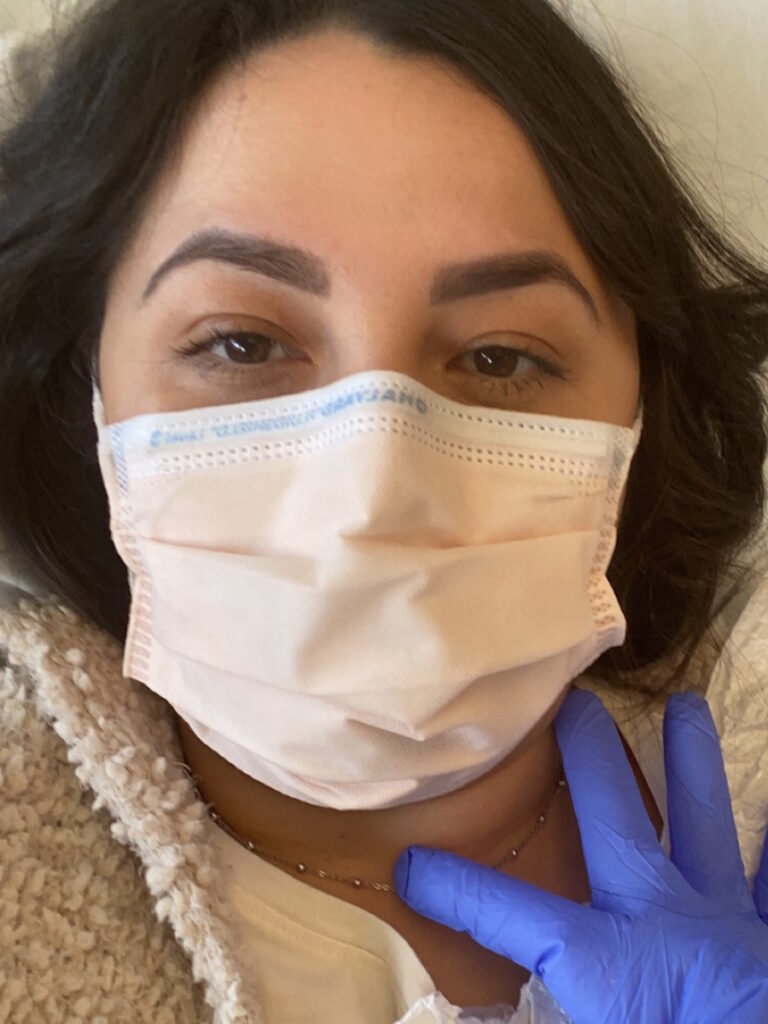
Brittany’s Stage 4 Liver and Bile Duct Cancer Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

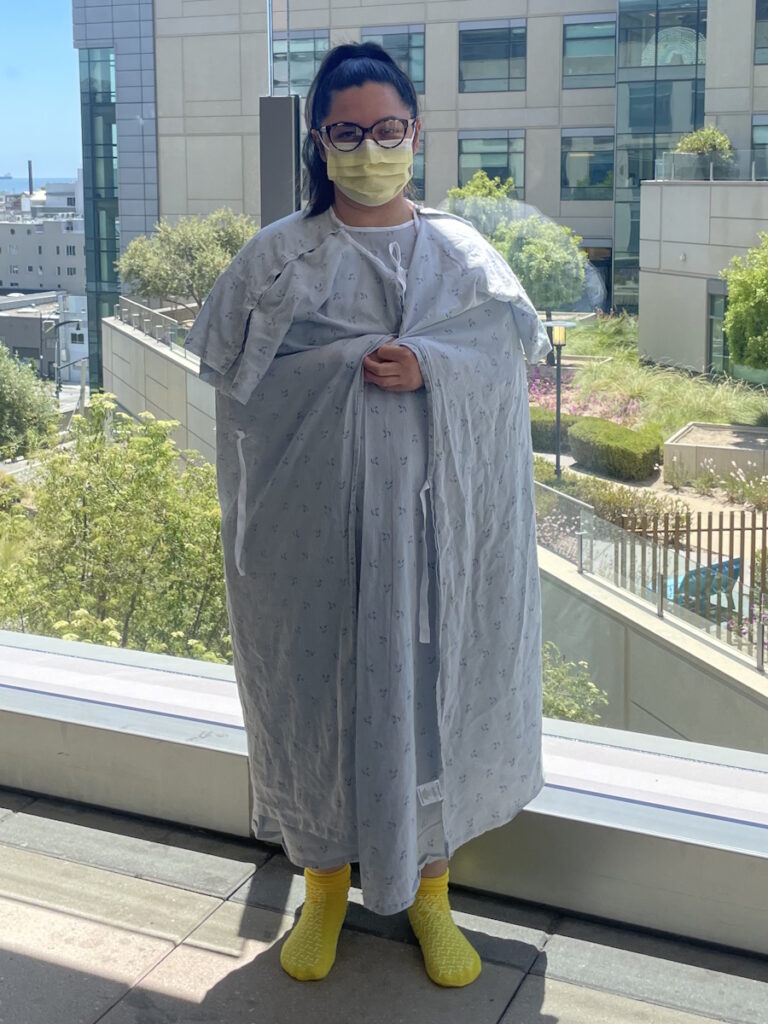
Brittany, a nurse who works in surgical oncology and a proud mother of 2, was diagnosed with stage 4 hepatocellular carcinoma (liver cancer) and cholangiocarcinoma (bile duct cancer). She is now officially “no evidence of disease” (NED) thanks to surgery and immunotherapy.
Brittany’s story starts about 3 years ago, when all of a sudden, she stopped menstruating. A pelvic ultrasound failed to turn up any potential cause. In September 2021, she began to lose appetite and her weight began to drop, and she ended up losing a total of 15 to 20 lbs. Her PCP ran a full array of lab tests, but they all came back normal.
In January 2022, Brittany started experiencing bad pain in the upper right quadrant of her abdomen. She rushed herself to a hospital where she had more lab work done and, this time, a CT scan of her chest, abdomen and pelvis as well. Once again her tests failed to turn up anything–but the CT scan found a 10cm mass on her liver.
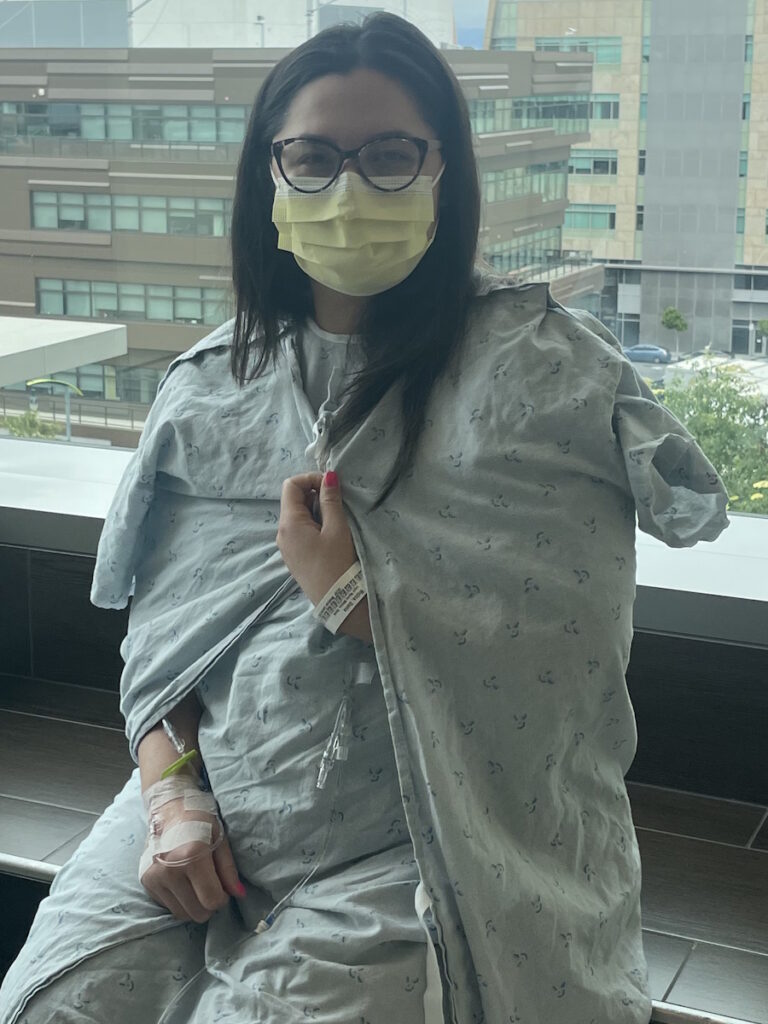
Brittany transferred to a larger hospital where she spoke with a specialist in liver surgery. A few days later, he and his team operated on her to remove the diseased portion of her liver (which amounted to 60% of the organ). However, they found out that her gallbladder had also been affected and portions needed to be removed too, and moreover discovered lesions on her lungs. Further testing finally revealed the true nature of her cancer, and the lesions on her lungs determined that it was stage 4.
Though Brittany’s doctors were optimistic about her chances, they were also realistic, given that liver cancer is not easy to treat and that cholangiocarcinoma is known to be extremely aggressive. But Brittany was determined to beat the odds and overcome her cancer.
Brittany began to undergo immunotherapy in April 2022. Her cancer responded favorably to the treatment; her liver has been cancer-free since the resection, and all lung lesions have disappeared.
Brittany’s last treatment was administered in December 2022. Since stopping treatment, she has gotten a CT and MRI with lab work every 3 months; these have recently been spaced out to every 6 months for surveillance.
Brittany would like to share that her experience has definitely changed her life. She refuses to take things for granted any longer, makes sure to enjoy every moment, and is intent upon giving back as much as she can. She also urges fellow patients to take full charge of their own healthcare, to educate themselves fully, and to be their own advocates. “Don’t believe the statistics!” she adds — they’re really just numbers.
- Name: Brittany B.
- Diagnosis:
- Hepatocellular carcinoma (liver cancer) and cholangiocarcinoma (bile duct cancer)
- Staging:
- Stage 4
- Initial Symptoms:
- Amenorrhea
- Unexplained weight loss
- Loss of appetite
- Pain in right upper quadrant of abdomen
- Treatment:
- Surgery: removal of portions of liver and gallbladder
- Immunotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.

Inspired by Brittany's story?
Share your story, too!
Related Cancer Stories
More Stories
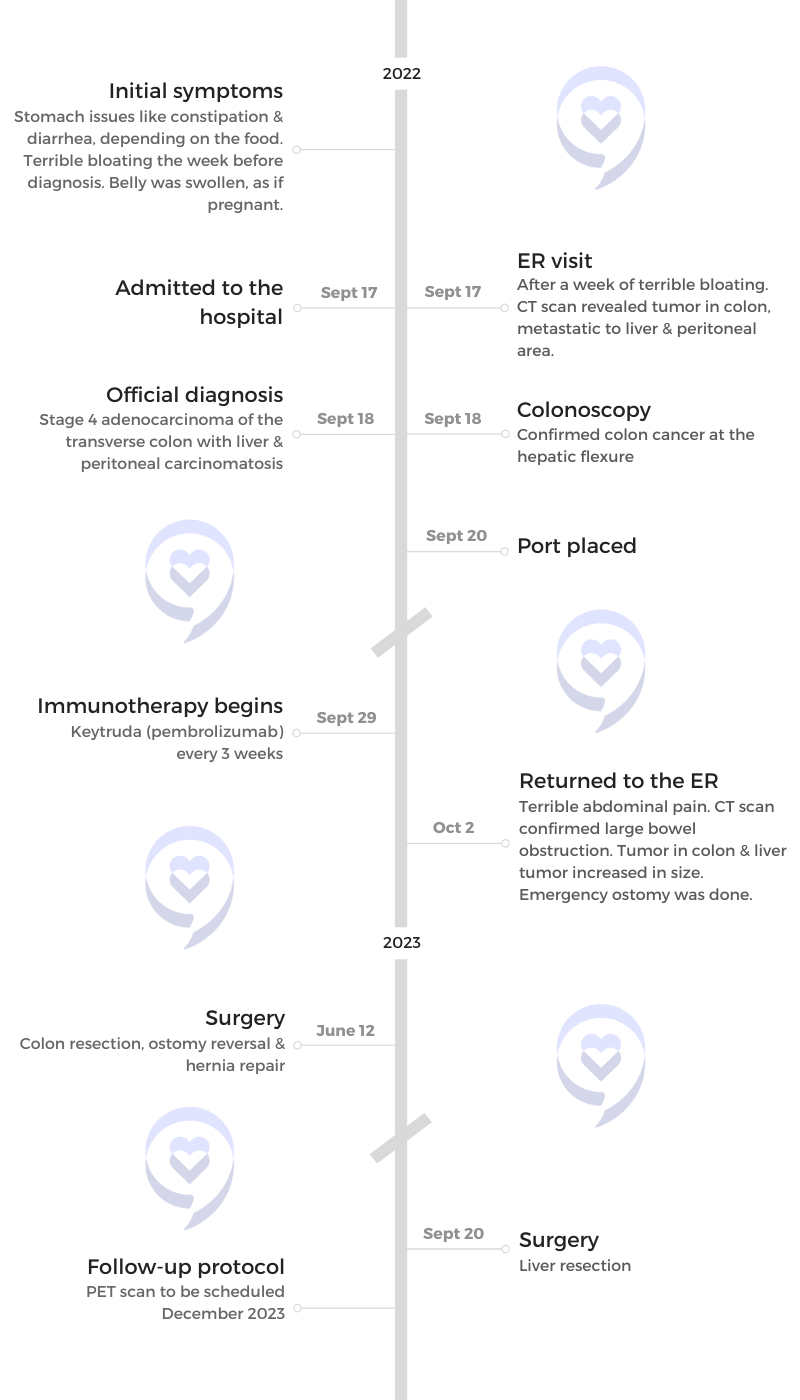
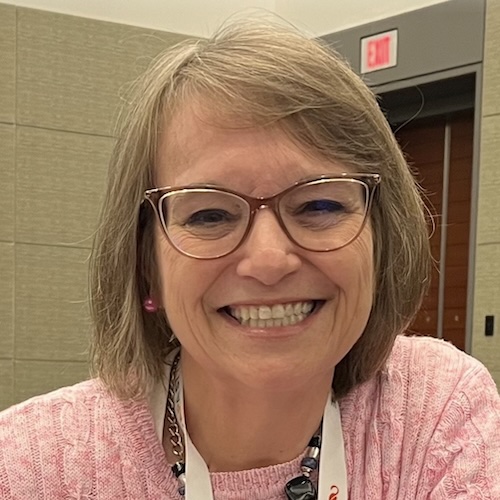
Dania M., Colon Cancer, Stage 4, with Liver and Peritoneal Carcinomatosis
Symptoms: Constipation, diarrhea, severe bloating, swollen belly as if pregnant
Treatments: Surgery, immunotherapy
Brittany B., Liver and Bile Duct Cancer, Stage 4
Symptoms: Amenorrhea, unexplained weight loss, loss of appetite, pain in right upper quadrant of abdomen
Treatments: Surgery, immunotherapy