Biomarker Testing Gave Lysa New Hope with Stage 4 ROS1+ Lung Cancer
I was 40 years old, very busy, still raising my kids, and working and going to school at the same time when I was diagnosed with stage 4 ROS1+ lung cancer. Lysa’s experience highlights her resilience and serves as a prime example of what self-advocacy can lead–in her case, lead to a new therapy.
At 40, she experienced severe mid-back pain that she and doctors initially thought was just a pulled muscle. Later, however, her symptoms worsened, leading to a shocking diagnosis: lung cancer that had already spread to her spine.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
Though her lung cancer was initially responsive to chemotherapy, Lysa was determined to learn more about it. This pushed her to reach out to fellow lung cancer patients on online patient communities. She also learned about biomarker testing, which empowered her to seek a second opinion, ultimately undergoing surgery solely to obtain tissue for comprehensive biomarker analysis. The result? She discovered she was positive for the ROS1 mutation. This qualified her for targeted therapy that significantly improved her quality of life.

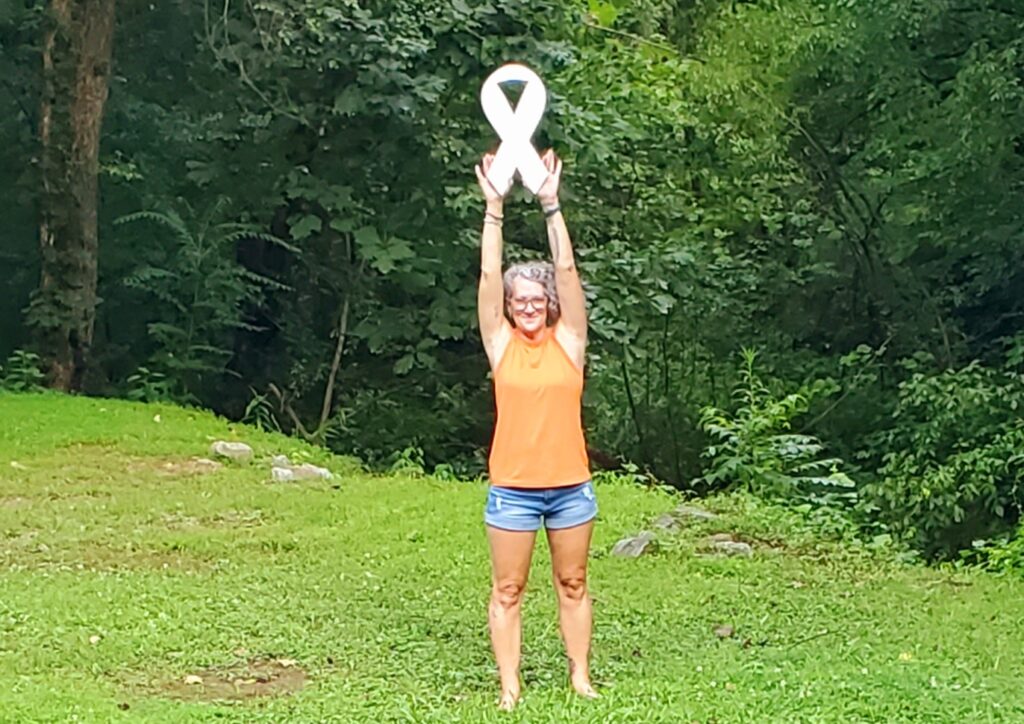
When her non-small cell lung cancer progressed, Lysa didn’t settle. She advocated for herself again, enrolling in a clinical trial that has kept her stable. Thanks to targeted therapy and clinical trials, she’s celebrated many milestones, including her daughter’s graduations and the birth of her first grandson, as well as other important moments with family and friends.
Lysa’s stage 4 ROS1+ lung cancer experience shows how critical biomarker testing and clinical trials are in expanding treatment options. Her story is a testament to the power of self-advocacy, community support, and the importance of never giving up on seeking better care.
Watch Lysa’s video and read her story below to:
- Find out how her back pain revealed her life-changing diagnosis
- Learn why biomarker testing became Lysa’s game-changer
- Discover how a targeted therapy and a clinical trial gave her more time with her loved ones
- See how Lysa’s self-advocacy with ROS1ders changed her stage 4 ROS1+ lung cancer care
- Meet the woman who thrives beyond her diagnosis
- Name: Lysa B.
- Age at Diagnosis:
- 40
- Diagnosis:
- Non-Small Cell Lung Cancer (NSCLC)
- Staging:
- Stage 4
- Mutation:
- ROS1
- Symptom:
- Severe but intermittent back pain
- Treatments:
- Chemotherapy
- Radiation therapy
- Targeted therapy, including through a clinical trial
- Surgeries: lung resection, metastatic spine tumor surgery


Thank you to Nuvalent for supporting our patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make treatment decisions.
- About Me
- When I First Noticed That Something Was Wrong
- The Moment Everything Changed
- How I Learned About Biomarker Testing
- Learning I was ROS1+ and Taking the Only Treatment Option Available Then
- I Joined a Clinical Trial When My Stage 4 ROS1+ Cancer Progressed
- Targeted Therapy Has Changed My Quality of Life for the Better
- Anyone With Lungs Can Get Lung Cancer
- My Advice to Others
You think you’re doing what you can to take care of yourself. I quickly learned that none of that really matters. If you have lungs, you can get lung cancer.
Lysa B. – Lung cancer patient
About Me
Hi, I’m Lysa.
I was diagnosed with stage 4 non-small cell lung cancer with an ROS1 mutation.

When I First Noticed That Something Was Wrong
I had just graduated from college. I was 40 years old, very busy, still raising my kids, and working and going to school at the same time.
I started having back pain. It wasn’t a typical lower back pain that you’d get by straining yourself doing something, though that’s what I kept telling myself. It was a little bit higher, right in the middle of my back.
My husband and I took our daughter to California for a vacation, and we visited SeaWorld in Disneyland. There were two nights when I would lie down, the pain was so bad that I felt like I couldn’t breathe right, and I couldn’t sleep. My husband said, “We have to go to the E.R., we have to figure out what’s going on.”
We went to the E.R. around midnight. There, they were concerned about my kidneys because of the back pain. But my kidneys were fine, so they thought I’d just pulled a muscle. They gave me a few muscle relaxers and pain medicines to get me through the weekend, and they told me, “Follow up with your doctor when you get home.” And the next day we went to Disneyland for 12 hours.
I agreed that I must have just pulled a muscle. Everything seemed to be fine. I was 40. I was healthy. I was a runner. I was in great shape at the time, or so I thought. So you shouldn’t ever believe that cancer is not on your radar.
The pain was intermittent, so I was able to ignore it and push through. I was taking a lot more Tylenol at that point, icing the area, and getting massages. But it wasn’t getting better.
I went on a vacation to see my family in Kentucky, and the pain got so bad coming home from the airport. I was traveling alone, and I remember calling my mom, crying, and telling her, “I can’t even walk through the airport right now.” She went, “Get a wheelchair, just get home. We’ll take care of it.”
The next morning, we went to the E.R. again, this time to an E.R. near where we lived. They did multiple tests, a CT, a full MRI of my entire spine to try and see where the pain was coming from, as well as a chest X-ray.

I was in great shape at the time, or so I thought. So you shouldn’t ever believe that cancer is not on your radar.
Lysa B. – Lung cancer patient

The Moment Everything Changed
Several hours later, the E.R. doctor came in and told us, “You have to sit down. It appears that you have stage 4 lung cancer that’s already spread to your spine.”
I had just lost a friend to lung cancer about five months before that, and she had only been 43. So I immediately thought, “Oh my God. Who’s going to raise my kids?” My son was 19, but he still needed me. My daughter was 11.
You think you’re doing what you can to take care of yourself. I quickly learned that none of that really matters. If you have lungs, you can get lung cancer. Unfortunately, sometimes you’re just dealt a crappy hand.
How I Learned About Biomarker Testing
Right after I was diagnosed, I found an online forum where I started talking to other patients. Mostly, I just connected with them and tried to seek support. And through that forum, I learned so much about lung cancer.
It’s not one disease. You don’t just treat it one way. And there are biomarkers, which are proteins that drive your cancer to grow. They are specific to certain lung cancers, and they typically tend to be in younger women, mostly under 50.
I did talk to my oncologist about it, but I was having a great response to chemo at the time. So she just said, “When the time comes, we’ll look into that.” I was okay with that for a while, and it wasn’t until I had progression about 15 months later that we decided to try and do another biopsy to get enough tissue to do biomarker testing.
At that point, my tumor had a lot of scar tissue around it. It was in a hard-to-access spot. We had done two needle biopsies through my lung, which were inconclusive and didn’t have enough tumor DNA actually to tell if there were any biomarkers or not. So my oncologist wanted to try another chemotherapy, and at that point I said, “There’s got to be something better than this.” And I switched oncologists.


Learning I was ROS1+ and Taking the Only Treatment Option Available Then
Within a couple of weeks, I was seeing a new doctor, Dr. Vogelsang. He pushed for me, and that validation helped me realize that this man was going to help me do whatever I needed to do for however long I wanted to do it.
At the time, it took several weeks to get my results back. It was stressful, and I was trying to be hopeful. Plus, I was recovering from surgery.
My phone rang at 10 p.m., and I don’t normally answer my phone if I don’t know who’s calling me, but I answered, and it was Dr. Vogelsang. He said, “We’ve got great news, your results are in. And you’re ROS1-positive.”
He was super excited about it, and I was too. I knew that meant I was eligible for targeted therapy. I wouldn’t have to do chemo anymore. So it was great. It was literally a game-changer for me.
By the time I found out what my biomarker was, it was 2013. I had already been diagnosed with and living with lung cancer for 18 months. I started getting nervous around that time; it was like I was feeling I was on borrowed time. I wondered when it was going to quit working.
I was eligible for targeted therapy. I wouldn’t have to do chemo anymore… It was literally a game-changer for me.
Lysa B. – Lung cancer patient
I Joined a Clinical Trial When My Stage 4 ROS1+ Cancer Progressed
We added chemo to my targeted therapy in the hope that it would get me at least to the end of that year, seven or eight months away, before I might start on that drug. Well, I remained stable with that combination for another five years, so I was able to stay on my first targeted therapy for ten years.
By the time I progressed again after those five years, I had a new biopsy. I did have new metastases in places I’d never had before, and it seemed to be fairly aggressive. It went from nothing on a scan to not significant to more than doubling in size two months afterward. I knew we had to do something quickly.
We did a biopsy on my 50th birthday. That was fun. And based on those results, I decided to go on a clinical trial. So in June 2023, just over two years ago, I started a phase one clinical trial that I had to travel to Tennessee for.
I’m still in that trial. I actually went again just last week. I just got my scan results back, and I’m still stable. So I’m extremely happy about that.
I feel pretty good on this drug, which is nice. And I don’t have to do chemo anymore. Because of this drug, I’ve lived long enough to see my first grandson. The drug is in pill form. I’m able to have my scans at home.


Targeted Therapy Has Changed My Quality of Life for the Better
When I was diagnosed, my youngest was 11, and she was in fifth grade. Honestly, my first goal was to see her graduate from high school. I wanted to give her that much, at least, to get her there. Of course, I was the loud lady at her graduation. I was so excited and crying and bawling.
I’ve since gotten to see her graduate from college. I have just had our first grandson this year. And my son was 19; he was older, but he still needed some help, and I have been able to see him flourish and find his way in this world.
My husband and I love to travel and eat. I have a great friend group here. We do trivia every week. My parents live two miles from me; I just hung out with my mom all day the other day.
I know I’m lucky that I can do those things. I’ve always been such an on-the-go person, the type who has to take care of everything right now. I can’t go to bed till the dishes are done, that sort of thing. I need structure, and I might have been a little extreme.
Now, I don’t care if there are dishes in my sink. I try not to let external things get me down. And I focus on trying to find the joy in every day.
My biggest happiness is when I’m with my family and my dogs. I love my dogs.
I try not to let external things get me down. And I focus on trying to find the joy in every day.
Lysa B. – Lung cancer patient
Anyone With Lungs Can Get Lung Cancer
One of the first questions many people ask you when you tell them you have lung cancer is, “Did you smoke?” It used to make me angry, because it felt accusatory. But I really think when people ask that question, if they’re nonsmokers, they’re trying to be like, “Oh, well, that’s why you got it.”
I honestly don’t think they come from a bad place, but it makes you feel bad, like you have to defend yourself. My grandmother died of lung cancer, and she was a smoker her whole life. Can we blame her for her death?
Everyone deserves access to care. We have lung cancer. It doesn’t matter how we got it. And there are many risk factors out there, so many that we don’t even know how to correlate them, though we do know that they contribute to lung cancer.
I have friends who are vegetarians, yoga instructors, lifelong runners, and so on. People who thought they did all the right things. And yet we still got lung cancer. I still ended up getting stage 4 ROS1+ lung cancer.
Cancer doesn’t discriminate.

You do not have to be alone.
Lysa B. – Lung cancer patient

My Advice to Others
There are patient groups for most of these biomarkers. There are maybe a dozen online. Many of them have websites. You can look them up and join them. You do not have to be alone.
They are a huge source of not only support but also knowledge. Like the ROS1ders in particular. It is scientifically vetted by researchers, as well as all of our information about the drug options. What works for us, what doesn’t, how to deal with side effects. There are patient stories on there. There is a large community out there that many people might not know exists. I am proud to be part of ROS1ders.
These patient groups aren’t just for other patients. We’re seen and invited to medical conferences now. Doctors and researchers collaborate with these groups to do better for the people in our community. So please reach out to them if you have a biomarker. It’s so important.


Special thanks again to Nuvalent for its support of our independent patient education content. The Patient Story retains full editorial control.

Inspired by Lysa's story?
Share your story, too!
More Non-Small Cell Lung Cancer Stories
Shira B., Lung Cancer, EGFR+, Stage 1B
Symptoms: None per se; discovered during a preventative full-body MRI
Treatment: Surgery (thoracotomy)
Phil P., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptoms: Persistent cough, nasal drip, shortness of breath, inability to speak in full sentences
Treatments: Chemotherapy, targeted therapy, radiation therapy, next-generation ROS1 inhibitor (clinical trial)
Stephanie K., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent and intense cough, general feeling of sluggishness
Treatments: Chemotherapy, targeted therapy through a clinical trial, radiation therapy
Ruchira A., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Mild intermittent cough while talking, low-grade fever, severe nonstop cough, coughing up blood, collapsed left lung
Treatments: Surgery (lobectomy), targeted therapy
Jennifer M., Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptoms: None per se; discovered during physical checkup for what seemed to be a sinus infection
Treatments: Radiation therapy (stereotactic body radiation therapy or SBRT), targeted therapy




