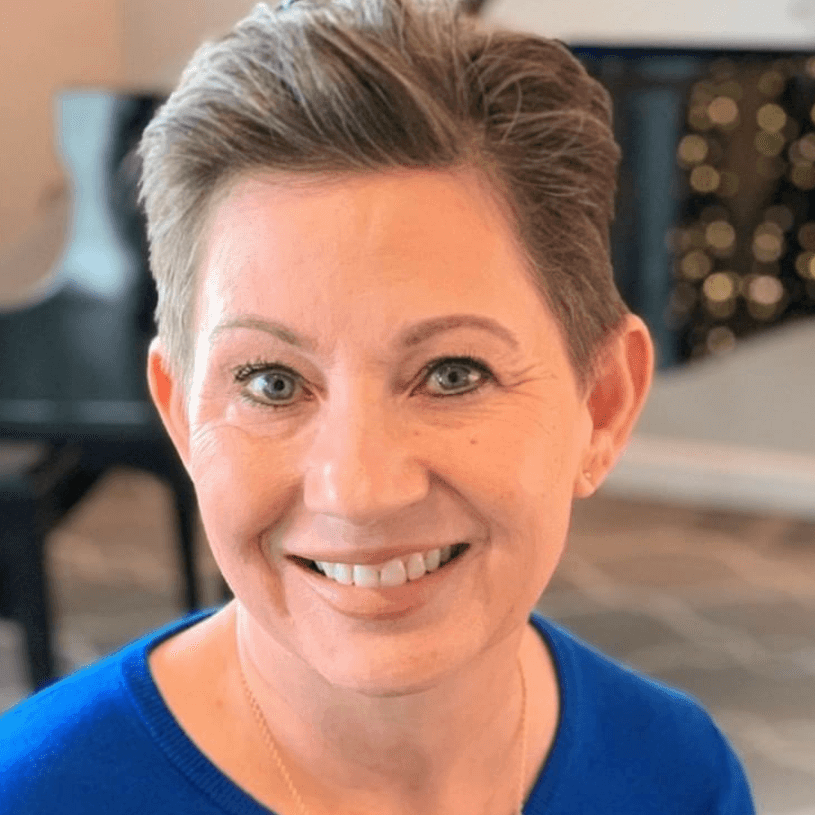
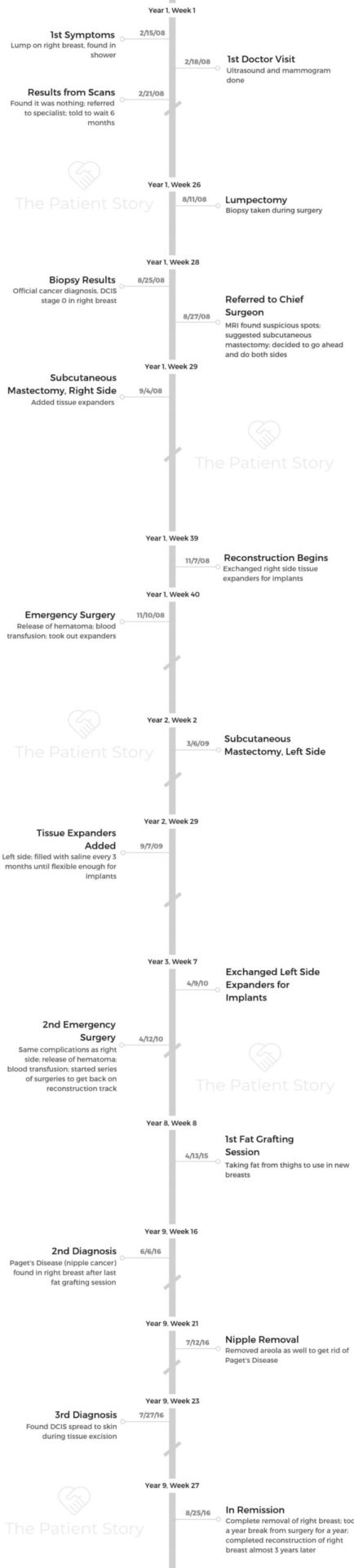
Natalie’s Stage 0 ER+ DCIS & Paget’s Disease Breast Cancer Story
Natalie shares her stage 0 breast cancer story, getting diagnosed after finding a lump on her right breast. She details undergoing multiple surgeries, including a lumpectomy, then double mastectomy, and reconstruction, as well as hormone therapy.
In her story, Natalie also highlights how she got through the emotional roller coaster of cancer, being a young mother undergoing treatment, and the importance of patient self-advocacy.

- Name: Natalie W.
- Diagnosis (2):
- Ductal carcinoma in situ, ER+
- Paget’s disease of the nipple
- Staging: 0 (earliest possible)
- 1st Symptoms: Lump found on right breast
- Treatment:
- Surgery:
- Lumpectomy, right breast
- Double subcutaneous mastectomy
- Reconstruction with implants
- Hormone Therapy:
- Tamoxifen, 5 years
- Surgery:
I wouldn’t be doing the things I’m doing now had I not had cancer. It’s sad that this had to happen, but sometimes these are the kind of things that have to happen before people realize that they need to change things up a little bit.
If you have a cancer or struggle that you feel like you can’t make it out of, you need to be able to say, ‘If tomorrow I’m taken away, at least I can say that the life I lived was happy, and I did things right.’
The life you’re living right now, make the most of it.
Natalie W.

- Diagnosis
- Treatment Decisions
- More Diagnoses
- Remission & Reconstruction
- Hormone Therapy
- Quality of Life Reflections
- The emotional impact of treatment
- What helped you deal with this level of stress?
- How important is it to have caregivers and support?
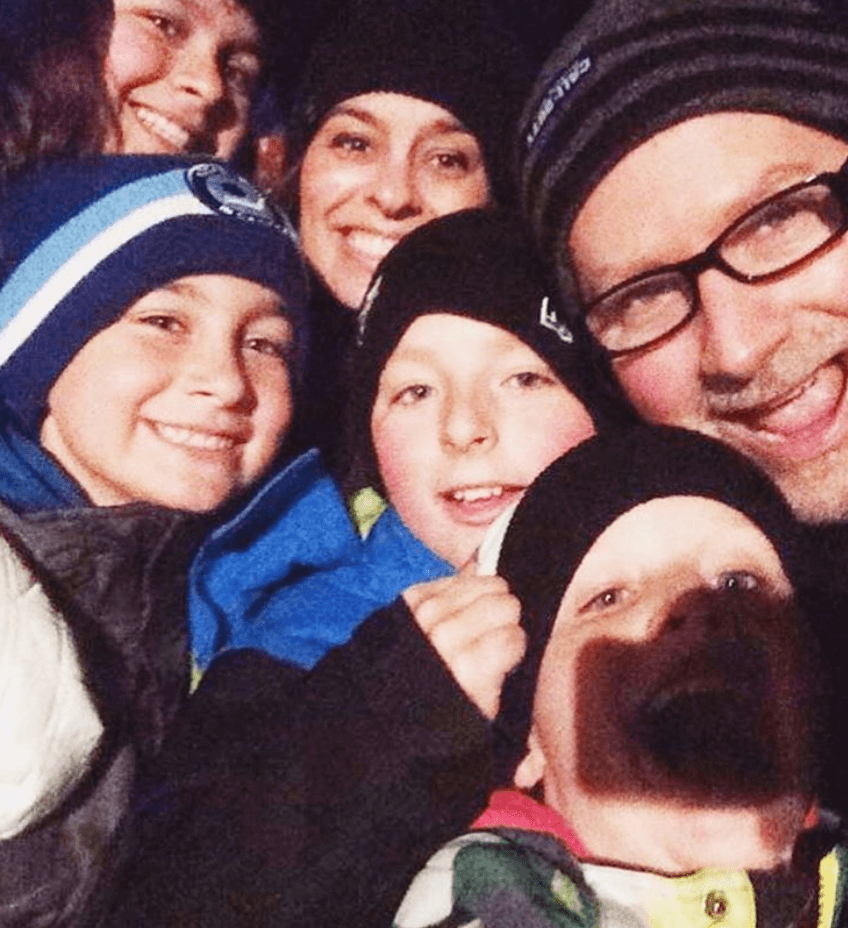
- How was it being a young mother and being diagnosed with cancer?
- Were there times during treatment you had to advocate for yourself?
- Do you have any advice on self-advocacy for others?
- How was the financial aspect of going through treatment?
- Your cancer inspired the work you do now
- What is your “new normal” after cancer?
- Do you have any final words for anybody who may be going through something similar?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Diagnosis
What were your first symptoms?
My first symptom was a lump, actually. It was not painful, but it was quite hard. I’m from a Jamaican background, and in Jamaica we have a fruit called guinep. On the outside, it’s kind of soft and squishy, but on the inside it’s hard. It was about like that, and I’d say 2 cm round on the side of my right breast.
I felt it when I was in the shower lathering up. I wasn’t one of those women that did the regular monthly check. It’s not something I learned growing up. It was just something that I came across while I was lathering up. That’s how I knew that something was there and wasn’t right.
My breast had never felt like that. My breasts had just gone back down to normal size after nursing my third child, and that was what allowed me to feel it.
Had I still been nursing and my breasts been engorged, I wouldn’t have felt it.
What do you remember of your first visit to the doctor?
The first visit was to see my family doctor. I’m not the type of person that gets too worked up about things if I don’t have a definitive answer, so I wasn’t feeling scared or worried.
I just wanted some answers and went in with an open mind. She’s a young woman herself, so she said, “Okay, let’s just get you in for a mammogram and ultrasound.”
Even through the mammogram and ultrasound, I was still quite level-headed. It wasn’t until the mammogram came back saying it was nothing that I had a concern because the feeling was still there, and I just knew. A woman just knows her body. I knew that this was not nothing.
That’s when I asked the doctor to send me to a specialist who deals with cancer patients and reconstructive surgeries and all that. That doctor said to wait 6 months. She wanted to wait and see if it changed.
How did your doctor give you the diagnosis?
Then 6 months later, I did have a lumpectomy. This is when I started to get worried. Between the lumpectomy and the 2 weeks I had to wait to get the results, that’s when I was concerned.
It was like they had something that could really give me a definitive answer, and I had all this time prior to that to stew in it, so I was nervous waiting to hear the answer.
My doctor and I are quite friendly. She’s a nice lady. We talk about fashion and all that. We always preface our conversations with that before we go any further. I don’t know if that was her way of lightening the mood this day or what, because she didn’t have good news for me.
She said, “I don’t know how I’m going to tell you this because I didn’t expect the answer myself, but you have breast cancer.” She said she felt the lump after surgery and didn’t think it was.
She said it didn’t look like it was cancer, but it was. She did tell me that if there was any kind of breast cancer to have, this was the one.
How did you react to the diagnosis?
I don’t know if anyone wants to hear that they have cancer, but it was coming from a doctor who knew what she was saying, or she wouldn’t have said it.
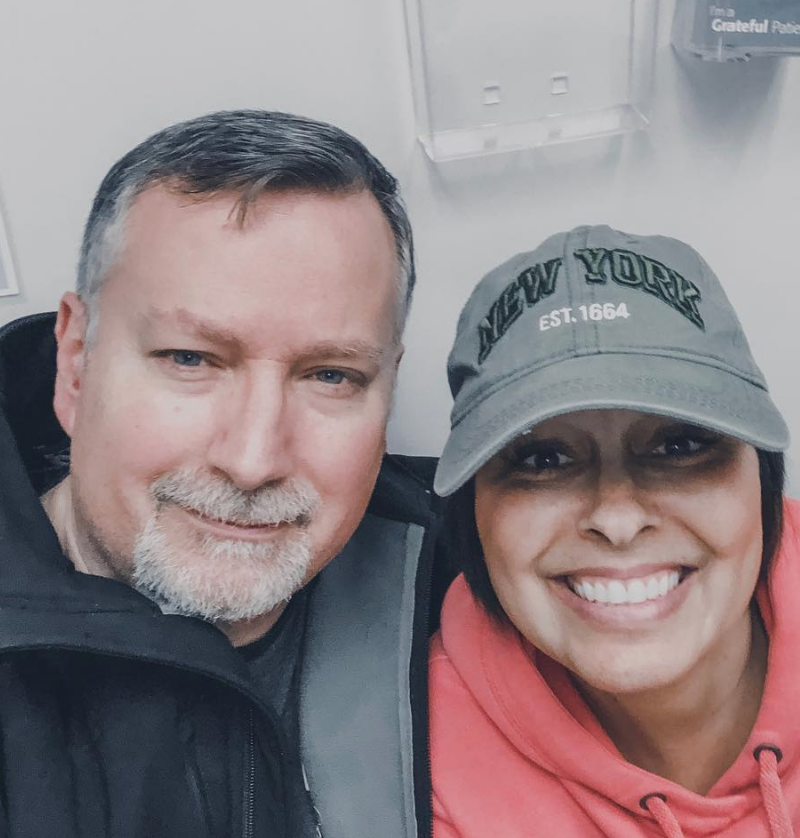
At that point, I was by myself. Then 2 weeks in after surgery, I was feeling pretty normal. My husband was working, so I said I could go by myself.
Shock. Disbelief. Sadness. Scared. Worried. All those feelings that a young mom has. I have 3 children. My youngest was just under a year.
I worried for them because this was new to me. Oftentimes when you hear cancer, you associate it with death, so of course the tears started falling from my eyes and the worry set in.

How did you break the news to your loved ones?
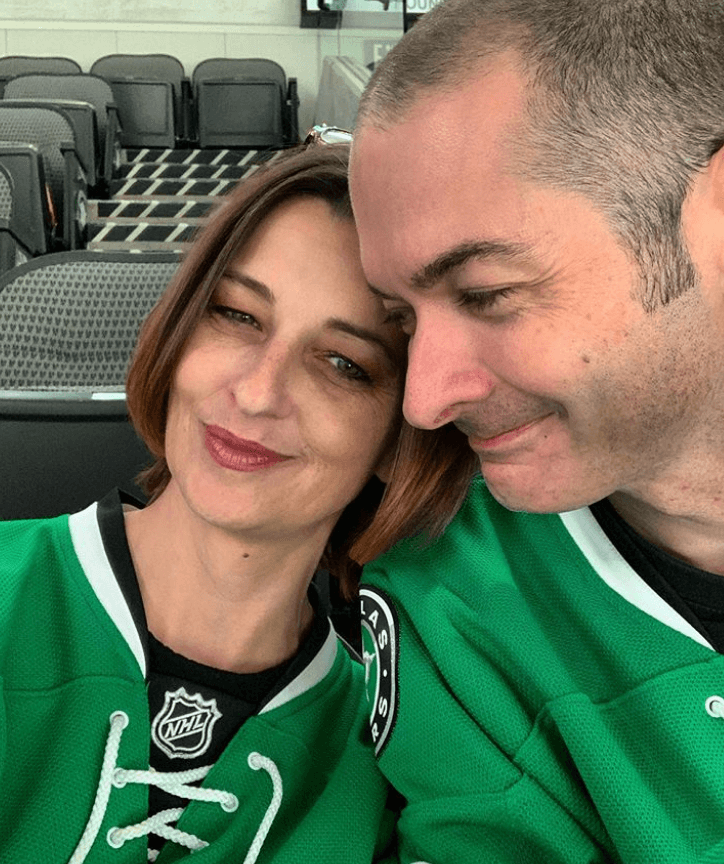
I definitely called my husband first as soon as I got in the car. I was overwhelmed and full of tears. He had me take a breath and calm down. His first question was, “What are they going to do now?”
My doctor had decided that she wanted to discuss it with the chief head surgeon of the hospital. When I left the appointment, she hadn’t given me a next course of action, so I didn’t know what to tell my husband. I was still waiting for answers myself.
He’s more of a worrier than I am. He’s a typical man, though, and keeps things within, but I know that was killing him.
I came home, and we said we were going to wait and just went back to business. Honestly, we went back to taking care of the kids [and] working. All the kids were in sports, dance, piano, so you just keep going.
»MORE: Breaking the news of a diagnosis to loved ones

Treatment Decisions
Did you get a second opinion?
The second opinion came from the chief of the hospital. My doctor called and said, “I’m going to send you to him, and he’ll talk to you about what the next steps will be.” That appointment was within a week.
When the doctor took the lump out and sent it for pathology at that hospital, the technicians damaged my sample. Instead of calling the doctor to tell her that the sample was damaged, they automatically sent it to another hospital — a cancer research hospital in Toronto. That hospital was the one who came back with the results.
It was upsetting for me that they took it upon themselves to send it away after damaging it without letting us know what happened, but at the end of the day, the results came back, and that’s what we needed to take the next step.
The chief now had both sample readings — the damaged one and the one that came back from the cancer hospital. They both said the same thing. It was stage 0 DCIS, still within its sack.
What were the next steps after getting the diagnosis confirmed?
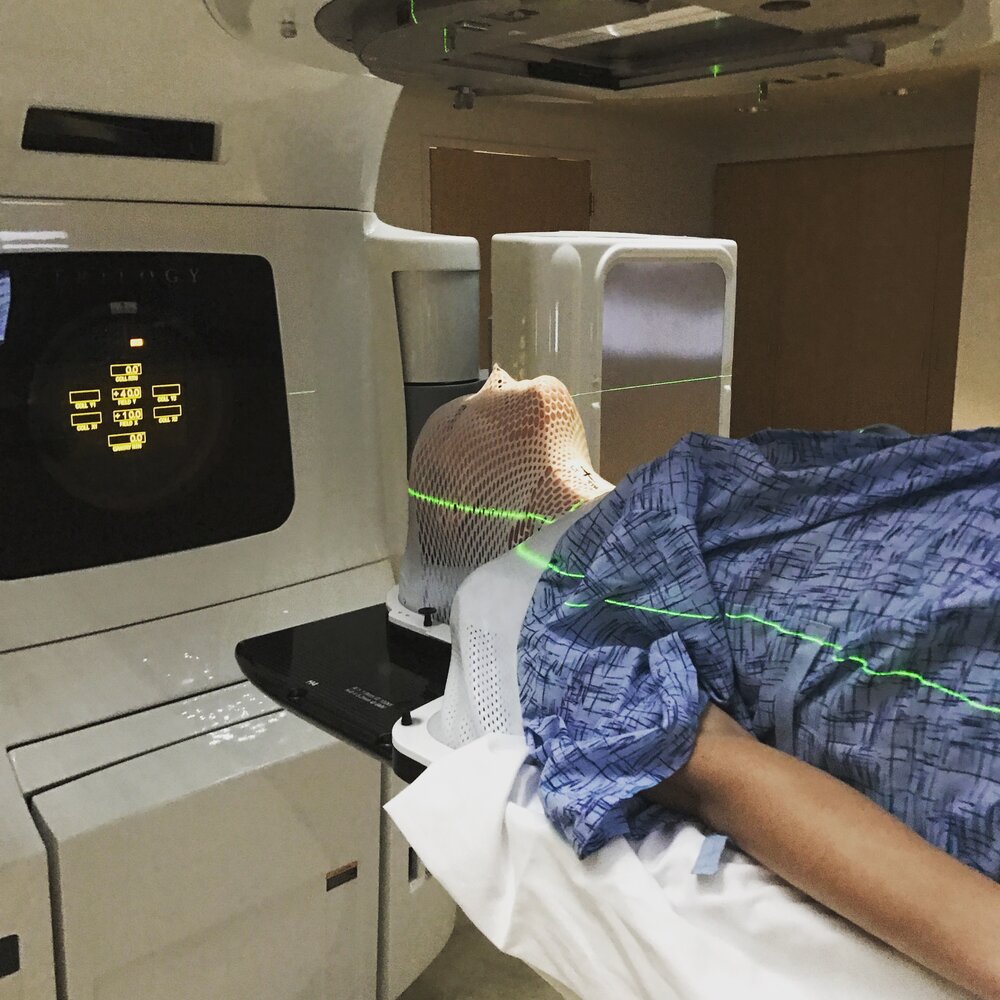
He suggested I have an MRI, and it came back that there were some suspicious spots in the marginal area near the lump. He suggested we either go in and take out more tissue — which would leave a big gouge in my breast — or have a subcutaneous mastectomy.
Subcutaneous, meaning they would leave the nipple and take out 95% of the breast tissue. He said, “Go home, talk to your husband about it, and let me know.”
I understand that a lot of things should be discussed between both parties, but that just kind of stopped me in my tracks. At the end of the day, this is my body, and this my decision.
I knew that I wanted to do what was supposed to stop the cancer from coming back again, which was to do the mastectomy.
On top of that, I knew that I had the opportunity to leave my nipples and do reconstruction, so we booked it. I told the doctor, “While we’re there, I would like to do both breasts.”
I didn’t want to have to worry later on in life about cancer resurfacing in my other breast. He suggested that I do some more research on because they usually just work on the problem breast, but I knew I wanted to do both. That was what happened. I got the double subcutaneous mastectomy.
Describe the double mastectomy complications
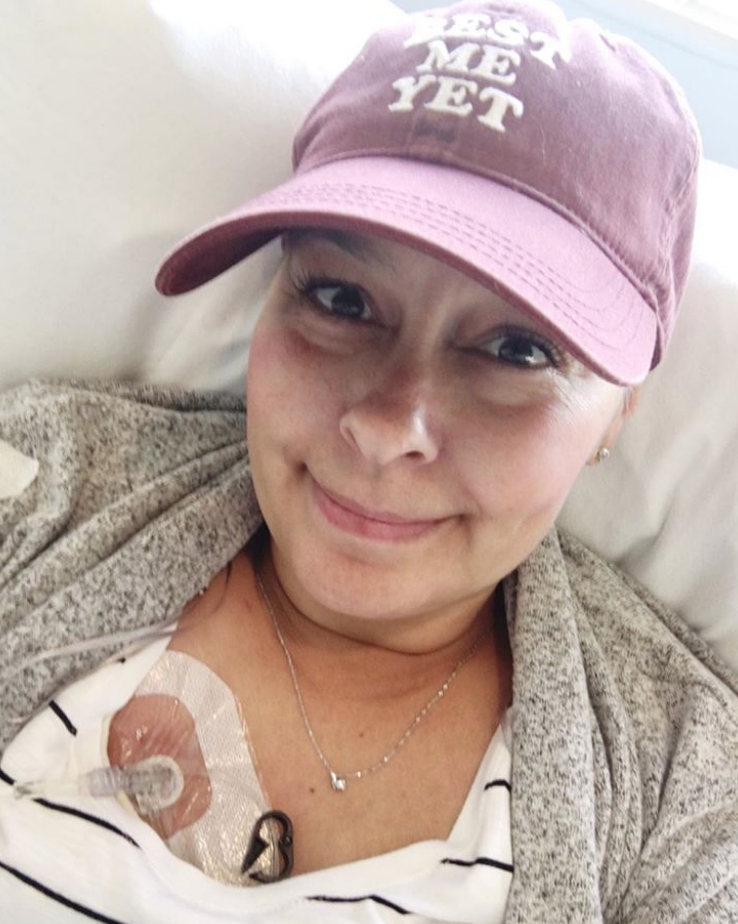
To make a long story short, I ended up having 10 surgeries with this doctor to get these breasts built back up after the subcutaneous mastectomy, including adding in the tissue expanders, the emergencies, and all that.
I formed a lot of scar tissue. That was causing a lot of problems because the implants were being squished. My breasts weren’t round. They were sort of oblong. The scar tissue was so hard and painful.
This doctor did so much research. She traveled to Europe, even, because they have a history of a lot of successful cosmetic surgeries, and she said she was going to go find out if there was a way to get rid of the scar tissue. She finally came back and said she couldn’t help me.
She found a great doctor for me at a teaching hospital in Toronto who uses a human cadaver tissue. They can use it in different parts of the body, but for me, she used it in my breast to give me some more muscle and form a hammock to hold the implant and stop the scar tissue from building. I think that took 3 or 4 surgeries with her in order to rebuild the breast.
She put in the human cadaver tissue to add to my muscle, let me heal, and had to go back in. She did fat grafting, so she took fat from my inner thighs and put it in my breasts. I had 3 sessions of that. Then she put back in the implants. That was surgery number 13.

More Diagnoses
Cancer found in nipples (Paget’s disease)
Around the time of that surgery, 8 years after diagnosis, I noticed my nipple started to look odd. My nipple was looking odd, cracked, and bleeding. It looked like how it looked when I first started nursing.
When you nurse and your baby suckles, the nipples get pretty irritated and red, and it looked like that. When I was going in for surgery 13, I told my doctor, “Look, something doesn’t look right. Maybe my nipple is finally dying after almost losing it.”
She said she would have a look at it. She took a sample of it when she was finishing up the surgery and sent it off. That came back as cancer of the nipple.
When she came back in to tell me that that was what that was, it was utter shock. First of all, I didn’t know there was such a thing as nipple cancer. Then, after going through 8 years of surgeries, you’re ready to call it a day. I was so glad to be at the end of it.
To hear that I had cancer once again, I was angry. I was thinking back to my previous doctors and how nobody informed me that there was such a thing as nipple cancer.
What did your doctor do about the nipple cancer?
What we ended up having to do was book another surgery to remove the nipple. It’s not a matter of just taking the circle. It’s taking away a good chunk of your breast tissue in order to get rid of the nipple, the areola, and the tissue around it. That was surgery number 14.
From that surgery, because she had to take so much tissue, my breasts started to basically burst open because I’d had so many surgeries. My skin and muscles were worn out.
My breasts were forming pressure ulcers. With that, I had to have surgery number 15. It was to fix the problems from the previous surgery.
She took out some extra tissue to just be sure she got all the nipple cancer, and that was great.

Then there was a third diagnosis. How did you react to that?
I went in for my results after the nipple removal, and she said, “We found more cancer.” She took out the nipple and had went in to take more tissue, and it showed that there was further DCIS in my skin.
I didn’t have tissue anymore. The bulk of what I have is muscle and implants. Of course, if you have skin, then you have connecting milk ducts, even if you just have 1% of tissue. That’s where the DCIS resurfaced.
This time, it was the weirdest feeling. It was like I had heard it so many times, I wasn’t surprised. I didn’t react right away.
I wasn’t heartbroken and sobbing. My husband had that reaction. I turned and looked at him, and he was sobbing. He looked like he was hyperventilating.
My role changed at that point. I had to console him. I was playing the role that he was to play. I asked the doctor what was next. She said, “I think we need to get rid of that whole reconstructed breast and start from scratch.”
All the surgeries I went through to get this breast back culminated in needing to remove the whole breast all over again. Surgery number 16 in the summer of 2016 was where I ended up losing the full breast again.
I was okay with that. It was like I was finally getting rid of the problem. It was like cutting off that infected limb that keeps causing other infections. We got rid of it.
Remission & Reconstruction
Deciding whether to reconstruct
After the last surgery, I just wanted to heal. I didn’t want to talk about surgeries for a while. I didn’t know if I was going to bother with reconstruction again at that point.
I just wanted to take some time and think about why I would want to rebuild them and whether or not I’d be doing it for the right reasons.
I decided that I wanted to know if I was going to rebuild because I was worried about how I looked physically or because I couldn’t live without a breast emotionally. I needed to know what my real reasons were.
I went to prosthetics. They’re great for women that don’t have breasts. They look and feel natural. Nobody could ever tell that I didn’t have a breast on one side. Because the left side was also reconstructed and part of the fat graft was shrinking, I was wearing a partial prosthetic on that side as well. I was wearing 1.5 prosthetics, and I was okay.
About a year and a half later, I decided that I wanted to try one more time. I decided I wasn’t going to let cancer win. The only option left for me was to use the LD muscle from my back. What they do is they take a good chunk of the muscle, tissue, fat, and skin, and they cut a diamond shape, bring it around your arm, and they place it where your breast will go.
From there, I had more fat grafting sessions. They had to start taking fat from different parts of my body because they had already taken from my inner thighs multiple times, and they were showing effects of that. She used fat from my abdomen.
When your fat dies, sometimes instead of absorbing back into your body, it can form an infection. That’s what happened across my whole chest.
I was on an IV and morphine until it went away. Then we proceeded with another fat grafting session since that one didn’t work.
On May 2th, 2019, I had my last surgery — which was surgery 20 — to implant more fat and put in the implant finally. What they do is they add the muscle, fat, more fat, and then the implant.
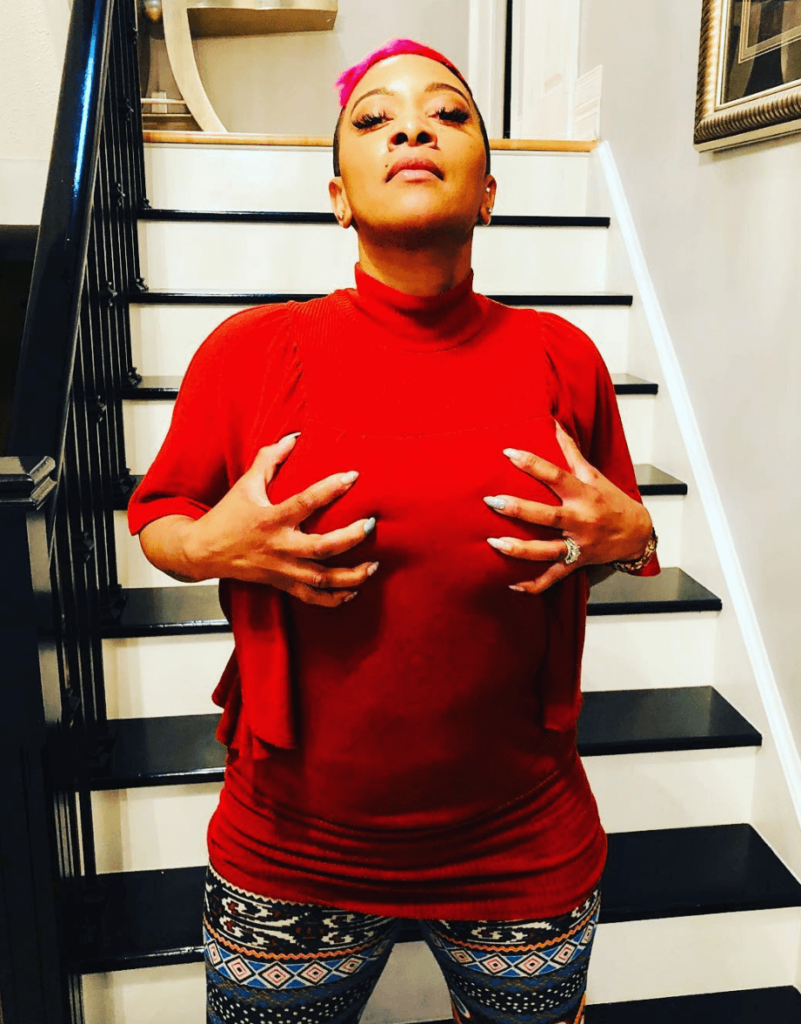
Finally, it’s completed as far as the major surgeries. To me, it’s a victory to have gotten this far. I have 2 mounds that I call my breasts. I still just have 1 nipple, but you know what, I’m fine. If I decide to add a nipple, I will. If I decide to leave it, so be it.

Is there anything you wish you had done differently during treatment?
The nipple thing was a big faux pas on a lot of people’s parts. No one told me that if I left my nipples that there was a high chance of cancer forming there.
If you’re leaving your nipple, you have to have some sort of blood supply in order for it to survive. I knew that there was 5% of the breast tissue left to keep the nipples alive, but I didn’t correlate that with cancer resurfacing.
What I wish had happened is that they would’ve given me all the answers. As doctors and health care providers, they should’ve been giving me all the possible scenarios and answers to questions I didn’t know to ask.
I made the decision that was best for me and my health, but if I don’t even know that something could happen, how was I supposed to ask those questions?

Are there any lasting side effects that you can think of from your surgeries?
With regard to the LD surgery, my doctor used so many fat grafting sessions so she didn’t have to take so much muscle from my back. I’m waiting to get back into the gym and to my regular fitness training to see if I have any mobility issues. That’s the one possible concern I could have.
Right now, I have to be gentle with my chest because they’re implants. They could always potentially rupture. With regards to my health, I go to an oncologist for him to feel around and see if he feels anything.
As far as lasting effects, my energy level isn’t perfect because of having so many of the transfusions. I have an underlying blood condition.
The doctors don’t quite know what it is. I take a lot longer to heal internally than others. I’m very low on iron, so I have to keep up on my iron pills. Other than that, I really live a full life.
What is your follow-up surveillance?
I don’t have MRIs regularly anymore, and to be honest, that’s the only thing that would keep me 100% worry-free because that’s the only thing that gives you all the answers you need.
Mammograms and ultrasounds don’t work for me anymore because I have implants. It’s a matter of physically feeling around and watching how I feel.
When I was diagnosed, I didn’t feel sick. I didn’t feel pain. There was just the lump. It’s like I don’t know what to look for, and I’m relying on the doctor to feel around and make sure nothing is wrong, and even that doesn’t give me confidence really.
It’s a matter of minutes in the appointment. I’m considering finding a new oncologist because of that. You have to advocate for yourself because you have to feel confident. If you don’t feel confident with your doctor, find a new one.
Hormone Therapy
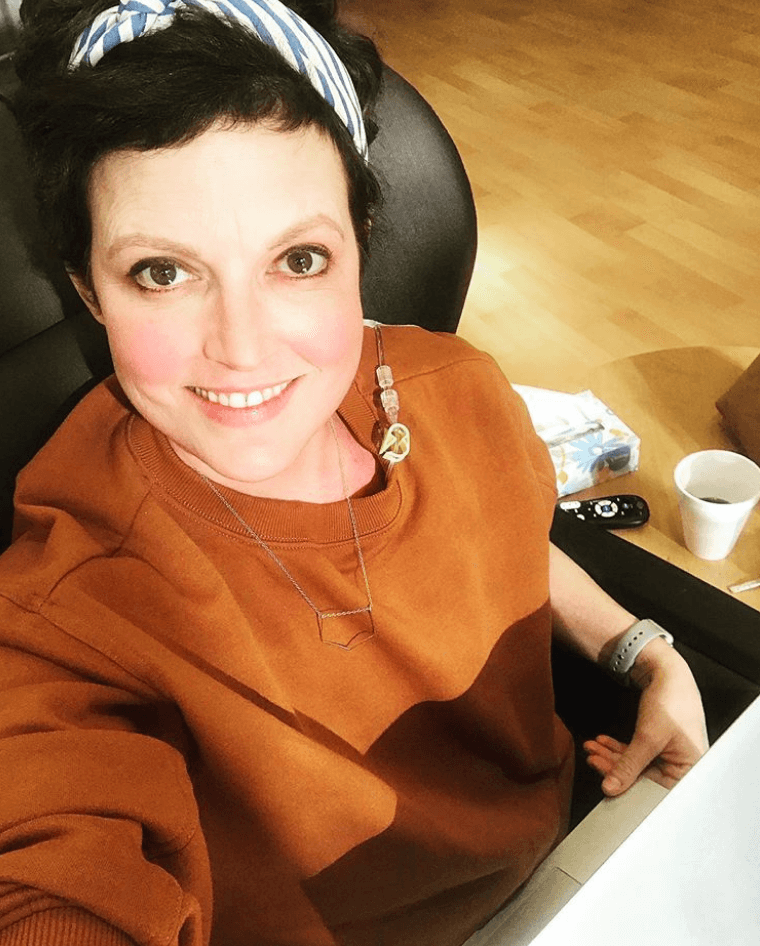
Describe the physical impacts of the hormone therapy
To be honest, there were a lot of low points in the first 5 years. When I got diagnosed, I was on the tamoxifen. The tamoxifen can throw you into early menopause. With that comes a lot of emotional struggles.
Describe the mental and emotional impacts of hormone therapy
When I speak about this, I’m very candid about it because women have to understand that when they’re on tamoxifen or any other medication like it, you’re going to feel a lot of side effects.
You’re on it for 5 years or more, so you have to learn how to deal with it.
One time I was driving home from my godmother’s house with my 3 kids in the truck, and I felt this overwhelming feeling to turn the wheel and drive the car over the bridge or to drive the car into another truck. It was just so overwhelming.
The drug plays tricks on you. You become depressed. There were a lot of dark moments. I recall a lot of times in the shower, wanting to be in the dark just sitting in the tub.

Quality of Life Reflections
The emotional impact of treatment
A lot of people think reconstructive surgeries are just reconstruction. You’re going through a lot of emotions because you’re not just fixing your physical body. It takes you back to the real reason why you’re even having the surgery in the first place.
You have to deal with the bad C-word: cancer. Like I said before, it’s hard not to associate cancer with death. You worry for your children. You worry that it’s going to come back. You just worry all the time that you’re not going to make it through surgery.
Even though they’re cosmetic or sort of routine-seeming surgeries, you’re always scared you won’t make it through because anything can happen. Each surgery I had, it played on my mind.
Even after this last surgery, I still think about it. I wonder if it’s ever going to come back. I don’t let it consume me, but I do wonder. Now that I have implants and that physical part is built back, I sometimes wonder if I risk masking cancer if it comes back.
I think that’s a big reason why a lot of women choose not to rebuild. They don’t want to hide the possibility of finding the cancer again at a later date if it shows up.
I trust in the technology and doctors, and I trust in God. I try to live my life as best as possible. I try to do good and support and give back, and I feel that I’m putting positive light out into the universe and hoping to get some of that back.
What helped you deal with this level of stress?
I went to my family doctor and said, “Something’s got to give here, because I’m not doing well. I’m arguing with my husband about things I wouldn’t ever argue about. I took a trip to Mexico for a week by myself. I’m doing all these crazy things.” I knew something was going on.
She put me on a very light antidepressant to bring the melatonin levels up to the happy place. I don’t know that I like this idea — give me medication to fix a problem and another to fix the problems the other caused — but it helped. I was weaned off of it within 7 or 8 months. That limited the stress.
In that time, I went to counseling, and I learned how to limit my stress levels because stress is a killer in and of itself. I knew I had to keep that under control. I knew I had to contain myself because I knew I couldn’t keep welling up like that.
I know that God spared me 3 times in not giving me such a late stage of cancer each time it was found. We had it taken care of. I knew I was here for a reason. I try to do things right. I eat well, exercise, give back, and I talk.
Speaking about it is what’s really helpful. When you get all the heavy stuff off, it’s almost as if you’re saying, “Here. Someone else carry this for a while.”
It feels so much better and so much lighter. That’s what I do right now as a business, and it’s really helped me.
How important is it to have caregivers and support?
There are caregivers in many forms. There are your doctors, obviously. There’s your partner. They’re the ones that are going to give you emotional support you need.
There’s the support of your friends that’s going to take loads off as far as your kids and activities they need to get to, and your house — helping keep it in order when you’re low. Your parents are there to give support.
There are your church and people of faith around you to help you build yourself up within. Without having that, it doesn’t make sense. If you don’t have faith that you’re going to be okay, you’re probably not going to be okay. You have to put the positivity out there in the universe, and that universe for me is my faith.
Your children give you support, too. They remind you that you always have something to look forward to. You have to be here to see them grow. You have to be at their graduations, games, weddings, and all that. It motivates you, and that’s caregiving.
»MORE: What kind of support cancer patients say helped the most
How was it being a young mother and being diagnosed with cancer?
Because it spanned for so many years, I had to deal with it in different ways. My oldest is 19 now, the middle is 14, and my youngest is 11. In the early years, my youngest, my son, was a newborn. My middle would’ve been about 4, and my oldest would’ve been about 9.
They were too young to explain the details. They knew that Mommy was sick and she was going to have surgeries, but she was going to be okay.
As the years went on, they knew I had cancer, they knew it was in an early stage, and they knew I had to be on medication to keep the cancer from coming back. They knew I was going to rebuild and that I have fake boobies. They would see my prosthetics in the bathroom, or sometimes I would just take them off because they’re uncomfortable.
When it came back in 2016 is when I sat down with all of them. At this point, it was a different kind of conversation. I didn’t want to keep things from them. This time, I told them it was the cancer I had before but had come back again. I told them it was going to go away, and I wouldn’t have to go through chemo or radiation, but I was going to need more surgeries to get rid of it. They understood.
They were still concerned, but I had to reassure them over and over again that I would be okay. I can only imagine what they were going through in their heads. I know how my husband and I felt when the cancer came back, so I can only imagine what they were going through. That was the hard part for me.

I needed to learn how to not wrap myself so much in the fact that I was in so much pain, and I needed to be there for my kids. I think that’s what forced me to get up and going so soon after all the surgeries.
I needed for them to see me normal. For me, it would mean that they knew I was okay. I think had I been in bed all the time, they would’ve thought I wasn’t okay.
My eldest daughter is like her dad. She’s more stoic. She wasn’t around with me much. She would ask if I needed anything, and she would message my other daughter to see if I was okay, but she stayed in her room a lot.
Much like my husband dealt with it, she was worried. She didn’t like to see me in pain. Seeing me that way was hard for her.
That’s part of what I’ve learned through my healing process. I had to learn how other people grieve and deal with emotional struggle. People deal with it differently, but that doesn’t mean that one cares less than the other does.
»MORE: Parents describe how they handled cancer with their kids
Were there times during treatment you had to advocate for yourself?
I saw an additional oncologist other than the initial doctor and aside from the chief head surgeon. They sent me to an oncologist. It was like I was the doctor, and he was the patient.
He said, “You had the mastectomy, so you don’t need to do anything. You’re good.” I said, “Well, what does that mean?” He said I was going to see the chief surgeon at the hospital, and he would tell me what to do next.
I said, “They sent me to you for a reason. I didn’t have a mastectomy. I’m going to have a subcutaneous mastectomy. They’re 2 different things.” He said, “Oh. Let me look at the chart.”
If you’re a doctor, you should be right. There’s a difference between the subcutaneous mastectomy and a mastectomy. The subcutaneous mastectomy where I left my nipples is why the cancer came back the second time.
If he was being diligent and looked at his chart, maybe he could’ve advised me further and said, “If you’re concerned about it coming back, you should know there’s a possibility of nipple cancer.”
I didn’t know about nipple cancer back then. After getting it, I realized there were so many things I didn’t know. I researched some more, and the onus should’ve been on the doctors.
Do you have any advice on self-advocacy for others?
You’re not just a number. These doctors have a lot of patients, but you’re a human. You go in there and let them know you’re not a number. You have concerns about your health, and your doctors should be concerned about you.

While you’re there, if you don’t understand something, tell them. If they say you need to do something and you don’t understand it, say something. If they’re failing to tell you that you need to do something, ask.
If there’s something that another doctor has recommended and this one isn’t, bring it up. I think that women should find another doctor if they’re not comfortable with the one they have.
Perhaps bring someone with you. In your time of turmoil and stress, you’re not going to have the wherewithal to ask all the questions you need to, so bring someone with you.
Research, ask questions, [and] tell them you want all your information so you can take it to another doctor if they’re not meeting your needs. You’re entitled to your scans. That’s your body.
If you don’t understand the lingo, tell them. Say, “I don’t understand what you’re saying. I’m not a doctor. Can you explain that to me?”
»MORE: How to be a self-advocate as a patient
How was the financial aspect of going through treatment?
I’m in a position where we’re financially okay. I could stay home and not work a day in my life. My husband’s business can take care of everything, but I’m not that girl. I’ve been working since I was 13. I love to work. I’m an independent woman. I like to have my own money that I know I brought in.
I like to activate both sides of my brain. I’m creative. I’m a licensed paralegal, but I’m also a decorator and stager, motivational speaker, and makeup artist.
I have my hands in a lot of things part-time. I don’t overdo it because physically, I need to take care of my health. I work as casual as I want to.
In Canada, we have unemployment insurance. You pay into that when you’re working, and it can kick in if you apply for it, but it only covers part of it. Your bills are not going to change just because you’re sick. Your mortgage isn’t going to change because you’re sick.
You want to keep your children in some normalcy, and life must go on. What happens then? For a lot of people, it is hard. I haven’t had the issue, but I understand it. I help women I talk to now with their utilities, groceries, transportation to and from the hospital, things like that.

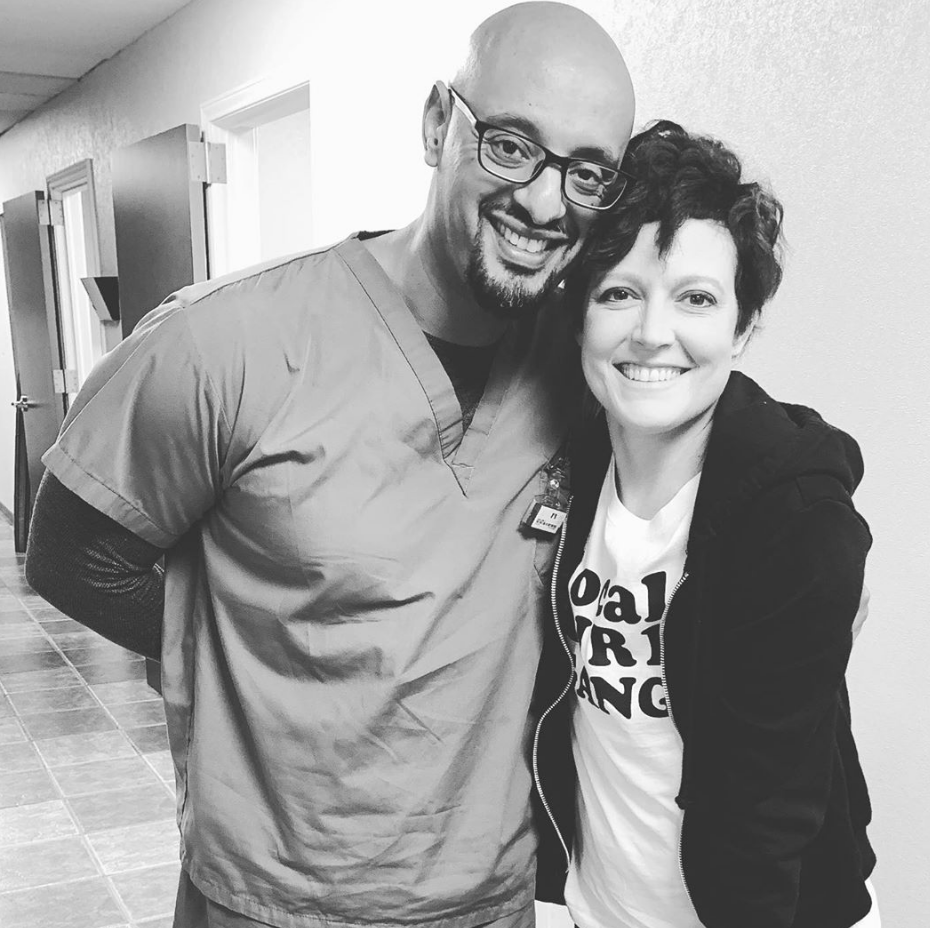
Your cancer inspired the work you do now
In 2016, when I realized I had been through cancer 3 times and was still standing, I had to do something with that. There was no reason why I shouldn’t be imparting what I’d learned through my experience to women who might be in a similar situation.
I went through all those stages of healing until I got to an end stage of philanthropy, where I just felt so overwhelmed and wanted to give back. I wanted to share how I was able to persevere through each circumstance. I wanted to show that I’d been through the dark times and depression and prove that you have to persevere. At the end of each day, there’s a beginning of another.
High Heal Diaries is a platform where women can share their stories with other women. Nobody’s judging anybody.
The platform comes in different forms. I do a YouTube talk show. I do the keynote speaking engagements. I do life-coaching. I’m a certified coach practitioner. For those not at a place yet where they are able to speak about their issues in a public form and want help, I can help them get there. I do inner and outer beauty makeovers.
I believe in look good, feel better. I believe when you feel good on the outside, it transcends and transforms how you feel on the inside.
If you look in the mirror when you’re sick and think you look horrible, you’re going to feel horrible.
If you put a little makeup on, get your hair done, and you smile at what you see in the mirror, you’re going to feel happier. If a woman is going through a struggle, we’ll help them with wardrobe shopping, maybe a little makeup, skincare, facials, whatever, in order to help them feel better about the outside and then coach the stuff on the inside.
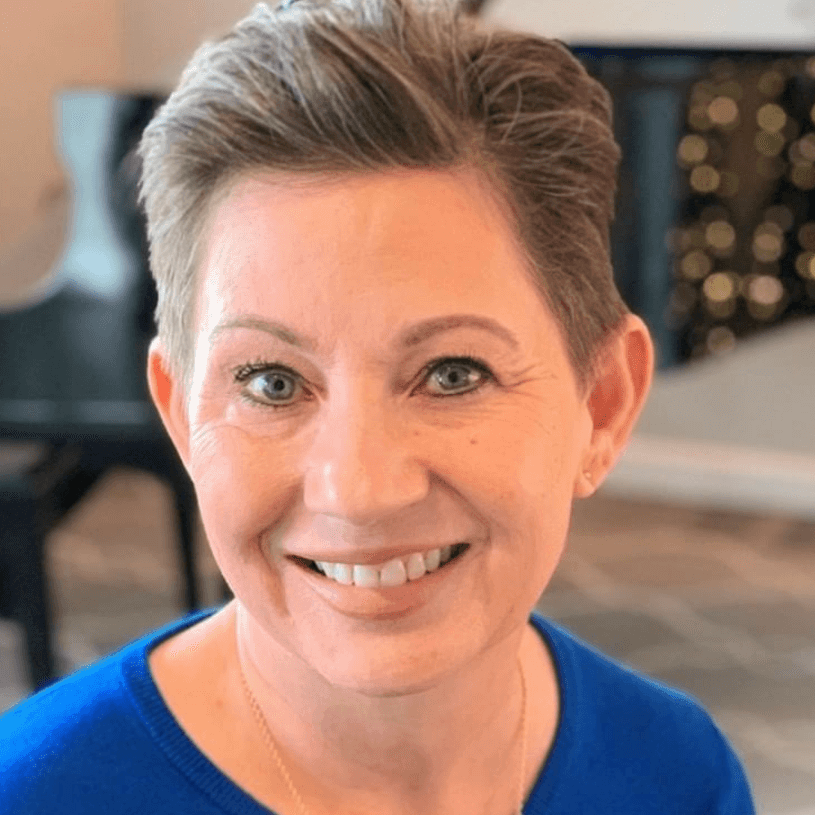
What is your “new normal” after cancer?
The new normal is really busy. The new normal for me is living a good, full life. It is not taking everything on. I’ve become a little more selfish. It’s not a bad selfish. I come first. If I’m not good, then nobody else is going to be good.
For my kids, if I want to sleep until 12 in the afternoon, they’re old enough to go downstairs and make themselves breakfast if I need to rest. Far too often, women put everybody else in front of themselves. We mask all of our issues. We take care of everyone else, but we mask our own.
On top of that, I don’t want cancer to ever come back. I think I’ve learned what I need to learn now. I would never take away the fact that I had cancer, though. I would never change that part of my life because I’ve become a better person.
I wouldn’t be doing the things I’m doing now had I not had cancer. It’s sad that this had to happen, but sometimes these are the kind of things that have to happen before people realize that they need to change things up a little bit.
Do you have any final words for anybody who may be going through something similar?
I just want women to understand that there are a lot of things out there in society and the environment that we need to cognizant of as far as what we’re putting in our bodies. I’m not going to go off on a tangent about doing all these drastic things because everybody’s going to do what they need to do, but a lot of times we just live, and we do. Sometimes we need to think of how we live and what we do because everything has ramifications.
Also, I’m not preaching. I’m not one of those Bible thumpers, but you have to believe in something. You have to believe in a higher power, because we are not doing it on our own. You have to believe that although you might be sick, you have to pick up and keep going as best as you can.
If you have a cancer or struggle that you feel like you can’t make it out of, you need to be able to say, “If tomorrow I’m taken away, at least I can say that the life I lived was happy and I did things right.”
The life you’re living right now, make the most of it.

Inspired by Natalie's story?
Share your story, too!
Combination Breast Cancer Stories
No post found