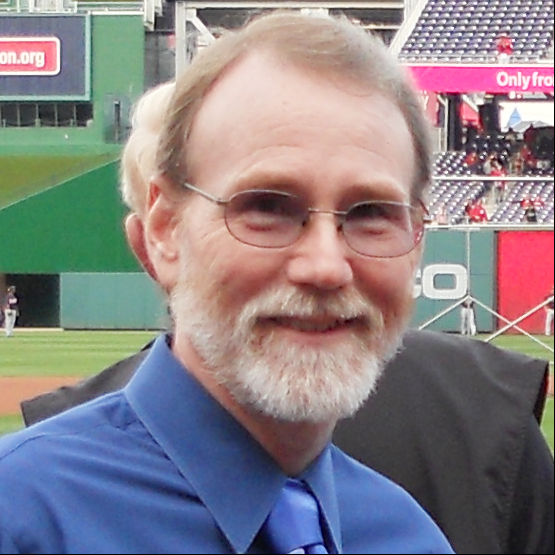
Diagnosed with Gleason 9, Stage 4 Prostate Cancer: John’s Blueprint for Living Well
John’s life took an unexpected turn in 2021 when he was diagnosed with Gleason score 9, stage 4 prostate cancer (stage 4A). His experience has been anything but easy, yet his story is packed with lessons on resilience, hope, and the power of proactive health management.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
John’s signs that something was amiss were nocturia (frequent nighttime urination) and a weak stream of urine. Despite visiting his doctor and undergoing a prostate-specific antigen (PSA) test, his results were misleading due to a medication called finasteride, commonly used for hair loss. Unfortunately, neither he nor his regular doctor realized that the PSA levels should have been doubled for accurate interpretation. This oversight delayed his diagnosis and, as they realized later, the cancer spread beyond his prostate in the interim.

After a biopsy of his prostate, John received the challenging diagnosis of Gleason score 9, stage 4A prostate cancer along with the revelation of positive margins (cancer left even after surgery), lymph node involvement, and other aggressive cancer indicators. But instead of dwelling on “Why me?”, he shifted his mindset to, “What can I do about it?” This pivot led him to embrace what he calls TIDES: Treatment, Inspiration, Diet, Exercise, and Sleep, as his personal blueprint to slow down the progression of prostate cancer.
John underwent surgery, hormone therapy (androgen deprivation therapy or ADT), and radiation. These treatments came with intense side effects — hot flashes, joint issues, urinary incontinence, and even the onset of Charcot-Marie-Tooth disease, a rare disease affecting the nerves linking the brain and spinal cord to the rest of the body. Yet, he managed to find new meaning in life despite these challenges. His secret? Focusing on what he could control.
John took a comprehensive approach to navigating his life after diagnosis. Optimizing his diet became a priority. He moved towards plant-based foods, inspired by studies showing that healthier lifestyles reduce prostate cancer mortality risk significantly. Exercise was another key element, helping him manage weight changes due to decreased metabolism from ADT. John also prioritized sleep and mental health, practicing daily gratitude, and finding joy in life’s simplest moments.
Now in remission, John is more determined than ever. His message to others facing stage 4 prostate cancer is simple, yet powerful: don’t let the fear of side effects stop you from seeking treatment. Life after a diagnosis isn’t over; it’s just different and can still be fulfilling.
Watch John’s video to find out about:
- How he found hope after his stage 4 prostate cancer diagnosis.
- The five lifestyle changes John swears by to manage his health.
- Why he says life is still great after a tough cancer experience.
- The overlooked PSA test factor that delayed John’s diagnosis.
- His secret weapon against cancer blues.
- Name:
- John B.
- Age at Diagnosis:
- 58
- Diagnosis:
- Prostate Cancer
- Staging:
- Stage 4A
- Gleason Score:
- Gleason 9
- Symptoms:
- Nocturia (frequent urination at night)
- Weak stream of urine
- Treatments:
- Surgery: prostatectomy
- Hormone therapy: androgen deprivation therapy (ADT)
- Radiation
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.

Inspired by John's story?
Share your story, too!
More Gleason Score 9 Prostate Cancer Stories
John B., Prostate Cancer, Gleason 9, Stage 4A
Symptoms: Nocturia (frequent urination at night), weak stream of urine
Treatments: Surgery (prostatectomy), hormone therapy (androgen deprivation therapy), radiation
Eve G., Prostate Cancer, Gleason 9
Symptom: None; elevated PSA levels detected during annual physicals
Treatments: Surgeries (robot-assisted laparoscopic prostatectomy & bilateral orchiectomy), radiation, hormone therapy
Dennis G., Prostate Cancer, Gleason 9 (Contained)
Symptoms: Urinating more frequently middle of night, slower urine flow
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Lupron)
Bruce M., Prostate Cancer, Stage 4A, Gleason 8/9
Symptom: Urination changes
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)