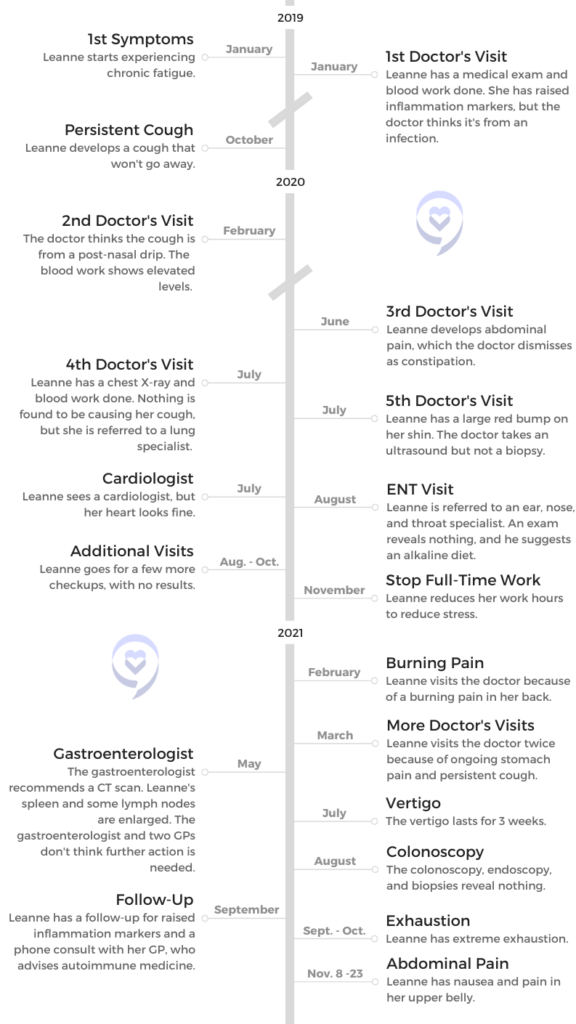
Leanne’s Stage 3B Non-Hodgkin’s Lymphoma Story
Follicular Lymphoma Transformed to Diffuse Large B-Cell Lymphoma (DLBCL)
Leanne had a high-stress career with long hours when she started feeling fatigued all the time. After a cough and abdominal pain led to a series of doctor’s visits, she was eventually diagnosed with non-Hodgkin’s lymphoma.
Leanne shares struggling to get a diagnosis for two years, processing the shocking diagnosis, and going through R-CHOP chemotherapy.
The experience rocked her world, and she also discusses how it changed her mindset, how it affected her friends and family, and how she manages anxiety.
This is an opportunity to take stock of your life and actually think about what do I want to keep in my life, and what things do I need to let go of?

- Name: Leanne T.
- Diagnosis (DX):
- Non-Hodgkin’s lymphoma
- Diffuse large B-cell lymphoma
- Stage 3B
- 1st Symptoms:
- Fatigue
- Persistent cough
- Abdominal pain
- Age at DX: 60
- Tests for DX:
- Blood work
- X-ray
- Ultrasound
- CT scan
- Laparoscopic biopsy
- Treatment:
- Chemotherapy
- R-CHOP
- 6 rounds
- Infusions every 3 weeks
- Chemotherapy
This interview has been edited for clarity. This is not medical advice. Please consult your healthcare provider for treatment decisions.
- Pre-Diagnosis
- 1st Symptoms
- Diagnosis
- Treatment
- Processing a Cancer Diagnosis
- Effect of cancer diagnosis on friends
- Importance of mental health
- What change in your life do you think needed to happen?
- Pushing yourself too far
- Time for making changes
- What helped with the stress of diagnosis and treatment?
- Seeing a psychologist
- Rethinking relationships with others
- What emotions were you feeling?
- Researching and asking questions
- Giving it a red hot go
- How cancer affected family
- Reflections
Pre-Diagnosis
Introduction to Leanne
I’m a person that loves being with other people. I’m an extrovert by nature, and all my life I’ve loved connecting with other people.


I’m probably not as quiet in terms of my leadership anymore, but definitely that’s been the theme of my life. I’ve fit in wherever I’ve gone. It’s just been one of those things where I’m one of those connectors of people.
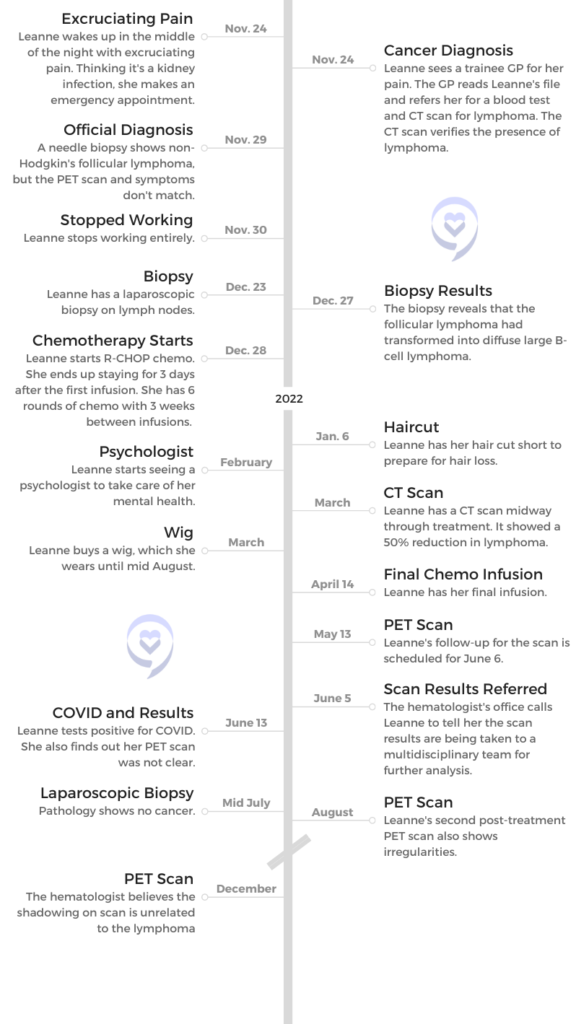
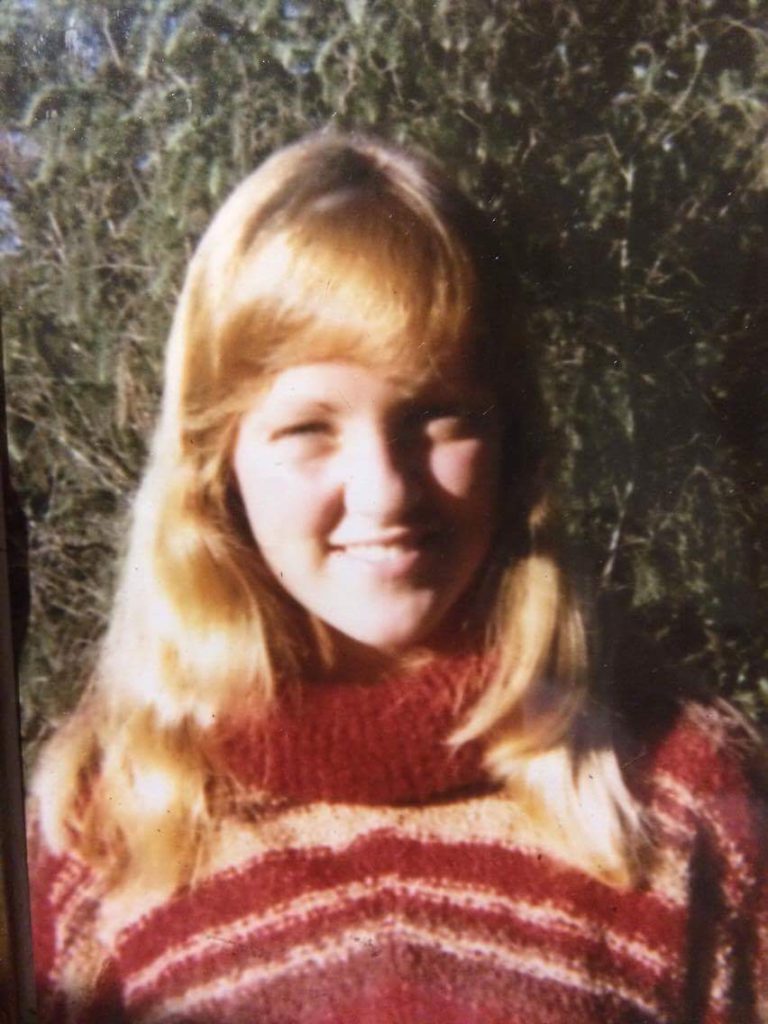
First and foremost, I’m a mother. I’ve got two adult children — one that’s 33 and one’s 31 — and I’m a grandmother for the first time. My first grandchild was only born in February last year, so she’s almost one.
I guess the theme of my life, too, has been one where I’ve been a high achiever. I’ve got several university degrees. I have a curious, inquiring mind and love to learn.
I’m a creative thinker. I’m one of those people that if there’s issues or problems to be solved, I’ll always come up with creative ideas and solutions. I’ve used that throughout my career, where I’ve been able to bring innovative ideas and ways of doing things into workplaces.

Leanne’s life now
I’m now 61. No longer working since I had the diagnosis, but still living a rich life, not worried about not working anymore, which is a curious thing given it’s been a theme of my life.
For a lot of my time raising the children, I was a single mother. That was a juggling act, bringing both the ambition for my career and my ambition for a good, quality life and a good life for my two kids.

But I’m pretty proud in the way that they’ve come together as human beings. They’re two very highly functioning adults, and both with their own great lives and careers, wonderful partners, and having a fabulous life for both of them. All in all, I’m very happy with the life that I’m having and have had.
I live in Australia. I live in a coastal town two hours just south of Sydney on the east coast of New South Wales.
1st Symptoms
Feeling fatigued
This was back in early 2019. I was working at that point for an aged care organization and was commissioning a very high-value new community and aged care home. I developed a new model of care and had traveled around Europe and Australia, looking at best practice to come up with models that I felt were right for this particular site.



The spend was over $300 million on the site, so a lot was riding on it. I just felt incredibly tired because it was a full-on demanding kind of a role. I went to the doctor and just said I’m feeling really tired and not sure whether it’s menopause. I’m 61 now. I would have been in my late 50s then.
They ran blood tests, and at that stage the results came back. Things were pretty normal except for my inflammation markers, which were raised. At the time, it was explained away by saying, “Oh, you must have been fighting off an infection, or something was going on.”



So I just accepted that, but made a decision to change jobs because I thought I’ve now commissioned the community, the home. It’s been now operating for a couple of years. I feel like I can step away. While I love that job, it’s turned into a toxic kind of a love, and I need to look after myself. I took on another leadership role in another sector.
My nature is to throw myself into things, so even though I was feeling tired, I plugged away again, trying to achieve, I guess.
Developing a cough
My son lives in London. I hadn’t seen him for 18 months, so [in October 2019] I went over to the UK and Europe for a three-week flying holiday.
We went to the north of Italy. While we were traveling around there, I caught the flu and just couldn’t shake it. On the way home, I coughed.



When I got home, I thought, “I’ll get over this cough. It’ll eventually heal.” Then that summer (our December, January, February) was a really bad time environmentally for Australia, and all around where I live were dreadful bushfires. The air quality was quite bad.
It’s very easy to explain away this cough, thinking, “There’s a lot of smoke and soot in the air, and this cough is being aggravated by that.” It seemed to be worse at night. In February of that year, I thought, “This is really getting me down,” and I went to the doctor, the GP, and said, “I think I need an X-ray. There’s something wrong with my lungs or something because I cannot stop coughing.”



At that point, she said to me, “I think it might be post-nasal drip. Here’s some things. This stuff to spray up your nostrils. That’ll solve the problem.” Anyway, I tried that. Nothing, Nothing.
Then I went back, and it was March 2020. COVID had hit, and she said to me, “We can’t send you over for X-rays because all of the radiology is being kept for patients with COVID, and you don’t want to be in that environment.” I kept coughing away, thinking this will resolve.
Then it wasn’t until about June that the situation with the radiology eased up enough where I could go and have a lung X-ray. At that point, the X-rays were clear. There was nothing wrong with my lungs.
»MORE: Read more patient experiences with first symptoms of lymphoma



Seeing an ENT, cardiologist, and lung specialist
I was sent off then on a round of visits with specialists. I went to an ear, nose, and throat specialist, looking for this post-nasal drip problem. They put a camera down my nose into my throat. He said to me, “I can’t see anything wrong with your ear, nose, and throat. Your throat is inflamed.” And obviously it was, because I’d been coughing for months.
He said, “I think it’d be worth trying an alkaline diet,” which basically is like a vegan diet, so that’s what I was doing, and avoiding dairy and meat and so on, and just very much a plant-based diet.



Then there was a question, like maybe there’s something wrong with your heart. I had an appointment to see a cardiologist, who wanted me to have an ultrasound of my heart before I went. So I did that, went and saw him. That was all perfectly normal.
Might I say, each time I saw these specialists, you’re looking at — I know the health system’s different in Australia — like 400 AUD, which is more than 500 USD, each time I went. That’s not claimable on my health insurance. It’s just part of the picture of feeling desperate, thinking I’ve got to find the solution.
After that, I then later in the year saw the lung specialist, who said to me, “No, I don’t think there’s anything wrong with your lungs either.”



Back pain and gastroenterologist
On I plugged, and then we’re now in February 2021. I’d gone away to Canberra for my girlfriend’s 60th. While I was staying away, I had this incredible burning sensation in the flank of my back and just couldn’t get comfortable in bed. I thought, “Gosh, I’ve pulled a muscle. There’s something weird going on here.”
I went to the physiotherapist, thinking it was a pulled muscle. That didn’t help. In the end, I went to the doctor again, who said, “This is very unusual,” and again thought it might be reflux or something. Why would that be a burning sensation?
[The doctor] sent me off to the gastroenterologist. The previous year I’d had some weird pains in my stomach, and the doctor said, “Maybe you’re constipated.” I knew I wasn’t. There’s always sort of trying to explain things away.



I went to the gastroenterologist, and she said to me — this is in May of 2021 — “I’d like to get a CT scan of your abdomen, and we’ll get an idea of what’s going on. Once you’ve done that, we’ll get you to do an endoscopy and a colonoscopy, so we’ll know from an internal perspective.”
The results of the CT scan came back, and when I looked at the report myself, I said to [the GP], “Why does it say my spleen is enlarged and some of my lymph nodes are enlarged?” Again, it was explained away. “Oh, you probably just had some sort of infection.” That’s at the point where it should have been picked up.
Now [for] the gastroenterologist, [the] endoscopy, colonoscopy, [and] everything was normal as well. They took biopsies. Everything was deemed to be normal.



Excruciating pain
It was now getting to be about July [or] August of 2021, and I was feeling really tired. I stopped working in that new job that I had in October 2020. That was full time. That was a CEO’s job.
I decided to take a little break just to sort of recharge. Then I picked up consulting work and was working maybe three days a week. By July of 2021, I thought to myself, “I’m still really tired. I’m going to cut back and just keep one client,” rather than the couple that I was doing some work with.


Anyway, it was in November of 2021. I woke up in the middle of the night with excruciating back pain. I thought to myself at that stage — still coughing, by the way — “Gosh, I must have a kidney infection.”
The pain was so bad I could have rung an ambulance, but I didn’t want to end up in hospital. So I thought, “I’ll just hang in there.” [At] like 8:00 in the morning here, if you want to get in to see a doctor, they leave some spaces open for last-minute emergency.
So I rang up, and I said, “I need to see a doctor immediately. I don’t care which doctor I see,” because normally I was seeing one doctor. “I’ll just see anyone. I think I’ve got a kidney infection. I need medication.” They fitted me in with a trainee GP who I’d never met before, but I was desperate.



Diagnosis
Seeing the GP trainee
This is all through the pandemic. I walked into the doctor’s surgery with my mask on, went into her rooms, and she started talking to me. I began to cough, and she said, “You shouldn’t be here. You might have COVID.”
And then I burst into tears and said, “I haven’t got COVID. I’ve been coughing like this for two years.” She went, “Oh.” Anyway, she got me to go away and do the urine test to check for my kidneys. While I was away, she got into my files and started reading the reports from all of these tests that I’d been having done.



I’d had the X-rays on my lungs, I’d had the ultrasound on my heart, I’d had the CT scan of my abdomen, and in between that, I’d had some other weird symptoms.
I had a lump on my shin, and so I’d had ultrasounds on that, which was sort of a raised red lump and which possibly was a lymph node or something. But no one did a biopsy on that.
When I came back and she tested my urine, she said, “No, there’s nothing wrong with your kidneys, but I think there’s something quite seriously wrong that I can see from your results. While you’ve been gone, I’ve booked you in for another CT scan this afternoon, and I need you to do some blood tests before you leave.”
She said, “I’ll have the results back tomorrow morning, and we’ll be in touch. Make sure you get that done today.” So off I went. I did those things, thinking, “Oh my gosh, what is going on?”



The diagnosis
The next morning at 8:00 in the morning, I got a phone call from the doctor’s surgery, saying, “Doctor would like to see you later today, and you’ll need to bring someone with you.”
I was panicking, and my appointment wasn’t until 5:30 that afternoon. I went, and I had my partner with me. She was the most delightful person. If there was somebody to break news like that, just really empathetic and kind. I sat there and thought, “I cannot believe this.”
Processing the diagnosis
This is in November 2021. In April of 2021, I turned 60, and thankfully I had a big 60th birthday party. At my party when I was giving the speech, I’m saying to everyone, “This is a milestone birthday, turning 60. I’m two-thirds of the way through my life.”





Because all my relatives that I tend to take after all lived into their late 90s, I really felt strongly that’s going to be me. So I’m saying, “Right, we’ve got another third of my life. I’m so excited to see what that third is like, and I’m so glad you’re all with me. Let’s go on this new journey for the final third of my life.”
One of my passions in my career was working in aged care and looking at how people lived in older life and living well. It’s all about having purposeful days and feeling really good about getting older, but feeling like you’re active and doing what you can with your life.



Having seen all of that and [having] worked with a lot of older people, I thought, “That’s going to be me. I’m going to be really active, live a long life, and really give back in a whole range of different ways.”
When I found out I had cancer and it looked like lymphoma, I was thrown. It was such a shock, terrible shock. We came home. We sat out on the balcony, and I just thought, “I just can’t get my head around this.”
Seeing the hematologist
She had rung the head hematologist for the region that I live in and made an appointment for me on the following Tuesday. When we went and saw him, he was absolutely delightful and reassuring. He said to me, “I have a feeling, based on your symptoms.” Prior to that time with the pain in the back, I’d started having night sweats.
He said, “I think you might have diffuse large B-cell non-Hodgkin’s lymphoma. We need to do some tests to find out for sure.” He said the next step is to go and have a needle biopsy, which I did. With those sorts of biopsies, you’ve got to wait seven days for the pathology to come through to confirm what the cells have told.



I went to that next meeting by myself because it was in early December by this stage. I was on a board of directors, and there was a Christmas party on at lunchtime. My appointment was at 10:00. I thought, “I’ll go to the appointment and then head on over to the Christmas party.”
I live 40 minutes away from the hospital where the hematologist was. Because I was so overwhelmed and stressed by the diagnosis, I was driving on the highway and had an anxiety attack in the car. So I’m driving and thinking, “I’ve just got to keep breathing.”
This is May. A person who used to be able to cope with absolutely anything — standing up in front of a crowd and I could chat, wing my behavior through things that I wasn’t really sure about, just totally competent — having an anxiety attack on the highway.



Calming down from anxiety
Somehow I got my car into the multi-story car park. I made my way up to the seventh floor, where the hematologist was. I’m sitting in the waiting room waiting to see him, thinking, “Breathe, breathe.”
Just to distract myself, I got my phone out, and I started looking at social media. The night before, I’d seen a fellow who’d worked for me 15 years ago that had just graduated from university, his first degree.
I’d written a little comment saying, “I’m so pleased and proud that you’ve been able to achieve this. Congratulations.” And then there was a private message. So I’m sitting in the waiting room, just had the anxiety attack, and there’s this message from this fellow.


I read it, and it said, “Leanne, if it wasn’t for you, I wouldn’t have done this study. You encouraged me every step of the way, and I plugged away as a mature-aged student, and here I am. I’ve got my degree. I’m now in a senior management role, and you are my role model.”
I’m reading this, thinking, “Aw.” He said, “Whenever there’s something tough that happens, I always think to myself, ‘How would Leanne handle this?’ And that’s how I do it.”
At that point, I thought, “I’ve touched someone’s life. That’s so important to me.” Anyway, I wrote to him that night. I said, “You don’t know how important that message was to me.” I went into my appointment. I’d calmed down by that stage.
The hematologist said, “Unfortunately, the results were inconclusive from your needle biopsy. It looks like you’ve got follicular lymphoma, but the symptoms you have don’t match up. We need to do another biopsy. This time it’ll need to be surgically done so we get a larger sample.”



Strategies for dealing with anxiety
Anyway, at that point, I thought, “Whatever.” I was so anxious and overwhelmed by the thought this cancer is running rampant in my body, and nothing’s happening. Weeks are going by. I was so anxious.
That’s something that not many people talk about. I really felt like I was losing my mind, to be honest. For a person that was so normally together and could handle anything, it shocked me to no end. I actually went back to that trainee GP, and I said, “I’m so worried about myself.”
Because she was a trainee, she had plenty of time to talk to me. She explained to me that when you have a diagnosis like this, you go into stress overload. The symptoms that I’d been experiencing — not being able to sleep and having huge anxiety and those attacks like I had in the car — were completely normal.



When I heard that, I thought, “That makes me feel a bit better. It’s not going to be like this forever.”
But she said to me, “Let’s look at some strategies.” One of the strategies was whenever I go for a medical appointment, I’m not to drive myself because that’s just a recipe for disaster.
Also, she did prescribe some sleeping pills and said, “Just take those for a couple of nights,” because I just needed some sleep to be able to cope. She also prescribed Valium and said to me, “This is highly addictive, so be very careful with it.”
Just knowing I had it there as a crutch if I needed it was really all I needed. I did take a few, but they were the days when I started treatment because that was pretty full-on. That was such a help.
Recovering during Christmas
Then on the 23rd of December, so two days before Christmas, I had to go in and have the laparoscopic surgical biopsy. Trying to find a surgeon just before Christmas was really problematic.
Fortunately, a beautiful surgeon made time for me on that afternoon of the 23rd, but then I had to wait over Christmas for the results of that with a very sore stomach.
Christmas normally every year is at my place, and the extended family come. That year, because I was feeling so anxious and stressed with a very sore stomach, I was here. Family stayed, but I didn’t do anything.
The practice was in the past that I did everything and made Christmas beautiful for everybody else. It’s been a big lesson for me being able to step back and let others do rather than me doing for everybody else.
Treatment
Starting treatment
On the 27th, the hematologist rang me up and said, “Right, we’ve got the results back. It looks like you’ve had follicular lymphoma that’s now transformed to diffuse large B-cell, so non-Hodgkin’s lymphoma. We’re going to start treatment tomorrow.”
[For] the cancer clinic, we can normally go as an outpatient during the day. That was closed down between Christmas and New Year. “We’ve got to get you started straight away. I found you a bed in our oncology ward in the public hospital.”
In Australia we’ve got public hospitals, where everything is provided free of charge, or you’ve got the private. I’m fully privately insured, but the hospital closes down over Christmas to New Year.
In I went to the public hospital in a shared ward. The only bed that was available was in the palliative geriatric oncology room. So there I was, looking at my future with these old people at the end of their lives. That completely upset me.
Being argumentative at the hospital
It’s funny how I’m normally a very upbeat, glass is half full kind of person, but when I was in there, I was argumentative [and] extremely unhappy. Every time they wanted to take blood tests, I’d argue.
Before all of this, the hematologist had wanted me to have a gated pool test on your heart to check on the functioning of your heart before you start any sort of chemo treatment.
I’d gone in to have that test. Two of the radiologists had tried to find a vein to do the injection of the dyes, and they had jabbed and jabbed and jabbed. Bearing in mind I was at my wits end emotionally, I ended up saying, “That’s enough.”
I just left and got into the car and collapsed. I thought, “I’m not having one of those tests.”
When I was in the hospital, they said, “First thing first, we’ll send you down to have one of those gated cultures.” And in my argumentative state, I’m saying, “No way. I’ve got an ultrasound of my heart. That’s enough of a pre-treatment test. It’s not going to change the outcome of anything. I’m not having it.”
There were all these conversations back in the office outside of the ward saying, “How are we going to deal with Leanne?”
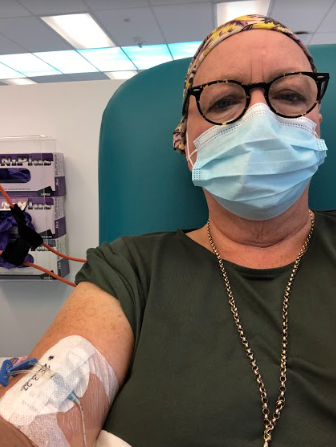
PICC line
Anyway, in the end, because I do have a bit of a problem with needles, that afternoon they sent me off to have a PICC line inserted in my arm. [It] was the best thing ever because I didn’t have to face needles and finding veins every time I went in for treatment.
I did settle down after that, and do you know the way I settled down? I actually said to myself, “I have to surrender to this process because if I don’t, it’s going to kill me. Just the process and the stress of the whole thing. I’ve got to surrender and accept.”
Those were the two words I kept focusing on while I was in that hospital ward because the doctor had said to me the day before, “Come in for the day. We’ll get you started on the treatment. Bring an overnight bag in case you have a reaction to something, but more than likely, you’ll be home.”
»MORE: Read patient PICC line experiences
Reaction to first treatment
Well, I was there for three days, and it just went on and on. I was there for over New Year’s Eve. I thought, “What a way to see in the New Year.” When the treatment started, that’s when the PICC line was there.
The nurses were just delightful. But there I was, lying in this hospital bed. When the rituximab started, so R-CHOP, that went on for hours. That went on all morning, the infusion for that. I couldn’t believe how long all of this took. Then the remaining drugs took the rest of the afternoon.
That night I slept so well because I think I was just exhausted emotionally and physically from the whole thing. They monitored me for the next day, and then I could go home.
Then four days later, I had an appointment back at the hospital to meet up with the hematologist. My whole gastrointestinal tract was riddled with Candida, so I just felt miserable.
When I went in to see him, he prescribed medication that I ended up having to take along with everything else for the remainder of the time that I was being treated to make sure that never happened again, which made me very worried about my gut health. But there were bigger fish to fry than worry about that at that point.



Neuropathy
After the second round, I started having incredible neural numbness in my fingers and feet. I went back before my third round of treatment, and I said to the hematologist what was going on. I’m really worried because I understand that this nerve damage can be permanent.
I wanted to get back into playing the piano, because when I turned 60, I was thinking, “What other things do I want to bring into my life that’s creative?” I said, “I cannot play the piano. My fingers are numb.”
Anyway, the drug that was causing that I think is called vincristine. They ceased that from that point on, so I didn’t have that in my regime after that. Through the dialogue, the conversation, and better understanding what was going on calmed me down.
What was your reaction to the GP trainee figuring this out after two years of symptoms?
I was extremely angry and upset about that. When the trainee GP, gave me the bad news, I said to her I always worried about the CT scan that I’d had in May. I’d asked my normal doctor, plus another doctor in the practice who I’d gone to to have a skin cancer check, to get in and have a look at my file.
[It was] because I just thought, “Why would my spleen be enlarged?” I didn’t understand the importance of looking at the size of lymph nodes. Not being trained medically, I didn’t understand that. But I thought it’s very unusual that my spleen is enlarged. Maybe that’s explaining why I was having abdominal discomfort in my left-hand side.
Thank God I crossed paths with her, because if not, who knows how much further along I would have gotten?
Those two doctors, as well as the gastroenterologist, did not say there was an issue. So I was extremely upset about that. The trainee GP said to me, “We can’t worry about that now. We’ve got to accept that that’s happened and move forward.”
Going to former GP for a skin check
It sat with me for quite some time. About July last year, I was due for another skin cancer check. In Australia, because we’re raised in the sun and at the beach and often [never] wore a lot of sunscreen, it’s just a standard thing that [when] we get to a certain age, we get our skin checked, usually annually.
The GP I used to see, who’d been explaining things away — talking to me about lifestyle, medicine, and relaxation — was the doctor who’s now moving into doing skin checks. So I went to see him because I thought this would be really important for him to see me now.
Anyway, I was in the waiting room and waited 40 minutes, much longer than normal. I was all dressed up, but I had my wig on because I had next to no hair. When I went in, I looked pretty normal because I had this wig on.



An apology from former GP
He said to me, “Leanne, I’ve just been reading through your file, and I’m so, so sorry that this has happened to you. I cannot understand how I missed this. I’m going to spend a lot of time reading back over your files and learning from this so that it never happens again. I am so sorry.”
That was important for me to hear. We spent a fair bit of time talking about what had been going on and how I felt. Then when it came time for him to do my skin check, I said, “Can you check my scalp while we’re at it? Because I’ve just noticed some marks up on my scalp.”
He said, “Sure thing,” and then I ripped my wig off, and that was the biggest shock he got. He didn’t realize I had a wig on. Then when he saw me with no hair, I could see tears in his eyes, and it really upset him.
I thought, “I’m glad I shocked you because this is not just a paper report. This is a person’s life. And you know that I’ve been coming to you for years.” Now, he has asked to see me every three months and doesn’t bill me for it just to keep in touch with me.
Doctors not having enough time
For me, the fact that he apologized was very important, and the fact that he’s saying he’s learning from it. It makes me wonder, as a doctor, whether that’s a pivotal moment in his career of listening. I think a lot of our doctors — and I’m sure it’s the same worldwide — are so overworked. You’ve got an appointment. You’re in and you’re out within 10 minutes or so.
Even though I was presenting that all the time and getting all these tests done, no one was looking at my case holistically. Actually, it took that trainee GP who had time. She told me her appointments were an hour apart because it’s all part of her just learning the profession.
She’d had all of the years of training and so on, but these placements were part of it. She had the time to sit and read and think and connect the dots. Thank God I crossed paths with her, because if not, who knows how much further along I would have gotten? So, yes, it’s not a good story.
Processing a Cancer Diagnosis
Effect of cancer diagnosis on friends
The shock for all of my friends in my circle when they heard what had happened. Because I’m a person that’s full of the zest for life, it shocked everyone. The hematologist thought I could have had follicular lymphoma for several years prior.
[My friends were thinking,] “If Leanne was walking around like that with cancer, who knows what we’ve got?” So a number of my friends all went with different ailments that they’ve been explaining away to get investigated. Even my son, who’s 33, went off and had a full medical as well, because you just never know.



The lesson I learned from that is never let go and advocate for yourself because there’s no other way. The shock that I got, even though I knew for some years I wasn’t right, and then stopped working full time and had started slowing down my career.
[I was] thinking, “I don’t feel right. Don’t know what it is. I just know I can’t keep pushing myself where I used to.”
To have that diagnosis was just a terrible shock. It’s taken me a long time to come to terms with it.
Importance of mental health
Moving on to another topic, the mental health side of things, cancer is a mind game. Managing your mind and your emotions through the process is something, again, I’ve never heard other people really talk about.
If there’s a message I can get across in this story, it’s talking about somebody who was in complete control of her life that had to really take stock. I almost feel like it’s Life that had been tapping me on the shoulder, saying, “Time to change. Time to change.” It took the massive shock to get me to change the way that I lived my life.
What change in your life do you think needed to happen?
I think for decades because of this need to be a high achiever, I pushed myself beyond what most people would do. I guess I’ve done everything the hard way. When you think about being a single mother, a lot of women that are single mothers would take a step back in their career and just think, “Focus on this for now.”
But I thought I could have it all, and so I wanted to have a beautiful home, live in a way I would have lived if I had been in a marriage, and had the overseas trips. We did fabulous holidays. We had a lovely home.
Plus, this drive to have a really good career, and so I chose jobs where after I might have been in the job [for] seven years, five years, then I’d move and try to get a new mountain to conquer.



A number of jobs I was in were non-traditional sectors for women. For example, I worked at the port that’s nearby, so shipping and logistics, and was in an executive role in that, which was so interesting. But again, women in those levels of jobs were not the norm, and so to perform in those, you’ve got to work even harder than the guys around you to be taken credibly.
Another role, I worked for the state government. I managed the southern half of New South Wales, the state that I live in, for Crown land, and that’s state-owned land. 50% of the state is Crown land, a lot of it’s leased and licensed, and the local government manages that under reserves. It was such a fun job. I loved it, but [it was a] massive load and lots and lots of trouble.


Pushing yourself too far
[I was] constantly pushing myself, not getting enough sleep, trying to be everyone, everything to everyone, and be there for my kids. It was just burning the candle at both ends.
I’ll give you an example when I was working where with the travel, if I was a guy, [it would have been different]. If I needed to travel out west to have meetings for several days, a man would have — and I’m generalizing, but I saw my other colleagues who did this.
They would drive or fly out the day before, go out and have a nice meal and a relaxed stay in a lovely hotel, have a leisurely start to the day, and then begin the meetings. Whereas me, I went home because I’m worried about my kids. They needed me around.
When they went to bed, I’d be washing school uniforms, making sure the lunches were ready, getting things sorted. I had a very good ex-husband who often used to come and move into my home and carry on the family while I was away. But then I’d get up at like five in the morning and drive up to the airport.
Then my days were jam-packed with meetings. I might stay overnight somewhere, but then a day later I’d be flying back late in the day, driving the two hours back from Sydney Airport. It was just frantic.
Time for making changes
No one realized, I don’t think, the personal toll because I never really talked about it. I didn’t want to be seen not to be coping, but also, I was in a very male world, where they all had wives doing all that stuff for them.
It’s funny. With society, women are applauded when they can do all of these things, but there’s a personal toll. I’ve realized now all those years of pushing myself like that exhausted me and I think created an environment in my body where whatever happened, it was an environment for cancer to get a hold.
I look back now. I don’t have any regrets because I’ve loved my life, and I’m so satisfied with everything that I’ve done and achieved. But yes, it’s time for a change, big change. That’s why through the beginning of the treatment, I sought out a psychologist to help me.
What helped with the stress of diagnosis and treatment?
When I was first diagnosed, living on the coast, I used to go for lots of swims. I found swimming in the ocean was particularly therapeutic for me and very relaxing. Even just walking along where the waves crash on the sand or around headlands because of the negative ions that are released.
That was very good. I used to love getting up early in the morning and just sitting outside listening to birds and just having time to just breathe, I suppose. But that was in the early days.
There were a lot of conversations with girlfriends about how I was feeling, and they completely wrapped around me. It was such a beautiful thing. I used to think to myself, “Gosh, I must have been really lovely to people over the years,” because in my hour of need, everybody just came. It didn’t matter where they lived.
My phone was ringing constantly, text messages. Then through the whole process, they were there for me in all different ways, dropping things off for me, food or groceries. One girlfriend came round during the time when my hair was falling out and brought lunch.
It was a pretty distressing time, and she walked into the bathroom and said, “Oh my God, look at the floor in the bathroom.” I said, “Look, there’s no point cleaning it because every time I go in there, more and more clumps of hair fall out. I’ll vacuum it shortly.” And she said, “Oh my God, it’s like carpet in there.”
For times that were really distressing, it was so lovely to have that. During the treatment, I settled down because I thought finally something’s being done to sort this problem out.
»MORE: Patients describe dealing with hair loss during cancer treatment
Seeing a psychologist
I also had started meeting with my psychologist. That started in February. So the treatment started on New Year’s Eve, and I met with her over Zoom weekly initially for the first few, and then it went to fortnightly and then three weekly and then monthly.
Is that my problem or theirs, and is that going to serve me by doing that?
That was a really great sounding board for me because I could talk to her about all sorts of things that I was concerned about, particularly when you’re facing death. I was thinking about what that meant to me and thinking about what my priorities were now and how I wanted to live my life moving forward.
I knew that that person and the way that I was living was not serving me at all. Those behaviors of pushing myself and being full-on active needed to change, and I needed to start looking after me as number one, not everybody else. It was so interesting going through those sessions.
She got me to talk about my life and the dynamics of family and so on. Through that, I discovered why I was pushing myself so hard. I’m the firstborn. There’s a whole range of dynamics in my family, which meant that I really wanted to get recognition.


By doing these things where I was winning awards and doing all of these fabulous jobs where women normally didn’t work and so on, that was filling my cup and feeding that need.
Now I realize I’m the only person that needs to approve and give recognition to myself. Really, I don’t need to do any of that anymore. I’ve conquered all those mountains, and I feel quite calm and content now to think that was during my career, but now it’s time for me.
Rethinking relationships with others
The psychologist has helped me really think about how I respond to things. It’s being more wise, using wisdom. Rather than the patterns of reacting to situations with behaviors that I developed over the years, now I’m thinking, “Is that my problem or theirs, and is that going to serve me by doing that?”
I’m even thinking about friendships and looking at some friendships where I think I had given a lot of energy to people to support them in issues, and now I realize I’ve got to have friendships where it’s a two-way street.
A lot of friends did step up and really support me. A couple of them didn’t. It’s an interesting thing, and I don’t feel any animosity because people cope with things in different ways.
Some people, I’ve realized, if they hear the word, “cancer,” they think, “My friend’s going to die. I can’t handle goodbyes and death. I might as well quietly disappear now because it’s all too hard for me.” And it’s a shame that that happens, but that’s life, and we’re all hardwired differently.


What emotions were you feeling?
The follow-up with the hematologist after the first treatment, when I had the terrible Candida, I had to go and have a blood test. Before I saw him and because I had the PICC line in my arm, I thought, “Oh, thank God. All these blood tests now will just use the PICC line.”
And when I went in to where the nurses took the bloods, they said, “Oh, we don’t touch the PICC line. That’s only for the cancer clinic. We’ll have to stick a needle in your other arm.”
That was all it took. I was feeling so miserable and unhappy. I sobbed and cried the whole way through and was saying, “I can’t understand why this is happening to me.” There’s a waiting room just outside with people waiting, listening to me carrying on.
After they took the blood, I walked out and sat there, quietly thinking, “Oh my God, I’m so embarrassed.” That was really a sign of how upset I was and just not coping at all. It wasn’t until probably by the second treatment that I had been through it a couple of times and understood then what I was dealing with.
Researching and asking questions
I spent hours researching, looking at videos on YouTube, conference papers, reading research papers, anything I could get my hands on to understand what I was dealing with, because I found that the medical profession basically told me information on a need-to-know basis.
I’m a person that I need to understand the big picture and then come into the details. If I don’t have that, then I’m anxious and worried because I can’t deal with ambiguity in that way.
Each appointment that I had with the hematologist, I had a notebook just like this size, carried it around with me, and every day I would write down the date and what symptoms I was experiencing on that day.
Then I had another section for questions if I was doing research or questions that I just needed to know based on what was happening to me, and I’d take those into my appointment with the hematologist.
He after a while started laughing, and he said to me, “Do you have a medical background?” And I said, “No, I don’t, but this is happening to my body, and I need to understand. I’m project managing this because this is my life.” He understood that.
After a while he would say, “I’ll send you to one of my oncology nurses. She’ll be able to explain a lot of these answers to the questions you’ve got.” But he did deal with a lot of them.
Giving it a red hot go
It’s almost like a treadmill. They get patients, they bring you in at the beginning, away you go through the process, and then you’re sort of spat out at the end. So I was in the middle of that.
I felt there was nothing more I could do. Everything that I could do was being done. When the treatment started, I was in that dreadful shared hospital ward, and I was saying to myself, “Surrender to the process and accept.”
I made a deal with myself. I would never have chosen this for myself, but I’m going to give this a red hot go. That’s an Australian saying. I’m going to give it a red hot go, and it means whatever I can do to make this a success, I’m going to do it.
So I made sure I walked every day. Hematologists talk about the need to have vitamin D, and I was seeing an acupuncturist on a regular basis. I was taking not only vitamin D, but also magnesium and vitamin B12. Just things that I felt that I could do to keep myself as healthy and help that treatment along.
How cancer affected family
Because I had all of my network supporting me, even though I was alone a lot, I still felt incredibly wrapped around. That really helped as well. But I think I needed a lot of time just to think things through.
I should just talk about the ripple effect on family as well. At the time when I was diagnosed, I thought this was all happening to me, but cancer just doesn’t happen to the person whose body it is in. It happens to the whole family and network.



I found that my two children were really rocked by the news.
»MORE: Breaking the news of a diagnosis to loved ones




Reflections
Where are you currently with your treatment?
The treatment finished on the 14th of April, and so I’ve had no more treatment since that time. But it’s been a rocky road after that time. Six weeks after the last R-CHOP treatment, you do a PET scan.
I had a CT scan midway through, and that was heartening because it showed there’d been a 50% reduction in the lymphoma activity, so that was good. At the end of the treatment, I was feeling absolutely wiped out and quite wretched and looked absolutely awful.
When the PET scan was done at the end of May, I then had a follow-up appointment with my hematologist. That was due to be on the 6th of June, and the day before, his office rang me up and said, “The professor wants to meet with you a week later. He’s decided he wants to take your PET scan results to a multidisciplinary team meeting.”
I thought, “Why? What are the results showing?” No one would tell me. So I then waited a week, thinking, “Oh my God, what is going on? Why has he got to do this?” Then the day before my allocated appointment, they rang and said, “The professor’s got COVID, but he’ll still meet with you over the phone tomorrow.”
»MORE: Patients describe dealing with scanxiety and waiting for results
Results of PET scan
I woke up that morning with a really sore throat and feeling unwell. I did a RAT test at that point. It was negative, and I thought, “At least I haven’t got COVID.”
When I spoke to the professor, he said, “I cannot understand the results of the PET scan. I thought that the R-CHOP would have worked, but there’s still activity. There’s inflammation in your abdomen, and we can’t understand why this is.”
I was at home alone on the phone, and I started to cough. He said, “You don’t sound well at all.” I said, “I think I’ve got a bad case of the flu.” He said, “Get yourself off and have a PCR. I think you’ve got COVID.” I was telling him the symptoms.
When I got off the phone from him, I did another RAT test. Yes, it was positive. Went off and had the PCR, and it was confirmed I had COVID. I’d found out on the day that my PET scan results that looked like my treatment hadn’t worked, I had to isolate for a week, and I was sick with COVID.
From a perspective of thinking, “Oh my God, I’m dying.” I felt really lousy. That was pretty awful, and no one could come to see me because I had COVID. I had all of that knowledge in my head of the treatment hasn’t worked. I’ve just lost six months of a limited life. What am I going to do now?


I was ravaged by all of the chemotherapy and the rituximab. That does shocking things to you. The rest of it kills the cancer, but it does shocking things to your body. He said, “We’re going to have to do another surgical biopsy to try and understand what’s going on.”
Mesenteric inflammation
In July, with all of this going on in my head, I had the biopsy again. They did quite extensive laparoscopic incisions to get lots and lots of samples, and then I had to wait for the results of that.
When I went to the doctor, I was expecting really bad news. The professor said to me, “There’s no sign of cancer, but it doesn’t mean there’s no cancer in your body. It just means maybe they’ve only got the lymph nodes from your mesenteric that weren’t impacted.”



But they did see lots of scavenger cells, which I thought was unusual, and he did, too, so late on. Anyway, he said, “I want to have another PET scan.” So in August I had a PET scan again, the second one, and then I had a third one in December.
By that stage it had gone to the multidisciplinary team several times, and the results then they now were saying to me, “It appears you have no cancer in your body. We don’t know what that inflammation is, but maybe it was there beforehand. It might be mesenteric inflammation.”
Meditation
In terms of the meditation, when all of this was happening in July and I was thinking I was dying, the psychologists that I saw said to me, “I think you need intensive support with meditation. I’m not the person to help you with that, but I know somebody who can, and she’s given some of my other clients incredible outcomes.”
So I went along and met this lady, and it’s a type of meditation called Vedic meditation. I used to think meditation [was where] I could just sit quietly and relax. I’d done other meditation over the years, where you might do the creative visualization or look at a light or a candle or something.
[Vedic meditation] is one where you sit with your back supported, your eyes closed, and you’re given a mantra. You say that in your mind. Nothing else external. This is something I would really encourage others to think about introducing into their life.
I do that practice two times a day, morning and afternoon, 20 minutes, and I believe it’s a form of energy healing. The feeling that I get doing that is like nothing I’ve ever experienced before. It’s quite magical.
I go to group meditations with others because I feel that that collective energy is very good. I also have been doing some advanced work around breath work and so on since Christmas. I’m very committed to that.
There’s a lot of things I have no control over in my life, but there are some practices like that that I’m definitely making sure I include. It’s really helped.
Final words of advice
I think in terms of words of advice, this is an opportunity to take stock of your life and actually think about what do I want to keep in my life, and what things do I need to let go of?
There’s an imbalance of some sort, obviously, for this to have happened. It’s a real opportunity to be able to rethink the way you want to take your life to the future and to see and realize a future for yourself that actually can be even better than what you’d experienced.
Sometimes experiences like this, you need to open your eyes to thinking and behaving in different ways. Really have faith and hope that things will turn out, because I’m a true believer that thought does create.

Inspired by Leanne's story?
Share your story, too!
More Non-Hodgkin’s Lymphoma Stories
Don S., Relapsed Diffuse Large B-cell Lymphoma (DLBCL)
Symptoms: Weight loss, fatigue, enlarged lymph nodes
Treatments: Chemotherapy, radiation, immunotherapy (epcoritamab)
Leanne T., Follicular Lymphoma Transformed to DLBCL, Stage 3B
Symptoms: Fatigue, persistent cough
Treatment: R-CHOP chemotherapy, 6 rounds
Robyn S., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL), Stage 2E
Symptoms: Enlarged lymph nodes
Treatments: Chemotherapy: R-CHOP, R-ICE, intrathecal, BEAM; autologous stem cell transplant, head and neck radiation, CAR T-cell therapy
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.





