Marti’s Stage 3 Multiple Myeloma Story
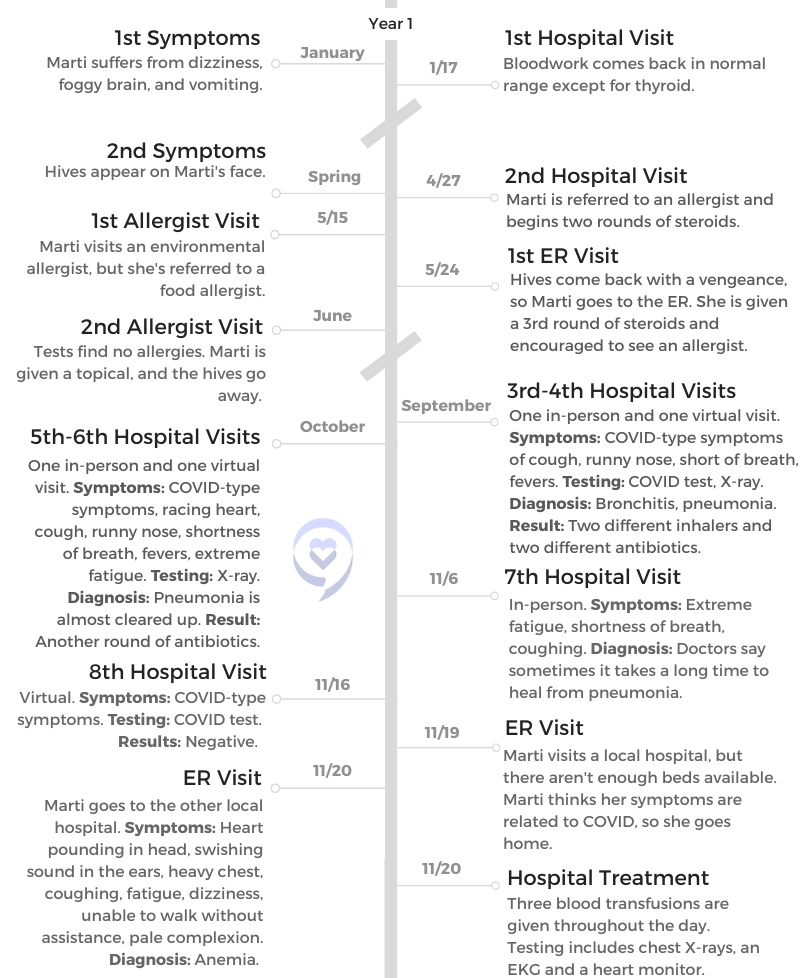
Marti’s first multiple myeloma symptoms started at the beginning of the pandemic. After visiting doctors and allergists, she had no answers for her extreme fatigue, vomiting and hives.
Marti was desperate for relief. Finally, an ER visit led to a diagnosis. Marti then underwent chemotherapy and a stem cell transplant.
Read Marti’s incredible story, including the struggle to get diagnosed, navigating hospital visits during COVID, chemotherapy and side effects. Marti also discusses her stem cell transplant, hair loss and staying optimistic while living with cancer. Thank you for sharing your story, Marti!
- Name: Marti P.
- Diagnosis:
- Multiple myeloma, stage 3
- 1st Symptoms:
- Dizziness
- Fatigue
- Hives
- Vomiting
- Treatment
- 3-drug regimen
- bortezomib (Velcade)
- daratumumab (Darzalex)
- lenalidomide (Revlimid)
- Stem cell transplant
- Maintenance therapy (ongoing)
- 3-drug regimen
- VIDEO: Multiple Myeloma Symptoms
- Introduction and 1st Multiple Myeloma Symptoms
- Doctor's Visits
- The Diagnosis and Support
- VIDEO: 1st-Line Multiple Myeloma Treatment
- VIDEO: Stem Cell Transplant
- VIDEO: Living with Multiple Myeloma
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
VIDEO: Multiple Myeloma Symptoms
Introduction and 1st Multiple Myeloma Symptoms
Introduction: Tell us about yourself
I am a wife. I’ll be celebrating 33 years in September. I am a mom of 2 daughters. I have 7 grandchildren, from the ages of 10 to all the way down to 6 months. I have a full plate with my family, and I love my grandkids. One of my favorite pastimes is to spend time with them and my daughters.
What were your 1st multiple myeloma symptoms?
Dizziness and fatigue
Some of the symptoms I ended up having were extreme dizziness and some fogginess. I think at times I had some confusion and just all in all fatigue. That fatigue was always there.
Then I started having some episodes of vomiting, and all of a sudden the whole room would start spinning out of the blue. I’d have to run to the bathroom. There were a few times I had to leave work, and then I just had an extreme migraine with it.

Some of the symptoms I ended up having were extreme dizziness and some fogginess…That fatigue was always there.
I didn’t know what was going on. It started to happen weekly. When it happened every week for 3 or 4 weeks, I decided I was going to make a doctor’s appointment because something was off for sure.
That is when I had my first blood draw just to see what was going on and to see if there was anything unusual. There wasn’t, except that my thyroid was just a little bit off. We decided to go ahead and wait on taking any medication and then just kind of went back to regular life. I still felt all of those symptoms even though the vomiting had stopped.
Hives
My next symptom that I had was the hives, and that started more in the spring. I had them all over my forehead, kind of in my eyes and all over my face. That was the only place I had hives. I thought, “Oh, my goodness, what is going on here?”
Again, I went back to the doctor, and I asked her if that could be a result of my thyroid. She said, “No, you probably are allergic to something. Let’s go ahead and have you see an allergist.”
She gave me steroids and all of the stuff for hives and sent me on my merry way. All of that kind of cleared up. I got a referral to an allergist and kind of delayed that because the hives would come and go. They wouldn’t stay consistent.
They came back, and so at that time I’m like, “Okay, I’m going to go to this allergist.” I went to that allergist, and he ended up being an environmental allergist instead of a food allergist. I was thinking I must have some sort of food allergy.
What was the timeline of your multiple myeloma symptoms?
This was kind of in the spring and throughout the summer. I did have one trip to the emergency room with my hives because they had gotten so bad.
The doctor said, “I am not an allergist,” and he ended up sending me home. I understand that. I said, “But I need some sort of relief, and the only way I can get relief is by coming to you because it’s a Sunday.”
We went ahead and did that. They kept telling me I had COVID, but the COVID-type symptoms did not start until the end of the fall.
It was very, very frustrating. It actually made me want to not go back to the doctor. It made me just think, “Oh, it’s just in my head. I will get better. I’m going to feel better. I’m just going to rest because I’m just so tired. I’m so fatigued. If only I could just get enough rest.”

At that point, I just wanted reassurance that I was going to get better.
Doctor’s Visits
How did you navigate in-personal and virtual doctor’s visits?
With COVID, most of us usually went to the Zoom meetings for the doctors if we went. My first meeting was a Zoom meeting with the doctor, and she diagnosed me with bronchitis.
I was like, “Oh yeah, this makes sense. I kind of feel like that’s what I have.” In fact, that’s what I told her: “I think I just have bronchitis. I’ve had that before. That’s what it feels like.”
I went on the antibiotic, but I did not feel better after the antibiotic and the inhaler. The next time, I went to an urgent care and decided to see them in person. I told them my symptoms, and at that time, that’s when I started having the racing heart and the the erratic heart rate.
They asked, “Are you anxious about anything?”
“Well, I guess I am. I just don’t feel good, you know? That’s why I’m here.” That’s when they did X-rays, and they said, “You have pneumonia, not bronchitis.”
They gave me another round of antibiotics and a new inhaler that I could have more frequently. I would contact them about once a week, and I would either go in or do a virtual visit with them. At that point, I just wanted reassurance that I was going to get better.
That’s why I kept in communication with them. There was also concern again about it being COVID and the possibility of me spreading COVID. That’s how I kept on going back and forth. I did that several times. I think I had maybe 6 visits.
When did you know you were experiencing something more serious?
I knew probably at the very start of November. I didn’t end up going to the hospital until the end of November. The very first part of November, I’m thinking, “Why am I not getting better, and why am I so fatigued?”
Toward the beginning of November, I’d be at work and then go for my lunch hour. Instead of eating my lunch, I literally would sleep in my vehicle because I was so exhausted.
That’s when I knew. Why do I feel like I cannot function right now? The bottom line is I knew that I wasn’t functioning very well.
We had some family things that had happened in the beginning part of November that also made me think, “Oh, this is probably just stress. I’m just dealing with a lot of stress because of our family issue that we were dealing with. I’m just fatigued because maybe I’m not sleeping the best at night. I got this on my mind. I got to get this off of my mind.” That was kind of the issue that I kept on having.
Visiting the ER
Finally, I told my husband, “Michael, something is really wrong. I’m thinking that maybe I need to go to the ER.”
He was like, “Okay, let’s go to the ER.”
Unfortunately, at that time, he ended up having COVID. We had been socially distancing for 1 or 2 days already. His brother ended up taking me to the ER. I don’t really want to go into what happened at the ER, but there was only 1 bed left because of COVID.

The ambulance came, and I was like, “I’m never going to get into the hospital.” At that point, I decided I was just going to leave and go home. I had that opportunity because I hadn’t checked in yet.
I was waiting outside, waiting for them to allow me to go in because those restrictions were so tight and they had so many cases at that time. I ended up just saying, “I’m going to go on home.”
My brother-in-law said, “Do you want me to take you to the other hospital that’s next to us?”
At that point, I was just angry. I was angry and frustrated. I said, “I just want to go home and eat, and then I’m going to go to bed.”
That morning I had told him, ‘Something is terribly wrong, and I do feel like I am dying.’
When did the doctors realize this was more than COVID?
My husband is very good friends with the hospital’s doctor in our area. The morning that I went into the hospital, he called that doctor because I was a gray ash color.
They were good friends, and he said, “Something is wrong with my wife. I think my wife is dying. I’m going to bring her in.”
At that point, I went ahead. That morning I had told him, “Something is terribly wrong, and I do feel like I am dying. Something is terribly wrong. I need you to mask up even though you have COVID, and I need you to take me to the ER because I’m not going by ambulance.” He did, and he stayed in contact with that doctor.
Honestly, if I have to say I had special treatment when I arrived at the hospital, I did. I did not have to sit. I had people in my room constantly. They were on top of it.
That’s when I definitely suspected that it was cancer.
The doctors were in and out during that time period. I did not have to wait very long. My blood work was done. Everything was just right in order. I was very, very fortunate for that.
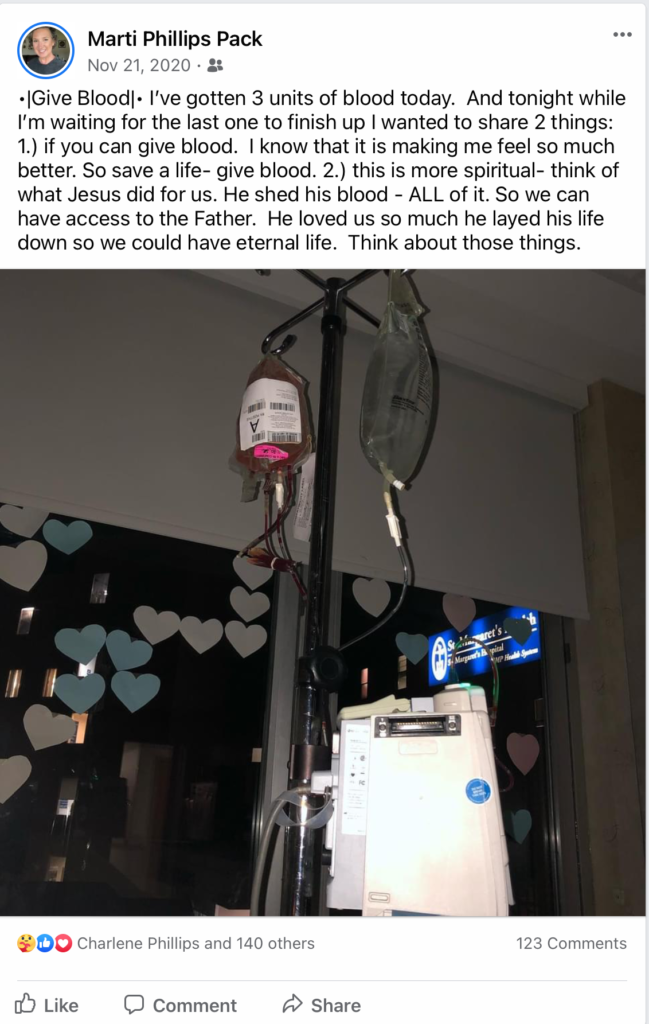
Within the first half hour, they knew that I was anemic and that I was bleeding from somewhere internally. That is when I did my first blood transfusion in the ER, and then they wanted to do another one.
At that point, my hemoglobin was at 5.8, which is rather low. I did get special treatment at the hospital, which I was really thankful for.
When did you think it might be cancer?
When it entered my mind was right after the ultrasound, because there was not anything that pointed to me having a bleeding source at that time. I am not a person who ever has stomach issues. They had been prepping me for maybe a colonoscopy and an endoscopy, but I didn’t have any stomach issues.
When the ultrasound came back and everything was normal, I kind of knew, especially when they said they were going to do a bone marrow biopsy. That’s when I definitely suspected that it was cancer.
In fact, my oldest daughter and I finally had an open conversation. She said, “Hey, Mom, do you think it’s cancer?”
I said, “I think it is. I don’t know what kind of cancer. It’s the elephant in the room. I’m just going to be a straight shooter and ask them about it.”
That’s how we kind of started down that path that it had to be cancer.
I was on the phone talking to my daughter because again, it’s COVID. At that time, the regulations were no visitors at all, especially because I was a close-contact exposure.
They were treating me as a close-contact exposure since my husband had it. Even though we had been distancing ourselves and we masked going into the hospital, I still was exposed at that point.
The Diagnosis and Support
How did you approach talking to your family about cancer?
I usually talk to my daughter every day. When I started not getting better, she was getting very concerned. She was the one who asked, “Mom, did you go in and get COVID tested?”
She’s a nurse, and so she’s just very proactive in the medical field. She just wanted me to be cautious. When I wasn’t getting better, she was getting concerned. Every time I would talk to her on the phone, I’d have a coughing attack, get short of breath, or have to let her go because I needed to lie down.
She said, “Mom, something is just not right. You need to go to the doctor and take care of yourself.” She knew that I had been going to the doctor pretty much every week or every 2 weeks at that point and not getting an end result.
At that point, it was almost an easy conversation. It was a place where it was like, “Yeah, we need to look at this because something is definitely not correct.” Having that conversation was a little bit harder with my husband.
Help from the hospital staff
Once I was diagnosed, the nurse practitioner was going to contact my daughter. Then the doctor, who’s my husband’s good friend, was going to contact my husband. He wanted to have his payment plan in place before he contacted my husband.
I was still kind of processing, so I wanted them to share that news. It ended up that the nurse practitioner called my daughter and had a good conversation, but the doctor hadn’t called Michael yet.
I ended up telling him, and that was where we both cried. He also usually responds in anger. That’s his first response, so he was like, “What are you talking about?” He was just mad. He had COVID, and he was feeling miserable.
I can understand why he was so angry, but I think he was just angry at everything. It had been a rough couple of months there before diagnosis.
Can you describe the moment you received the diagnosis?
The hardest was just being by myself. When you hear that news, you want to have someone there to hold your hand. I just remember feeling very alone. Also, when you don’t feel good, you just can’t get it together. Both the doctor and the nurse practitioner were in the room.
Benadryl reaction
I’m going to rewind real quick. When I went to have my CAT scan, I had a little issue with the dye, the drink that they gave me, and this is how we figured out that I had multiple myeloma. It’s a pretty important factor. I was starting to have some issues with the drink, and I started feeling hives and itchy all around my mouth.

The nurse practitioner decided, “We don’t have to be in a hurry to get this CAT scan with the dye. Let’s go ahead and back off. Let’s give you some Benadryl and then give that a little bit of time to settle in your system. Then we’ll take you on down, and we’ll get the CAT scan.”
They did the first shot of Benadryl, and I reacted fine. The second shot of Benadryl basically caused me to not be able to breathe. It was just like everything closed in on me.
They did a code. I did not code or anything, but they called a code just to be on the safe side. They just took care of me, and everything was fine.
I was finally situated back into my room after all of that happened. The first thing I did once I was settled was I Googled — and I know that’s the worst thing to do — a Benadryl reaction to see what came up, and it said cancer. That reaction was specific to a blood cancer.
Even though I got the diagnosis myself, everyone was still very much a part of that conversation, even though it wasn’t all at once.
Receiving the diagnosis
When they came in, it was the doctor and the nurse practitioner. At that time, we had become very close. My daughter had a relationship with the nurse practitioner. My husband had a relationship with the hospitalist. There was constant communication, I think, behind the scenes with my husband and my daughter talking to them, plus me.
Even though I got the diagnosis myself, everyone was still very much a part of that conversation, even though it wasn’t all at once. Everybody was in the loop. Everybody was a part of that and made me feel like I was not so alone at that point.
Then they went ahead and had that bone marrow biopsy. They had the preliminaries, and then that’s when they said it. That was 48 hours, and usually it takes about 4 days for them to get the full report. At that point, they could do a preliminary, and it was multiple myeloma.
They did come in and tell me. Like I said, the hardest part was just being alone and not being able to hold my family’s hand. Later on, I was able to ask questions and process things with them. The human side of things is that I bawled like a baby. It was so emotional.
At the same time, I was thinking, “What does this mean? I have never even heard of this blood cancer. Never even heard of it.” I’ve heard of leukemia, and I’ve heard of lymphoma, and I’ve heard of non-Hodgkin’s. But I had never heard of multiple myeloma.
»MORE: Reacting to a cancer diagnosis
How did you approach sharing the diagnosis with everyone in your life?

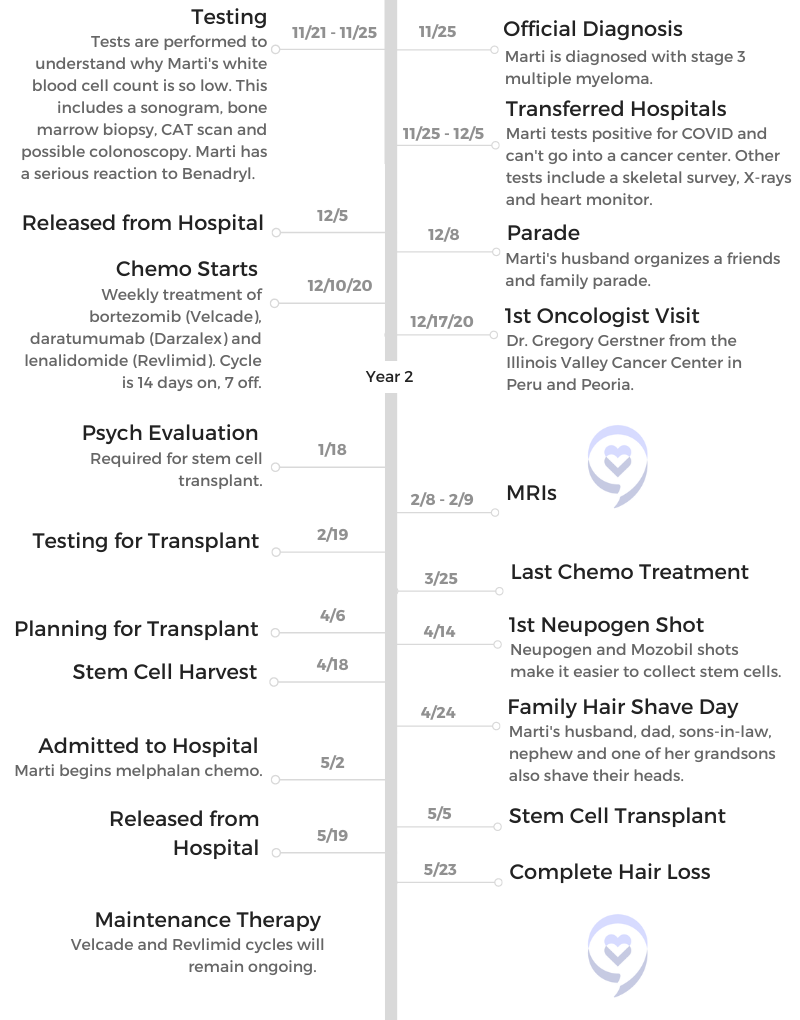
Social media is a powerful tool to get the communication out to people. We have a really strong faith community. The first thing I did was share a social media post saying that I am in the hospital and had to get some blood, and we don’t know what the bleeding source is. We instantly had amazing response from people.
Of course we told our immediate family first, like our parents. Each one of us ended up doing that. Then when I posted that, that was when we were able to tell our friends and our family. They knew at that point that I was in the hospital, and I told them I would keep them posted on what was going on.
Social media for us was a big deal, actually. It was a big deal to get people praying, and it was a big deal to get people informed with what was going on.
Were there any questions you wish you would have asked?
That’s a tough question because I was very, very sick at the time with all of these other symptoms. I had the dizziness and this swooshing in my ear. When I was talking to people, I was hearing the squishiness all the time.
I was in a place where I was not able to walk because I felt very dizzy and faint. That is because I didn’t have enough blood. I was very low on blood with anemia.
It’s hard to say, “This is what I wish I would have done at that point.” I was just thinking, “I wish I would feel better.” Even though I had this diagnosis on my plate, I felt alone. I was struggling in that aspect on what I was going to do and say and ask.
It’s hard to say, ‘This is what I wish I would have done at that point.’
Marti P.

My daughter gave me some of the questions to ask, and then I would speak those into my phone as a reminder. When they came back in, I would remember to ask them, because I would forget very easily.
She was the one that was asking. The reason why I had the nurse practitioner call my daughter is so that she could ask all the questions, and then later on we could talk about it when I felt better.
VIDEO: 1st-Line Multiple Myeloma Treatment

Multiple Myeloma Treatment Regimen
Did you consider getting a second opinion?
I ended up going to the bigger hospital. He was a hematologist-oncologist. At that point, I was so, so sick that it wasn’t even in my mind to get a second opinion. I just wanted to get better. I just wanted to get to a place where I felt better. That was where I was. For me, there really wasn’t any time to process.
Honestly, at the time when I went into the hospital, I really felt that I was dying in every way. When they were getting to the treatment part, I think that was more of what I was looking for. I just wanted to feel better, and I had felt so lousy for so long that I just wanted to feel better.
If he said he could make me feel better, I was just going to trust him. At that point, I never thought about getting a second opinion at all. I just wanted to be treated so I could get better.
How did COVID impact your treatment?
I was on the oncology floor. Because I kept on having chest pains, they were like, “Let’s just test her one more time for COVID.” It had been several days since I had been tested, so I did it. It was 7 days after I had been exposed.
Immediately, I had to go into quarantine. They put me on the COVID floor to finish my treatments, because once you start your treatment, you have to do it on Day 1, Day 3, Day 5 and Day 8. All of that would have put me where I wouldn’t have been able to get treatment, and therefore I wouldn’t have gotten better. Their solution was, “We’re just going to keep you.” So they did.
I started to feel more like myself physically, where before it was hard for me to function in everyday life.
What was the multiple myeloma treatment regimen?
For the first one, they did it as an IV treatment. At that point, I didn’t care what they were giving me. Once I was released and I was better from COVID, I could go to the cancer center.
I did a weekly shot and then Velcade. They gave me Zometa also for my bones. Then I did a couple of rounds of the Velcade. I think I did one cycle of Velcade, which is 4 weeks, and then I started what they call “dar,” or daratumumab.
That one, I went down to the bigger cancer center because they had a bigger staff. For the first IV treatment of that, usually they just like to keep a very close eye on you so that you don’t have any reactions.
I am one of those people that did have a reaction to it, so I ended up having to spend 2 treatments down there. It was 2 weeks in a row in the bigger hospital, with an 8-hour IV both times of that. That was probably the most effective in bringing my numbers back into balance.
Everything was working. As I went through treatment, I have to say for me personally, I started to feel better. Because I had been so, so sick, I just started to feel better. I started to have more energy. I started to feel more like myself physically, where before it was hard for me to function in everyday life. It had been rough there for several months.
Side Effects
What were your side effects from the multiple myeloma treatment?
My treatment day was on Thursday. I would go in, and I would get the Darzalex and Velcade shot. They also did steroids on that day. If it was time for the Zometa, that was the day that I would do the Zometa.
Usually Friday with the steroids, I’d be pretty wound and ready to go almost all evening with not a lot of sleep that night into Friday. Usually by Friday night, I would start getting neck pain, and it just felt like everything was swollen. It would start in my neck.
How I resolved that was I just used a heating pad. They advised Claritin because it’s an anti-inflammatory, and so I took Claritin and Tylenol. Those were the things that helped my side effects.
»MORE: Cancer Treatment Side Effects
Taking time to rest
I would have those side effects until about Sunday. There was fatigue and all the aches and the pains in your body.
Usually one of those days, mainly Sunday, would be just a rest day for me, and I did not feel bad at all about it. I would just lie and watch my iPad. I really wouldn’t have to think, but I could just let my body rest.
The other side effects didn’t really happen. I went through treatment from November all the way until February. In February, my white counts began to drop, and then fatigue came with that. Back to the extreme fatigue, not just a little bit of the fatigue from the treatments. It was more where I would sometimes be down for a few days because of the fatigue.
At that point, we stopped all treatment for my body to rest for a little bit and regroup. I would encourage people to know that that’s kind of normal, and it’s not anything to be concerned about. My numbers were really good at that time, too, so it was okay for me to take a rest.
What advice would you give for other patients?
I want to encourage people to not feel guilt or shame for lying down and resting. Your body takes a lot of your energy to heal. If you can, get to a place mentally where you say, “You know what, this is what it is. My job right now is to heal, and it is what I’m supposed to be doing right now.” For me, that really helped.
I’m also an empty nester. I do not have small children in my home, and I don’t have to have that constant care of children. For me, that was something that I could do. I’ve seen others where they are parents of small children, and they’re not always able to do that.
If a family member could come alongside or a really good friend for those few hours, just say, “I need a little bit of time.” I hope that people have that support system to be able to do that. I hope that they do. It is definitely important not to have the guilt or the shame for lying down and letting your body heal.
How did the genetic factor of 1q affect your treatment?
The genetic factor just made me have to change medication. I think I was on an oral medication at first, and it made me switch over to Velcade, to the shot, because it was more effective with that genetic issue. That was really just the change.
I was still going to have to be on Revlimid, and I did 14 days on and 7 days off with the Revlimid. Otherwise, they still would have done all the treatments that they did. They just changed that one oral medication to be able to fight the cancer better.
Every week I just had my blood levels drawn. It was mainly the CBC, the normal blood work, just to make sure that my white counts, my platelets and my hemoglobin were normal. Once a month, they would do the light chains, the bigger draws of blood.
»MORE: Genetic Testing for Cancer
VIDEO: Stem Cell Transplant
Stem Cell Transplant Process and Doctor-Patient Relationship
When did your doctor discuss a stem cell transplant?
He started dropping things shortly after we got out of the hospital about the stem cell transplant, because those who have them have such a better result and a better quality of life. He started talking about that pretty quickly into treatment.
By that time, I really liked my doctor. I had a really good relationship with him, which I think is really important. I trust my doctor, and because I had started feeling so much better, that helps with that trust.
I didn’t really want to go to a new doctor. I didn’t want to have to do anything different. He said, “Now if you want to get another opinion or anything like that, do it.” I watched my myeloma groups on Facebook and had done my own research about myeloma, and he was doing things that I would do anywhere, except I had that relationship with my doctor.
For me, it’s really important to have a good relationship with the people you’re working closely with. I wanted to keep that relationship. By the end of January, we made the decision that we were going to do the stem cell transplant.
How important is a good relationship with your doctor?
For my husband and I, we kind of built a friendship with them. Not that they know everything about our family or we know about their family, but there is a little bit of that friendship there.
I’m a list maker, so I always have a list of questions for him. He’s always very patient with me when I ask him the questions. He really takes the time to answer those questions. Even if I feel like I’ve asked something stupid, he’s still okay with that because I have no clue on what any of this is.
It’s all a new journey for me, and he’s maybe dealt with hundreds of patients. There’s only one me. Also, just being appreciative of their care goes a long way in relationships. We’re appreciative of his knowledge, the care that he’s given, and the care that the rest of the staff has given us there. That’s what it means to me.
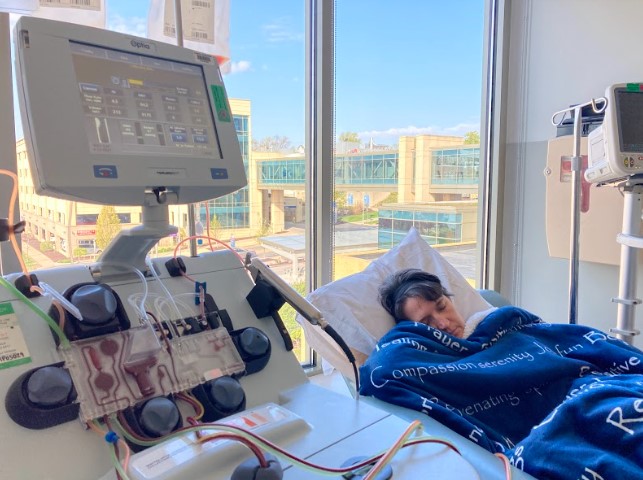
What is the stem cell transplant process?
Usually, they do a bunch of pre-testing, and that involves your heart, your lungs, your breathing, X-rays, EKGs, all of that. You do all of the pre-testing. You also see a psychologist because they want to make sure you’re in a good mental place going into the transplant. I had all of that pre-testing done.
After the pre-testing, as soon as you’re done with your cycles of chemo that they give you — I believe I went through 5 cycles altogether — they prepare you for the Neupogen. That makes all of your stem cells grow, and then they give you a shot called Mozobil.
Mozobil brings them up to the blood so that they can just take it out like kidney dialysis. They give your body a little bit of a break after you’ve had the Neupogen shots and the Mobozil and your collection.
Your doctor knows about how many stem cells they want for that collection, and they’re able to count all those cells and let you know. That’s a series of days that you go. I went from Sunday to Thursday for my collection.
After collection, you get a little bit of a break, and then you go in and are admitted to the hospital. The first 2 days you’re in the hospital, you have the melphalan for the stem cell. Usually the third day, which they call day zero, is when they give you your stem cells back.
»MORE: Stem cell transplant FAQ

Stem Cell Transplant Side Effects
What was the recovery process for the stem cell transplant?
I was pretty fortunate. I was only in the hospital about 19 days altogether, and then I came home to recover. That was pretty uneventful, too. One time I had to go in to get some fluids because I was a little bit dehydrated. I always felt like I was dehydrated. That was probably the hardest part besides the fatigue.
Then you do have muscle aches. You do have some side effects from that melphalan chemo. That’s pretty hard on your body, for sure. Not only do you get the hair loss, but you also have a lot of aches and pains and digestive issues.
It’s just really rough. I still had some of those in coming home. For 2 to 3 weeks after I got home, I had the symptoms from the chemo.

What helped with the side effects?
They prescribed nausea medications for the nausea and for the diarrhea. I took them whenever I needed them. It was a great help, and so I definitely recommend those. Because I didn’t feel like eating, I was just trying to find food that I could eat that was easy and tasted good.
I wouldn’t be too picky about what I ate. I wasn’t trying to be too healthy, even though I did try to keep a lot of protein. I also did a lot of protein shakes. That definitely helped a lot during that time.
Get calories in because without the calories, you can’t heal. You need those calories so that you can heal, and then you’ll have more energy. I also got some powdered electrolytes that I could put in water.
That was kind of a game changer for me without having the IV to be able to have that liquid hydration. That really helped me. I still take some of that about every other day, and that helps me have the energy that I need.
Now, 3 months later, are you still experiencing side effects?
I’m still dealing with that. I think my expectations were that I was going to bounce back right away, and I haven’t. That part is hard.
I still have not returned back to work either. I’m hoping to be able to return back to work by December, but I will be almost off of work for a whole year because I’ve been off since I went into the hospital. I went on FMLA right after because I didn’t know how treatments were going to be and all of that.
Actually, at the time I couldn’t drive. Like I said, I had been very, very ill for several months. I was just not able to go. I was not functioning.
»MORE: Cancer Treatment Side Effects
Experiencing Hair Loss
How did you approach losing your hair?
That was the hardest part, I think. It was very, very difficult when they told me that I was going to lose my hair. I think sometimes it’s maybe your safety net or your security blanket.
When I was first diagnosed, I decided, “Well, if I have to go through this and if I have to do this, I’m at least going to do it with dignity and grace.” I started thinking of ways that I could maybe cope with what I was going to go through in a positive way.
I just simply decided I’m going to go shorter and shorter and shorter. Every month I would go in, get a haircut and post it on social media. It was just your family and friends giving you that affirmation that it’s going to be okay. It’s going to be okay, and it’s going to be short lived.
»MORE: Hair Loss and Regrowth After Chemotherapy
The big shave
I think I did that in December, January, February and March, and then finally we decided to go ahead and do the big shave. My husband, my dad, both my sons-in-law, my nephew and one of my grandsons decided to do a shave for me all on the same day.

We kind of made it more of a celebration instead of a loss. For us, that was how I was able to cope. At that point, it was just such a relief to know that I had so much support.
I would post it on social media. There were even a few people that would message me and say, “Hey, I just wanted to let you know, today I shaved my head for you.” Then they would send me a picture.
One of my classmates that I went to school with, he said, “I’ve been struggling for years because I’ve had to shave my head because I was half bald and it would come in funny. But today I’m shaving it for you.”
Just the community support that I had while I went through that process made it really special for me, and I’m really grateful that I did that.

It’s just a season, and you’ll get through that season. It’s hair; it’ll grow back.
Right now, I’ve chosen not to have a wig. I use headbands because it’s so hot here for summer that I just didn’t want to deal with the wig. My hair is finally starting to come back. I decided I was just going to embrace it and know that it’s just a season. It’s just a season, and you’ll get through that season. It’s hair; it’ll grow back.
Do you have any styling tips for others experiencing hair loss?
I found some makeup that I liked, and I probably spend a lot more money on makeup than I ever did. Then I do headbands, and then I do ball caps or just some cute hats that I have found. For me, that’s what’s worked.
In the winter, I know I’ll do more beanies, and I’ll do heavier hats because my hair grows pretty slow. I’m almost at 3 months, and I’m just starting to get the peekaboo. It’s not growing very fast. Just find something that makes you feel good.
Sometimes we have to embrace the hard to get through it, and it makes it a lot easier to go through it.
Like I said, I wanted to have grace and dignity. I try to make sure that I get up every day. I get my shower in. I get myself ready for the day, just like I was going to go to work, because it makes me feel good. It makes me feel normal when I’m doing normal things. I just wanted to do that.
It does stink. Cancer stinks all the way around. But I think the bottom line is sometimes we have to embrace the hard to get through it, and it makes it a lot easier to go through it.
VIDEO: Living with Multiple Myeloma
Maintenance Therapy
What is the follow-up for a stem cell transplant?
Maintenance therapy for me requires 2 cycles of the Velcade, which is 8 weeks of a weekly shot, and then I’ll do the Revlimid at 15 milligrams. Then starting in October, they’ll reduce the Revlimid milligrams. I’m not sure where they’ll reduce that to, whether it’ll be 10 or 5.
Then we’ll go to only having the Velcade shot once a month. I will do the Revlimid and the Velcade until I get a break. Then I’ll get a break, and then we’ll start up again. Since there’s no cure for multiple myeloma, you’re usually on maintenance for the rest of your life.

Have you processed what your future looks like with maintenance therapy?
That is something I have been processing. I don’t think I’m completely through processing what that’s going to look like because everything is still so brand new. I don’t have the years under my belt. I only have just the last few months under my belt.
I do kind of look at it being more like just a chronic illness, whether it’d be like diabetes or someone who had heart disease and has to be on certain heart medications. For me, that’s how I am viewing that and coping with that, knowing that it’s going to be a lifelong thing.
I don’t have to be alone, and you don’t have to be alone with this diagnosis. We’ll just take it one day at a time.
It doesn’t mean it’s the end either. It doesn’t mean that I’m only going to have 5 or 10 years left. There are people that have had a longevity of life. I still strongly believe that God, when he’s done with what I’m supposed to do here on Earth, then that’s when I’ll go on home.
I’m not looking at it as a death sentence, so to speak. I don’t want it to be a death sentence. I want it to be where I can encourage people while I’m here, and we can walk through it together. I don’t have to be alone, and you don’t have to be alone with this diagnosis. We’ll just take it one day at a time.
Support Systems
The importance of staying optimistic while living with multiple myeloma
I think, again, go back to that communication and that relationship with your doctor. Keep going and keep believing that there is going to be a cure. I think probably the biggest message is never give up. Just never give up. Just keep at it.
Your body will know when enough is enough, but just never give up. Keep going at it and putting one foot in front of the other and taking it one day at a time. Draw strength from others. For me, I draw strength from God.
I think I just want people to know that they’re not alone in whatever they’re going through, whether it’s cancer or whether they’re struggling with things with their family. It doesn’t have to just be cancer.
You don’t have to be alone in what you’re going through. You don’t have to feel like you’re on an island. You can have a strong support system, and you can reach out to people. If you’re too afraid to reach out to people, then hopefully people will reach out to you.
I think never giving up and then just having that support system, that’s where my emotions are coming from. Having both of those things has meant the world to me and my journey, knowing that people were out there caring for us and loving on us and being the kind of human that I want to be.
What support from your friends and family was the most helpful?
I still am getting cards from people in the mail, and sometimes there’s some financial support in those cards. My husband’s place of work did a fundraiser for us. That was a blessing. I had another friend that did a GoFundMe, and that was a blessing.
This is the thing that has probably meant the most to me. The weekend after I got out of the hospital — and you couldn’t get a whole bunch of people together because of COVID — my husband organized a parade for me. I sat in the garage out in our driveway and wrapped up in a heating blanket so I could stay warm because it was December.
There were people that just came out of nowhere. I didn’t even realize we had that many friends, but there were like 100 cars in this parade. The police had closed off our block.

There were people that just came out of nowhere, people I hadn’t seen for years that sacrificed their Saturday just to drop off a card and say, “Hey, I’m thinking of you, and I’m praying for you.”
It was probably the most memorable thing out of all that has happened in the last few months. That’s probably been the thing that has stood out the most.
How do you navigate the financial aspects of cancer?
There are also scholarships that you can get from wherever you do treatment at your cancer facility. They have someone that you can reach out to in their finance department, and they’ll help find you scholarships. We’ve had some scholarships that have come through. There are also scholarships available to pay for your medications and for any type of chemo that you have.
I went through that, and I overcame that.
Most of your cancer clinics will be able to help you with that, and you’ll be able to do that. You can even connect with your city if you have issues with power bills. There’s just a lot of scholarships out there that people donate so that the cancer patient doesn’t have to stress about the finances.
»MORE: Financial Assistance for Cancer Patients
What is the importance of sharing your story, and what is the importance of people listening?
I think it’s important for you to share your story because it helps with healing. It helps not only give it a voice, but to say, “I went through that.” For me, it’s also, “I went through that, and I overcame that.” That’s why it’s really important. Also, to share my faith with people. I think that for me, it’s really important to share my faith.
The reason why it’s important for you to hear it is because I have watched some people go through maybe not cancer, but maybe another illness. I really didn’t understand. As I’ve walked the journey and not only experienced it but also heard other people’s story, it shows me where I can help. Maybe I need to be that person to drop a card in the mail to someone and give them a gift card for food or for a restaurant, like people have done for me.
I think it’s important for you to hear so that you know where you can help and where you can meet a need. There are plenty of needs out there, especially when it comes to cancer patients. It’s important to also be sensitive to the other people that have a chronic illness.
»MORE: How to Help Someone with Cancer

Inspired by Marti's story?
Share your story, too!
Other Active Multiple Myeloma Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...




