Eve’s Gleason 9 Prostate Cancer Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

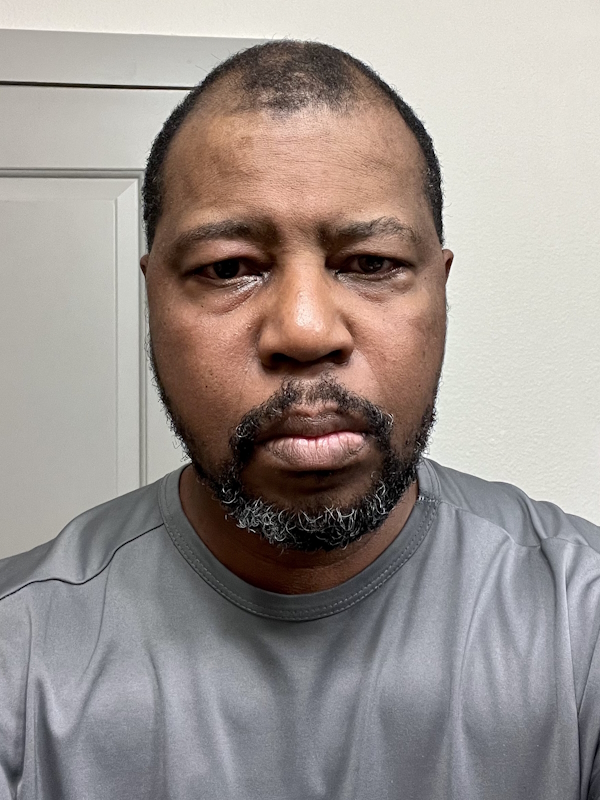
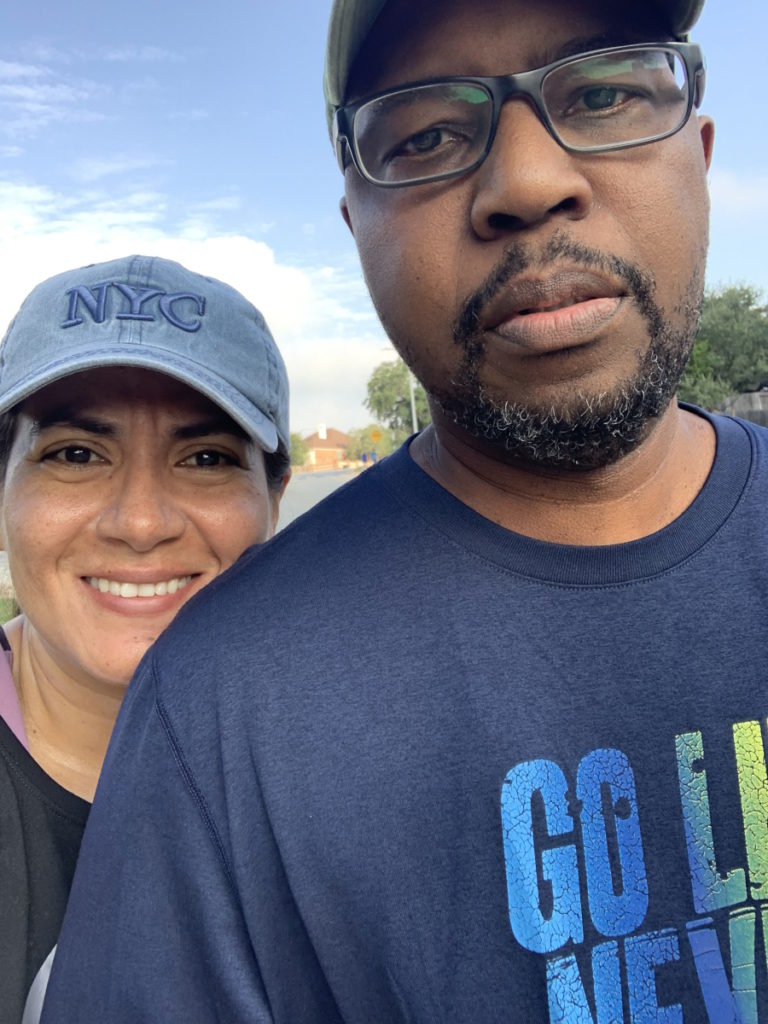
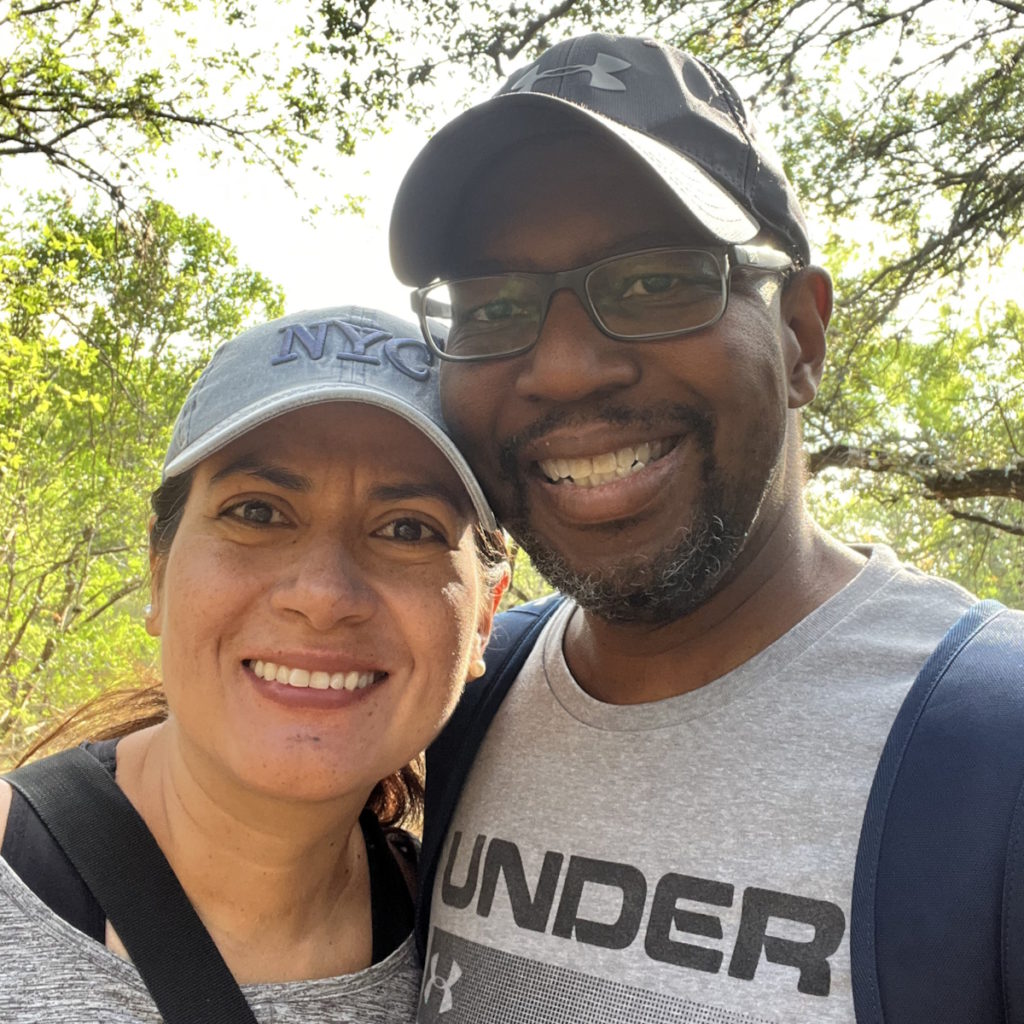
Eve shares her story of facing prostate cancer while embracing her gender identity. Diagnosed at age 57, she recounted how her health scare intertwined with her self-realization and how confronting cancer pushed her to live authentically.
Her cancer diagnosis was unexpected, identified during a routine physical when a PSA test began to rise from 4 to 12 by the following year. A biopsy revealed an aggressive Gleason score of 5+4.
She underwent a robot-assisted laparoscopic prostatectomy (RALP) in early 2018. The surgery affected her physically, removing erectile function and leaving her feeling disconnected from her former male identity, pushing her deeper into her non-binary reality.
Despite surgery, the cancer persisted. Radiation therapy followed, involving 18 rounds over several months. Her PSA initially decreased but started climbing again. Realizing that testosterone fueled the cancer, she decided to remove her testicles, undergoing a bilateral orchiectomy. Although it slightly reduced her PSA, it wasn’t a definitive solution. A significant turnaround came with an oncologist who devised a plan that stabilized her PSA to undetectable levels for four years.
Embracing life, she acknowledged cancer’s role in catalyzing her authenticity and resilience. Facing a traditionally masculine disease as a transgender woman highlighted the need for inclusive medical practices. She advocated for gender-sensitive language in healthcare and called for the inclusion of trans women in prostate cancer research.
- Name: Eve G.
- Age at Diagnosis:
- 57
- Diagnosis:
- Prostate Cancer
- Gleason Score:
- 9 (5+4)
- Symptom:
- None; elevated PSA levels detected during annual physicals
- Treatments:
- Surgeries: Robot-assisted laparoscopic prostatectomy (RALP) & bilateral orchiectomy
- Radiation
- Hormone therapy

Thank you to Johnson & Johnson for supporting our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
My prostate cancer and my gender transition were intimately related.
Introduction
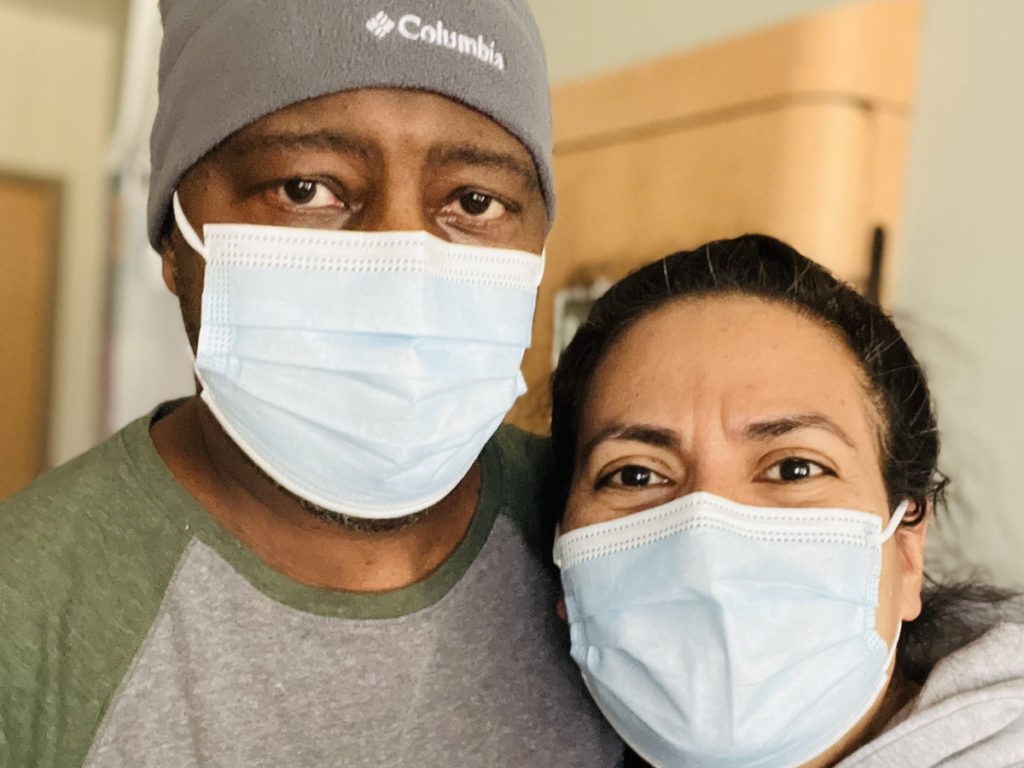
I’m a transgender woman, I’m married, and I’m fighting prostate cancer. I was diagnosed in 2017 at 57 years old. I faced my mortality, so the best I could do was to live my life happily. I bought a 42-foot sailboat and moved to Texas.
I’ve been telling a lie about my authentic self for almost 60 years. I recognized my authentic self, which was freeing. I don’t have any secrets anymore. I don’t have anything to hide from anymore. I faced my demons.
My prostate cancer and my gender transition were intimately related. I might not have transitioned if I didn’t think I had to. I might have gone on enjoying my male privileges. I enjoy some female privileges now but not as many. I’m a member of a discriminated-against minority.


Getting the Cancer Diagnosis
In 2016, I went for my annual physical with my primary care provider. They did a PSA test. It was the second or third that I’d done, but it had gone up to a 4. They didn’t think it was of great concern.
The following year, I went for another test and it was a 12. It started going up to 18 and they said, “We think it’s cancer.” I had a biopsy and they said it was a Gleason 5+4 or a 9. The maximum you can have for a Gleason score is 10 (5+5), so there were a lot of cancerous cells in my biopsy.
They took the nerves on one side of my prostate gland, the nerves that control a male’s erection, and I lost my erection. It left me feeling less than male.
Treatment Options
They told me that my choices were radiation or surgery. I told them to remove the gland. When they did, they took the nerves on one side of my prostate gland, the nerves that control a male’s erection, and I lost my erection. It left me feeling less than male. I was always non-binary and my wife always knew that since our first date.
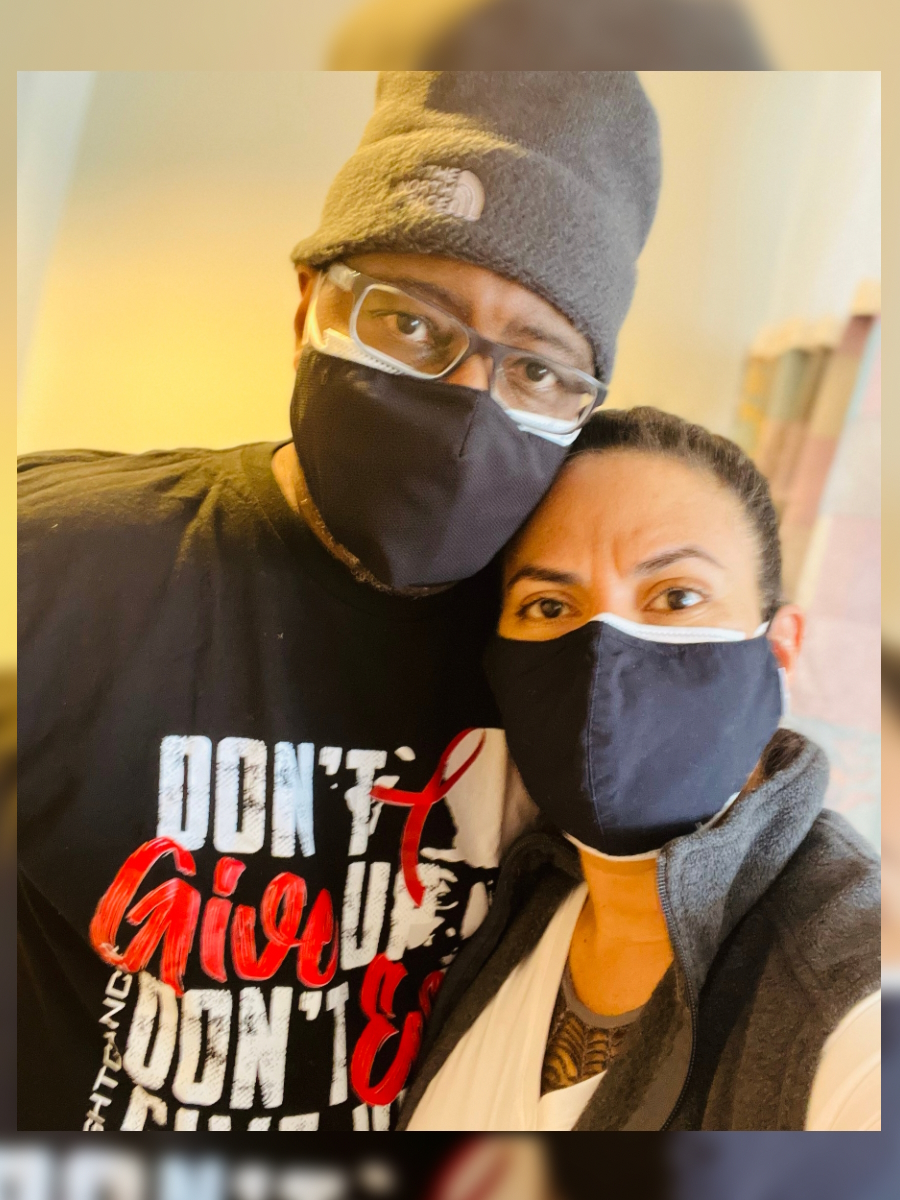
When they said, “You can’t have your testosterone anymore,” I started having hot flashes. I went through something similar to menopause. I coined it androgenopause.
It was a rough few years. I decided that I was going to transition. If I only have a few years left and I don’t feel male anymore, I better live it authentically.
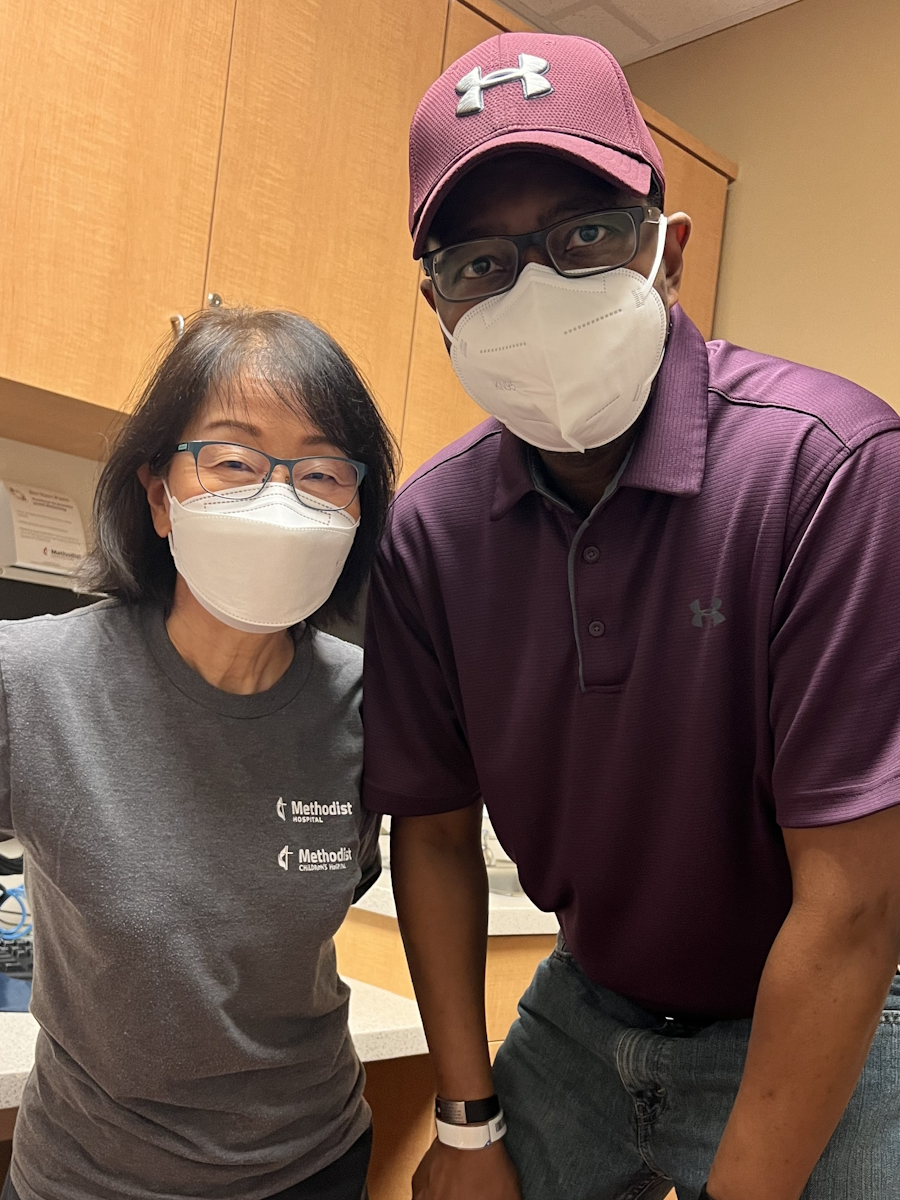
I went to the Veterans Affairs office and told them about my plan. They had a program through the Michael E. DeBakey Department of Veterans Affairs Medical Center and what the VA does for their transgender veterans.


Cancer Remains
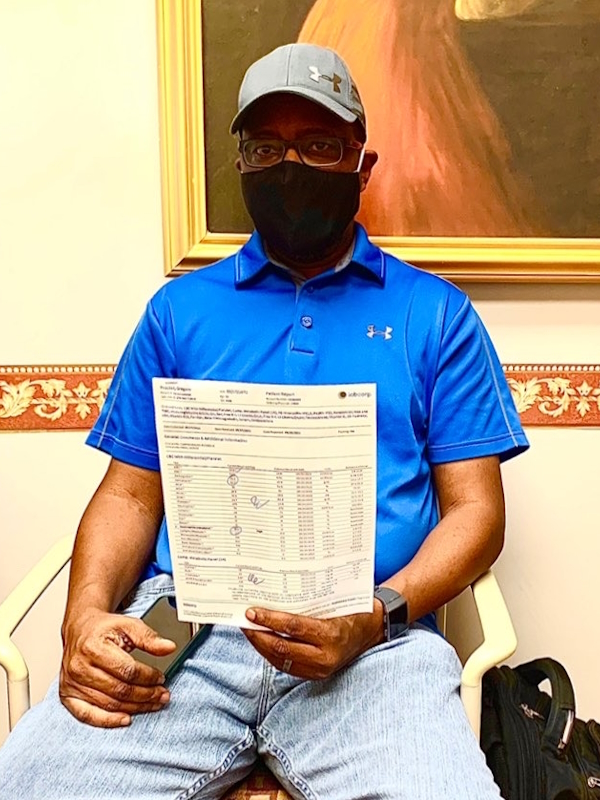
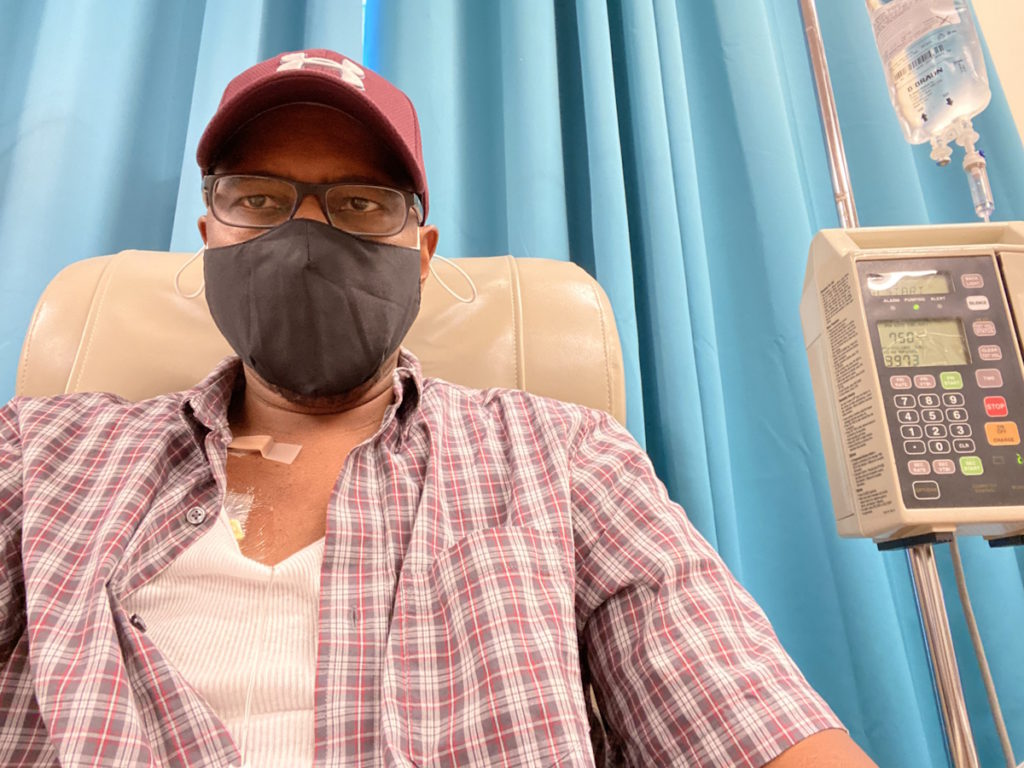
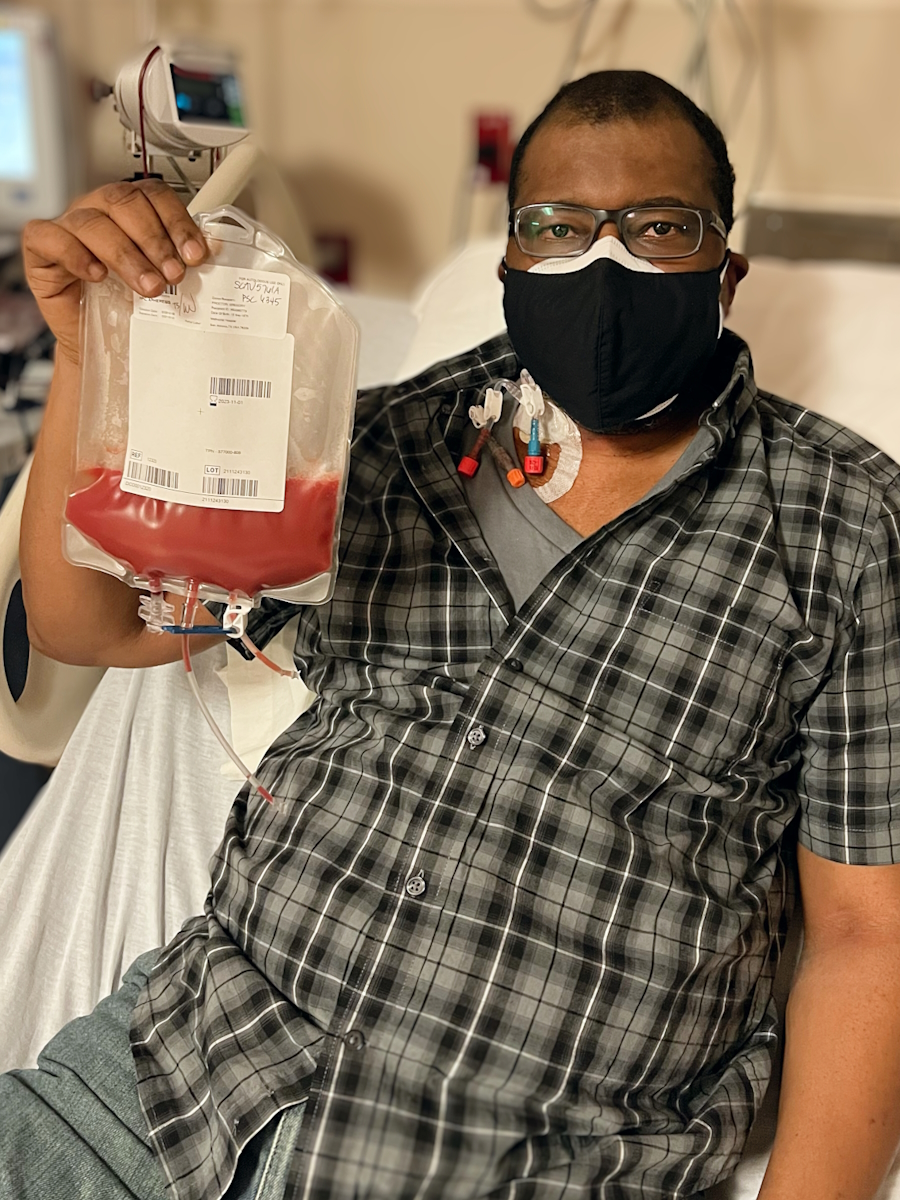
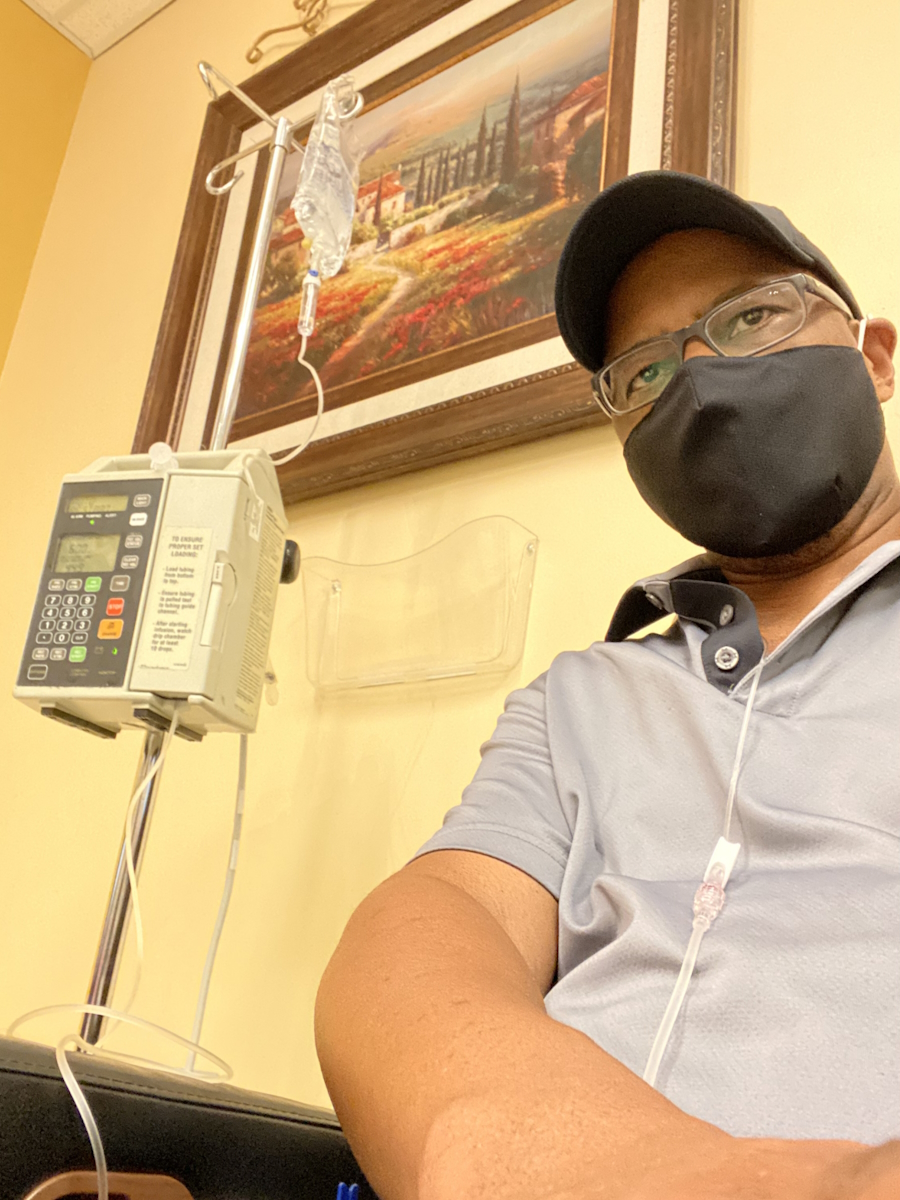
My cancer was aggressive. I underwent surgery in January 2018 called a robot-assisted laparoscopic prostatectomy (RALP). The pathology report indicated that the margins were positive and there were some cancerous cells in my bladder neck. My PSA didn’t go all the way down. They expected it to go to 0 after they removed the gland.
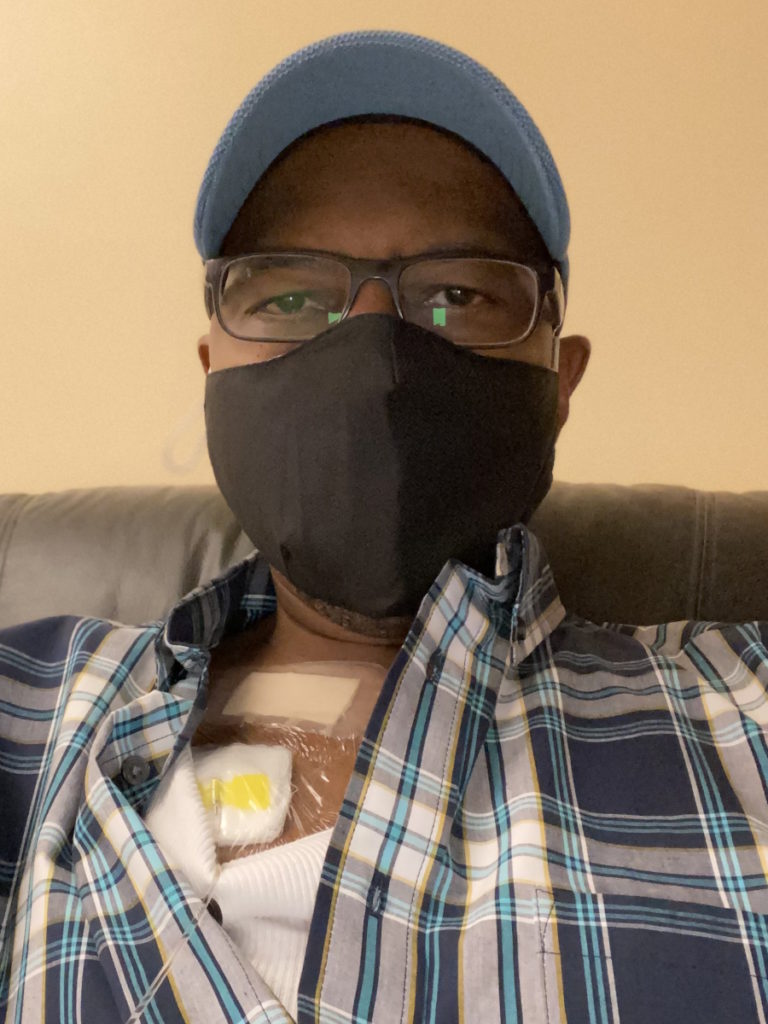
They recommended adjuvant radiation, so I saw the radiologist. They gave me a little tattoo right where they would hit their beam. I did 18 rounds of radiation over a few months. The surgery and radiation took their toll on me.
I was already non-binary and I had begun my transition hormonally, so if I don’t need my testicles, they’re not my friends anymore.
Removing Both Testicles
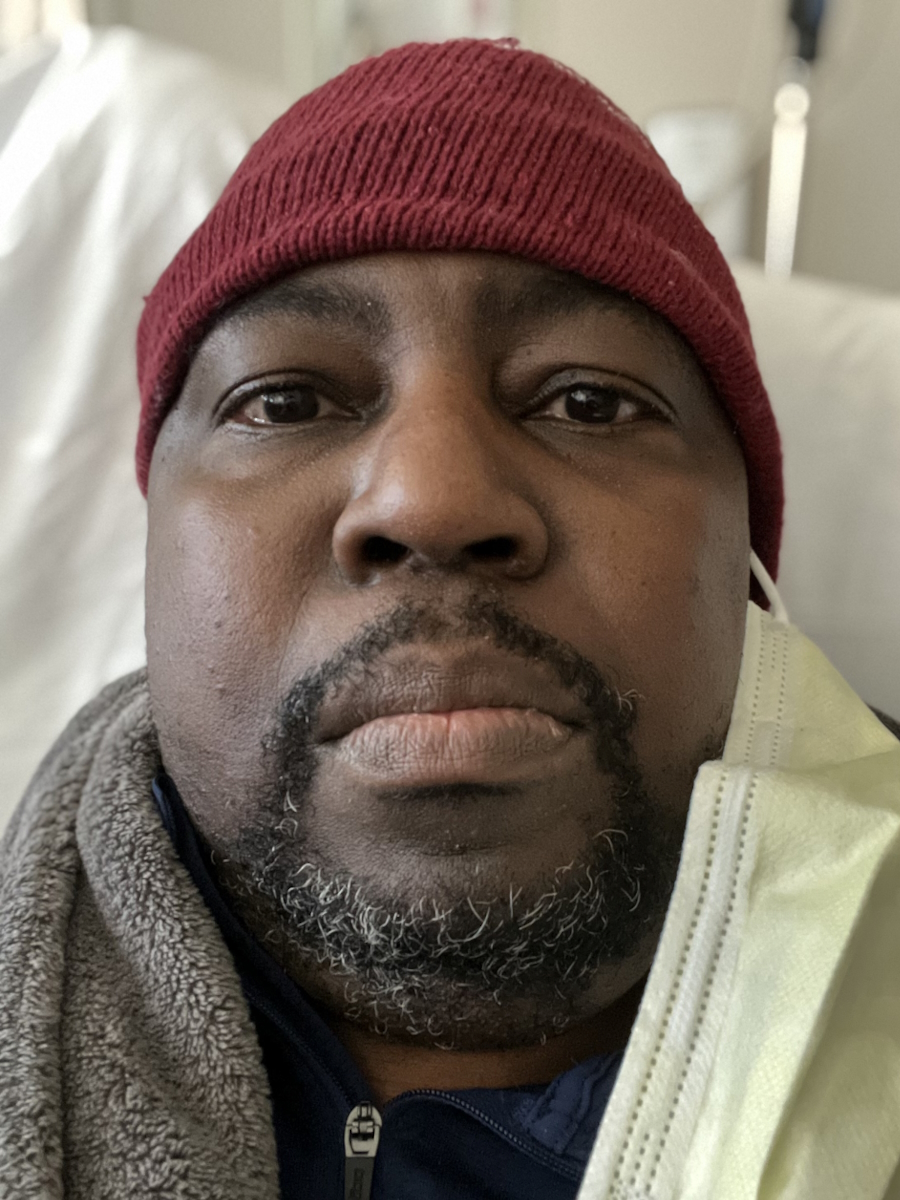
The cancer still didn’t go away. My PSA went down to 0.15, but it started climbing back up. Before we knew it, it was 4.5. I said, “Testosterone is not my friend.” I was already non-binary and I had begun my transition hormonally, so if I don’t need my testicles, they’re not my friends anymore. I did a bilateral orchiectomy. I had a difficult time with that surgery. My body did its job and I started feeling better, but it still didn’t bring down my PSA. It took it down a little bit more, but it was still rising.


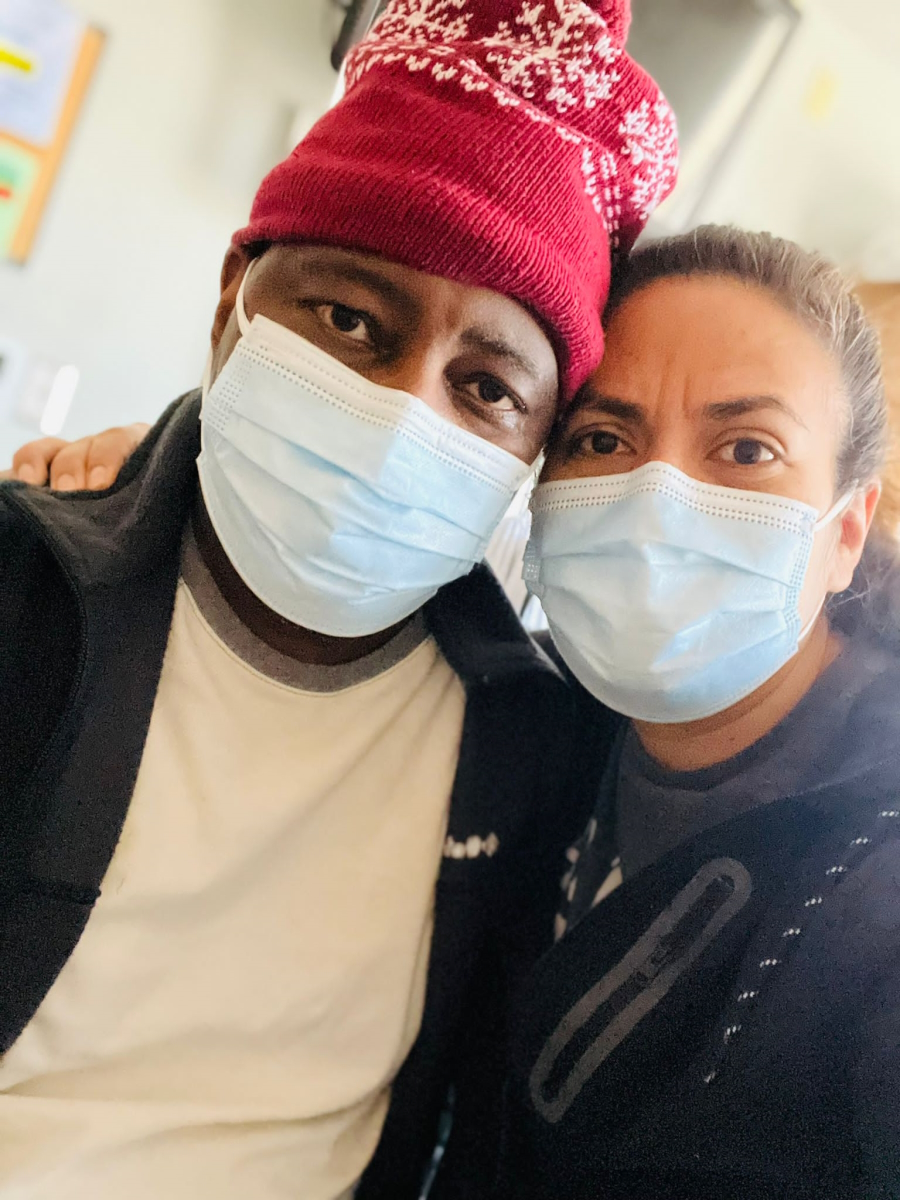
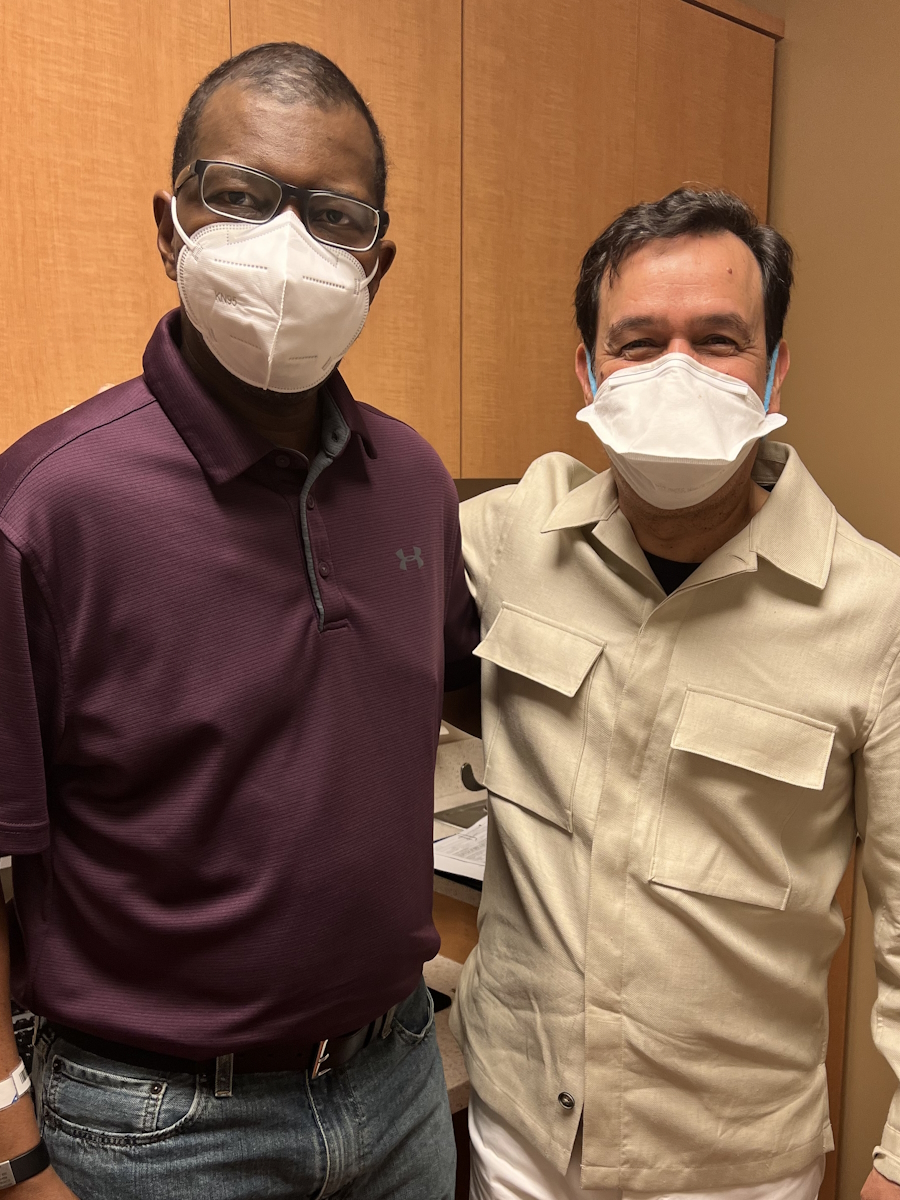
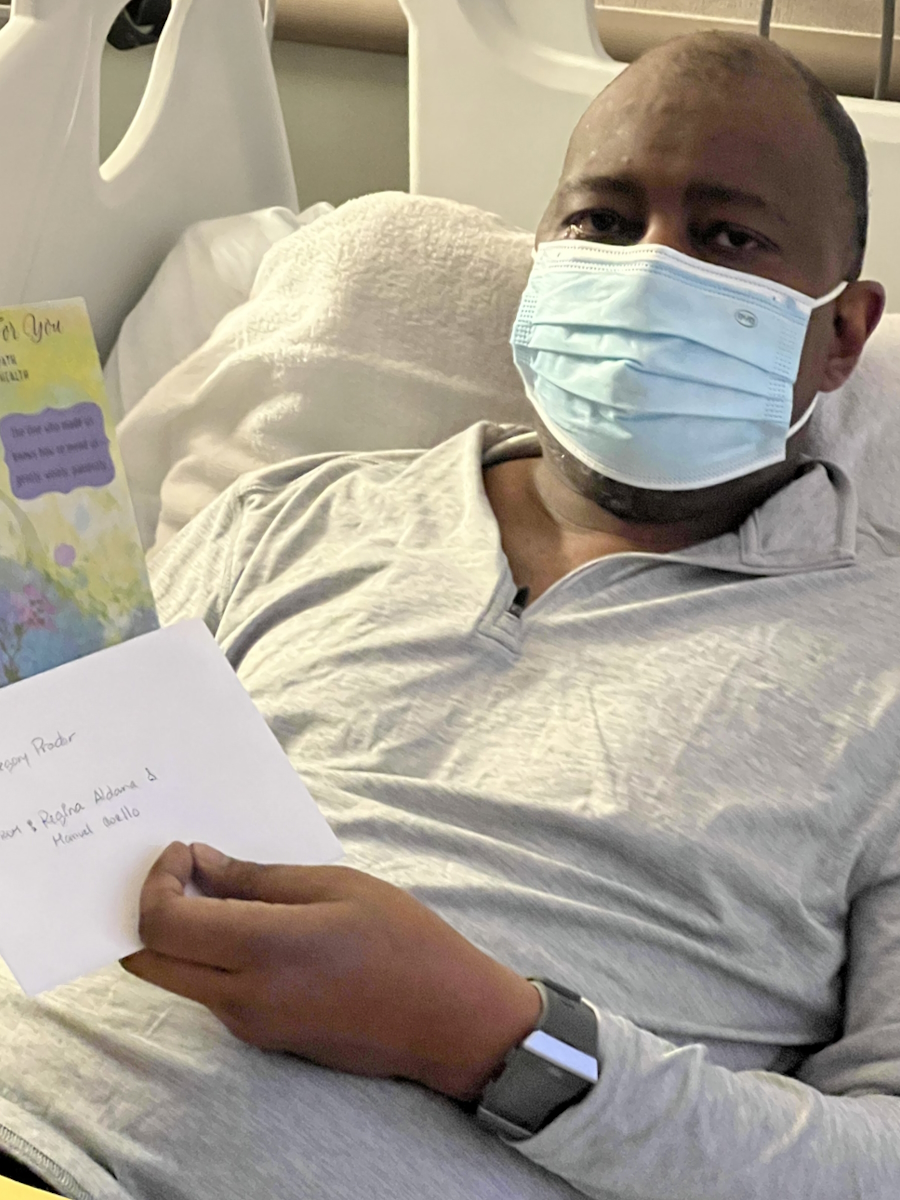
Urology referred me to oncology. The first oncologist I saw talked to me after I had sent her an email before my consult. I told her I’m a trans woman, I’ll be presenting feminine, and these are my pronouns. I hadn’t changed my name yet because I had to wait a while before I could do that, so she still saw my former name in my chart.
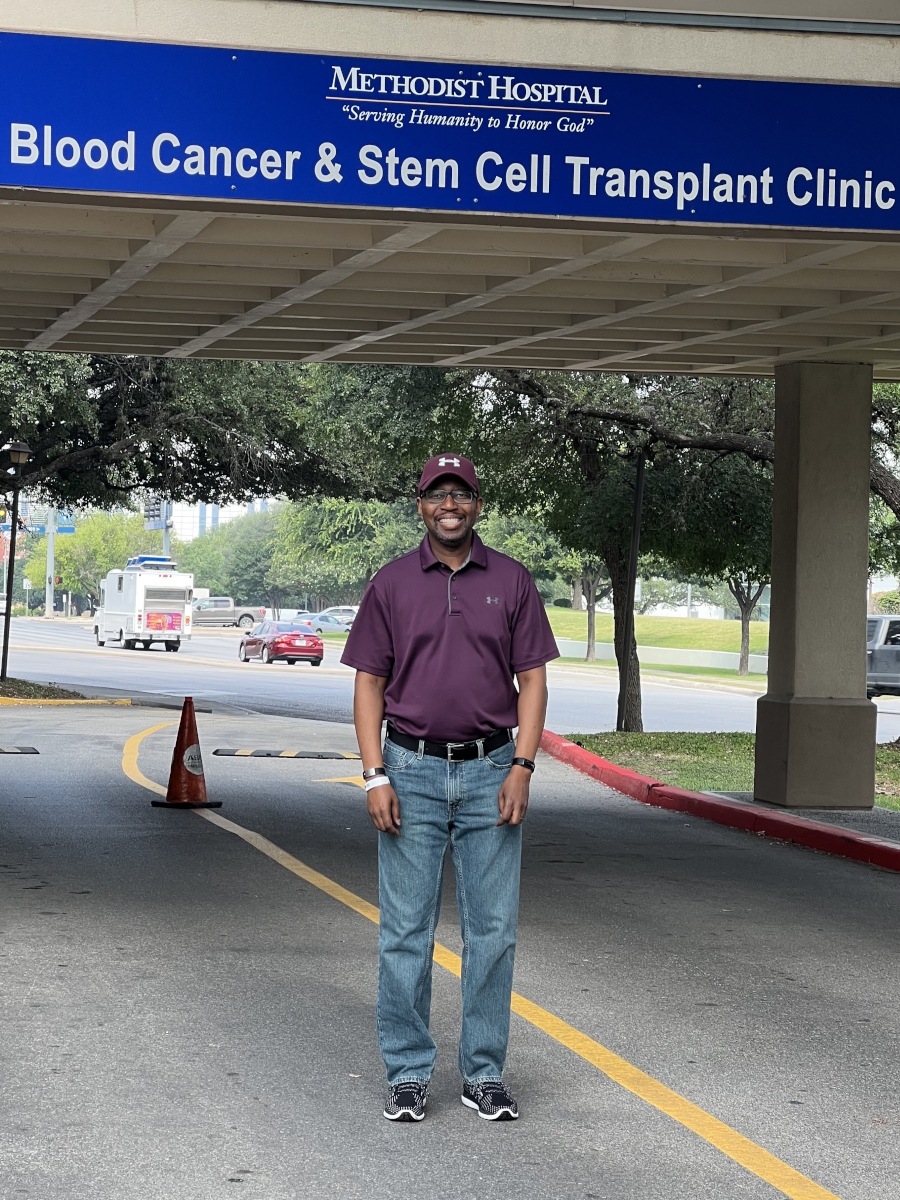
She wasn’t sure how to deal with a trans woman with a traditionally male disease, so she referred me to an oncologist at Rice University. He saved my life. My PSA went down to 0 and I’ve been on treatment for four years. I’m surprised that I survived this long, as aggressive as my cancer was. I thought I had maybe two years. I made some changes. I’m happy and I’m trying to keep a good attitude. My cancer hasn’t killed me yet and as far as I know, my PSA is still close to zero or undetectable.
My prostate cancer influenced me to live more authentically… With my diagnosis, I got lemons and made lemonade.
Reaction to Being Diagnosed with a Masculine Cancer
I rationalized it as a bunch of cancerous cells in my body that don’t define who I am and that I didn’t have much control over. Things happen. I didn’t have control over having cancer.
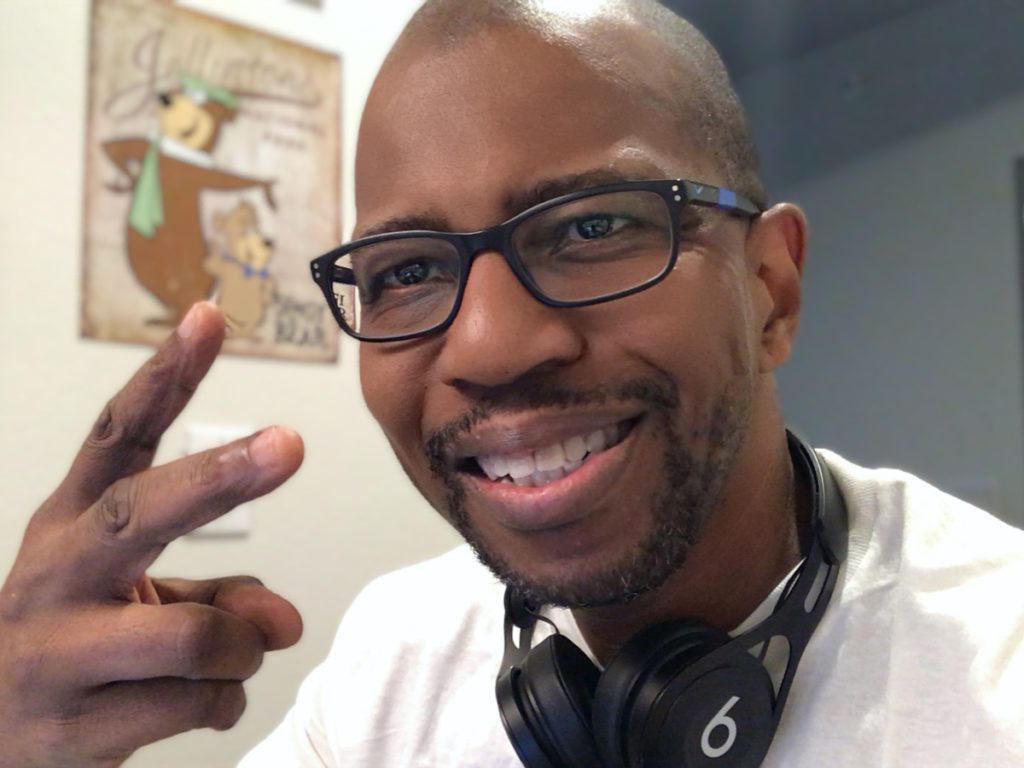
I knew that I was non-binary, but I had to come out to the world when I transitioned. I don’t blend in and I don’t care if I don’t. I’m going to be me. Everybody’s got a little ugly in them and everybody’s got a little pretty in them. Nobody’s perfect. I decided to be my authentic self.
My prostate cancer influenced me to live more authentically, to live more honestly, to be braver, to have greater confidence, to be a richer person, to be a more beautiful person I hope, and that’s been a gift. With my diagnosis, I got lemons and made lemonade.

Trans women exist. They also have prostate glands, even after gender reassignment surgery.

The Importance of Including Transgender Women in Prostate Cancer Research
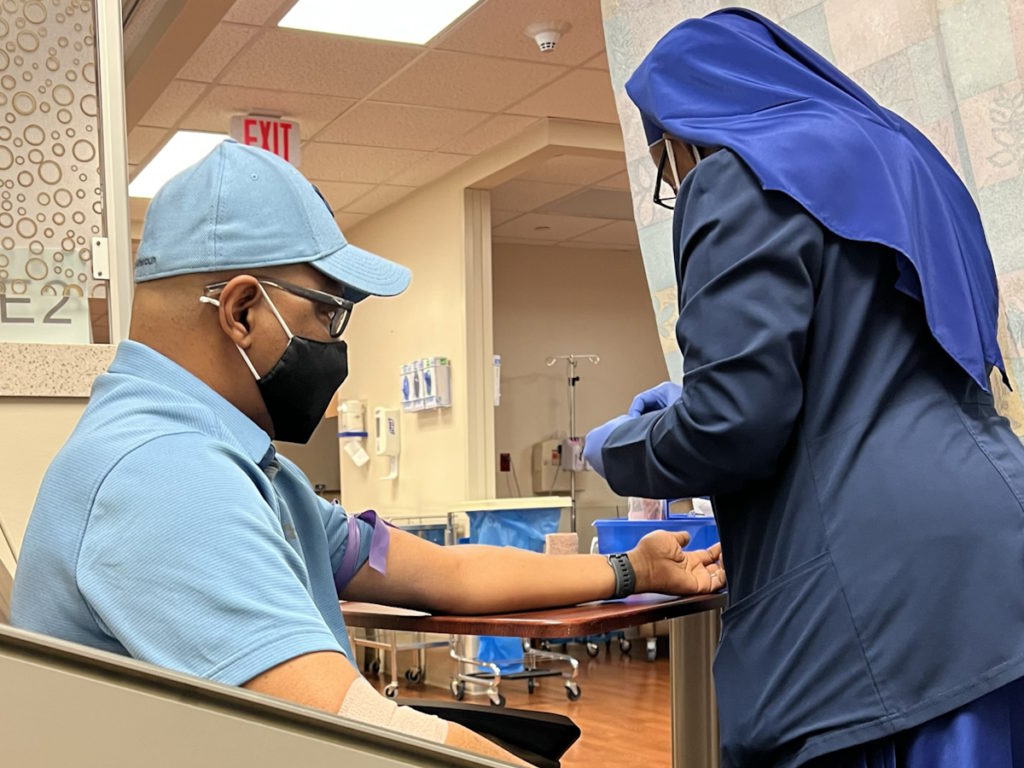
What I would like to help happen is for them to find new treatments that address prostate cancer without androgen deprivation therapy. I’d also like for the whole profession to quit talking about men with prostate cancer. I don’t consider myself male. Why don’t we talk about people with prostate cancer, patients with prostate cancer, or individuals with prostate cancer? Why all the mispronouns?
I’d like to change society so that they realize that pronouns are important. I correct people when I get misgendered. I used to get irritated; now, only if it’s done cruelly. If it’s accidental, I correct them and float right down the road.
With the community at large, the reason I do interviews is so that we can talk about patients with prostate cancer and recognize that trans women exist. They also have prostate glands, even after gender reassignment surgery. They don’t remove the prostate. I’d like to educate more people, more trans women specifically, to get their PSA checked and to monitor it.
I’d like to encourage the medical community to be aware that trans women have prostates too. Ask people what their preferred pronouns are. Put it on the forms that patients fill out. Practice using them.

I’d like to educate more people, more trans women specifically, to get their PSA checked and to monitor it.

Words of Advice
Secrets are toxic. Closets are places where you keep your clothes and not where you live. They’re dark and cramped. Authenticity is knowing who you are, being who you are, and being comfortable with who you are. It’s a gift that you give yourself.
Celebrate yourself and love yourself. I still have some masculine traits. I still have my masculine memories. I learned to love myself as this magnificent blend of masculinity and femininity. Whether it’s magnificent or not, it is to me. I like that I’ve been able to do that with myself. If you don’t love yourself, nobody’s going to love you. Go have fun, explore it all, and enjoy what you like.
Special thanks again to Johnson & Johnson for supporting our independent patient education content. The Patient Story retains full editorial control.

Inspired by Eve's story?
Share your story, too!
More Prostate Cancer Stories
Jamel Martin, Son of Prostate Cancer Patient
“Take your time. Be patient with the loved one that you are caregiving for and help them embrace life.”
Joseph M., Prostate Cancer
When Joseph was diagnosed with prostate cancer, the news came as a shock and forced him to face questions about his health, future, and faith. He shares how he navigated his diagnosis, chose robotic surgery, and learned to open up to his loved ones about his health.
Rob M., Prostate Cancer, Stage 4
Symptoms: Burning sensation while urinating, erectile dysfunction
Treatments: Surgeries (radical prostatectomy, artificial urinary sphincter to address incontinence, penile prosthesis), radiation therapy (EBRT), hormone therapy (androgen deprivation therapy or ADT)
John B., Prostate Cancer, Gleason 9, Stage 4A
Symptoms: Nocturia (frequent urination at night), weak stream of urine
Treatments: Surgery (prostatectomy), hormone therapy (androgen deprivation therapy), radiation
Eve G., Prostate Cancer, Gleason 9
Symptom: None; elevated PSA levels detected during annual physicals
Treatments: Surgeries (robot-assisted laparoscopic prostatectomy & bilateral orchiectomy), radiation, hormone therapy
Lonnie V., Prostate Cancer, Stage 4
Symptoms: Urination issues, general body pain, severe lower body pain
Treatments: Hormone therapy, targeted therapy (through clinical trial), radiation
Paul G., Prostate Cancer, Gleason 7
Symptom: None; elevated PSA levels
Treatments: Prostatectomy (surgery), radiation, hormone therapy
Tim J., Prostate Cancer, Stage 1
Symptom: None; elevated PSA levels
Treatments: Prostatectomy (surgery)
Mark K., Prostate Cancer, Stage 4
Symptom: Inability to walk
Treatments: Chemotherapy, monthly injection for lungs
Mical R., Prostate Cancer, Stage 2
Symptom: None; elevated PSA level detected at routine physical
Treatment: Radical prostatectomy (surgery)
Jeffrey P., Prostate Cancer, Gleason 7
Symptom: None; routine PSA test, then IsoPSA test
Treatment: Laparoscopic prostatectomy
Theo W., Prostate Cancer, Gleason 7
Symptom: None; elevated PSA level of 72
Treatments: Surgery, radiation
Dennis G., Prostate Cancer, Gleason 9 (Contained)
Symptoms: Urinating more frequently middle of night, slower urine flow
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Lupron)
Bruce M., Prostate Cancer, Stage 4A, Gleason 8/9
Symptom: Urination changes
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)
Al Roker, Prostate Cancer, Gleason 7+, Aggressive
Symptom: None; elevated PSA level caught at routine physical
Treatment: Radical prostatectomy (surgery)
Steve R., Prostate Cancer, Stage 4, Gleason 6
Symptom: Rising PSA level
Treatments: IMRT (radiation therapy), brachytherapy, surgery, and lutetium-177
Clarence S., Prostate Cancer, Low Gleason Score
Symptom: None; fluctuating PSA levels
Treatment: Radical prostatectomy (surgery)