What’s Promising in Multiple Myeloma Treatment?
Dr. Saad Usmani & Cindy Chmielewski

What are the emerging, most promising therapy options potentially available in 2022/2023?
Cindy Chmielewski (@MyelomaTeacher) talks with Dr. Saad Usmani, Chief of Myeloma Service at Memorial Sloan Kettering, about CAR T-cell therapy, bispecific antibodies, novel therapies and combination therapies, focusing on the relapsed/refractory patient population along with newly-diagnosed myeloma patients.

Thank you to Janssen for its support of our educational program. The Patient Story has full editorial control of our content.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- CAR T-cell therapy
- Who might have a greater tendency for severe neurotoxicity?
- Allogeneic CAR T-cell therapy
- Efficacy of allogeneic CAR T-cell therapy
- Are there any CAR T-cell therapies that are looking at different targets on the myeloma cell?
- Bispecific antibodies
- Possibility of getting bispecific antibodies at a community hospital
- Side effects of bispecific antibodies
- Frequency of subcutaneous injection
- Efficacy in comparison to CAR T-cell therapy
- Talquetamab
- Bispecifics with other targets
- Combination therapy
- Earlier lines of treatment
- DETERMINATION trial
- ENDURANCE Trial
- New & exciting studies
- CAR T-cell therapy for transplant-ineligible patients
- Words of wisdom
- What will cure myeloma?
Introduction
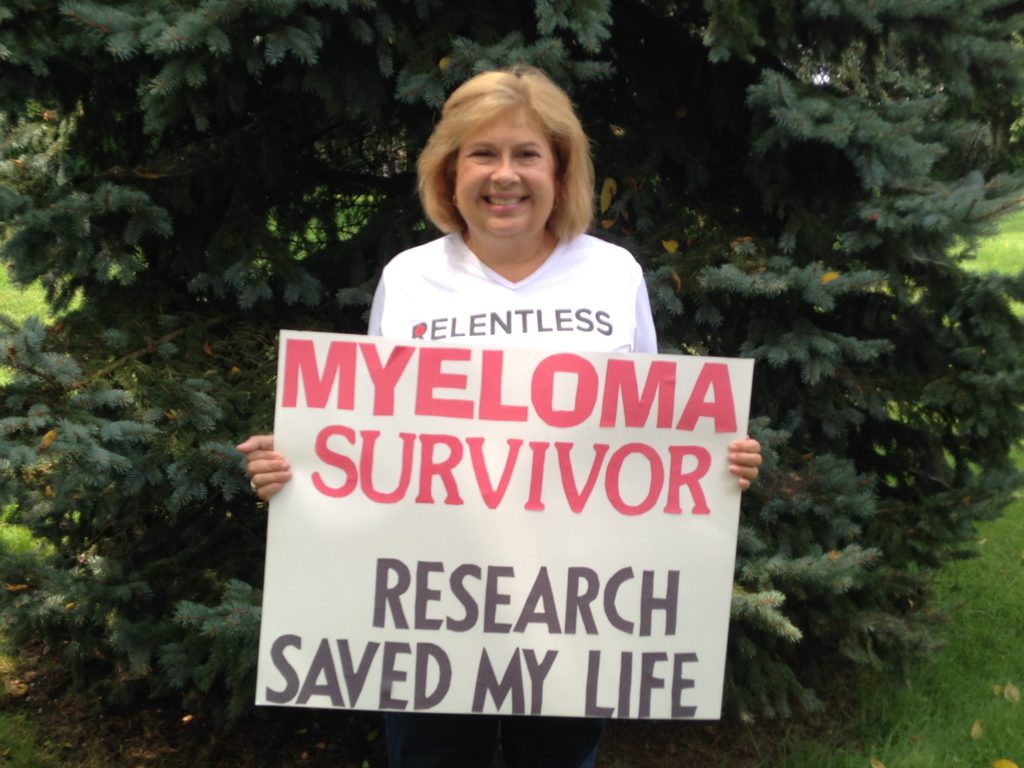
Cindy Chmielewski, @MyelomaTeacher: I’ve been living with myeloma since 2008 and more recently, became a research advocate in the multiple myeloma community.
Saad Z. Usmani, MD, MBA, FACP: I’m the chief of the Myeloma Service at Memorial Sloan Kettering Cancer Center in New York. I’ve been involved with myeloma research both on the clinical and translational side for well over a decade. I’m looking forward to so many exciting things that we have in the field and how things are moving forward for our myeloma patients.

CAR T-cell therapy
What is it & who are they for?
CC: There have been some meetings going on. There’s ASCO and EHA and the IMW is coming up. There are a lot of things happening in multiple myeloma.
Let’s start talking about the CAR Ts because CAR Ts have been around for a while. There are two approved CAR Ts. Can you talk a little about them and who they’re for?
Dr. Usmani: CAR T-cell therapies have been around for a while. They started early on in another disease — ALL in children, actually — but the ones that have been developed in myeloma are targeting a specific surface protein on the myeloma cells called BCMA.
There are two that are FDA-approved for patients who have had four or more prior lines of treatment — including a proteasome inhibitor immunomodulatory drug as well as anti-CD 38 monoclonal antibodies — people who have had a lot of prior therapy.
Those two products are called ide-cel and cilta-cel and they both target BCMA, but they are unique products. The general side effects are similar but tend to happen at different time points. Both products actually show good clinical activity.
The patient’s T-cells are taught to recognize the cancer cell and they’re grown outside the patient’s body in the lab.
Dr. Usmani
Where can you get CAR T-cell therapy?
CC: These CAR T-cells have to be given in a center of excellence, is that correct? I can’t just go to my doctor and say I want some CAR T treatment.
Dr. Usmani: These are cell therapy products so they need to be given at a center that does transplant and cell therapies. Many of our myeloma patients go for a transplant evaluation and end up getting a stem cell transplant during the early course of their treatment.
The process is similar. Your doctor is going to refer you to a transplant center. They will do the evaluation and then get you those commercial products.
Typically, when you’re getting a stem cell transplant, you go through a process of getting growth factor shots and then getting the stem cells collected from your bloodstream through central venous access. In CAR T-cell therapy, we are selecting T-cells from the patient’s peripheral blood, but you don’t need growth factor shots so you can get those T-cells collected just off of the peripheral bloodstream.
Side effects of CAR T-cell therapy
CC: There are some unique side effects to CAR T-cell therapy that maybe myeloma patients haven’t experienced before. Can we talk a little bit about them?
Dr. Usmani: When you get these T-cells from the patients, you send them off to the specific company that’s manufacturing them. What happens is the patient’s T-cells are taught to recognize the cancer cell and they’re grown outside the patient’s body in the lab essentially; that production and expansion takes 3 to 4 weeks. When that product is ready, it’s shipped back to the center and patients get a certain lymphodepleting chemotherapy for three days before they get that product infused through the veins.
Those T-cells are active. They know how to recognize the cancer cells through the surface marker BCMA and they’re going to expand. There’s an expansion that happens in the patient’s bloodstream. These cells are growing and trying to go after the myeloma cells. It’s like introducing an inflammatory response in the patient.
The side effects are like the patient’s body is going through an inflammatory process. The two common side effects are what’s called cytokine release syndrome. These immune cells are releasing certain chemicals that enable them to go after the target. Due to that, patients can feel fevers [and] hypertension, as if they were infected with something. That tends to happen with ide-cel within the first two days. With cilta-cel, it tends to happen with a delay of 5 to 6 days typically.
We manage those side effects by giving antipyretics, fluids, sometimes steroids, or an antibody called Tocilizumab to patients. But for the most part, these side effects are grade one or two. They’re low-grade and are managed with those kinds of medications.
The other side effect that can happen because these T-cells are active is what we call neurologic side effects. Sometimes patients can feel loopy or have neuropathy. Very rarely, patients can have more serious neurologic side effects, such as seizures. Those tend to happen in a very low proportion of patients. Neurotoxicity tends to happen more commonly with ALL CAR T-cells rather than the myeloma CAR T-cells.
The side effects are like the patient’s body is going through an inflammatory process. But for the most part, these side effects are grade one or two. They’re low-grade and are managed with medications.
Dr. Usmani
Who might have a greater tendency for severe neurotoxicity?
CC: Are there any biomarkers that predict who might have a greater tendency for severe neurotoxicity? Or is that just up in the air?
Dr. Usmani: What we’ve observed is patients who have a higher burden of disease at the time of getting CAR T-cell therapy can be at a higher chance of developing these side effects. One can develop CRS and neurotoxicity independent of each other so it’s not that they come in as a package. In fact, CRS is more common. Neurotoxicity tends to happen in less than 10% of the patients. CRS tends to happen in almost all patients to some degree.
There aren’t typically specific markers that we can follow that are specific for CRS or neurotoxicity. There are certain markers that can give you a hint that there is a heightened sense of inflammation, like serum ferritin levels or CRP elevations in patients. We tend to follow some of those labs, but they’re not predictive. They’re just telling you that something is going on, just be careful.
Patients who have a higher burden of disease at the time of getting CAR T-cell therapy can be at a higher chance of developing these side effects.
Dr. Usmani
Are there any trials for more newly diagnosed patients or first relapse?
CC: The currently approved CAR Ts are for more heavily pre-treated patients who’ve exhausted many of the options. Are there any trials that have been reported for more newly diagnosed or first relapse? Are they coming closer?
Dr. Usmani: There are two randomized phase 3 studies that have looked at comparing each of these CAR Ts — both ide-cel as well as cilta-cel — in one to three prior lines of treatment comparing them to the standard of care triplet regimens. In fact, BMS (Bristol Myers Squibb) just announced that their phase 3 trial in one to three prior lines of treatment is coming out positive. Now, this was a company announcement so we haven’t seen the data but that is good news for our patients. I’m keen to hear more about this.
The key is the process [of] CAR T-cell therapy. It takes a while for that production time and so there are certain bottlenecks to the process.
Dr. Usmani
We do have smaller cohort studies that have reported out experience in one to three prior lines or early relapse patients with very high response rates of 80, 90% with Cilta-cel. In fact, well over 90% with Cilta-cel. We just need more updated data, though those are looking promising.
The key is the process [of] CAR T-cell therapy. It takes a while for that production time and so there are certain bottlenecks to the process. The big question is how applicable this technology will be to all patients that we treat.
Allogeneic CAR T-cell therapy
CC: What about allogeneic CAR Ts? Are they going anywhere? What are they? Can you explain? They seemed a little exciting.
Dr. Usmani: The idea of allo CAR Ts is you can take T-cells from a donor but knock out certain surface markers to make those T-cells more benign so that the recipient’s immune system is not recognizing them as the enemy and they’re not recognizing the recipient’s immune system as the enemy.
The advantage of having allo T-cells utilized to manufacture CARs is you can have one donor and make a product that can be given to a hundred different patients instead of taking the patient’s own T-cells. And those hundreds of products can be given in a very short duration of time. Essentially, if I see a patient today and I have an allo CAR T available, that patient can technically get that product three or four days from now. They can start getting lymphodepleting chemotherapy and they can get that product very quickly. Whereas if I were to see a patient today and try to collect their T-cells, even with everything aligning, it might take 5 to 6 weeks for them from today to get that product. That’s the major advantage of allo CAR T products, but they’re way behind in terms of clinical development and seeing the light of day.
The advantage of having allo T-cells utilized to manufacture CARs is you can have one donor and make a product that can be given to a hundred different patients… but they’re way behind in terms of clinical development and seeing the light of day.
Dr. Usmani
Efficacy of allogeneic CAR T-cell therapy
CC: Do we have any efficacy data? Are they working?
Dr. Usmani: They are working. We have seen some efficacy data. There’s an Allogene CAR product. In fact, Sham Mailankody from my program presented those data [in 2021] showing about 60% of the patients responding to that allo CAR product.
Now, the follow-up is short. We know that these patients, too, get CRS and neurologic side effects but the follow-up was only about three or four months so we need [a] longer follow-up to see. Is this activity long-lasting or just a short-duration activity? What kind of long-term side effects do we get from using this strategy?
Are there any CAR T-cell therapies that are looking at different targets on the myeloma cell?
CC: Right now, the approved ones go after BCMA. Are there any CAR T-cell therapies that are looking at different targets on the myeloma cell?
Dr. Usmani: Yes. Another target is called GPRC5D. That was a homegrown CAR T at MSK (Memorial Sloan Kettering) that Dr. Mailankody presented, showing good activity in patients who have had prior BCMA CAR Ts and BCMA therapies as well. The response rates, again, [are] in [the] high 60, 70% range looking at the various cell doses that the patients received. That CAR T is now being developed by BMS. There are other programs that are utilizing that CAR T.
We also have some very interesting dual CAR T data — BCMA and CD19 CAR T — that was presented by colleagues from China at the ASCO and EHA meeting showing high response rates.
The cool thing about that platform was the short production time. That product was manufactured within 48 hours. What we’re seeing is the new platforms are actually reducing the production time and that will be a good challenger to the allo CAR T strategy. If we are able to shorten that time, then there might not be as big an advantage for an allo CAR compared to [a] patient’s own T-cells.
Bispecific antibodies
Teclistamab
CC: Moving on to other types of T-cell redirection, there’s the bispecific antibody. There’s one that I hear it’s almost ready to be approved. Can we talk a little about Teclistamab?
Dr. Usmani: It got a favorable response from EMA, but it’s not yet approved. We’re waiting to hear from the FDA. I’ve been involved with Teclistamab from the very beginning. In fact, the first patient who was ever treated in the world was my patient. I’ve been with that program from cohort one, patient one.
CAR T-cell therapies are very effective, but bispecifics are therapies that will change how we manage patients in the community at large. They actually might challenge CAR T-cell therapies because they’re an off-the-shelf option, giving high response rates of, again, 60, 70% in relapse/refractory myelomas — [a] very similar patient population to CAR T-cell therapies — and it’s given subcutaneously.
Now, cytokine release syndrome is something that we see with the bispecific antibodies as well and that’s something that we have to watch out for.
The concept of this technology is very interesting. You’re going to hear TCE or T-cell engager as terminology. You’re going to hear bispecific antibody as terminology. The concept is the same. One part of that molecule recognizes the surface marker on myeloma cells. It could be anything. It could be BCMA, it could be GPRC5D, or something else. The other part of that molecule recognizes the T-cells. There is surface marker CD3 that recognizes.
The difference between [a] T-cell engager and bispecific antibody is the structure of that molecule. If it’s a whole antibody, then you call it a bispecific antibody. If it’s only a fragment of an antibody, you call it a T-cell engager.
Different companies and platforms have different molecule structures that are proprietary so the names are going to be different. Long explanation but a lot of excitement about that technology.
Teclistamab is the frontrunner. We might hear some good news about it later [in 2022] in the US and Europe. We’re all really excited about that platform.
Possibility of getting bispecific antibodies at a community hospital
CC: For patients, it’s exciting because it doesn’t involve having to probably relocate like the CAR T-cells. You have to go to a CAR T center and spend time away maybe from your home and family. Would the bispecifics be something that could be given maybe at [a] community hospital? Or is it something that you need to go away for?
Dr. Usmani: I think there will be a learning curve for our community physicians because giving bispecifics does require some education and comfort in managing cytokine release syndrome. It’s quite possible that they might ask the academic centers to give the first cycle of treatment.
Patients do need to be monitored during that first cycle as they’re going through the various step of dosing to full dose for that cytokine release syndrome. And because our community colleagues don’t see myeloma as frequently as some of the other solid tumors, they might ask us to give that first cycle.
Once patients are beyond that first cycle, it’s like getting any subcutaneous treatment so the short answer is yes, it will be possible for patients to receive this treatment out in the community. But I don’t see this happening during the first year of the FDA approval. It will be a steep learning curve for our community docs.
Side effects of bispecific antibodies
CC: Usually after the first cycle or two, the CRS and the neurotoxicity seem to go away?
Dr. Usmani: The likelihood of having those side effects is during the first three or four doses, so that first month. It’s really about engaging the T-cells.
Once the T-cells are active, they know exactly what to do, and they’re fine with the job assigned to them, it’s that early part where you’re trying to say go and kill the myeloma cells. They get revved up and release those cytokines. Once that process is done, the risk goes down to negligible.
Yes, it will be possible for patients to receive this treatment out in the community. But I don’t see this happening during the first year of the FDA approval.
Dr. Usmani
Frequency of subcutaneous injection
CC: For Teclistamab, is the infusion weekly [or] monthly? How often would I need to get this subcu injection?
Dr. Usmani: The subcu injection is on a weekly basis. [For] the first ten days, the step of dosing is given every fourth day for the first two doses before you get the full dose. That’s how it was done in the studies. I would be surprised if the FDA-approved label says something different. But again, we will know what the FDA says later [in 2022].
Very interesting and very encouraging data for our patients who have had triple-class refractory disease.
Dr. Usmani
Efficacy in comparison to CAR T-cell therapy
CC: What about the efficacy? How does it compare to CAR Ts?
Dr. Usmani: Response rates are around 63, 64%, which is very high. The median PFS (progression-free survival) is about a year, almost 12 months. The approvals for Carfilzomib, Pomalidomide, and even Daratumumab, the response rates were 25 to 30% for each of those products and the PFS for those products was about four months.
That gives you the context that you have this bispecific antibody, these are patients who have progressed on treatments like Carfilzomib, Pomalidomide, and Daratumumab, and you’re still seeing these high response rates and median PFS. In fact, the median PFS is similar to what was reported for ide-cel. Ide-cel’s PFS was less than a year and the response rates were over 70%, but median PFS was in a similar range. Very interesting and very encouraging data for our patients who have had triple-class refractory disease.
Talquetamab
CC: There are other bispecifics besides Teclistamab. There’s Talquetamab. Is that going after the same target or a different target?
Dr. Usmani: It’s in the same patient population, but the target is GPRC5D. GPRC5D is a unique target to plasma cells. Talquetamab appears to be active. Response rates are up in the 60% as well.
We don’t have the PFS data because the development of that particular bispecific is a little behind Teclistamab, but we’re seeing activity of Talquetamab even in patients who have had BCMA-directed treatments, including CAR Ts and bispecific. It’s looking very promising.
Bispecifics with other targets
CC: There are many others, not just these two. There are a lot of bispecifics out there. Are they all doing quite as well?
Dr. Usmani: Yes. For BCMA-directed bispecifics, there are several options. Elranatamab is very active. ABBV-838 is very active. There’s a Regeneron bispecific. There’s a BMS Celgene T-cell engager that’s targeting BCMA as well. All of them are showing very similar activity. I think there are some differences in the safety profile percentage of patients getting cytokine release syndrome when they’re getting it. Some of those issues will be the distinguishing factors.
There are some that are given less frequently. I think the AbbVie bispecific, which was actually developed by a smaller company called Teneobio, is given every three weeks. There will be some nuances or differences between these BCMA-directed bispecific.
It’s good to know that there are other targets where we can see good clinical activity in patients.
Dr. Usmani
For GPRC5D, we only have one, but there are others that are in early development.
We have another target called FcRH5. There’s an antibody called Cevostamab, which appears to be active, [with] response rates of about 50% in patients who have relapsed/refractory myeloma beyond four lines of treatment.
It’s good to know that there are other targets where we see beyond BCMA and even GPRC5D where we can see good clinical activity in patients.
CC: As a patient, that makes me feel good. Even though some people say you might be able to use another BCMA-directed therapy, for me, I would like to have another target in my back pocket.
Combination therapy
TRIMM-2 Trial
CC: TRIMM trials are not only using the bispecifics, but they’re combining them with things. Can you talk a little bit about those?
Dr. Usmani: Once the efficacy and recommended phase 2 dose of both Teclistamab and Talquetamab were ascertained, the next step was can we combine them with other myeloma treatments and see if we get better clinical activity.
The TRIMM-2 study is looking at the subcutaneous Daratumumab administered with Talquetamab as well as with Teclistamab. There is a combination study of adding Pomalidomide to those combinations as well. We haven’t heard about the Pom combos, but we know the subcu data combinations. They have been reported out by my colleagues — Drs. Krishnan, Ajai Chari, van de Donk — each of them presented these data at different congresses over the past six or eight months, and I’ve participated in those studies as well. The overall response rate with each of those combinations is about 80 odd percent, which is remarkable because most of these patients were Daratumumab refractory in a previous line of treatment.
Why are we seeing a higher response rate compared to what we would expect with Teclistamab and Talquetamab? Daratumumab also is inhibitory to regulatory immune suppressive cells by virtue of blocking CD38 so it’s really acting as an immune modulator and enhancing the effects of these. I feel that’s probably the reason why we’re seeing this activity.
Those are very high response rates. With both Teclistamab and Talquetamab, the responses are in the 60%, but you’re seeing a higher percentage. Very encouraging. It means that we can potentially use this combination in earlier lines of treatment, even for newly diagnosed patients. It would be really cool to have a non-chemotherapy approach just using antibodies.
CC: Right now, is it still in that triple-class refractory population?
Dr. Usmani: Yes, but there are clinical trials in earlier relapse and even in the newly diagnosed setting being planned. They’re not in the public domain yet, but they’re planned and we are probably going to have these bispecifics examined for newly diagnosed patients.
CC: Yes, that might be something to consider for the high-risk group, which is really still quite an unmet need here in myeloma.
Earlier lines of treatment
CC: There was a trial that was presented that talked about RVd plus or minus Elotuzumab. Was that correct?
Dr. Usmani: Yes, this was an update from the SWOG-1211 trial.
To give you a context about high-risk patients in general, myeloma is a very heterogeneous disease. Biologically, we have eight or nine different subgroups depending on how you classify it on a molecular basis. From a clinical behavior standpoint, the way that we classify myeloma is patients who are at a higher risk of relapsing early after getting front-line treatment compared to those who have standard risk; in those patients, we don’t expect the myeloma to relapse early.
High risk is defined by certain clinical features, such as circulating plasma cells or extramedullary myeloma, or certain stereotypic abnormalities, like translocation for 14, 14;16, 14;20 or deletion 17p as well as amplification of 1q21. The SWOG-1211 was the first clinical trial that I had the privilege of designing and running when I was a junior faculty within the US cooperative group setting focused on high-risk myeloma. If you look at all the clinical trials, all the major studies that have been reported, they take all comers — any myeloma patient can participate. What we recognized as clinicians is high-risk patients don’t do well.
The idea of the SWOG-1211 was [to] design a trial just for high-risk patients and see if we can make a difference for those patients; that was the first effort. The idea was [to give] RVd for induction and then [continue giving] RVd as maintenance — the dual PI/IMiD maintenance strategy. Then in the experimental arm, Elotuzumab was added to that same RVd backbone, both in induction as well as maintenance. It was a randomized phase 2 study and the study did not show a benefit of Elotuzumab adding anything to RVd. However, the trial showed better PFS than our historic control. The median PFS for just the RVd was about 34 months. Our assumption was that the median PFS for those patients would be about 26 months and that assumption was based on patients getting tandem transplant so this was from the total therapy time. The RVd arm actually performed better than the older therapy.
SWOG-1211 set up a benchmark for other high-risk trials to follow. At the ASCO meeting, we heard about a UK study looking at KRd-Dara for high-risk patients. There’s an IFM trial and there’s also a KRd-Isatuximab study from the German myeloma group. These are smaller single-arm studies that are trying to do the same thing — do enrichment design trials for high-risk patients.
I wanted to give the whole context of why that study is important. The results by themselves for SWOG-1211, it’s considered a negative study because Elo (Elotuzumab) didn’t add anything. But then it set up a very important benchmark for other studies to improve upon.
CC: That’s good to know. I really didn’t know that background and I’m glad to hear that more and more studies are just targeting that high-risk myeloma population. It’s so important to figure out how can we control that disease early on in that group of people.
DETERMINATION trial
CC: How about the DETERMINATION trial? I hear so much about it. I still haven’t quite figured out what the results mean. Can you try to clarify that?
Dr. Usmani: It’s very interesting. It’s a positive study. The primary endpoint for this particular trial was showing PFS benefit between doing an early transplant or delaying it at the time of the patient’s first relapse. There is a 21-month benefit in favor of doing [the] transplant early for that young myeloma patient.
The median age [in] this study for patients enrolled was 55 years so this is a young patient population. This is a sister trial to [the] IFM 2009 study that had already been reported out about five years ago.
The depth of response in terms of MRD (minimal residual disease) negativity and sustained MRD negativity appears to be higher in the transplant arm as well. The study has a median follow-up of about 70 months and, at that point, median OS (overall survival) has not been reached in either of the arms.
Some investigators, the way that they’re framing that is incorrect. They’re saying there’s no difference; that’s not how you read the statistics. You don’t say there’s no OS different at a time point when the median OS has not been reached in both arms because there’s not enough follow-up. If that was the case, we would be saying the same thing about the MAIA trial, the ALCYONE trial, the CASSIOPEIA trial… All of those trials had no OS benefit when they were reported out because the median OS had not been reached in those arms.
The new questions should be what about CAR Ts [and] what about bispecifics? We’re designing trials with that question in mind.
Dr. Usmani
The other important thing that we see is there is no difference between the two arms between second primary malignancies as well. The second primary malignancies that people get in one arm over the other are different, but the overall percentage is about 10-odd percent that was reported out. Again, that’s my take on the study. It really doesn’t add any new information. We already knew the IFM 2009 study data.
What it does augment is the use of Len (Lenalidomide) maintenance because the IFM 2009 study stopped maintenance after a year but the DETERMINATION trial continued maintenance for everyone until relapse, progression, or intolerance. The study really doesn’t add a lot more to what we already practice.
I hope that this is the last trial that we’re thinking about early versus late transplant because that is an old question. Now, the new questions should be what about CAR Ts [and] what about bispecifics? We’re designing trials with that question in mind. I think there’s a lot of hype around DETERMINATION but really it’s hype. I don’t think it adds much to what we are doing right now.
CC: Early transplant means transplant is part of your induction therapy. Late transplant means at first relapse. Is that what the trial was talking about?
Dr. Usmani: Yeah. Both arms did pretty good in terms of median PFS. Median PFS if you got [a] transplant was around 68 months. Median PFS if you just got RVd and delay transplant was about 47 months. There was a 21-month difference in favor of early transplants.
The follow-up is short on the study so you’re not going to have a lot of people even in the RVd arm relapsing to get their transplant.
Myeloma patients are doing so well today. The median OS is at least 10-plus years. You can just say after a four or five-year follow-up that we’re seeing OS differences. I’m hoping that by the time we get the DETERMINATION OS data, it’s going to be ten years from now. Because our patients are going to be doing so well that we’re going to be looking at this historic data and saying it was a good question at that time, but probably not relevant to us by the time that reads out.
CC: Exactly. In ten years, who knows what our induction therapy is going to look like? Much better, I’m thinking.
ENDURANCE Trial
CC: What about the ENDURANCE trial? Can you talk a little bit about what that was?
Dr. Usmani: The ENDURANCE trial ran side by side [with] the SWOG-1211 study and it was asking an induction question for standard-risk patients. Is KRd better or RVd better for induction?
ENDURANCE was a randomized phase 3 study. Half of the patients got Carfilzomib with Len-Dex (Lenalidomide-Dexamethasone) as induction. The other half got VRd or Bortezomib with Len-Dex as induction for eight cycles. Then everyone got Len as maintenance.
This study enrolled standard-risk patients because high-risk patients were going on the SWOG-1211. Translocation for 14 patients were enrolled [in] this study as well.
Trial readout [showed] no differences between PFS on either arm of the study. Essentially for standard-risk patients, it established RVd as the right treatment choice just like the SWOG-777 trial had shared with us.
The other interesting thing about the median PFS of RVd on the ENDURANCE trial is the median PFS was around 34 months. Again, the SWOG-1211 with the PI/IMiD maintenance showed the same thing. My colleague, Shaji Kumar, presents this slide saying what makes the difference in high-risk patients is the dual maintenance if you look at the ENDURANCE trial and SWOG-1211 together because both of these were enrolling at the same time.
CC: So dual maintenance is what’s happening now in high risk?
Dr. Usmani: For high-risk patients.
New & exciting studies
CC: Anything else that we should be talking about? Anything else new and exciting?
Dr. Usmani: There are a lot of new trials that are in the works. There’s the CARTITUDE-5 study, which is looking at patients getting RVd as part of induction. These are patients who either are transplant ineligible or they’re deferring their stem cell transplant to first relapse. Everyone gets RVd as part of induction treatment but then half of the patients get randomized to getting CAR T-cell therapy; [the] other half move on to their maintenance treatment. The people who get the CAR T-cell therapy don’t get any maintenance. That’s a really cool study. We’re hoping that it can provide a good answer for those patients.
The second trial is actually looking at transplant-eligible patients. Everyone gets the quadruple regimen of Daratumumab with RVd and then patients get randomized to either a transplant or CAR T-cell therapy. That’s a very exciting study. We’re hoping we can get a positive answer for our patients.
High-dose Melphalan and transplants have been a part of myeloma treatment for a long time but if we can replace them with another cellular therapy approach, which is more specific to the myeloma cells, I would really welcome that.
CC: I would welcome that, too.
CAR T-cell therapy for transplant-ineligible patients
CC: When you talk about transplant-ineligible patients — there’s that group of patients that really are not eligible for transplant for whatever reason — would those group of patients not be eligible for CAR T-cell therapy or would they be possibly eligible? I know you have to look at them individually, but as a group, is it just like you’re not eligible for this or you’re not eligible for that?
Dr. Usmani: We are a little bit more lenient in CAR T-cell therapy eligibility compared with stem cell transplantation because patients are not getting the same level of myelosuppression with high-dose chemotherapy like a stem cell transplant. There might be patients who are in their mid-70s or even late 70s who are able to get CAR T-cell therapy that we would not necessarily pick for transplantation. We’re thinking about CAR T-cell therapy in a more lenient way because of the safety profile.
CC: That’s good to hear. It’s just amazing all these new therapies. When I was diagnosed back in 2008, most of the things we talked about weren’t FDA-approved except Revlimid and Velcade.
Words of wisdom
CC: When you see a newly diagnosed patient or even an older patient who may be relapsed/refractory, how do you provide them with hope with all these new treatments? What are your words of wisdom to these patients?
Dr. Usmani: I give them the context. I tell them about the time when I was starting in the field in the early 2000s and how the outcomes were for myeloma patients. I walk them through how things have improved, what our goals and expectations are today for our patients, and the treatment options we have. I provide them with measured hope.
We do recognize that myeloma is still not a disease that we can cure, but we can control it for a long duration of time. Even for patients who have high-risk myeloma, we’re thinking about things in a different way and trying to be proactive in giving different strategies for those patients rather than just treating them in a vanilla, one-size-fits-all way. I provide that context to patients and then it’s really about individualizing treatments based on patient preference as well. This is really a partnership. Our job is to provide patients with as much information as they can gather to make good, informed decisions.
I give them the context. I provide them with measured hope. We do recognize that myeloma is still not a disease that we can cure, but we can control it for a long duration of time.
Dr. Usmani
What will cure myeloma?
CC: Good. Now, you did mention the word cure. Do you think we’ll be curing any myeloma patients any time in the future? What do you think that would look like?
Dr. Usmani: I would say, yes. This is something that I’ve shared on other forums as well. If we’re able to get patients to MRD negativity and maintain them in that negativity for a certain period of time and then stop therapy at that time, then we can functionally cure [a] majority of patients.
Myeloma is a disease that tends to occur later in life. There are other competing health issues that patients have so a true cure cannot be determined in that situation compared to someone who was 20, got diagnosed with cancer, and dies of a heart attack at 90. You can say this person was cured [of] cancer. You can’t say that about a myeloma patient who’s getting diagnosed in their sixth or seventh decade of life.
If you can kick myeloma down to undetectable levels, start treatment, and patients continue to thrive for years and cancer doesn’t come back, in my mind, that’s functional cure.
My answer is yes, we’re going to get our patients there. The key would be finding the right recipe to get patients to that sustained MRD negativity before stopping.
CC: Right, and now we have so many ingredients for that recipe that I’m sure we’re going to find it soon.
It’s really about individualizing treatments based on patient preference as well. This is really a partnership. Our job is to provide patients with as much information as they can gather to make good, informed decisions.
Dr. Usmani