Kelly’s Osteosarcoma (Bone Cancer) Story: How a College Cheerleader Faced a Life-Changing Diagnosis
Kelly was in the midst of college life in March 2025, balancing her studies with the rhythm of cheerleading practices, when her world shifted with a diagnosis of bone cancer (osteosarcoma). What started as lingering soreness and knee pain that seemed like overexertion gradually progressed to swelling and persistent discomfort. An MRI ordered by her doctor revealed a tumor, and her daily routine changed from cheer workouts to clinical tests and questions about what would come next.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez & Jeff Forslund
Kelly’s emotional landscape transformed with her diagnosis. She initially struggled to grasp the gravity, believing that osteosarcoma (a kind of sarcoma that usually affects the long bones of the legs or arms) wasn’t cancer, before her oncologist explained the reality of chemotherapy, hair loss, and surgery. Overwhelmed by fear and loss of control, Kelly paused her studies and cherished plans, including college cheer nationals and studying abroad. This pivot fueled a deeper introspection and the gradual acceptance of her cancer patient identity; she found hope through setting new goals, supported by a determined effort to walk, travel, and participate in local events, wherever possible.

Communication became central as Kelly shared her news with loved ones and teammates. She navigated support systems within her sorority and friend group, ultimately choosing vulnerability, including posting openly on Instagram to empower others and remove stigma. Her surgical experience, especially limb-sparing or limb salvage surgery, required profound mental preparation, trust in her care team, and courage to meet postoperative challenges. Kelly describes physical therapy as intensely difficult, yet rewarding; her first full steps post-surgery marked a turning point in rebuilding confidence.
Fertility preservation emerged as another major decision, with the help of a supportive oncology nurse. The experience gave Kelly confidence and certainty in an uncertain period, easing subsequent encounters with medical treatment. Throughout her experience, she faced emotional and physical changes, including issues with self-image arising from chemotherapy-related hair and eyebrow loss. She pivoted those moments into advocacy, supporting others diagnosed with sarcoma and participating in awareness events.
Kelly’s experience highlights complexity, courage, and communal strength, culminating in her heartfelt message: “Everything will be okay and things will work out.” Watch her video and read through the edited transcript of her interview for more on how:
- Listening to your body and advocating for medical answers is crucial
- Emotional support from friends, family, and care teams can reshape a difficult experience
- Adapting to unexpected changes fosters strength even in vulnerable moments
- Transformation happens when patients pursue proactive goals and self-care even after setbacks
- The experience of cancer doesn’t define worth or identity. It reveals new sources of strength.
- Name: Kelly M.
- Diagnosis:
- Bone sarcoma (osteosarcoma) of the left femur
- Age at Diagnosis:
- 18
- Symptoms:
- Persistent soreness and knee pain
- Visible knee and leg swelling
- Treatments:
- Surgery: limb salvage surgery
- Chemotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Hi, my name is Kelly
- When my first symptoms started
- The emotional impact of my diagnosis, and how I dealt with it
- How I told my teammates and friends
- Preparing for limb-sparing surgery
- I had physical therapy after surgery
- What it’s like to do an egg retrieval when you’re 18
- My biggest challenge and how cancer changed my perspective
- What I learned about myself
- Becoming an advocate and supporting others
- What I want people to know
Hi, my name is Kelly
I was diagnosed with osteosarcoma in March 2025. I’m from New York.
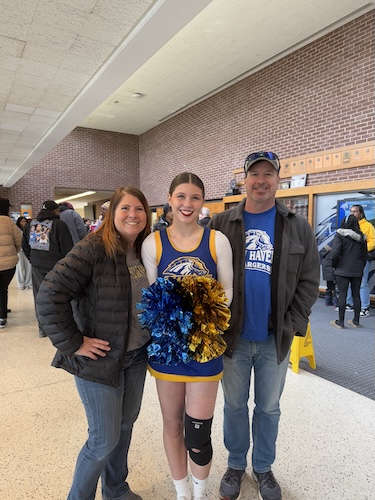
I’ve been cheerleading since I was five years old. I’ve always been active in any way I can. When I wasn’t cheerleading, you could find me running or at the gym. I was very into running 5Ks since my parents would run together. They actually ran marathons together. So, it’s kind of in my genes to be active. I’ve always been very involved in school, whether through sports or clubs.
When I was younger, I tried different sports, but cheer was the only one that stuck. I cheered throughout elementary, middle, and high school, and in my first year of college, I was on the cheer team as well.
A lot of my self-determination comes from cheerleading and tumbling, especially by pushing myself to get new skills. The joy of landing a new skill for the first time is unmatched. It’s such a rush of excitement, knowing you’re the only one who can do that because you pushed yourself. You decide if you can or cannot do something. Landing new skills always kept me motivated.
When my first symptoms started
On top of cheerleading practice, which I had twice a week in college, I would also go to the gym three times a week. After a leg workout, I stayed sore for days and noticed my knee felt a little off. I thought I’d gone too hard that day and should take it easy.
Weeks passed, and I still had on-and-off pain, especially while lying in bed. I could not find a comfortable position on the train home from school for my knee. I thought maybe I was just really sore from doing a lot.
I kept cheering for months. By December, I decided to see a doctor since the pain hadn’t gone away for over a month, and I was starting to limp. My mom said, “You need to go to the doctor; this is not normal.” The orthopedic doctor did an X-ray and concluded I was overworking my knee, prescribed physical therapy, and thought it was nothing serious. I was happy; it was supposedly not a real problem.
I iced my knee, put tape on it, and wore a brace, but nothing helped. At my first appointment, a follow-up for spring break was scheduled. After an amazing Florida vacation, I returned for my follow-up, still thinking nothing serious was wrong. My parents were at work, so I went alone. The doctor saw that my knee was visibly swollen, not dramatic but noticeable. He said, “It should have healed by now. Let’s do an MRI today.” I had no idea what an MRI was, but said “okay.”
After the MRI, I went on with my day. About an hour later, the doctor called, earlier than expected, and said, “We think there’s a tumor.” I was alone, 18 years old, and I freaked out. In my mind, tumor equaled cancer. They dropped the bomb with no further information. I called my dad: “This is what they told me. I don’t know what to do.” He said, “Come home, we’ll talk about it.”
From there, it was test after test. I had a biopsy within days since they needed to figure out what it was. Less than a week after the MRI, I was diagnosed with osteosarcoma.
The emotional impact of my diagnosis, and how I dealt with it
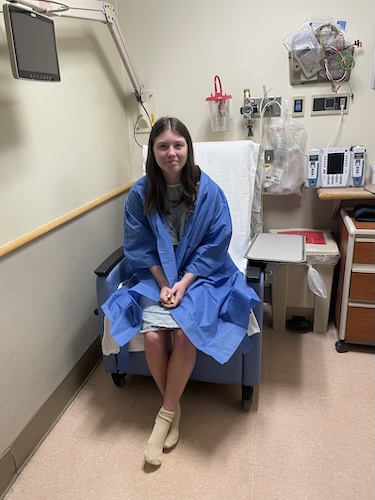
After the MRI, I went back to school for two days. The plan was to come home, have my biopsy, then go back. I had never had a procedure or anesthesia before, so I was worried about the procedure itself, not realizing I should fear the results more.
After the biopsy, my parents got the call and spoke privately, then said, “We’re going to the hospital for a talk with your new oncologist tomorrow.” I clung to hope. At the oncologist’s office, she laid everything out. When she told me it was osteosarcoma, I thought, “Oh, that’s not cancer.” That’s a huge problem; I’m passionate now about making others aware of what this is. No one has heard of osteosarcoma unless it’s part of your life.
Initially, I thought, “It’s just osteosarcoma, not cancer,” until she explained chemo, hair loss, surgery, everything I’d go through. It finally hit: I am a cancer patient.
I didn’t go back to school that semester. I missed huge plans to study abroad and college cheer nationals; everything felt taken away. My life plans felt completely discarded. That loss of control was very scary for me.
A lot of people told me, “Everything happens for a reason.” I’m making new plans: to study abroad this summer for my major, and likely not continuing with cheer when I go back. Maybe this is the universe’s way, since I’d never have stopped cheering on my own. I try to stay positive; it’s really hard sometimes, but my treatment plan gives me motivation to move forward. Tomorrow, I’m being admitted for my second-to-last chemo. Having things to look forward to keeps me going, like study abroad opportunities and concert tickets
I try to incorporate fun when possible. My doctors call me crazy because I’ll get discharged and the same day go to Pickle Fest. When I’m feeling good, I make the most of it, especially now that I’m walking much better after surgery.
How I told my teammates and friends
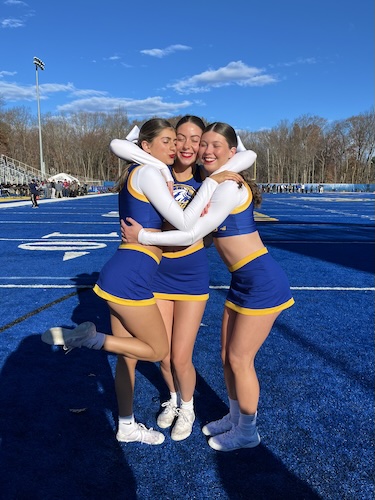
For cheer, we practiced Tuesdays and Thursdays. Home for my biopsy, I told teammates, “I won’t make practice; I just had my biopsy.” I didn’t know my diagnosis yet, so I thought I’d be back soon. Then, after everything started happening, I had to send another message: “This is what’s really going on. I’m so sorry, but I won’t be back this semester.”
I also told my sorority sisters, who were incredibly supportive. They made Zoom options for me to join the chapter meetings, inventing ways to keep me involved. For my closest friends, I shared updates step by step. My roommate, one of my closest friends, got the news about the tumor, then comforted me after I found out I needed surgery.
It was hardest telling acquaintances, people who’d just ask “How’s school?” How do you just say, “I have cancer now”? Two months after diagnosis, I posted on Instagram. Once I felt peace with my plan, I wanted to put it out there, not hide or feel embarrassed. It just happened to me, not because I did something wrong.
Preparing for limb-sparing surgery
I found out about surgery the same week as my biopsy. I had four procedures in March: biopsy, port placement, egg retrieval, and a second biopsy for a lymph node. By then, I’d gotten used to anesthesia. I’d tell myself, “Getting the IV is the hardest part; the rest I’ll sleep through, then wake up okay.”
It was strange going into surgery, knowing I wouldn’t walk afterward, and would have to work to regain weight-bearing on my leg. When I had free time, I felt pressure to use my leg while I still could.
I had immense trust in my doctors, especially my surgeon, who’d been with me the whole process. What scared me was the pain after surgery and how my leg would feel; I didn’t know what to expect.
My surgery was a huge success. In the recovery room, my surgeon told me, “It’s gone. The tumor is gone.” I was on cloud nine; I was so happy and proud to have gotten through something so big.
I had physical therapy after surgery
Recovery was a long, difficult process. I had to do PT while on chemo, walking with a walker while trying to make progress, then feeling set back during inpatient chemo days in a hospital bed. Sometimes it seemed impossible to progress while balancing chemo.
One of my favorite PT moments was in September when I got cleared to fully weight-bear and took my first steps in three months, holding my surgeon’s hand. I realized how hard recovery is, but proving I could do it made me feel capable of anything.
There was a tough period over the summer when my surgeon wasn’t happy with my progress in knee flexion, and I broke down, feeling I wasn’t doing enough despite working so hard with chemo on top.
What it’s like to do an egg retrieval when you’re 18
The day after I was diagnosed, I had a fertility consult because chemo brought a risk of infertility. I had just done a biopsy; I didn’t want another hard thing, and I’m terrified of needles. But I thought, “Future me will want this chance to have children.”
So, I chose to go through with it, and my family friend Jen, a former oncology nurse, helped every night with injections and supported me mentally. She was like my therapist, prepping me for what chemo would be like.
Every morning and evening, Jen did injections. My trigger shot was very time-sensitive, and she was there at 12:30 a.m. The procedure itself was remarkably quick, just 15 minutes.
Knowing I have healthy eggs ready to be used if needed gave me certainty in an uncertain time. It made me so much stronger, and after that, bloodwork and IVs were much easier for me.
My biggest challenge and how cancer changed my perspective
The hardest part was seeing other people live the life I wanted, like friends studying abroad and having fun, while I was stuck in a hospital bed. It makes you wonder if you did something to deserve it, but there’s no answer. Osteosarcoma doesn’t have a known cause; genetic testing showed no genetic link.
It felt like I was being punished for something I didn’t cause, working so much harder than my peers just to return to school.
I am much more independent, and everything is now in perspective. I want to live my life and never take anything for granted. Sometimes I think, “I wish delayed flights or hard assignments were my biggest problem.”
I don’t want to say no to any opportunities anymore. I want to do everything while I’m healthy.
What I learned about myself
I am way stronger than I thought. I always considered myself physically strong through cheer, but mentally, I now know I can handle anything thrown my way.
It encourages me through hard assignments. If I got through cancer, I can get through anything.
I have more emotional confidence, but I also face identity issues stemming from my experience.
People ask if I’m excited for my hair to grow back, but I’m more excited for my eyebrows and eyelashes. Your face changes after chemo, and losing my eyebrows made me not recognize myself, especially when my iPhone’s FaceID stopped working for me.
I never had confidence issues before, but now I do, because of things I can’t control. Wearing my wig helps a little, but my face still looks different, and people say it’s temporary, but I don’t like how I look. I used to think I was beautiful, but now I don’t recognize myself, and it hurts.
Sometimes I’ll ask my dad to go to the store instead; I don’t want to be seen. Watching old videos makes me sad for my younger self, who didn’t deserve this.
Becoming an advocate and supporting others
Although I never wanted this, it gave me a chance to advocate for sarcoma awareness, which I’m now passionate about.
Recently, a girl who saw my story reached out, saying she’d just been diagnosed and my story gave her hope. It amazed me to have such an impact, to be the person I wished I had when first diagnosed.
Connecting with her and learning that we have nearly identical chemo drugs and experiences was refreshing. I’ve met many through cancer, but never someone so similar.
As an advocate for sarcoma awareness, I joined the Sarcoma Foundation of America’s Race to Cure Sarcoma in October. I set a goal to walk a mile with no crutches, even though I’d relied on crutches for months.
I achieved that with my family, close friends, boyfriend, and their parents supporting me. It was one of my favorite experiences, proving I can reach my goals and showing how much progress I’ve made.
What I want people to know
Everything is going to be okay.
When I started chemo, I couldn’t imagine reaching the end. 17 more rounds felt impossible, but now I’m almost there. I did it.
I want everyone to know everything will be okay and things will work out.

Inspired by Kelly's story?
Share your story, too!
More Sarcoma Stories
Ashley W., Desmoid Tumor
Symptoms: Leg tightness, increased swelling in leg
Treatments: Chemotherapy infusion (Methotrexate, Navelbene), oral chemotherapy (Nexovar)
...
Demi D., Desmoid Tumor
Symptoms: Fatigue, lump in hip
Treatments: Surgery, radiation, chemotherapy
...
Alicia B., Desmoid Tumor, Stage 4
Symptom: Lump in right armpit
Treatments: Chemotherapy, radiation, targeted therapy, clinical trials, surgery, including forequarter amputation
...
Ariane B., Ewing Sarcoma (Bone)
Symptoms: Aching in arm, lump in forearm
Treatments: Chemotherapy (14 rounds), surgery (of radius), radiation (36 sessions)
...
Brandi B., Ewing Sarcoma (Soft Tissue), Stage 1B
Symptoms: Extreme fatigue, lump in pelvic area
Treatments: 17 cycles of chemotherapy in-patient at hospital with (leg-sparing) surgery in between
...
Sophie F., Ewing Sarcoma (Soft Tissue), Stage 2
Symptoms: Appearance of a nickel-sized, blue, and solid but soft and spongy mark on upper left arm
Treatments: Surgeries (cyst excision surgery, wide excision surgery), chemotherapy
...
Louis D., Gastrointestinal Stromal Tumor (GIST)
Symptom: Feeling the need for constant urination
Treatments: Surgery to take out the tumor, maintenance chemotherapy (3 years)
...
Kara L., Synovial Sarcoma, Stage 1B
Symptoms: Pain behind left knee, needle-like sensation in left foot
Treatments: Surgery to remove what was thought to be benign tumor, chemotherapy, final surgery, radiation (36 sessions)
...
Jillian J., Synovial Sarcoma, Stage 3
Symptom: Pain in leg for over 15 years
Treatments: Surgeries (tumor resection, thoracotomy)
...
Marisa C., Synovial Sarcoma, Stage 4
Symptom: Small bump on the foot (stable for years, then grew during pregnancy), pain when pressed
Treatments: Surgeries (below-knee amputation, pulmonary wedge resections, segmentectomy), chemotherapy, radiation (lungs & hip)
...
Julie K., High-Grade Poorly Differentiated Spindle Cell Synovial Sarcoma, Stage 4
Symptoms: Chest and back pain after car accident, trouble breathing
Treatments: Chemotherapy, surgeries (lung resection, video-assisted thoracoscopic surgery or VATS, neurectomy, rib removal), radiation therapy (CyberKnife)
...
McKenna A., Synovial Sarcoma, Stage 3 Grade 3B
Symptoms: Insomnia, weak immune system resulting in persistent illnesses such as UTIs and strep throat, severe swelling in left leg
Treatments: Surgery (tumor excision), chemotherapy, radiation therapy (proton radiation), integrative therapies
...
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Symptoms: Tightness and lump in left breast
Treatments: Chemotherapy, radiation, surgery
Nicole B., Undifferentiated Pleomorphic Sarcoma, Stage 3
Symptoms: Severe intolerance to food, nausea
Treatments: Surgeries (cholecystectomy, Whipple), chemotherapy (Gemcitabine and Taxotere)