instead of letting it happen to you.
Quality of Life
What was the lowest point you had during all of this?
The time in between getting out of the hospital after the second relapse and the unknown of not knowing what the next step was and not having any control over the options. I was pretending to live a normal life, but I was not really participating in the same way.
I just wasn’t there. I was checked out. I was thinking about the next closet to clean or whatever. It was hard to enjoy the little moments that were had.
In the back of my mind, I was thinking, “Wow, this is the last Christmas I’m going to have with everyone.” I was just watching my life as if it were a movie. I wanted to savor everything but didn’t want to participate in any of it. I was trying to soak everything in but not participating.
I never really lost hope. I just didn’t know if I would physically make it. I knew at some point there would be a crossroads. I knew I could potentially die from it, but I knew it was going to be slow and awkward and painful. How do you compartmentalize that and keep moving about the day?
It put me in a place that I was [so] desperate for hope that I was clinging onto anything. I took it one day at a time and just focused on that.
Preserving fertility
I unfortunately did not have a chance to get fertility preservation done. I was hospitalized, they started me on chemo, and the next day the woman from the fertility preservation center came into the room.
She said, “I’m sorry, I don’t think we can help you anymore because you’re already doing chemo.”
For a woman, it’s not as easy as a man. You actually have to go through the 28-day cycle to get the preservation done. I didn’t have that time.

I found out early in 2018 that I was infertile. I had the test where they look at how many eggs you’re producing. I’m not producing anything.
At the initial appointment when she told me this, I knew it was a possibility, but it’s a grieving process. I’ve gone through the 5 stages of grief. I still have good days and bad days.
Some days, it’s really heartbreaking for me because of how it affects my family. My husband didn’t really have a say. Some days it hits a little closer to home than others.
I’m at the age where that’s the first question people ask. “Do you have any kids?” It’s not on them. They’re just asking because that’s what you do. Sometimes I explain why I don’t, and other times I don’t. It just depends on how I’m feeling. It’s an emotional rollercoaster.
My doctors tell me I can still “have” children probably and bear them. But it’s not mine. They tell me I won’t feel that way, but I’m not there mentally or emotionally. I get it. I could still birth a child. It just wouldn’t be mine genetically. It would be my husband’s and some egg donor’s. I’m just not there.
I’m still not there with adoption either. I don’t know if I ever will. Some days it sounds like a really good idea, and other days I don’t think I can do it.
I don’t know if I’ll ever get there. I’m not closing the door, but it’s not fully open either. There’s a screen door basically.
My husband and I have had very open conversations about it. I’ll even tell him when I’m having a tough day with it. He listens and understands. He has tough days, too, sometimes. He doesn’t know if it would feel fair that we had a kid that was genetically his and not mine.
For that reason, he’s more open to adoption. He reassures me that it’s totally up to me. It’s not a yearning for him right now, but he’s open to it. He lets me steer that conversation.
»MORE: Fertility preservation and cancer treatment
How did the cancer affect your relationship with your spouse?
Marriage is really hard, period. We’ve been together for more than 11 years, and no jokes about it, it’s hard to live with someone that long. Having this on top of it was even harder.
We separately see therapists, and we have also seen a therapist together to make sure we’re communicating and on the same page. If you don’t have open communication with your partner through this process, it will destroy you.
I’ve seen it with other people. They just fall apart. Being married is hard, and adding this on top of it is just really really hard.
I would recommend immediately going to see a therapist. Even if you know you have a really strong relationship, there are so many tools they can give you.
The way I grew up, I’m half Japanese, so if you have emotions, the culture is you shove the emotions down and don’t talk about it at all.
Honestly, I did that during cancer. I shut it down and went through survival mode. My husband was much more open to talking about it, suggested the therapist, and wanted to do the emotional and mental care the right way.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer

What helped you process your emotions after cancer?
I go to a therapist who specializes in cancer. My initial visit with her was pretty funny. She and I disagreed a lot. She told me later that she didn’t think I was coming back. I knew I needed the help.
I didn’t know how bad I needed it, but in that moment, I knew I needed some support. She was honestly a lifeline. Without her during my last relapse, I don’t know if I would’ve made it through in one piece.
I highly recommend seeing a therapist. The mental side of everything is so important to take care of. It’s so essential because there are so many emotions and thoughts you don’t even realize you’re having. There are so many layers to it.
Even after you’re done with treatment, there are things that happen that change your perspective, and it’s so vital to have the right tools to cope with it. It’s something we don’t really talk about at the oncology appointments. I think my team brought it up once, but it’s not really something they suggest for people.
The doctors should push mental health more. I get it. They’ve got bigger things going on — like keeping you alive — but I do think it should be more incorporated in the overall care.
»MORE: Read different experiences of a cancer diagnosis and treatment
Paying for cancer treatment
When I was initially diagnosed, I was hospitalized. I didn’t really have a choice. I immediately went on short-term disability with work. Thankfully, because of the laws in place now, they can’t just drop you because of your insurance. I was able to keep my insurance through this whole process.
I have looked at a few of the bills before insurance covering them, and there was more than $200,000 in care. That’s just a few of them I randomly pulled out of our paperwork.
The second immunotherapy I got was free for me because it wasn’t technically FDA-approved. They wanted me to have it, and they wanted to use it for research and getting it through the approval process. God knows how much that would’ve cost.
My deductible is really high. It’s $10,000 a year, but after that they cover everything with little to no pushback. I’m so thankful because out of pocket during those 4 years, we spent $60,0000 of our own money. That doesn’t count a lot of the day to day. The hospital charges you for parking and things like that.
Thankfully, my husband and I were both very successful prior to this and saved a lot of money. Without that and the great insurance we had, it would’ve bankrupted us. I don’t know how people get through it, financially speaking, without draining savings and dipping into accounts that they don’t want to touch.
It scares me to death to think that someone may have to compromise their care because they can’t afford it. It makes me sick to my stomach.
My hospital had a good financial aid office. They had two or three people always there for financial assistance questions on the floor that I saw my doctor. My insurance company gave me an actual health care provider contact that I could call and ask questions. They were a case manager, I guess.
Without those 2, I don’t know how people figure this stuff out. It’s still so confusing. We threw away 100 pounds of paper this last year.
Be your own advocate
When I went to the Rehab Institute for my stroke, I was getting day passes all the time. Even if you’re not in the best shape, they’ll give you a pass so you can leave the premises and get outside. I was doing that a lot. I wanted to get out.
I shared a room with another girl. There was no privacy. There’s only a curtain between you. Whatever each of you is going through, the other can hear it all. The doctors just kind of dove into what was going on with you without too much regard for my privacy, so I would leave.
I had day passes, and we actually went home. My husband drove me home from the hospital because we only lived a few miles away. We hung out and watched movies on the couch.
It dawned on me, ‘Why am I sleeping at the hospital if I’m going home every day?’ I was still really messed up, but I was able to be at home.
As soon as the next Monday came, we went up to whoever was in charge that day and told them I needed to get out. She said she didn’t know if she could discharge me in time, and I said, “No, I don’t think you understand. I’m not staying here another day.” We explained to her that I’d be going home during the day and coming back to sleep.
I told her I’d do all the rehab every day and put in the work, but I was not sleeping there another day. That’s where the disconnect started happening. They were saying they weren’t sure if I was healthy enough for that, and I said, ‘No. I’m fine. Let me go.’
That was the only time I really felt like I had to fight for myself. I really didn’t want to be there anymore. My husband eventually said sarcastically, ‘We’re all very smart people here. I know if we put our minds to it, we can make anything happen.’
»MORE: How to be a self-advocate as a patient

Do you have any advice for someone who’s nervous about standing up for themselves?
Always speak up. Even if it’s nothing, whatever. If you get that gut feeling, always say something.
It can be a question or telling them that something doesn’t feel right. It doesn’t matter. Speak up.
Because my hospital was a teaching hospital, I’ve had pokes and prods where I’m helping the residents because they’re clearly learning. Even nurses who keep missing veins or something like that. Just be vocal.
You have to be understanding, of course, because they might not see you every day, but you know what your body is capable of.
It’s about taking steps to say, “Hey, maybe this way is the best way to do it,” in a way that doesn’t offend someone. That’s always better than getting poked 20 times and not saying anything.
Support & Survivorship
Do you remember the last time you went into remission? How did you feel?
For a long time, I kept waiting for the other shoe to drop. I was waiting for them to say the cancer was back a fourth time. I thought, “No way this works for real.”
I had a really aggressive cancer, and my body really likes making these angry cancer cells, so I thought, ‘When is it gonna start again?’
I held my breath for about 4 months after and then started to really accept the fact that maybe it did work.
I stopped checking my skin every single day or thinking that every single cough was something. I eventually got a little more comfortable, but I was a hypochondriac for a while.
How important was it for you and your husband to have outside support?
My dad was like a freaking rock. He would come see me every day he could. Even if it was only 10 or 15 minutes, we would talk or watch “Law & Order.” He was supporting me the best way he knew how, which was just being there. He would come take me to appointments if my husband couldn’t.
My mother-in-law was a freaking rockstar as well. She took me to several appointments and sat with me during infusions. Without those 2, I don’t know if we could’ve done it. I don’t know how I would’ve gotten physically to the appointments without them helping out when we needed it.

Did you feel like you could ask for help when you needed it?
It was extremely difficult for me at first, but when I had my stroke, I was completely reliant on everybody for everything. I’d have to ask my husband to put my bra on and everything.
After that, I was willing to ask for anything I needed because I knew I wasn’t going to get through it if I wasn’t going to ask. I tried to do things myself before the stroke, and it was already hard. After that, I absolutely had to have the help, so I learned to accept it and ask for it.
Was there any gift or service anyone gave to you or did for you that really stood out?
Blankets are always essential for the hospital. It’s so freezing in there, and they only give you the thin little blanket. It just doesn’t help that much. Definitely bring blankets with you.
There is one gift in particular that my friend gave me that stands out. I was in the hospital for 60 days straight at one point.
My friend went to Target or wherever and got a bunch of basic cotton shirts. She cut the entire side of them off and velcro-ed it back together. That way I didn’t have to ask the nurses to take out my IV if I wanted to shower.
I could just take the shirt off, wrap my arm, and shower. Before that, I would have to wait for someone to come unhook me. That was the best gift anyone could’ve given me in a million years. Having the independence to shower when I wanted to was awesome.
»MORE: What kind of support cancer patients say helped the most
The “new normal” after cancer
I kept going through my treatment wondering when my epiphany was going to happen. I kept waiting for an ‘a-ha!’ moment.
I asked my therapist this, too. “When is my big lesson coming?” Finally, she told me, “You haven’t had one big moment. You’re having a lot of little ones. Your perspective has shifted so much, and you don’t even know it.” She’s right.
I didn’t have this one big moment per se, but I had a lot of little shifts over 4 years that made me realize that all the physical stuff we have in this life doesn’t matter. It’s all dumb. Yes, it makes you happy for like 10 minutes, a couple of days, or maybe a year, but it all doesn’t really matter.
What is your advice for someone who has just been diagnosed?
Just breathe. It’s going to be okay. You and your body are so much more resilient and strong than you think. Your body can withstand so much and recover.

There is a whole other level you can dig deep and find that can get you through anything. You just have to be open to it. You cannot get through it without digging really deep sometimes and knowing that you can get through it.
Do you have a message for anyone reading this?
My name is Casey, and I had acute lymphoblastic leukemia. My message for you is to keep moving your body. I equate the body to the tin man. If you don’t keep moving it, it will eventually freeze up.
You have to keep your body lubricated by moving it. Sometimes that’s the best way to heal — through movement. You are able to tap into a deeper source of something inside of you, and it can almost be therapy.
Inspired by Casey's story?
Share your story, too!
Acute Lymphoblastic Leukemia (ALL) Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)



