Anna’s Ph- B-Cell Acute Lymphoblastic Leukemia Story

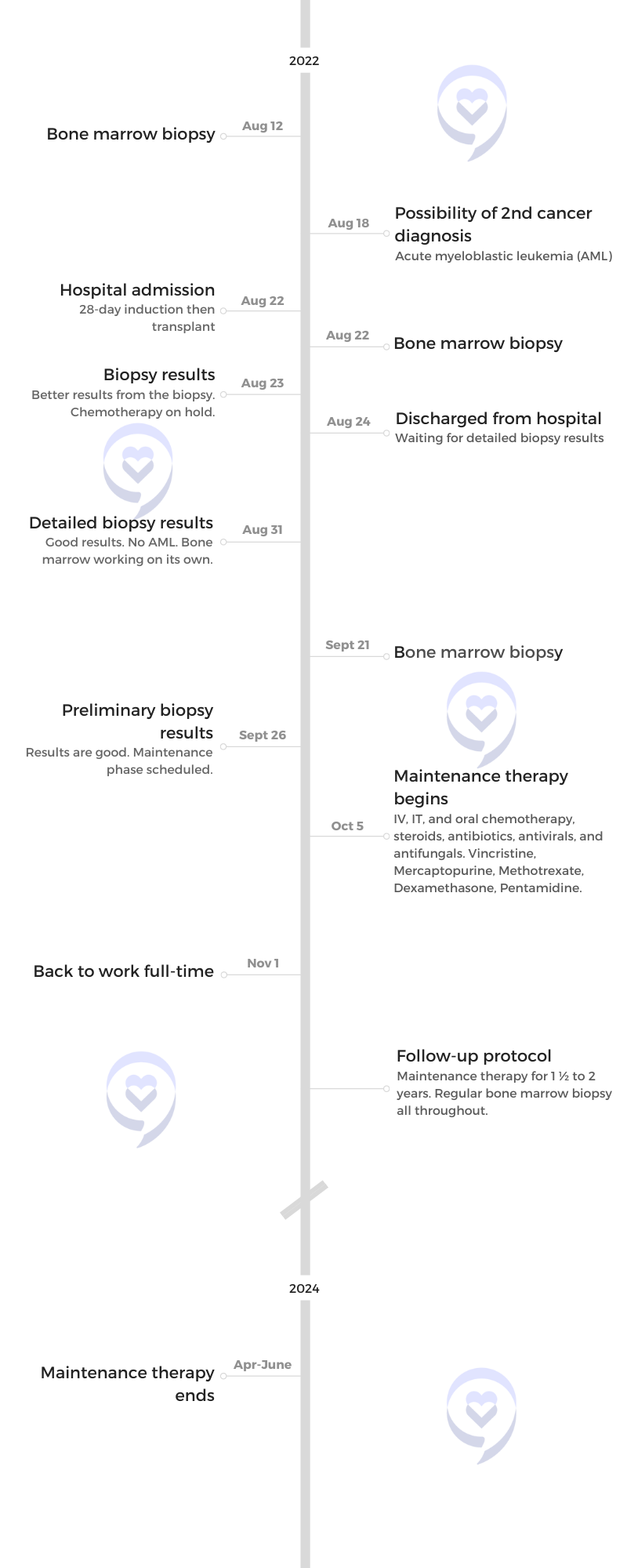
Anna was diagnosed with B-cell acute lymphoblastic leukemia (ALL), Philadelphia chromosome-negative, five months after she moved to the US to marry her husband.
She shares her journey of going from the ER to being airlifted in a matter of hours to a different city for treatment, navigating the US healthcare system, getting a serious infection that resulted in an electrolyte crash, and coming close to a second cancer diagnosis.
- Name: Anna T.
- Diagnosis:
- B-Cell Acute Lymphoblastic Leukemia (ALL)
- Ph- (Philadelphia chromosome-negative)
- Symptoms:
- Heavy period for a few hours
- Fatigue
- Fever
- Sweating
- Mysterious bruises on legs
- Treatment:
- ECOG 10403

- Pre-diagnosis
- Diagnosis
- Treatment
- Plans after cancer treatment
- Words of advice
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
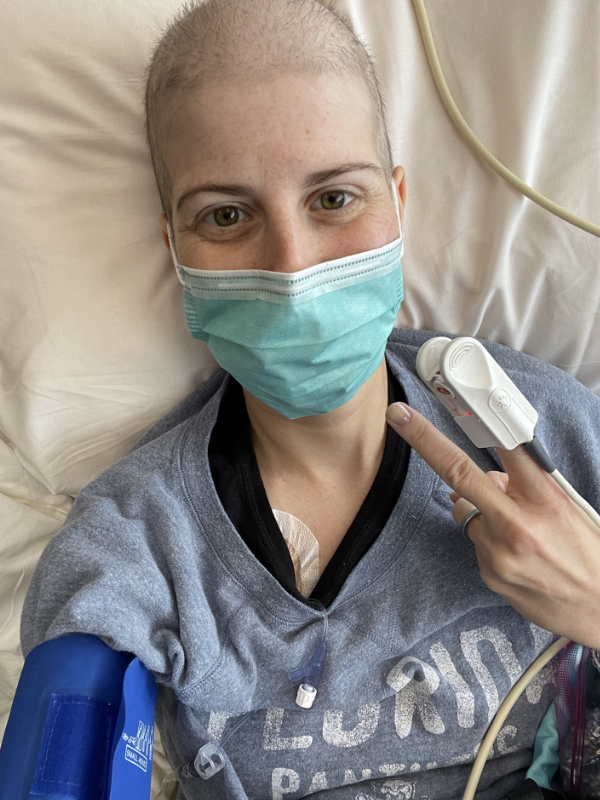
I was diagnosed five days before Christmas so I spent Christmas and New Year’s Eve in [the] hospital.
Pre-diagnosis
Introduction
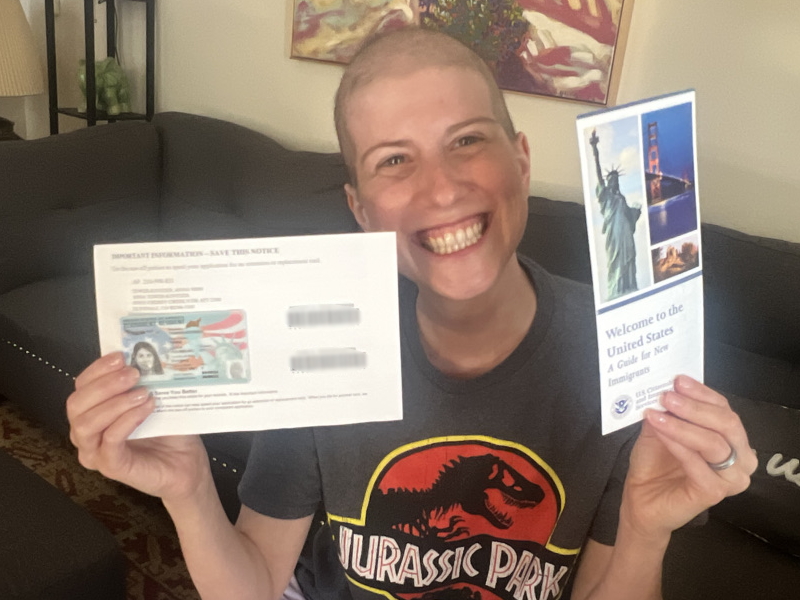
I’m originally from Hungary. I moved to the US [in July 2021] to marry my husband. Five months after moving here, I was diagnosed with leukemia. Since then, it’s [been] a crazy, crazy year.
I’m a communications specialist. I work for a nonprofit in Durango, southwest Colorado. [I’ve worked] in public relations and marketing my whole life. I’m a former university lecturer.
I really like outdoor activities — hiking, biking, mountain biking, running, walking outside, winter sports rafting — everything which is active and outdoors, I am a fan.





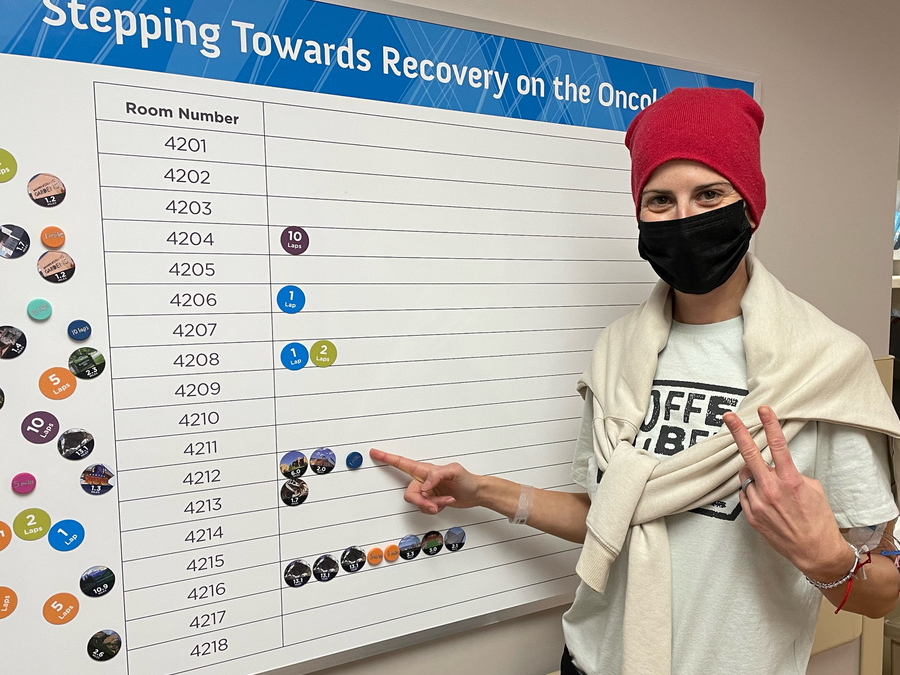
I was diagnosed five days before Christmas so I spent Christmas and New Year’s Eve in [the] hospital. The first time, it was 37 days inpatient.
I’m taking it day by day. Sometimes I’m just in survival mode [and] sometimes I feel better, but this is how it looks right now.
Initial symptoms
I was always healthy and had a healthy lifestyle. I was very active. I was very aware of what [I was] eating. I tried to sleep a lot.
I got COVID [in] Halloween [2021] and one and a half [weeks] later [during] a long weekend in Chicago is [when] my symptoms started.
I worked a lot in Chicago. On the third day, I started to feel very fatigued. [While] I was in a museum, I felt that I might have a fever and I had to sit for a little [while]. Just out of the blue, I was very under the weather.
Then I had my period and for a few hours, it was very heavy, which was not normal but I considered, We just [flew] to Chicago from Colorado. We woke up early. We walked a lot so probably that’s why. Then we went back to Durango.



That week, I felt feverish every night. I was out of breath after washing my hair [that] I had to sit down. I had night sweats, which was also very new to me.
I went to [the] urgent care finally because I had mysterious bruises all over my legs. I [had] a massage before that and I was thinking, Oh, maybe it was a little strong. All these symptoms for a healthy person, you just feel something is not okay so I went to the urgent care. It was a Sunday afternoon. I spent three hours. They took a full blood panel and told me that someone will call me from the hospital.
[That] same day [at] 9 p.m., the head of the emergency unit in the Durango hospital called me that my blood numbers looked really [bad] and I should be in the hospital. I should pack a bag because I would stay. My husband should come with me and it shouldn’t take longer than an hour.
I obviously freaked out. I didn’t really know what was happening.

I rushed into the ER. Ten minutes after my arrival, they told me that 80% [chance] it’s leukemia. I was like, “Okay, but what’s the other 20?” I still was optimistic. “I don’t care about that 80. What’s the 20?” And the doctor just said, “No, it’s leukemia.”
I was airlifted to Denver at 3 a.m.
My white blood cells [were] very, very high. My platelets [were] very, very low. I was anemic and actually, I needed blood products to be able to be admitted because I wasn’t stable at all.
They told me [that] if I didn’t go to urgent care, [in] one [or] two weeks, I may not be here anymore. It’s crazy.
[At] 9 p.m., the head of the emergency unit in the Durango hospital called me… I should pack a bag… My husband should come with me and it shouldn’t take longer than an hour… I was airlifted to Denver at 3 a.m.


Diagnosis
Reaction to the diagnosis
Immediately, I was crying. I told my husband I don’t want to die. I told him if he doesn’t want to do this with me, then he doesn’t have to. And he said I’m stupid and I should stop. I was in shock, honestly.
It was really hard because first of all, I was only in the country for five months. We just got married. Everything was new. The language was new. All these medical terms and everything is just new. It’s not easy even in your own language, but in another, it’s like, “Sorry, what’s that? What’s that? What’s that?” So I was in shock, freaked out, and scared. But you cannot really do anything.
I felt lucky they caught it and they were so prepared. After I was airlifted, I met with my oncologist [for] the first time at 5:30 a.m., half an hour after I arrived [at] the Denver hospital. He’s amazing. I [felt at] ease and relieved that, “Okay, I’m in good hands. I have a good doctor and he will cure me.”
Reacting to a cancer diagnosis: How cancer patients feel in the moment »


At that point, we didn’t know the exact diagnosis. We just know that it’s leukemia but didn’t know the type. After I got my exact [diagnosis], besides asking, “Why me? Why now? What did I do wrong?” stuff like that, I felt that we have to accept and we have to fight.
I never considered a death sentence. I was like, “Okay, it’s one of the biggest challenges in my life. If you paused everything, my life and our life will be delayed. But I’m going to do this and I will fight.” I think that was key that I accepted it and I tried to be positive.
When I heard leukemia, I also saw that it’s one of the worst blood cancers. They [said] that 10 or 15 years ago, it was kind of the worst and there was no cure. But treatments and research are improving day by day so it’s not the situation now.
Initial appointment with oncologist
They found the oncologist for me in Durango. My doctor goes to Durango to care [for] patients there so they [found] him for me.
When I arrived at the hospital, we did a bone marrow biopsy. Then the next day, I had the exact diagnosis. My doctor said I can have a second opinion if I would like to, but I don’t really have time for that. So [there] wasn’t really an option to choose another doctor or to think about that.
I read really good reviews about him and all of it was true because he’s amazing and I feel very lucky. Colorado Blood Cancer Institute and the Presbyterian/St. Luke’s Medical Center are amazing so I really feel lucky. Everyone says that if you have to be somewhere with blood cancer, then this is the place you want to be.
I was so worried that I didn’t have time to think about that so it wasn’t like for a lot of people. They got the diagnosis and then, “Okay, let’s find a doctor. Let’s find an institute.” It was given but I feel lucky because it’s awesome.





Treatment
Outlining the treatment plan: ECOG 10403
First, he [drew] the treatment plan. He told me what will happen. He told [me] it’s a three-year-long treatment. I freaked out because I thought [it will be] half a year and I can forget about that. So when he [said] it will be three years, I was like, “Sorry, what?” That was really crazy to hear.
Then he told me I will do [an] induction phase where [the goal] is to get in remission because I had 95 or 98% cancer cells in my bone marrow, which is pretty high.
He told me what kind of chemos I will get, what kind of medications, and all the side effects, which he had to list. I was very scared about staying at the hospital for 30 days. It became 37 days because your numbers have to increase a little before they let you out.
The treatment [included] an induction phase, consolidation, and maintenance. The consolidation phase has three different courses or cycles.
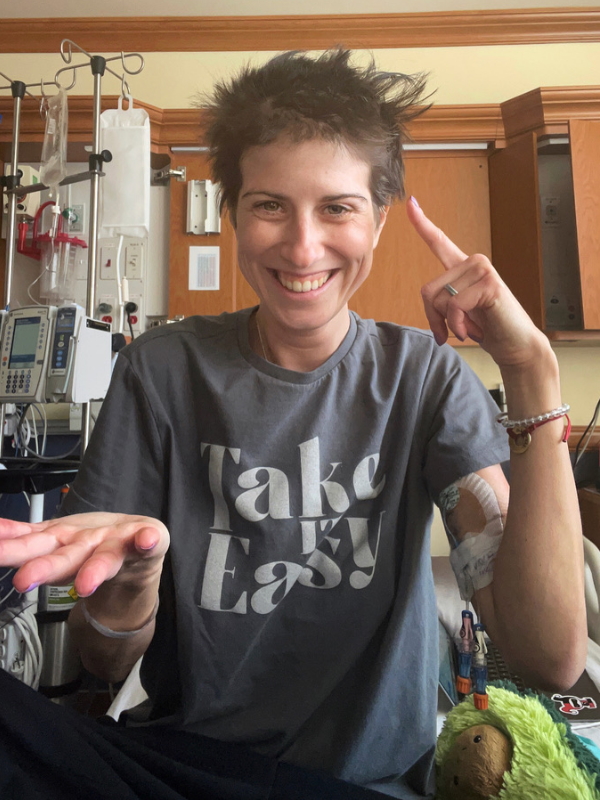
I was very scared about the side effects. I was like, “Oh my God, I have to get in remission.” But besides staying in a hospital, it was one of the easiest parts, I would say.
Induction phase
It’s a pediatric treatment, which they used first for children [and] young adults also get it. I get five different kinds of chemotherapy via infusion. I got steroids every day, which was probably the worst part considering the side effects because it just makes you totally immunocompromised. It makes you totally fatigued. I lost all of my muscles so I was weak.
I had lumbar punctures and IT (intrathecal) chemos, which means they put chemotherapy into your spinal fluid. I had one bone marrow biopsy [on] the first day and another one on the 28th day. Sometimes, blood transfusions and other blood products [were] needed. I have anti-viral tablets and antibiotics every day.
Consolidation phase
I came home. I had two weeks off — one and a half [to] two weeks off — and then I went back to the hospital for a week for the consolidation part.
Consolidation is separated [into] three different parts and almost every part, I had to go to the clinic for a couple of days or a week to see how [I would] react to the different chemos. I got infusion chemos, oral chemos, lumbar punctures, blood transfusions as needed, and sometimes steroids.
I got [an] infection once during the summer… I couldn’t eat and drink anything for ten days so I lost 15 or 20 pounds in 10 days.

After two weeks, I went back to the hospital for a week. I [got] my port inserted, which I still have, and I got everything through that. I got a new type of chemo so they wanted to check how I [reacted].
The second part, which we [also] separated [into] three different parts, lasted until August. I considered this the hardest [part]. I had pretty bad days and weeks.
I got [an] infection once during the summer, which was severe diarrhea and I got dehydrated so I spent eight days in the hospital and I thought, I’m gonna die. I had [an] electrolyte crash and that was very, very scary. I kind of saw myself already in the ICU, in a coma, and I couldn’t eat and drink anything for ten days so I lost 15 or 20 pounds in 10 days. It was one of the craziest [things]. Then I got a little time to get better after the infection.




Possibility of a second cancer
We then [had] a panic situation because I had a bone marrow biopsy and my doctor called and told me I developed another type of leukemia. I have 50% blasts in my bone marrow and it seems I developed AML — acute myeloblastic leukemia. I had to go to the hospital again for a month and [I was told I] will need a transplant. [That] was a Thursday and they scheduled the hospital stay for Monday.
I went to the hospital. I had another bone marrow biopsy and we were waiting for the results to start the chemo the next day. The doctor came into my room to tell me that the bone marrow biopsy looks better and [we’ll] put a hold on starting chemo for another day. The next day, they discharged me because they said another result came back and it seems better.
All in all, we waited [for] two [to] four weeks [and] checked how my bone marrow [was] doing on its own. I had lots of blood tests.
I didn’t develop another type of leukemia, which was amazing. When they are in a growing phase, these blasts can seem like cancer and they probably [caught] them [at] the wrong time. But I don’t wish [those] one and a half months [for] anyone because it was crazy.
Find out how cancer patients and survivors cope with scanxiety »

I felt that I’m not strong enough to do this again… I felt so tired mentally and physically.

Reaction to a possible second cancer
My first question was, “I did the last eight months for nothing?” My doctor said, “No, you would be dead if you wouldn’t [have] so it was for something.”
I remember I just cried. My husband [held] one hand and the doctor [held the] other and I was just crying and sobbing. I just couldn’t understand how I got this or how unlucky I [was].
I was also shocked [at] these cancer cells. They said they rotated to this other type, which is not targeted by the chemo I got, because they felt attacked. I was surprised that, “Oh, it’s a thing and it can happen. Wow.” I was totally shocked.
That day, my husband and I were just crying. I just couldn’t believe that it can happen again. I started to think about the transplant. I started to think about another month in the hospital, which I really didn’t want. I was shocked, to be honest, and I felt I’m not strong enough to do this again. Even if somewhere deep inside I knew [I would have to], I cannot give up, it’s not how it works. But I felt so tired mentally and physically [and] I just didn’t know how I [would] be able to do that.
It was amazing but also so many days and weeks waiting and the uncertainty was also like, “I just want to know something. Even if it’s bad news, I just need to know something.” But [thankfully], it wasn’t so.
We waited when I was discharged. I had weekly blood tests and we saw how my bone marrow was doing on its own. Then I had a repeat bone marrow biopsy months later. It was another two [to] three weeks waiting for those results. I got the preliminary results quite fast, in maybe a week, but we were still waiting for detailed results [to find out] if there is a mutation or stuff like that. But everything seems good.


Maintenance phase
The maintenance phase seems to be the phase when people go back [to] work full-time. They kind of have a normal life. If everything goes well, you don’t have to stay in the hospital. But it takes one and a half [to] two years so it’s not a short thing.
It was one infusion of chemo monthly, oral chemos every day, lumbar punctures, [and] steroids once a month for five days so I wouldn’t say it’s easy. So far, the last three weeks [were] pretty good. I could exercise, I could walk, I could work — I could almost function as a normal person. But my numbers are dropping and my liver numbers are elevating, which is the result of one of the chemos so hopefully, it will stay on this level. Then I can do the next one and a half [to] two years [on] this level.


Side effects from chemotherapy
It could be vomiting, nausea, fatigue. You could have rashes. You could have fevers. My doctor told me, I [could] get any kind [of] infection. I can have that so-called moon face [when] your face gets a little moon-ish. You have a bigger belly but everything will be so skinny so it’s kind of weird. I didn’t have that.
I was thinking about my marriage, too. Oh my God, how will I look? And also hair loss, which was a big thing for me, too, which I think I handled better than I thought. All of these [symptoms,] it’s just so scary.
It wasn’t that bad [because] I didn’t get [an] infection. I didn’t vomit even once. I didn’t have moon face. I didn’t get rashes.
I became fatigued. There were days when even [taking] a shower was a challenge. I had some headaches and nausea from lumbar punctures because the first two, they did it with a bigger needle. Since then, they changed it to a small one and I [didn’t] have any problems. But the first two, [I got] pretty intense headaches and nausea after.

I had a good appetite. I do believe that food and drinking water is very important, too, to have [fewer] side effects and to be strong. I felt pretty lucky. I didn’t have mouth sores, which they said might happen. I could eat. I was hungry. Tastes didn’t change that [badly].
I could work almost every day so I felt kind of okay. There was one day, January 1st in the morning, when I passed out — probably blood sugar. It was scary for my husband and the nurses [but] not for me because I [didn’t] know about that.
I did really [well] in the first month and I achieved remission, which was amazing. I felt pretty good. The nurses, all the doctors, the hospital itself, and the food [was] amazing so I didn’t [feel] bad there, even if it sounds weird.
Learn more about the common and not-so-common side effects of cancer treatment »


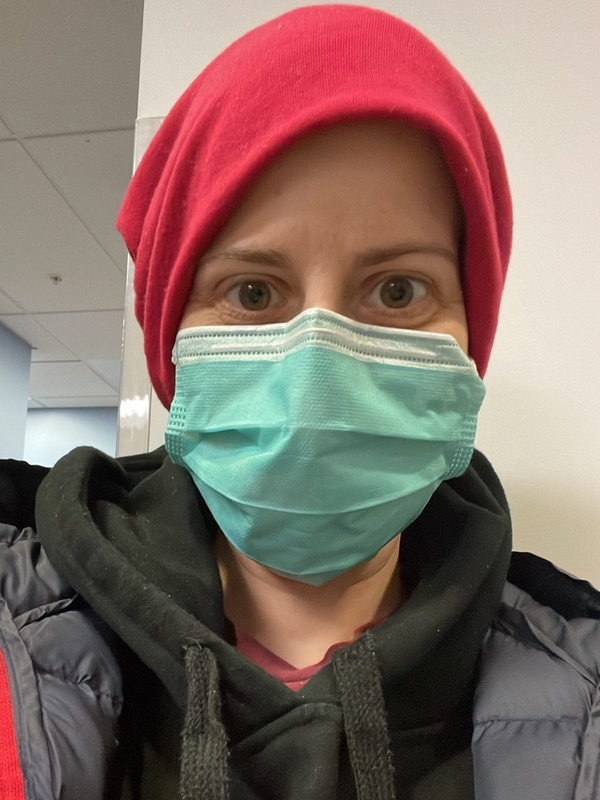
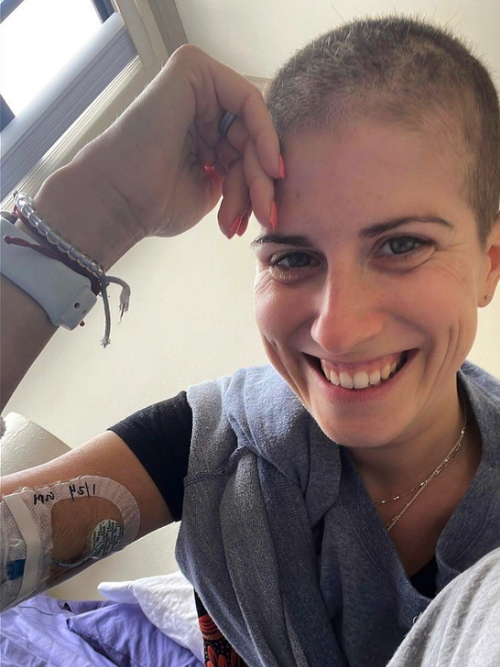
Hair loss
I had long hair. I asked five different doctors on every visit, “Will I lose it or not?” Then I discussed with my husband that I would just cut it shorter so I wouldn’t wait until it’s falling and have hair on my pillow when I wake up and everywhere. So I asked everyone to be sure that I will lose it. And when they said I will, [so] I cut it short.
When it started falling [out], that’s when we shaved it. When I looked into the mirror, that was the first time I started crying. My husband shaved it then he showed me the mirror and I started crying but that was it. I started to wear beanies when I was out of the hospital room [or] on the floor working.
Two days later, I looked into the mirror and I was like, “Okay, it’s a sign of the fight,” and I will be not proud of that, but I will just accept that. Since at that point, I was totally fine.
I thought I will freak out when I cut it but that didn’t happen so it was great.




Working during treatment
I stopped working for three months, but after, I went back part-time but remote. Now I’m going back full-time, [fully remote]. That’s pretty important because even if I feel okay and my numbers are kind of good, there is no guarantee that I won’t be immunocompromised through this whole journey. And at that point, I cannot be with people so that’s important.
Can I work during chemo or radiation? »
Importance of a strong support system
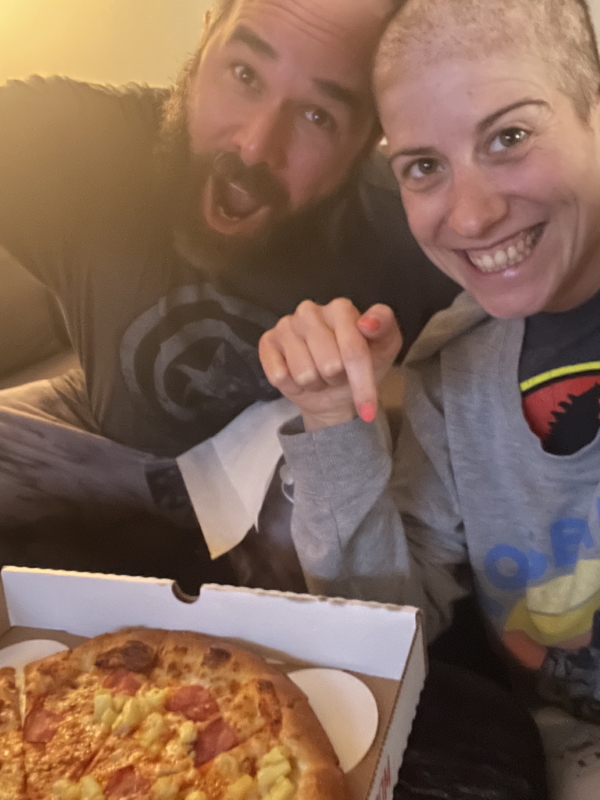
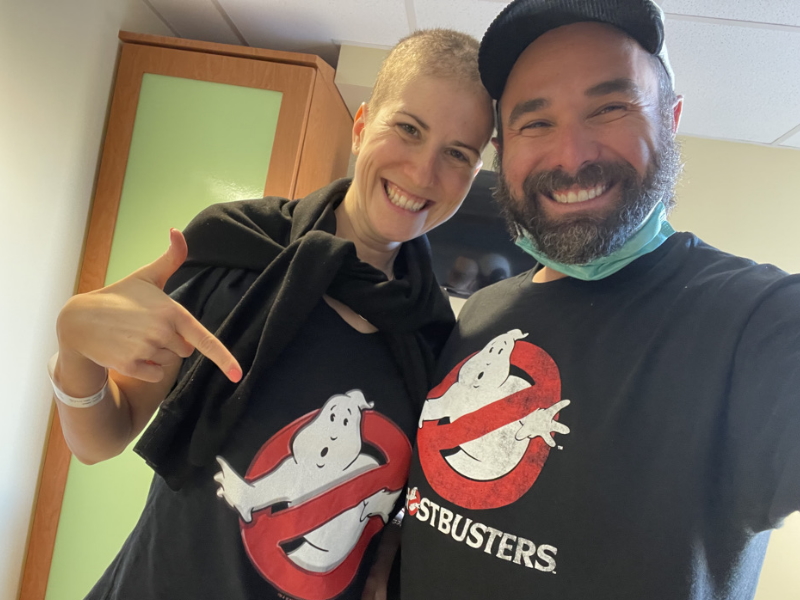
[My husband], he’s amazing. He’s with me 24/7. He has different types [of] remote jobs so he finishes one then continues [with another] to be able to be with me all the time.
He helped me shower. After I [got] out of the hospital, he made me breakfast. He did my laundry. He was there with me every day. He sometimes stayed nights in the hospital. He came every morning [and] sometimes got my food. He was working from there just to be with me. He was there for every important appointment. He was just amazing.
In the hospital, you have to talk to the doctors and nurses about every symptom, every bathroom visit, every period — sometimes in detail. It was really weird to talk about this kind of stuff in front of my husband. Even if we are best friends, even if our relationship is amazing and we can talk about everything, after five months [of] being married, bathroom visits and period details [are] not the kind of stuff you want to talk about. But I can say we became stronger and it wasn’t even a [big] deal. It was big for me at first but not for him.
Three things to remember when your spouse or partner is diagnosed with cancer »


Even if our relationship is amazing and we can talk about everything, after five months [of] being married, bathroom visits and period details [are] not the kind of stuff you want to talk about.
He’s just amazing. I don’t know how he does it. I was never in a caregiver role and I think it’s one of the hardest. Patients have to survive. They have all the pain, the treatments, and everything they have to deal with, but caregivers feel helpless seeing their loved ones. They also have to work, do stuff around the house, and handle insurance, which was also a big deal for me. When I [got] to the hospital, my insurance didn’t cover this doctor and this hospital so we had to change it and it wasn’t easy.
Caregivers have to be everything. Their life doesn’t stop. He’s amazing and I feel pretty lucky.
Cancer treatment is not like in the movies. And I think lots of people like, “Oh, yeah, so you vomiting 24/7 and you are just totally down and you cannot do anything.” And I’m not saying it’s not happening or it cannot happen and every person is different, but it’s not always the case.
He had to go through all of it. I’m not saying it was easy because it’s probably harder for him than me, to be honest, to see your loved ones getting through this and you feel helpless and useless.

Caregivers have to be everything. Their life doesn’t stop. He’s amazing and I feel pretty lucky.



Understanding medicalese as a non-native English speaker
I feel lucky because my husband was with me all the time. [In] the beginning, when the doctors came in and they [talked], sometimes I had to discuss it with my husband after. “Okay, so am I right? Am I correct? This is what they said, right?”
But I think if they have problems or concerns, then maybe they can record the whole discussion with the doctors if they are okay with that. Then you can just listen back and that can probably help. Recording can be helpful.

Plans after cancer treatment
[Some days], I don’t feel that good. [Some days], I’m almost normal-ish. I’m a little more tired than before my diagnosis. Sometimes I need a nap during the day. But I was in the gym three times a week. Sometimes I walk six miles a day. I could do everything around the house. I cannot clean [but] I did my own laundry [and] my own food, which I couldn’t do previously.
I only worked part-time but [I’m going] back full-time. I work remotely so that’s good.

I don’t think I can really plan or really want to, to be honest, because I feel you cannot really. I just realized that anything can happen at any point so I feel, let’s just do everything day by day.
Obviously, I would be really happy if everything would stay like this, that my numbers are kind of okay. I’m not immunocompromised so I’m able to go to a restaurant and have lunch or I can go to a gym when there is more than one person. That would be amazing. But I don’t think I want to plan.
The only good thing [is that] probably from the beginning of next year, I won’t have weekly blood checks, just monthly. If I have to go to the clinic only once a month, that is amazing. That’s a huge difference.


Words of advice
There will be probably three things [that] I would suggest to anyone.
First of all, do not stress about anything. If it’s not health-related, there is always a solution. You can always change. I did the same. I was stressing about the deadline [at] work or having a call with my boss. Just little things. “It’s raining again and I wanted [to] run and I cannot now.” These are not the things. This is nothing so it’s not worth it.
Second, enjoy life as much as possible and surround yourself with people you like. And say no because this will be fine. Be selfish and do things [that are] good for you.



Third, which is probably the most important, [is] to go to yearly checkups. If you feel something is odd, that something doesn’t feel good, just immediately go because it can actually save your life. I think that’s one of the most important things.
I didn’t need to go to the doctor that often so I cannot say that it was a frequent thing. But if I felt something is probably not okay, then I went. Like I said, I was really active and I know my body so I always tried to listen to that. And I think that’s also important: get to know your body and know when it says something.


Inspired by Anna's story?
Share your story, too!
Acute Lymphoblastic Leukemia Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)



