Paige’s Stage 4 Diffuse Large B-Cell Lymphoma Story

Paige was diagnosed with stage 4 Diffuse Large B-Cell Lymphoma at 28 years old. After initially dismissing her symptoms, her insistence on getting a CT scan put her on a path she never thought she’d be on.
She shares the importance of self-advocacy, a good support system, having a positive attitude, and how sometimes, you just need to take things a day at a time.
- Name: Paige C.
- Diagnosis:
- Diffuse Large B-Cell Lymphoma
- Non-Hodgkin’s Lymphoma
- Staging: 4
- Symptoms:
- Weight loss
- Extreme fatigue
- Swollen lymph nodes in the neck
- Treatment:
- R-EPOCH chemotherapy
This is your journey and however you want to choose to have it, you’re able to do it. At the end of the day, it’s your journey and you’re going to have to figure it out.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
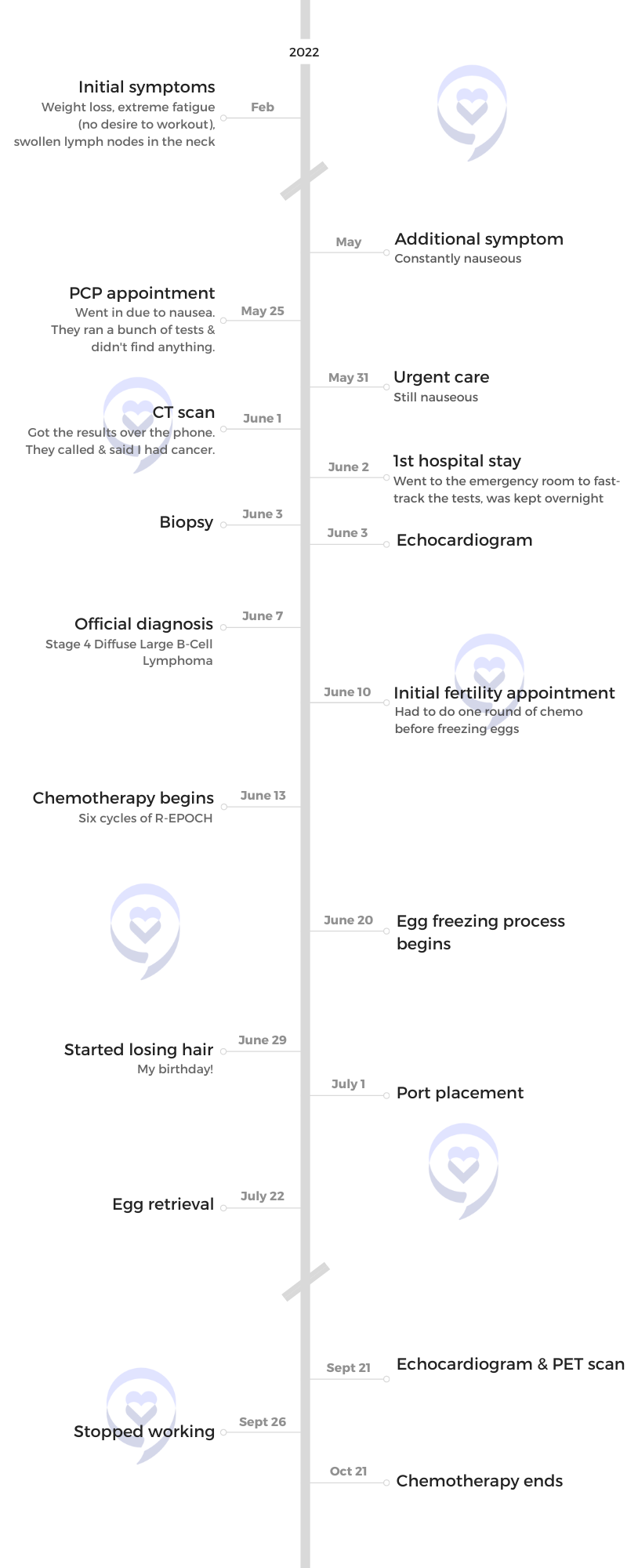
Pre-diagnosis
Introduction
I live in California. I like to go to the beach, tan, go out with my friends, [and] try new restaurants. I love a good glass of rosé, espresso martinis, [and] just living the normal 20-year-old lifestyle while trying to balance having cancer and everything.
I’m a very positive person. I’m enthusiastic. I’m social. I try and look at the bright side of things. I think everything happens for a reason. Any challenge you have, just face it one step in front of the other. That’s how you’re going to get through life.




Initial symptoms
I was really, really nauseous. I [noticed] I’ve lost a lot of weight. I was like, “Great! This is awesome!” But obviously, it’s not awesome. I didn’t really put two and two together.
I was always tired [that] I stopped working out. I used to work out all the time and I was just too tired to work out. [I] started losing weight and didn’t really think anything of it.
Then I always have chest pain. I’m like, “Okay, just anxiety.”



Every symptom could be your day-to-day: bruising, night sweating (very common if you live in California), losing weight, being tired, [and] having chest pain, which I thought was just anxiety.
Then, all of a sudden, I was unbelievably nauseous for about a month. It would creep up to the point that I even started wearing seasick bracelets. There’s something going on that I had absolutely no clue [about]. I thought it was a stomach ulcer or a bacteria.
I went to the emergency room one day after work and they’re like, “You have to get an ultrasound.” I was like, “I need a CT scan. I don’t think an ultrasound is going to tell me anything.” They were like, “An ultrasound’s fine. You can’t even get a CT scan until you do an ultrasound.”
I end up getting a CT scan and they see a mass in my chest and a little below. The emergency room calls and tells me, “You have cancer until proven otherwise.” Basically, cancer until proven guilty, which is just wild to me that that’s how you tell somebody.
Read about real-life cancer survivors’ experiences and their own reactions »


I was unbelievably nauseous for about a month. It would creep up to the point that I even started wearing seasick bracelets. There’s something going on…

Deciding to get checked
I was so nauseous to the point that I was not able to work. I would lay in bed. On the weekends, I would normally go out [but] I would come [home] to hang out with my parents and just sleep.
I was in New York and we were visiting my little sister who was doing an internship. I slept for two days, exhausted. I was drinking champagne to try something to make me feel better and nothing would work. I would just power through it but I was so incredibly sick. I even called the doctor, “Can you send me Zofran in New York?”
After that, I was like, “Something is wrong.” I had every symptom of morning sickness and I was like, “Am I pregnant?” But I took pregnancy tests and [the were] all negative.
It was just wild because all that doesn’t add up to cancer, which is just insane to me.
Diagnosis
Reaction to the diagnosis
The lady [from the] emergency room called me and was like, “I’m sorry to be the bearer of bad news, but here’s an oncology number.” I called the number she gave me, bawling my eyes out, and left a message. They called me back in 10 minutes and it was like, “Oh my god. It’s okay. Are you okay?” It was this really nice lady. She is an onboarding person. I was just hysterically crying. I was by myself in my apartment [when I] got the phone call.
I made an appointment. Then I called my parents hysterically crying. It was insane. I did not process it well. I just cried. Then I think I drove home. I don’t really remember. It’s all kind of a blur.
I got home from New York Sunday. Tuesday, I went to the emergency room and then Wednesday, I had a CT scan. Wednesday at 5:30, they called me and told me. Then Thursday, I was in Newport. I had an appointment that Monday with oncology and my parents were going to be there. They’re both very involved [and] supportive, which I’m so grateful for.
Find out what you can do and how you can support a loved one who’s been diagnosed with cancer »


On Friday, I was so nauseous [that] I couldn’t get out of bed. I was so, so sick. I called the oncologist, “Can I come in today? I don’t know what to do.” He was like, “If you go to the emergency room, I’ll admit you.”
Never been to a hospital in my life so I call my mom. One of my friends actually drove me, which I’m so grateful for. I had to call my friend and be like, “Hi, I have cancer. Can you drive me to the emergency room?” That’s an interesting phone call that your friend gets. She ended up driving to the emergency room. My mom met me there [with] overnight bags.
I go to the hospital, go to the emergency room, [and] the oncologist met me before I was admitted. She did a biopsy, a CT scan, and [an] echo gram. We did fast-forward the entire process, which, looking back, I’m so grateful for. If I [wasn’t] in the hospital, I probably wouldn’t have gotten treatment until [later].
I was at Hoag and USC Keck. I could not be more grateful for all the doctors. I hate the hospital but I couldn’t imagine it being at another hospital.



No time for a second opinion
The hardest part is trusting the doctors. I didn’t have time to get a second opinion. He was like, “You can get a second opinion, but you have no time.” I had to start treatment. I think I went in Tuesday and I start treatment that Monday so I had no time to process [everything].
It’s just overwhelming. Trusting the process and realizing that non-Hodgkin’s lymphoma is what they call “curable” so just trusting that this is the best treatment.
I’m doing six rounds of chemo. That’s insane. I didn’t really trust the entire process until I got my PET scan and the results turned out really, really good so that’s what made me realize, Okay, the doctor knows what he’s doing. Everyone has told me, “Oh my god, that’s your doctor? You have the best doctor. Wow, that’s amazing.” Just really having to put faith in someone else’s hands. Not having control is really hard.
The hardest part is trusting the doctors. I didn’t have time to get a second opinion.


Treatment
R-EPOCH chemotherapy
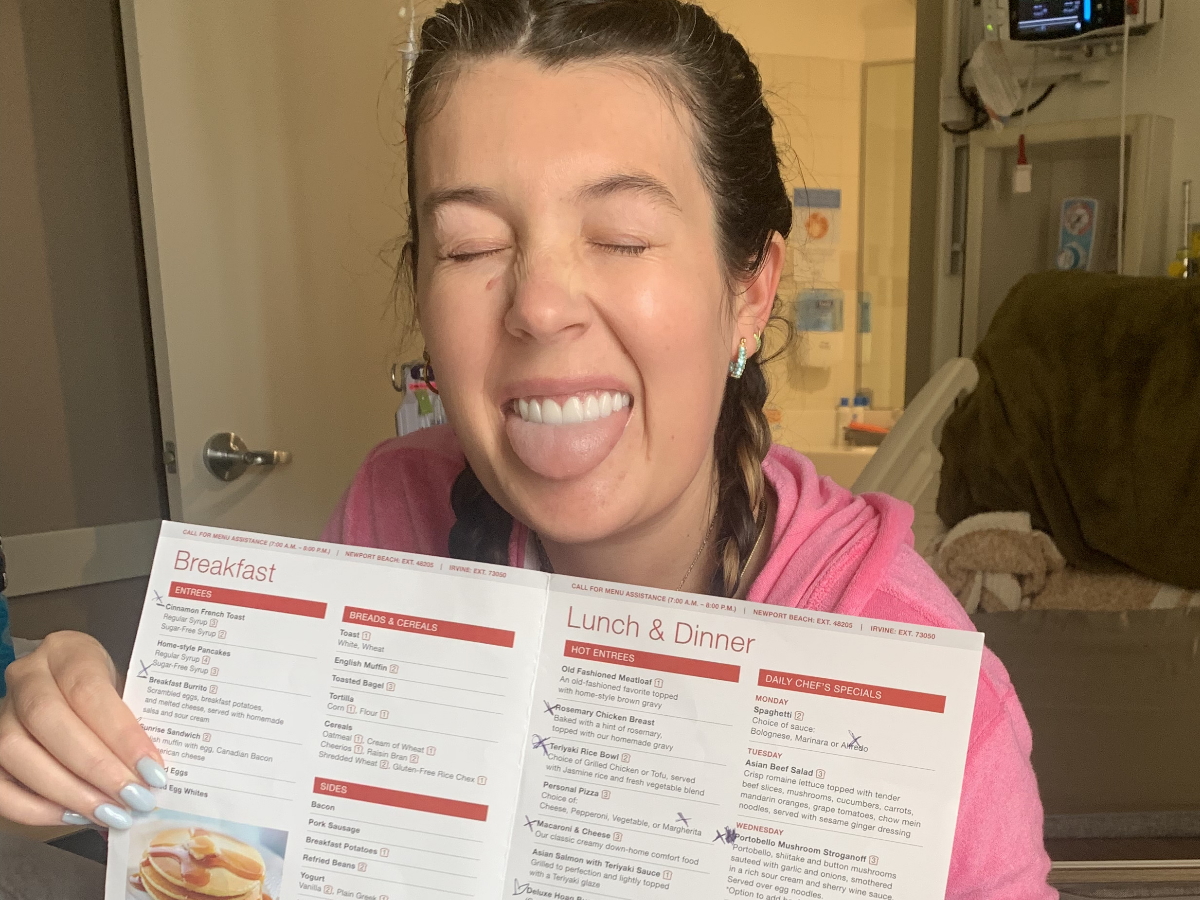
The treatment’s called R-EPOCH. It’s six rounds and five days in the hospital so it’s 96 hours of chemo. I was so overwhelmed when he told me [about] the treatment. It was a lot.
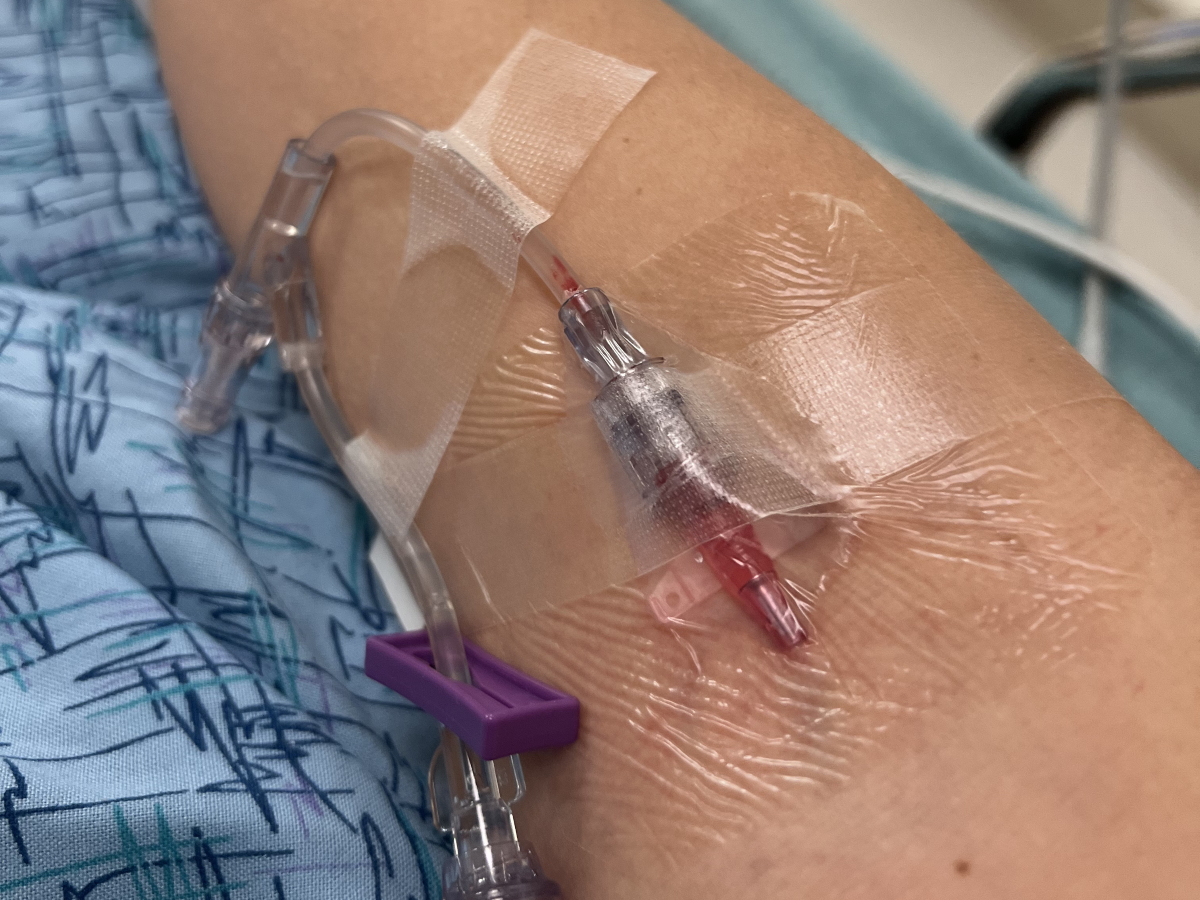
I get in the hospital and they have to do a COVID test, a MRSA test, all these crazy tests. They have to access my port. My port is really hard to access because I didn’t want it noticeable so that’s kind of a positive part, I guess. Then they start the 96 hours of chemo.
They start it Monday and then Friday, I end up being out at 4:00 or 5:00, whatever time they’re able to start the chemo that Monday. It’s at their mercy. They call me up whenever the hospital has room and tell me [to] pack a bag.
My week one [of] chemo was a nightmare. I don’t remember any of it. I’m an Advil gal and that’s about it. I was pumped with so many drugs — Zofran, Xanax, Ativan — and just the emotional toll of all of it so I do not remember most of my first treatment at all.
It was scary being in a hospital for five days. It’s actually terrifying. I [ended] up getting really good headphones because I’ll wake up in the [middle of the] night and hear screaming. It’s like, “Nurse, get off me” or “Stop putting an IV in me.” I’m terrified of the hospital and I think it’s going to give me PTSD [for] the rest of my life. They try to be really supportive. The nurses are amazing, but it’s not their fault.
The nurses have been nothing but great. They come [into] my room and hang out in there. The night nurses come in and do funny dancing so I have a bunch of videos of me dancing. They just try and do anything to put a smile on your face.
Looking back, after my PET scan, it was a lot bigger than I ever thought it was. I didn’t realize how huge the tumor was and I was just feeling extremely overwhelmed. I just had to keep going forward and put one foot in front of the other.




Hair loss from chemotherapy
Two weeks after your first treatment, you end up losing your hair. I haven’t lost all of my hair and I decided not to shave my head. I know a lot of people do and more power to them. I just couldn’t do it. But it’s really hard to see clumps of your hair falling out. That is a whole ’nother ball game in itself.
And then being on hormone pills when you already don’t feel like yourself… You’re already emotional. I don’t know how I handled it to this day.
I cried every day. It was miserable. I started journaling a lot, writing down all of my feelings, and everything. I think that has really, really helped me. Just journaling every emotion — the good, the bad, the ugly.
How can you cope with losing your hair during chemotherapy? »



Status
It shrunk [by] about 80% and they think right now it’s just dead tissue, which is amazing. My tumor originally was active 10 and now it’s 2.9. They want it active at 2.
I only have one more until my last treatment. The PET scan was looking great so I am excited to be in remission. I’m just stoked about it.

Plans after treatment
I’m going to take [a month] for myself. It’s going to be like a Paige month, what I want to do.
I’m going to get a personal trainer, get back into working out, go on walks, try new restaurants, and travel. I’m going to Switzerland for about two weeks.
I am also starting a podcast with one of my girlfriends. It’s called “Our Life Changes.” Life can change. It doesn’t matter if you have cancer, if you’re Navy SEALs, if you got hit by a car, or won the lottery. Life always changes. Things always happen.
I think I’m just going to look at different opportunities. I am in marketing so I will probably go back to looking for a 9-to-5 job. I don’t know what I want to do exactly. I want to do something meaningful.
I’m going to try [to] get back out there and date. It’s going to be a wild ride. I was talking to my therapist and she was like, “Do you want to date that person? You’re a friggin’ rock star. You kicked cancer’s ass. You did amazing. Do they get to spend time with you?” Reverse psychology and not like, “Is he going to text me back?” I want to spend time with him. Are they worthy of my time? Your friends — do they get to hang out with me? Just reverse psychology all of that instead of thinking the way a lot of people think.




Living life as a young adult with cancer
I just had to do what made me feel right and push myself forward. I still wanted to be normal. I still wanted to be able to go out with my friends. I still wanted to be able to work. I still want to be able to have all the energy traveling, which obviously had to get put on [hold].
Your twenties is hard enough. Dealing with dating, friends, life, job, [and] finances, then having cancer on top of it is just insane. I think just really figuring out who I am as a person and what my goals are, what I want in life, and what I want to achieve.
I was single [at] the time. I was dating a bit. Then when I got the news, I put everything on pause and really wanted to focus on myself and who I am, what I expect in a person, what I value, [and] what I want. Right now, the ball’s in my court. What do I see in a person? What do I want? Do I want someone motivated? Do I want someone with ambition? Who do I want to spend my time with?
I don’t know if it’s hit me yet. I believe everything does happen for a reason. I think maybe I’m able to handle it. I have no clue why it happened to me. I’m not looking for someone to be mad at or, “Why is it me and not you over in the corner?” That’s not the person I am. Yeah, it sucks. Do I wish this upon anyone? No, but it is what it is.

Fertility preservation through egg freezing
I want to have kids in the future and when you’re going through chemo, there’s a chance you can’t have kids. I was fortunate enough to be able to freeze my eggs, which I am so grateful for. I couldn’t even imagine not being able to.
But that whole process alone was insane. I was on hormone pills for a month. I had to do treatment first then I had to go back and start the fertility processes and that took a whole entire month. Most people are only on them for about a week. Luckily, I got a bunch of eggs out of it.
Learn about fertility options before and after cancer treatment »




Importance of a good support system
I tried to turn to my family and friends, but I shut everyone out because it was such a dark spot in my life that [I’d] never been in before. I don’t do well on hormones in general and then losing your hair is another thing.
I turned to Instagram and started reaching out to a couple [of] girls who posted about it. I asked for any tips and tricks. There [are] probably 20 different messages I [sent]. I ended up meeting a couple [of] girls through Instagram and now we’re all friends. We’re all going through the same process at the same time.
I did try and do support groups — that wasn’t really my thing. But then if you have lymphoma, there’s a support group I joined and I actually am speaking at it. It’s called Lymphoma Ladies — I’m helping run that one. That’s a really positive group. When you put all the support groups together, I was so overwhelmed and I would just be hysterically crying. “Is this going to happen to me? I don’t know what to do. Oh my gosh.” And that’s not the case.
My family has been a huge, huge support. I could never imagine doing it without my family. They are amazing. They’re at the hospital all the time. My friends have been amazing. They’re always at the hospital. No one leaves. Everyone’s there with me all the time. I can reach out to people if I want.



Letting people in
A support group is literally what you need 100%. You just have to accept the fact they don’t know what you’re going through, but you need to let them in. They’re really just trying to be there and they’re really trying to help. And yes, they’re going to say the wrong thing, but you just have to be okay with that.


I think when I got off all the hormone pills because I was not myself. I was like, “I have to go back for my second treatment. I need support around me. I need friends. I need family. Am I going to be the biggest brat in the world and lose everyone that I’ve built a whole life of making?”
I just really had to look at it from trying to be positive again. You’re going to have rough days. You can have the worst day in the world and you’re at rock bottom then maybe the next day could be the best day in the world. You don’t know what the next day [brings].





Having a positive mindset
People have asked me, “Paige, how are you so positive?” You have two ways to look at it. You can look at it by being so angry at the world, so negative — and, believe me, I’m negative, angry, a lot of emotions — but you can also look at it as you have to do the treatment no matter what. You have to do this. You can look at it glass half full and just try and get help. Basically, I can be negative, I can be a total brat, or I can be positive, try and move forward, move on with my life, and learn something from it. And that’s the way I looked at it instead of being angry and shutting the world out.


I’ve always tried to be happy and live in a bubble [and] brush things off. “Oh, no, it’s fine. Whatever. It doesn’t matter.” Don’t touch my bubble, don’t pop my bubble. And then cancer popped my bubble. I was like, “Oh my god. Wait. My bubble’s gone. What do I do?” I just looked at it [as] having to just be happy, positive, and grateful for things.
At the same time, I can still be sad, I can still be upset, I can still be mad, but what’s going to make me get through this treatment? It’s going to be having people around that love you, support you, [and] care about you. Even the nurses are some of my friends now. They’re my age and they’re awesome. I’m just trying to look at the bright side of things.



Social media for support
I’m really active on social media. I might have posted a bit early before but I think I was in such shock. I didn’t really realize what I was up against. I was like, “Oh. It’s cancer. It’s stage 4. It’s fine. No big deal.” I have always posted my life and I was like, “Okay, I’m going to share this. I’m going to make a post [about] being a self-advocate and just trying to reach others.”
The feedback I’ve gotten has been amazing so I just keep posting my whole journey. I know a lot of my friends, family, my parents’ friends, and everyone has been super concerned. The amount of support I’ve had is insane. People want to know, “Is Paige okay? What’s going on? What’s happening?” I think that’s the whole reason why I just keep posting. Once I did my first post, I was like, “Okay, well, I just got to keep posting about this entire journey.”
Words of advice
Your twenties are [when] you’re finding out who you are and what you want to become. And if you get this crazy, scary diagnosis, you don’t have to have all the answers today. Keep chugging along and eventually, the roller coasters and the back flips will stop, everything will be a smooth ride, and you’re going to have different bumps in the road.


You’re not alone in this. Reach out to people who want to help you. I want young people to reach out because I feel bad. I don’t want people to go through this alone because I wish that I didn’t have to go through this alone. I went in so blindsided and that’s not the way you want to go in.
[In] the beginning, you’re going to get a million messages and it’s the most amazing. It’s the best thing [knowing] you have so much support.
When they bring you gifts, really appreciate that. They are taking the time to do that. Take them up on [what they’re offering to do]. “Can I bring you dinner?” “Can I drive you somewhere?” “Can I bring groceries?” “Yeah, you can bring me groceries.” “Yeah, I can’t get out of bed today.” “Yeah, I would love to watch a Netflix movie with you on Zoom.” There [are] so many things people want to do. Let them help you.
If you know something’s wrong with your body, you have to say something. I could have been nauseous for months and months and just not have said something. You have to be a self-advocate.
Get your blood work taken. See your doctor once a year. Go to your dentist. Go to all your appointments because you could never know what could happen to you. I see a wellness doctor. I get my blood work taken all the time and I wish it would have shown up in my blood work. I could have had it be stage one cancer and that would have been amazing. I wouldn’t have had to be in the hospital and I would have done treatment sooner. But since I didn’t have any of these signs and thought it was anxiety, that bruising was normal and night sweating, I end up being stage 4.
Listen to your doctors. Try and make friends if you can. Have a support system, accept people, and let people in. This is your journey and however you want to choose to have it, you’re able to do it. At the end of the day, it’s your journey and you’re going to have to figure it out. It is what it is.


Inspired by Paige's story?
Share your story, too!
Diffuse Large B-Cell Lymphoma Stories
Erin R., Diffuse Large B-Cell Lymphoma (DLBCL) & Burkitt Lymphoma, Stage 4
Symptoms: Lower abdominal pain, blood in stool, loss of appetite
Treatments: Chemotherapy (Part A: R-CHOP, HCVAD, Part B: Methotrexate, Rituxan, Cytarabine)
Jonathan S., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Severe shoulder pain
Treatments: R-CHOP chemotherapy, methotrexate, focal radiation, autologous stem cell transplant
Kris W., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Pain in the side of the abdomen
Treatment: R-CHOP chemotherapy
Luis V., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Persistent cough, fatigue, unexplained weight loss
Treatment: Chemotherapy (R-CHOP and methotrexate)
Nina L., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Hip and lower extremities pain, night sweats
Treatment: Chemotherapy (R-CHOP)
Richard P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Relapse Symptoms: Swelling in leg, leg edema Treatments: R-CHOP chemotherapy, clinical trial (venetoclax-selinexor)