Living with Prefibrotic Myelofibrosis: A Father’s Journey Through Pain, Perseverance, and Purpose
Neal, a proud father to his four daughters, faced baffling symptoms — persistent upper rib pain, night sweats, relentless itching, and overwhelming fatigue. Initially misdiagnosed, he navigated a maze of specialists and medications, which only worsened his health. His determination paid off when a rheumatologist studied his lab results and knew where to send him. Neal was referred to a hematologist oncologist, who finally uncovered the truth: a rare blood cancer, essential thrombocythemia, which later progressed to prefibrotic myelofibrosis.
Interviewed by: Stephanie Chuang
Edited by: Chris Sanchez

Living with prefibrotic myelofibrosis is no small feat. Neal describes his pain as “pressurized,” often incapacitating, affecting his mental health, and challenging his role as a parent. Yet, it’s his daughters who anchor him, fueling his perseverance. His candid reflections reveal the emotional weight of not feeling heard by medical professionals and the relief that comes when the right doctor finally listens.
Mental health challenges have been central to Neal’s experience. The anxiety and frustration of not being understood were as draining as his physical symptoms. But receiving an accurate diagnosis was just as transformative — it validated his suffering and restored his self-confidence.
Neal’s proactive approach to his health is inspiring. His potential involvement in a clinical trial offers renewed hope, not just for him but for others with prefibrotic myelofibrosis. His advice? Trust your instincts, advocate for yourself, and never settle for medical indifference.
Read this story and watch Neal’s video for more on:
- How his parenting inspired his fight for answers.
- The symptom that nearly led to an amputation.
- Why one doctor’s words made Neal’s appointment the “best one” of his life.
- How clinical trials revived his hope.
- The surprising link between Neal’s mental health and his rare diagnosis.
- Name:
- Neal H.
- Age at Diagnosis:
- 31
- Diagnosis:
- Prefibrotic Myelofibrosis
- Symptoms:
- Night sweats
- Severe itching
- Abdominal pain
- Bone pain
- Treatments:
- Tumor necrosis factor blocker
- Chemotherapy
- Targeted therapy
- Testosterone replacement therapy


Thank you to Karyopharm for supporting our patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Explore the resources available to you — they’re out there, even if you don’t live in a big city.
Don’t be afraid to get help. You don’t have to fight this alone.
Introduction
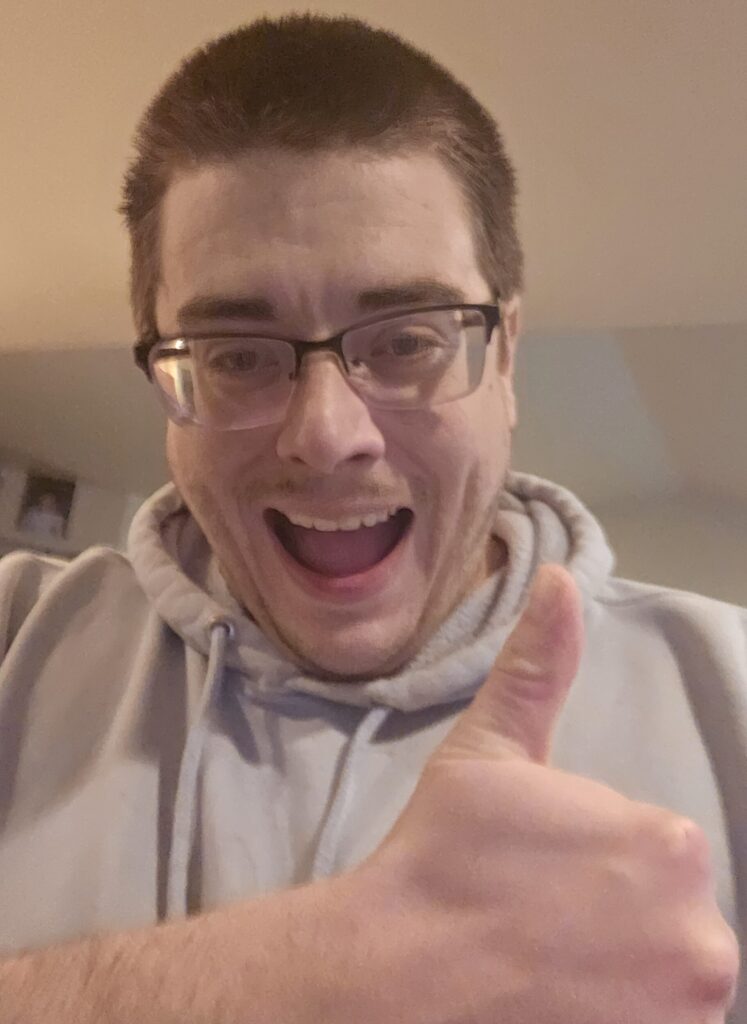
Hi, I’m Neal. I’m 35, a father of four daughters. My partner and caregiver, Kayla, has been with me for the past seven years.
I’m the life of the party, and I’m always very animated. I’m a unique person — I’m authentically myself, and I wouldn’t change for anyone. And most people who know me would say the same thing.


The Long Journey to My Diagnosis
It all started with what we thought were bowel issues like irritable bowel syndrome, and my left quadrant area, the upper rib area, started hurting and feeling congested.
We did a colonoscopy and an endoscopy, and they found nothing. But the pain persisted. Then I began to have bad night sweats, and I started to itch a lot too.
I consulted a neurologist and rheumatologist. They thought I might have rheumatoid arthritis, and so they put me on high-dose prednisone to treat it. But then I got sicker. I started having bad bone pain.
The rheumatologist recommended a special medication for it. But by that point, my immune system was pretty torn up — not only because of my undiagnosed cancer, but also because of all the medications I had been taking.
I ended up with an infected elbow and cellulitis from my fingers to my arm, which almost had to be amputated.
I also told them I had fatigue, and they didn’t think I did, but then I was blacking out.
My platelet and blood volume levels were also quite high, with platelet counts in the 900s, a hematocrit of over 51%, and elevated hemoglobin and white blood cell counts. The numbers continued to rise.
My spleen was enlarged, too, but they didn’t think it was anything to be worried about. But it would give me bad acid reflux because it was pushing on my stomach, and I would end up in the ER with quadrant pain. They would give me medicine to treat the symptoms, but not the underlying issue.

I was so worked up that I didn’t sleep for three days before the appointment.
I left that appointment knowing I had cancer.
I Was First Diagnosed With Essential Thrombocythemia (ET)
Given all these symptoms, my doctor finally agreed to send me to an out-of-network rheumatologist, who ran a whole bunch of tests that came back negative. The rheumatologist looked at me and said, “I think I know where I can get you help.”
That’s when Neal was referred to a hematologist-oncologist who listened to me, took note of all my symptoms, and did some blood tests. I was so worked up that I didn’t sleep for three days before the appointment. I left that appointment knowing I had cancer.
We saw the diagnosis of reticulin fibrosis, which refers to an abnormal accumulation of reticulin fibers (a type of connective tissue) in the bone marrow. The specialist confirmed that I had essential thrombocythemia (ET). She added that the fibrosis was nothing to worry about at that particular point in time.
I had a phlebotomy or a blood draw, and the specialist put me on palliative care immediately afterwards. Within a week, I was getting calls from all sorts of doctors — psychiatrists, psychologists, dietitians, and so on.
Editor note: Palliative care is specialized medical support, often recommended as soon as cancer is diagnosed. Its goal is to help people with serious illnesses, like cancer, feel better by treating pain, symptoms, side effects, and stress—so they can live as comfortably as possible before, during, and after treatment, no matter their age or stage of illness.
How My Diagnosis Made Me Feel
Being diagnosed after having felt unheard by the medical community for so many years was an eye-opener. That had repercussions for my work, too.
Seeing doctors repeatedly can raise flags. When you do that and the medical system doesn’t believe you, especially with myeloproliferative neoplasms (MPNs), which can be almost invisible, your employer isn’t inclined to believe you either. So mentally, it was just super defeating.
On top of all the physical symptoms I had been experiencing, constantly being misunderstood by the people I was seeking help from made me very anxious. I would think, “Why can’t somebody understand me?”
But my kids helped me keep going. I knew I had to provide for them. So no matter how many phone calls I had to make or how many hours I had to spend on hold with the state, I managed.


And successfully getting diagnosed with MPN eventually helped me deal with the anxiety and anger I was feeling.
I finally felt like someone was going to take me seriously and thought that I wasn’t just faking it. I’d say that the appointment I had where I was diagnosed was the best appointment of my life.
I cried halfway through when my specialist said, “I know what to do for you. This is the path we’re going to take. This is a real thing. Your symptoms are all connected.”
I’ve been with her for three years now.
I cried halfway through when my specialist said, “I know what to do for you. This is the path we’re going to take. This is a real thing. Your symptoms are all connected.”
My ET Progressed to Prefibrotic Myelofibrosis
I had a good year or so after my diagnosis with ET. And then all of a sudden, things started getting worse again.
I felt like my body was just working too hard, and I was in pain again. I also felt bone-tired — too fatigued to have just ET.
My pain was mostly focused on my hands and feet, although I did also experience some pain in my long bones — my shins, thighs, and forearms. I felt like I had pressure on my hands from the inside of my bones, pushing outwards.
The only way to describe it is pressurized pain.
The pain incapacitated me. It just dominated everything, including my thoughts. It made me sick enough to vomit, and I couldn’t eat. Thankfully, I’m now on pain management, which helps reduce the pain enough for me to be able to eat.
This pain prompted my doctor to undertake three bone marrow biopsies. Each one showed progressively worse fibrosis. The last one, which was done in February 2025, showed grade one prefibrotic myelofibrosis.

I’m Exploring a Clinical Trial
My prefibrotic myelofibrosis diagnosis qualified me for a clinical trial at City of Hope National Medical Center.
I had done some previous research on clinical trials, and my doctor had also brought them up as possible options if the medicines failed. So she outlined how they would work, how I could get the free housing during cancer treatment and travel to City of Hope, and what the expectations would be like.
Everything she explained was consistent with what I read, which was that they wanted patients like me there and that they wanted to help us. She just gave us hope.
I think that patients need to learn everything they can about clinical trials as an option. Patients need to be as prepared as possible.
If they don’t, they might be doing a disservice to their care. Especially patients with prefibrotic myelofibrosis or overt myelofibrosis, as it’s a very rare and disabling condition.
And if you get the right doctor and the right treatment quicker, it can be a lot less scary and disabling.
… if you get the right doctor and the right treatment quicker, it can be a lot less scary and a lot less disabling.
How I Track My Symptoms
I’ve kept myself in the know about my bloodwork and everything like that. Because of this, my doctor can talk to me in a way that makes it less concerning for me.
She tells me about trends and how my bloodwork can get worse, how my white count would go higher, how we would be seeing lower drops in my hemoglobin or hematocrit, or if we would be seeing peripheral blasts — refers to immature white blood cells (blasts) that show up in the bloodstream when the bone marrow isn’t working right — in the bloodwork.
“Until that point,” she says, “Don’t freak out. You’re gonna be okay. Just keep your head above water.”
She’s always been positive. She knows my youngest daughter, and we’ve always sent her pictures, or she meets her at some appointment, She’s really personable—everything you’d want in a rare cancer specialist.


I Have Hope Going Forward
Having access to clinical trials and great cancer doctors is a must for patients with this illness.
I’ve gone from diagnosis to prefibrotic myelofibrosis in four years. It’s driven home the importance of my time with my kids.
And these trials make it a possibility that I’ll get a chance to see them all graduate, get married, and raise families of their own.
Who knows? I can only hope that I stay around for my daughters as long as I can.
Some patients who’ve joined clinical trials have responded really well to them. It would be the greatest gift if the trial works for me as well as theirs have worked for them. It would be life-changing.
As of now, it’s been so difficult to function, much less take care of my kids. The clinical trial has given me hope. More than I ever had before.
The clinical trial has given me hope.
More than I ever had before.
What I’d Like People to Know
If your bloodwork is a bit off — if something’s high or low — if you’re feeling tired, if you’re losing weight, you need to have a doctor check you out.
And if the doctor you see shrugs it off or says, “Well, this doesn’t make any sense,” find a new doctor who listens to you.
Don’t be afraid to fire your doctor and find someone else who can give you a second opinion. I’ve seen second, third, and fourth opinions save the lives of patients with this disease.
Explore the resources available to you — they’re out there, even if you don’t live in a big city. Don’t be afraid to get help. You don’t have to fight this alone.
There’s a great community of MPN groups out there that support patients and guide them through this illness.



Special thanks again to Karyopharm for supporting our patient education program. The Patient Story retains full editorial control over all content.

Inspired by Neal's story?
Share your story, too!



