Sophie’s Stage 4 Bowel Cancer with BRAF Mutation Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

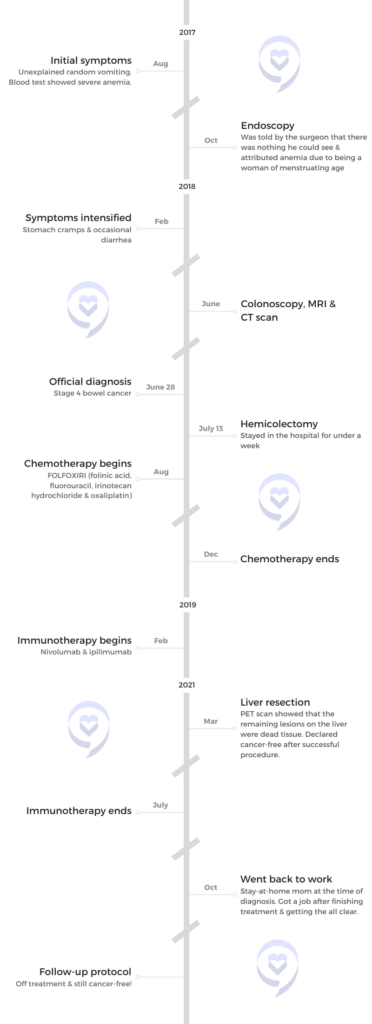
Sophie was diagnosed with stage 4 bowel cancer after experiencing symptoms for almost a year. Initially thought to have Crohn’s disease, her condition was finally identified after having a colonoscopy, a CT scan, and an MRI. The diagnosis revealed multiple lesions and a significant tumor, leading to a hemicolectomy.
Post-surgery, Sophie underwent aggressive FOLFOXIRI chemotherapy due to her BRAF mutation, enduring severe side effects like neuropathy, extreme fatigue, and significant weight loss. Despite the grueling treatment, the initial response was positive but when the chemotherapy failed, her oncologist pursued a different approach with immunotherapy drugs nivolumab and ipilimumab.
The immunotherapy had manageable side effects and led to significant improvement. After two years of treatment, Sophie was declared cancer-free following a PET scan and liver surgery biopsy confirming the absence of cancerous cells.
- Name: Sophie U.
- Diagnosis:
- Bowel Cancer
- BRAF
- MSI
- Staging:
- Stage 4
- Initial Symptoms:
- Vomiting
- Anemia (found in blood test)
- Treatment:
- Surgery: hemicolectomy
- Chemotherapy: FOLFOXIRI (folinic acid, fluorouracil, irinotecan hydrochloride, and oxaliplatin)
- Immunotherapy: nivolumab & ipilimumab
I went to my doctor because I felt something wasn’t right.
Introduction
I’m from Warwickshire, England, and I was diagnosed with stage 4 bowel cancer in 2018.
I’m married with two kids and I currently work in Motorsport.
Pre-diagnosis
Initial Symptoms
It was a Monday night. I went up to bed and vomited all of a sudden. There was no reason for me to be sick. I’d eaten nothing suspicious, so it seemed a bit off.
It didn’t happen again until nearly the weekend. It was a bit strange because it was a single occasion both times. It happened again the week after, but it came out of both ends this time, so I thought I’d eaten something bad.


The following week, I went to my doctor because I felt something wasn’t right. I wasn’t vomiting a lot, but it didn’t seem normal. The doctor ran some blood tests and then we would go from there.
She called me the next day and told me that I was so anemic, she wondered how I was still walking. I was almost at the point where I needed a blood transfusion. My son was two then and wasn’t a good sleeper, so I was always tired.
In hindsight, they thought the tumor had gotten so big by that point that it was stopping food from going down. Before that, I hadn’t noticed anything.
Luckily, I had a great GP. She wanted to get to the bottom of things and was willing to go the extra mile.
Unfortunately, I didn’t have any typical symptoms, so that led us down a different path, thinking it was a stomach issue. We tried an elimination diet because we thought it might be an intolerance. She referred me to have an endoscopy, which showed nothing. We did all kinds of things, but that was it as far as symptoms for the first few months.
I was in a lot of pain. My stool wasn’t bloody, but it looked red.
Symptoms Intensified
When we went to Disneyland Paris in February, I was getting bouts of diarrhea. It wasn’t consistent, but I was in a lot of pain. My stool wasn’t bloody, but it looked red.
When I got back from the trip, I told my GP. I went to see her for something else but told her what I noticed while on our trip. She said, “Now I can refer you to the inflammatory bowel clinic because it’s moving towards that. It might be something like Crohn’s or colitis.”
It takes a while for the referrals to go through. That was February, but I didn’t see him until April or May. He was convinced it was Crohn’s disease, so he wanted to get all the tests done to get them out of the way and confirm the diagnosis so we could move on.

Colonoscopy & MRI
He ordered a colonoscopy and an MRI. That ended up happening in June. I had the colonoscopy on a Friday and then the MRI the following Monday. By this point, my stomach pains were getting worse. I couldn’t eat much because I wasn’t keeping anything down.
The colonoscopy was so painful. I didn’t realize what was going on at the time because I was under a lot of medication. I could see it on the screen, but I didn’t know what I was looking at although I knew something looked different. They said, “There’s a lesion and we can’t get the camera past it, so you have to talk to your doctor.” I didn’t know what lesion meant. I thought it was a cut or something. I started searching online, but cancer wasn’t in my mind at all.
It was a relief in some way to know that there was something wrong with me. I just didn’t want it to be that.
Diagnosis
Getting the Official Diagnosis of Stage 4 Bowel Cancer
They didn’t tell me at the time what it was. They called me the next day and said I need to have a CT scan before I see the doctor on Thursday. I thought it was another thing to get done.
I was really sick at that point, so I asked my husband to come with me. At no point had we’d been thinking it was cancer, so no one told me to bring him with me. He came because I couldn’t physically move. I had my CT scan then we walked to the IBD doctor and that’s when he told us.
They staged me at stage 4 bowel cancer. I did all the tests for Crohn’s disease, so they could see where it spread. There were multiple lesions in my liver, all throughout my torso, and a lot of my lymph nodes. No other organs. The tumor was tennis ball sized.


Reaction to the Diagnosis
To be honest, it was a massive shock for it to be cancer because I thought it was Crohn’s disease. It was a relief in some way to know that there was something wrong with me. I just didn’t want it to be stage 4 bowel cancer.
It wasn’t the IBD specialist’s area of expertise. He hadn’t had to give that kind of news before, so I don’t think he handled it in the best way because he didn’t know how to say it. It was delivered in quite a shocking way. He wasn’t an oncologist, so it wasn’t very sensitive, I guess.
The tumor was so large that it was almost cutting off my bowel and that’s why I was being sick.
Treatment
Hemicolectomy
I was told that I’d be assigned an oncologist and have a multidisciplinary (MDT) team. They were going to meet with me the following week and come up with a plan, so I didn’t get to speak to my oncologist until the week after. He said I was going to have surgery first because the tumor was so large that it was almost cutting off my bowel and that’s why I was being sick. Nothing was getting through. He said, “For you to get through any chemo, we’re going to have to get rid of this first.”
The surgery was called hemicolectomy and it happened the week after, around 10 days from when I was told I had cancer. I was in the hospital for about a week. It was quite “messy,” they said. It spread back towards my spine and wrapped around blood vessels. They removed a few lymph nodes and had to cut off part of my stomach because it attached itself to my stomach. It was quite a rough recovery, to be honest.

FOLFOXIRI Chemotherapy
I was told that I’d be put on the strongest chemo they could throw at it. Because of my age, they thought I could handle it. They were able to do a biopsy and found out that I had a BRAF mutation, which is very aggressive and has the worst prognosis of a bowel cancer diagnosis but because of that, they could also add another type of chemo.
The median survival rate of stage 4 bowel cancer is 8 to 12 months. My doctor didn’t know anyone with a BRAF mutation who survived. It’s known for not having good survival statistics, especially back then. More recently though, a lot of people have been living a lot longer because they’re finding out different treatments for it. It’s still not a great diagnosis, unfortunately.
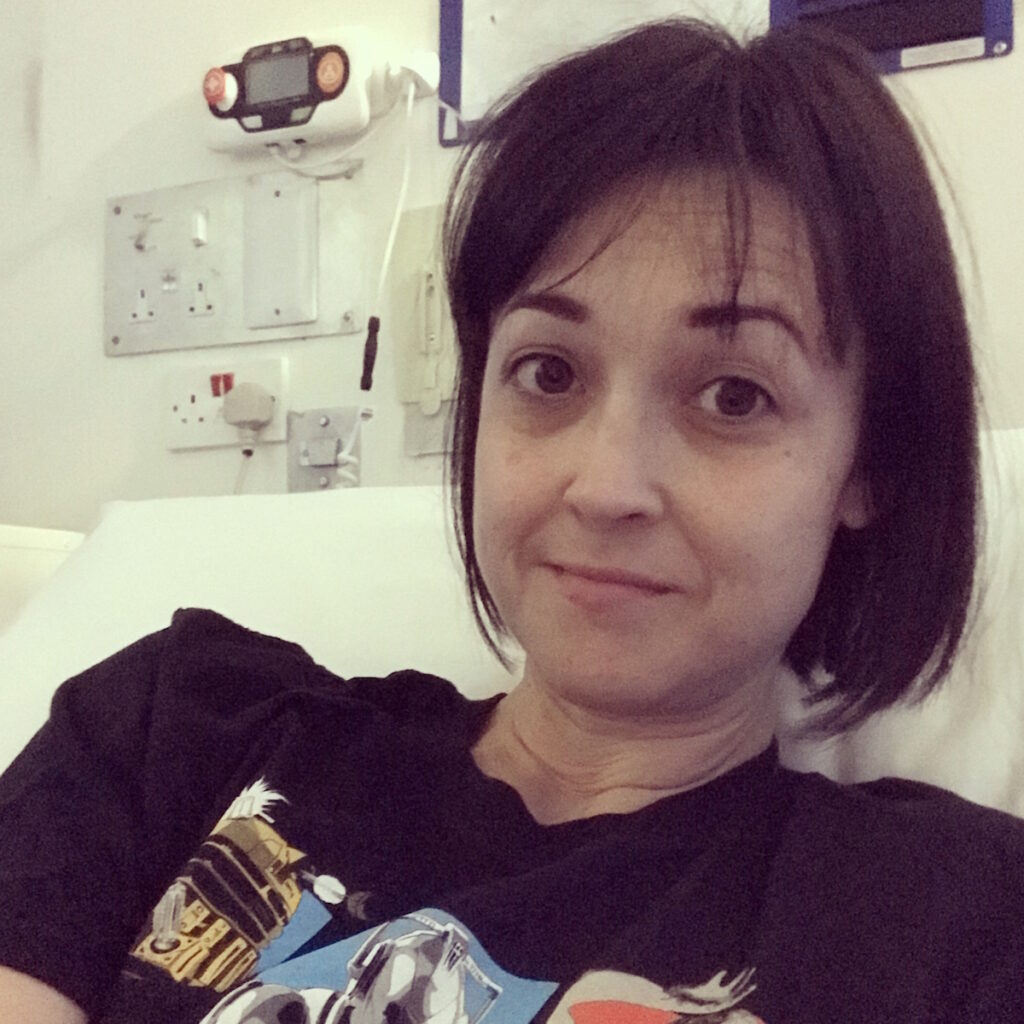
I had a portacath fitted because they said the chemo was too strong to have in my veins. I had that done about three weeks after surgery and then a week after that, I started my chemo.
I was put on FOLFOXIRI, which is a combination of FOLFIRI (folinic acid, fluorouracil, and irinotecan hydrochloride) and oxaliplatin. I would go to the hospital and have an infusion for about six hours. I would come home with a pump attached to me that would stay on for the next 48 hours before I go back and have it removed.
Chemo was the most horrific thing I’ve had to go through… I was probably just surviving by the end of it.
Side Effects of FOLFOXIRI to Treat My Stage 4 Bowel Cancer
It was rough on me. During those 48 hours, I was horribly sick. The first cycle wasn’t too bad, but I was sick a lot. I also recently had bowel surgery, so they were expecting that. I had bad diarrhea. I was very tired all the time. It progressed because the side effects from the chemo were cumulative.
The oxaliplatin also gave me neuropathy. My feet weren’t so bad. I was having chemo over winter, so my hands were like needles and on fire. I couldn’t put them in the fridge.
They reduced the amount of chemo I was getting and extended my time, so I ended up being at the hospital for eight hours plus the 48 hours after. Honestly, chemo was the most horrific thing I’ve had to go through.
I lost my appetite and my taste of things. I lost a lot of weight. I was probably about 40 to 50 lbs lighter. I couldn’t eat anything. Nothing tasted like anything. Bread and pizza were like cardboard. I was probably just surviving by the end of it. I was living off nutrition drinks.

I had such bad brain fog that I couldn’t even talk to people anymore. I would try and say something, but I would forget what I was saying mid-sentence and be so exhausted that I couldn’t be bothered to correct myself.
I would sleep most of the time. My kids at the time were 6 and 3. My daughter was at school, but my son was at nursery. They were lovely enough to take him on for additional hours so I could sleep all day.
For the two days I had the pump at home, I would not be able to keep anything in my body. By the end of it, it was coming out both ends horrendously. I couldn’t leave the house because I had to be near a toilet all the time. I couldn’t even drink water at the end because it was like everything was being rejected.
I didn’t lose my hair, but it did thin quite a bit. I lost a lot of muscle. I melted away and became weak like an old lady. It was horrible because I couldn’t do anything for myself. I couldn’t look after my kids and that was the hardest thing.
One thing I wish I’d done is accept help more and ask for it… I was exhausting myself.
I wish I’d known that it affects everyone differently. If you go on social media, you see people dancing around their chemo poles. I couldn’t even stand up, let alone hold my phone to make a video or take a photo. I was asleep all the time. If I’d known that there were people like me, then I probably wouldn’t have felt so bad.
One thing I wish I’d done is accept help more and ask for it. People always offered to help. It’s hard to admit that you need help, but at the same time, I realized I should have done it because I was exhausting myself.
I only had eight cycles in the end. I was supposed to be on it indefinitely, palliatively. My first scan showed that it shrunk a lot. In bowel cancer, some of the CEA is measured and with me, it was a good indicator of how things were going. When I was first diagnosed, it was off the charts at around 7,000. The chemo got it down to 650 after my first scan. After that, I went downhill rapidly.
I had my last chemo session on New Year’s Eve 2018. The week after, I ended up in the hospital because I couldn’t eat anything or keep anything down.


Immunotherapy
We had time between having surgery and starting treatment, so my husband was looking into what else we could do. He read about immunotherapy and that it had been successful in the US. I was looking into it and we were seeing if we could go to Germany and get it done there.
We talked to my oncologist before I started chemo and my husband brought it up. He said he’ll look into it, but because of how far off in the distance it is treatment-wise, I wouldn’t be alive by the time it would be available. We would either have to go to Germany or see how we could afford it because it costs over $190,000 to get this treatment.
When the chemo failed, I met with him and he said he had been working behind the scenes with a different oncologist who was looking for someone like me with BRAF mutation and MSI. Most bowel cancer patients are MSS. I don’t know how it works and why immunotherapy works for people who are MSI, but that’s generally what they figured out.
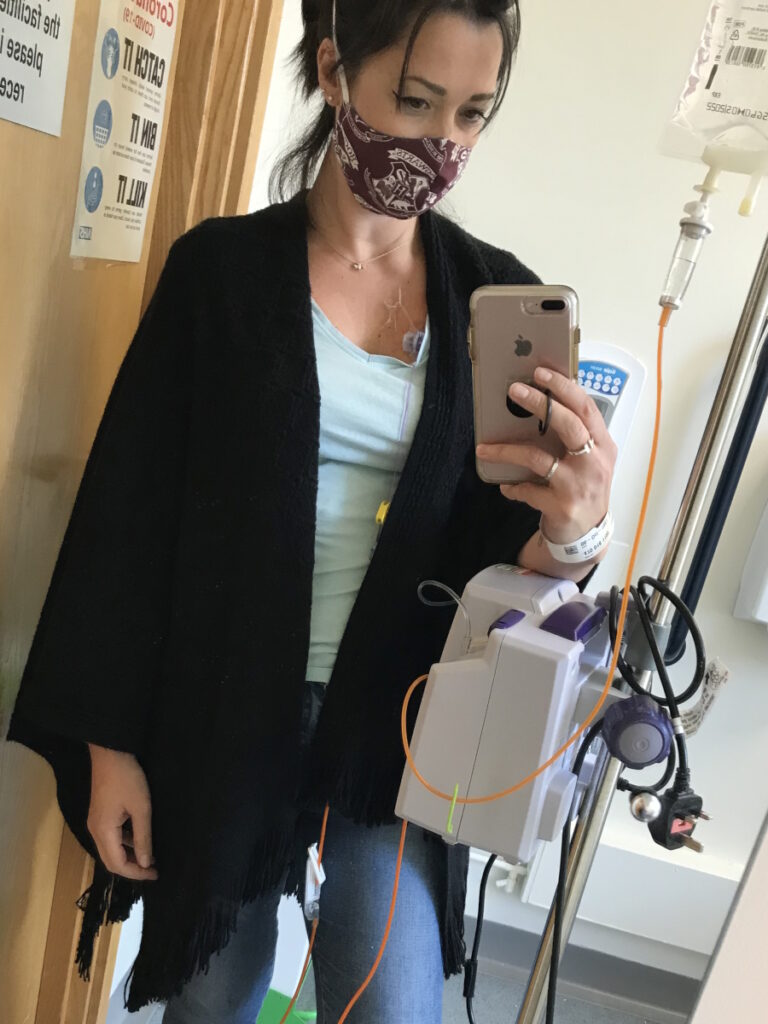
The drugs were called nivolumab and ipilimumab. The plan was to have both for four cycles and then after four cycles move down to nivolumab alone.
They tested the immunotherapy in melanoma patients and there was something that we have similarly that it might work. They were working with Bristol Myers Squibb, so I could get the immunotherapy on compassionate use if all my other treatment options failed. My oncologist knew this, but he didn’t tell me until it did fail. At the time, that was the only treatment available for BRAF mutation. He said that now it’s failed, he can refer me to get the immunotherapy.
I had to transfer care to another oncologist, which was a further away hospital. The drugs were called nivolumab and ipilimumab. The plan was to have both for four cycles and then after four cycles move down to nivolumab alone. I had the first cycle every three weeks and then nivolumab every two weeks.
Because of the newness of the treatment, they didn’t know how it was going to affect me. I was having the dual drug, so they said I had double the chance of getting any autoimmune disease, which could happen at any point. They had to do blood work every time and check everything. If I noticed anything different about myself, I had to report it to them. They would then report back their findings to the drug company.


Side Effects of Immunotherapy
The immunotherapy compared to the chemo was night and day. I was only there for a couple of hours and that was it. The infusion was around an hour and a half to two hours for the first one and then it eventually dwindled to an hour. I could drive out of there when I was done. With chemo, I couldn’t drive out of the hospital. I was barely moving. With the immunotherapy, I felt a little bit sick and a bit tired, but that was it.
After I had the PET scan, he called me up the next day and said, ‘Nothing’s showing on your PET scan. No cancerous cells anywhere.’
Being Cancer-Free
I’d been on immunotherapy for two years. They didn’t know where to go with it because there weren’t many people in front of me, but they knew it was getting to the two-year mark.
I asked my oncologist if I could get a PET scan because they don’t do PET scans so much over here. He wouldn’t do it at first until he agreed eventually. After I had the PET scan, he called me up the next day and said, “Nothing’s showing on your PET scan. No cancerous cells anywhere. It looks like those are dead tumors and we think that your lymph nodes are probably filled with white blood cells and that’s where they’re showing on the CT scans.”
There wasn’t a defining moment of being cancer-free. The only moment I can say that did happen was after I had my liver surgery. My surgeon said they had the biopsy results back because he wanted to wait to make sure. Sometimes when they cut them out, there can still be cancerous cells in the middle. He said they didn’t find anything. He said, “I can tell you now that that means you’re cancer-free.”
It’s a great feeling. I was happy. When I got out of the hospital and sat in my car, I called my husband and cried. That was probably the first time I cried out of relief because it was unbelievable.


Words of Advice
Appreciate and enjoy life. We’re all so busy doing things and thinking that we’re living when we’re not. You don’t want something like a terminal cancer diagnosis to make you realize that, but sadly, it does take that for a lot of people. It’s not until you get to this point that you realize how much we’re not living and how much we should be enjoying everything and everyone. Be kinder to each other and enjoy what you have.
We’re all so busy doing things and thinking that we’re living when we’re not. You don’t want something like a terminal cancer diagnosis to make you realize that.

Inspired by Sophie's story?
Share your story, too!
More Colorectal Cancer Stories
Allison R., Colorectal Cancer, Stage 2C
Age at Diagnosis: 32
1st Symptoms: Extreme fatigue, unexplained weight loss, blood in stool, "blockage" feeling after eating
Treatment: Concurrent adjuvant (oral) chemotherapy + radiation, colectomy, oral chemotherapy
Michelle C., Colorectal Cancer, Stage 4
Symptoms: Felt like either a UTI or yeast infection
Treatment: Chemotherapy (carboplatin and paclitaxel), surgery (hysterectomy), and radiation
Jason R., Colorectal Cancer, Stage 4
Symptoms: Blood in stool, diarrhea, tenesmus, feeling run down
Treatment: Chemotherapy, radiation, HAI pump
Raquel A., Colorectal Cancer, Stage 4
Symptoms: Frequent bowel movements, pin-thin stools, mild red blood in stool
Treatment: Chemotherapy (oxaliplatin, 5-fluorouracil, and irinotecan)
Symptoms: Frequent blood in stool, lower back pain, rectal pain
Treatment: Chemotherapy (5-FU), radiation, surgery