William’s B-Cell Acute Lymphoblastic Leukemia Story
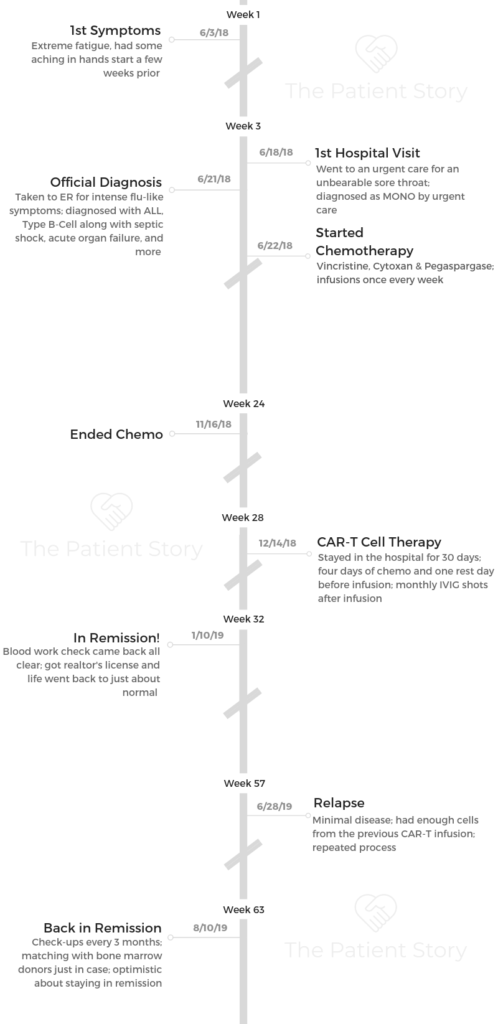
William shares his story of getting diagnosed with acute lymphoblastic leukemia (ALL) at 21 years old. He describes undergoing chemotherapy and CAR T-cell therapy twice.
William also highlights issues with navigating cancer, including the issue of fertility preservation and the support that meant most to him.
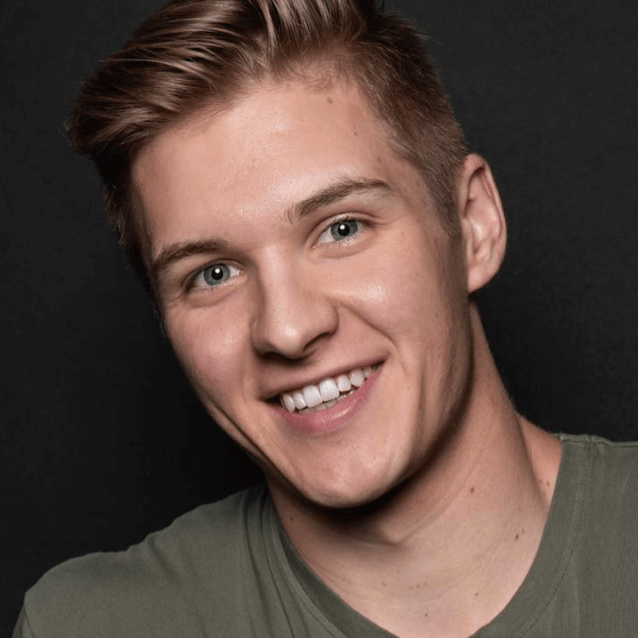
- Name: William Y.
- Diagnosis (DX):
- Acute lymphoblastic leukemia (ALL)
- B-cell (most common)
- Misdiagnosis: Mono
- Age at DX: 21
- Staging: N/A
- 1st Symptoms:
- Achy hands
- Sore throat
- Extreme fatigue
- Treatments:
- Chemotherapy
- Vincristine, Cytoxan & pegaspargase
- Once a week, either on Wednesday or Friday
- Vincristine, Cytoxan & pegaspargase
- CAR T-cell therapy (twice)
- Chemotherapy
Welcome to the show. You’ve got tons of people who have already gone through it. You’re not the only one.
If we’re talking about leukemia, it doesn’t have to be a life-or-death thing by any means. We’re very fortunate these days with the medical advancements we’ve made. It’s a very treatable cancer.
Regardless of how this might affect your life in the short-term, don’t worry too much. Your social life isn’t over. Your life isn’t over. Make a story out of it, and document it if you need to.
William Y.
- Diagnosis
- Chemotherapy
- CAR T-Cell Therapy
- Relapse & Remission
- Quality of Life
- Losing hair after chemotherapy
- Advice on dealing with hair loss
- Fertility preservation
- What was the lowest point for you mentally and emotionally?
- How do you feel now?
- How important was it for you to have a support system?
- How was the financial aspect of treatment?
- The “new normal” after cancer
- Do you have any advice for someone has just been diagnosed?
- Do you have a message for someone reading this?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
The first thing I noticed that was out of the ordinary was my fingers would ache. I didn’t really understand that. I was 21 years old at the time and figured I shouldn’t be having any arthritis or anything like that.
I was in Washington, D.C., and I didn’t want to go to a doctor and get it checked out. It was something I had texted my mom about and told her it was annoying because it was hurting to write at work. It was just one of those weird things.
I also had a really bad, swollen sore throat. It was having strep throat but way worse. It was almost swollen shut.
I had some insane fatigue as well. I was absolutely exhausted. I would wake up for work and be ready for bed again by 10 a.m.
For some reason, I didn’t think anything of it. I was in a new city for an internship, and I thought I was just tired from all the stress.

What made you finally go to the doctor?
The sore throat sent me to an urgent care place. They diagnosed me with mono. They didn’t give me antibiotics or anything since it’s a virus, but they did give me a mouthwash. I think it’s actually called magic mouthwash. That was about it.
I just went home and laid in bed for a week. About 4 days later, I went out into the kitchen to grab a bottle of water, and my roommate was talking to me. I couldn’t hear a word he was saying. I was in a delirium. I didn’t even know where I was really, and I didn’t even have the strength to open our refrigerator.
He said, ‘Okay, we’re going to the ER right now.’
He drove me there that night. We got straight in, and I was diagnosed with everything right then. It was an intense evening for sure.
After that period, I blacked out basically for a week and a half. My body was just so weak. I didn’t have the ability to stay cognitively present. I didn’t come to and understand what was going on for about 2 weeks after the diagnosis.
How did your doctor tell you about the cancer?
I remember getting told and blocking everything else out after that because it was so traumatic. They came back into the ER with the results of the tests, and he said, “You’ve been diagnosed with leukemia.”
At first I didn’t believe him.
Prior to this, I took really good care of myself. I like to think of myself as the epitome of health. I really went out of my way to make sure I prioritized my health. I was in complete disbelief, and he asked if there was someone they could call.
I called my mom, told her I thought the doctor was joking with me, and handed her the phone.
What tests did they run at the initial ER visit?
They ran a urine and blood test. Other than that, they just swabbed my nose and throat because of the mono, but the blood tests are what ultimately revealed everything.
How did you process the cancer diagnosis?
Disbelief from the diagnosis and the shock was huge. I was also just really tired, though. I was in and out of a drowsy state all the way to the ER. It was so weird.
Those last few days when I had been laying in bed, even with how sick I was, I was still taking care of myself. I was drinking water, trying to eat, sleeping, getting up to use the bathroom when I needed to, and using the opportunity to walk around for a minute.
I felt lucky that they caught it, but it was just so unexpected because I was so healthy before.
What ended up saving my life was probably how well I had taken care of myself before all this.

I was really terrified. I was bedridden for about a month after I was diagnosed. I had to relearn how to walk. I was scared. At the same time, my mind has always been very strong.
Even when I was dazed, I was still talking about beating the cancer. I had no problems doing whatever the doctors and nurses needed to do to make me better.
Right after being diagnosed, I said, ‘Let’s just get this shit going.’ They wrote that quote up on my board.
The emotional side was mostly being terrified, but also the why’s and how’s. However, I quickly understood that I couldn’t change the situation and that I needed to do whatever I could to fix it. Ruminating wasn’t going to solve anything.
»MORE: Patients share how they processed a cancer diagnosis
What was the first conversation with your oncologist like?
That was a conversation between my mom and the oncologist actually. I was in the ER in Washington, D.C., and I got transferred to a hospital in Baltimore. My mom actually beat me somehow. It’s a 10-hour drive from Indiana, where we’re from, and somehow she beat me.
She started talking to the oncologist when she got there and got everything set up for me. They found out what type of leukemia I had pretty quickly. They have an incredible team at Johns Hopkins.
They set my plan up before I got there because she knew I would want to get started. She knew I would want to do whatever it took to get better.
We just went ahead and started chemo the day after I was diagnosed. It was kind of a no-brainer at that point. I was so full of antibiotics and other drugs for the septic shock that I figured adding a little chemo to the mix wasn’t going to hurt.
Transferring closer to home
They wanted to try to transfer me home as soon as they could. It wasn’t ideal for my family to try to stay there because it was so expensive. It was hard for my mom to stay there. As soon as I got my ability to walk again after working with physical therapy, I could sort of take care of myself.
They cleared me to go back to Indiana and continue my chemo there. That was actually a pretty seamless transition. The doctors did pretty well. It was great to be home. That by itself helped my recovery tremendously.

Chemotherapy
What was your chemo regimen?
I was in the hospital for about 2 weeks when I got back home. They just wanted me close in case I needed any blood transfusions or anything like that.
I went in every Wednesday or Friday. It all depended on how much time needed to pass between each drug.
At this time, I was on vincristine, Cytoxan, and pegaspargase. I was at the hospital once or twice a week for a while.
We did lumbar punctures and bone scans every month to check my status. Those would be randomly scheduled throughout the week.
Infusions took anywhere from a simple 15 to 30 minutes to one of the drugs taking all day. That one required fluids before and after, so it took much longer.
Side effects from chemo
I was very fortunate. The main side effects I had were hair loss and neuropathy.

I actually shaved my head right when I got to the second hospital. I didn’t want to watch my hair fall out. I didn’t want to find hair in my bed or random places. That just grossed me out.
The neuropathy was numbness in my fingers and toes. That made walking a lot harder than I expected. I had some numbness settle in my thighs. My quads were numb and sensitive.
I wasn’t aware that it was a possibility. The PT girls had this prick system. They would use things like the end of a pencil and ask if I could feel any of it. I didn’t. The neuropathy in my feet was so severe that they said I could’ve walked on broken glass and I wouldn’t feel it. It was a weird thing.
My mom would joke about me ‘walking drunk’ all the time. I just didn’t understand where my feet were in space. I’m really tall — I’m 6’7″ — so it made walking extremely difficult.
I only got sick from chemo once, and it was because I ate too quickly after the infusion.
About a month into chemo, I think that’s when everything really caught up to me. I was extremely fatigued all the time, and that’s when I got the neuropathy.
»MORE: Dealing with hair loss during cancer treatment
Describe the bone marrow biopsy and lumbar puncture (spinal tap)
I’ve been very lucky. I was diagnosed with the pediatric form of leukemia, so I was allowed to be put under for the biopsies. I wasn’t allowed to when I was in Johns Hopkins, though, and I had lumbar punctures with only the loopy medicine and some local anesthetic. I was awake for those, but they numb it. After I went back to Indiana, I started getting put under for them.
Side effects of the bone marrow biopsy and spinal taps
It is a little painful, but you chuck right through it. Afterwards, you have a sore back for 2 or 3 days. I recommend planning on relaxing for 2 or 3 days and trying not to strain yourself too much.
There are things called spinal headaches, and I’ve had one of those. It can happen, and if it does, just know it will definitely be the worst headache you’ll ever have.
That’s simply when they do a bone marrow biopsy or lumbar puncture and the spot where they drew the spinal fluid from doesn’t completely close over, and it leaks onto nerves or something like that. It gives you an extremely severe headache. It makes you want to be in a bubble, kind of like when you have a migraine.
I’ve had a lot of lumbar punctures and bone marrow biopsies, and I’ve only ever had the one headache, so try not to worry about that too much.
The scan anxiety you get before the bone marrow biopsy you get before can be pretty bad, but the news you get after can be freeing because you understand your place and can plan your next steps.
How did you deal with “scanxiety”?
For those who don’t know, “scanxiety” is the anxiety you have about any scans that will update you on your current status. Dealing with that can be tough.
I’ve been talking with a therapist ever since I was diagnosed. That helps out a lot. Voicing your thoughts and feelings on everything that could go wrong or could go great helps.

If you just say out loud the best- and worst-case scenarios, it helps you ground yourself and realize where you are.
It’s something that every cancer patient faces. Whenever you’re going back in to get a scan and check your status, it’s anxiety-ridden.
The best way to cope is to keep a strong head and have a good mindset and believe that things will turn out the way they’re supposed to.
»MORE: Dealing with scanxiety and waiting for results
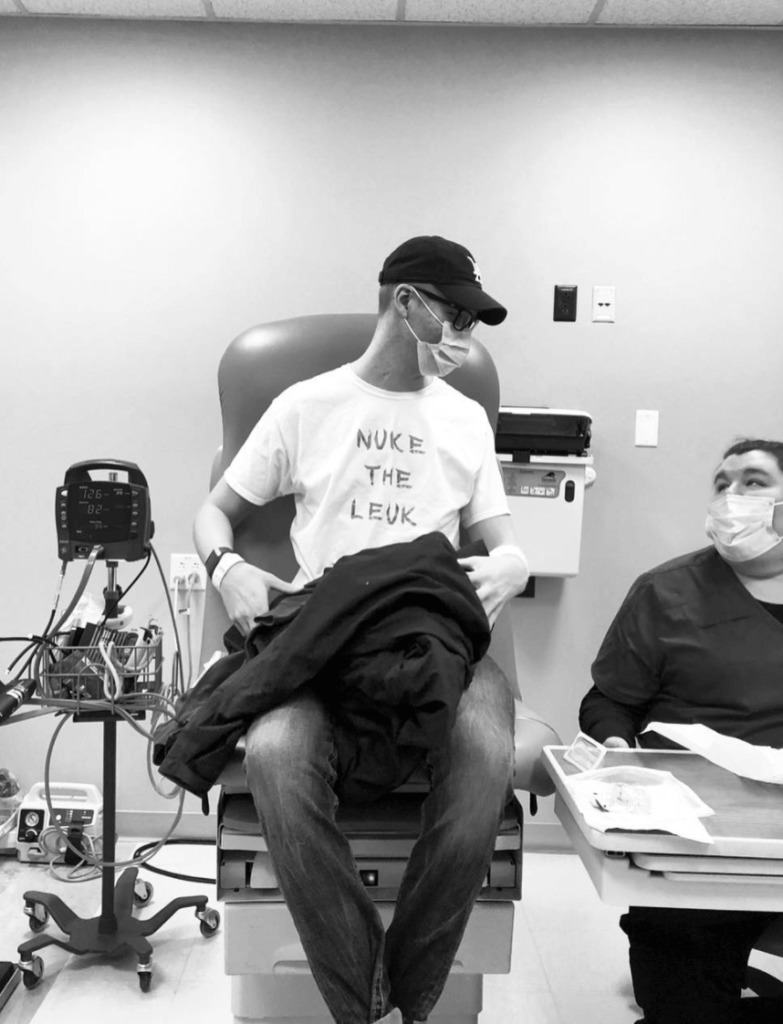
CAR T-Cell Therapy
Leukemia in bone marrow meant a different treatment path
They ended up not doing radiation because by the time I ended my first chemo, there was still leukemia in my bone marrow. It was enough that they wanted to take a different approach.
I had 2 options: CAR T-cell therapy or a bone marrow transplant. I went with the CAR T-cell therapy.
Why did you choose the CAR T-cell therapy?
I get asked why I chose to go with that a lot. First of all, it was new. Secondly, it’s a lot less intense and toxic than the chemo and radiation I’d have to get in preparation for the bone marrow transplant.
I liked the idea of genetically modifying the cells. I liked being a small part of cancer research in a way. The main thing for me was you can do CAR-T and then bone marrow transplant, but you can’t do it the other way around. I figured we might as well give it a shot.
The CAR T-cell therapy put me in remission. I did that and some chemo in December, and I was in remission in January.
What’s the CAR T-cell therapy process like?
They have to extract the cells from your body. Then they ship them off to a lab to grow, and then you get them infused back in you at the hospital later. While you’re waiting for the cells in the lab, leukemia can still be growing in your body.

They gave me a maintenance chemo regimen to keep my leukemia at bay. They wanted it to stay in at a manageable level. I rode that until December, when I got the cells infused.
They took the cells in October, so the growing process takes a while. They hook you up to an apheresis machine, which looks kind of like a dialysis machine. They stick a needle in your arm on both sides. On one side, they draw out the cells, and the other is where they put the blood back in without the cells. They withdrew a lot. I don’t remember the number, but it was a lot.
It took 4 or 5 hours. That process wasn’t that bad. I was used to having an IV, needles, and pokes. That was just part of the deal. The withdrawal process wasn’t bad at all. I was a little tired afterwards, but that’s about it.
Before you get the cells infused, they start you on 4 days of chemo, and then you have one day of rest before infusion. The 4 days of chemo are fludarabine and Cytoxan.
During the rest day, you get prophylactic medicine, immunoglobulin, and some sort of anti-fungal. That day isn’t bad at all.
You just get to chill out. The chemo gave me heavy loss of appetite, but that was it.
On the fifth day, you receive the cells. They’re in a small bag that’s been hanging out in liquid nitrogen for however long. They heat the cells in a liquid bath, and they hook you up to your port or PICC line or wherever you’ve been getting infusions.
It has to be a gravitational infusion, so they just drip in themselves. You just hang out.
It’s very anticlimactic for something that you’re hoping will save your life, honestly. It was a really cool experience nonetheless.
What are the side effects from the CAR T-cell therapy?
The side effects are pretty intense. They put them in 2 categories. You either have an immuno response or a neurotoxicity response.
With the immuno response, you might end up in the ICU because you get really bad flu-like symptoms. I don’t think it’s a life-or-death thing usually, but they definitely have to take care of you.
With the neurotoxicity, you can get seizures, forgetfulness, confusion, numbness, and things like that. It can mess with your heart. Those are the things they really look out for because those can be more serious.
I didn’t actually have either. I didn’t really have an adverse reaction.
They put me on a lot of prophylactic medicine. Stuff for seizures, nausea, anti-fungals, antibiotics, and stuff like that. I had to stay in the hospital for about a month. They like to watch you for a while and make sure everything looks okay.
»MORE: Read more patient stories and info about CAR T-acell therapy
Relapse & Remission
When did you go into remission?
On day 30 after your infusion, they check your bone marrow. When they checked mine, I was completely clear and in remission as of January 10th. I got the 3-month checks and monthly blood checks.
I relapsed on June 28, and I’m back in remission as of August 10.
We have started the bone marrow transplant process to line me up with donors just in case it returns, but right now we’re staying positive.
How did you feel when you were told you were in remission the first time?
I was extremely relieved. I was also a little naive, though. I for sure thought it could never come back. I don’t think I could’ve done anything differently to take care of myself mentally, emotionally, physically, spiritually, or any other area.
I checked all the boxes for staying healthy. I was so relieved and naive to the fact that it could come back.
I thought that cancer was a chapter of my life I could close. I had a great 6 months of life without it, but it returned nonetheless, so I got humbled again.
How did the relapse affect you mentally and emotionally?
It was far more mentally taxing to deal with the relapse than it was to deal with the original diagnosis.
The relapse was really hard because I was in really good condition. I was in a lot better shape, and I wasn’t sick like I was when I got diagnosed. When I was originally diagnosed, I felt sick. I was in bad shape. I was bedridden.
When the relapse happened, I was socializing, going places, and I was active and working on my career. Realizing that it could interrupt my life like that again and even more so this time around is something that I’m still working through.
What was the treatment plan the second time around?
The exact same CAR T-cell therapy procedure. They had an extra dose of my cells. I had no mutation in the relapse, so they were able to just use those. Repeat December/January and put it in July and August, and you have almost the exact same experience.
It’s like it was act 1, scene 2 of the same show. We’re preparing for a bone marrow transplant just in case it comes back a third time, and that’s what we’ll do next if it comes to that.
Are you anxious about the cancer coming back again?
Definitely. I’m 1 of 2 people who have gotten a second CAR T-cell infusion at Johns Hopkins, and the data on that cohort of people is so small.
Knowing that and reading my oncologist’s face, I think we almost anticipate a bone marrow transplant in the next year, but they aren’t counting out the fact that the second infusion could completely work.
They don’t know because there’s such little data. I’m really just nervous about it because I know if it does come back, there will be a 6-month period of suffering I have to go through with the chemo, transplant, hair loss, and side effects. That would be rough to do again.

Quality of Life
Losing hair after chemotherapy
Interestingly enough, it was pretty hard for me. I haven’t had a buzzed head since maybe even grade school. I’m always used to having thick, styled hair on my head.
What was more shocking for me than anything else was that I couldn’t recognize myself. All the sudden, I looked like a hairless cat. It changes how you perceive yourself.
It’s a confidence wrecker. It’s hard because it’s a universal label for sickness. It was definitely hard.
I was inpatient with a girl who actually decided to keep her hair. She got a bone marrow transplant. She chose to let it fall out and document it. I thought that was really interesting. She had this beautiful long hair, and that was a really interesting experience to watch.
I don’t know how she feels on the inside, but on the outside, she rocked it. I would kill for that confidence. She would wear hats, but she had no problems walking around without a hat.
Everyone handles the hair thing a little differently, but I’m [part of] the many who wanted to control it, in a sense, and shave it off.
Advice on dealing with hair loss
If you want control over it, definitely just chop it off. If you have longer hair or are nervous about it, get a wig. Why not?
I don’t know about anyone else, but prior being a part of cancer world, I couldn’t tell the difference between real hair and a wig. You can rock a wig just as much as you can rock your own hair. It gives you an opportunity to try new hairstyles.
Hair loss is inevitable. Face it. You’re not alone. It will grow back. Sometimes it’ll surprise you and grow back a little curly or a different color. That can add to the fun of it if you’re able to have a good perspective on it.
Fertility preservation
With the condition that I was in, I was unable to do any kind of fertility preservation. I was on my deathbed practically, so there was no time. That was a conversation we had after coming back to Indiana and moving towards the CAR T-cell therapy.
If I was going to have a lot more chemo, like if I have to end up doing a bone marrow transplant, I’m definitely going to have to do some fertility preservation.
Right now, the doctor is confident that my reproductive organs are all working properly. He didn’t think there would be a large effect on any of that with the drugs I got and the way I responded to everything, so as of right now, I haven’t preserved. It will most likely happen if I have to get the bone marrow transplant, but luckily I’m still fertile now.
That’s something that goes amiss for some folks, so that’s an important conversation to have with your doctor. I’m someone who really wants to have a family when I get older.
Having to make decisions about that and think about it at such a young age is pretty strange.
Surprisingly, my mom is the one who brought the topic up. At first, I didn’t really think about it. She knew I wanted to have a family later on down the road, and she brought it up to me. That was a conversation I took to the oncologist and social worker.
»MORE: Fertility preservation and cancer treatment
What was the lowest point for you mentally and emotionally?
I’m someone that likes to be the strong one in the room and not be too vulnerable. The lowest point was coming out of my daze after that first week and a half or 2 of being so sick.
Looking in the mirror for the first time and not being able to recognize who I was. That was probably the hardest.
Before all this, I had my hair and was really fit. Now I was barely able to walk. I lost 50 pounds at one point. I remember crying a lot after seeing myself in the mirror and really realizing what had happened. I had to come to terms with that whole thing.
It was mostly the trauma from the septic shock rather than leukemia at the time, but now obviously living with leukemia is still here. It lasts a lot longer than the septic shock. It’s hard to deal with it.

How do you feel now?
I just met with my therapist yesterday. I’m learning to not fortune-tell my life. I don’t know what’s going to happen in the future, and that’s okay.
I’m going back to school this fall. I got my real estate broker’s license this spring when I was in remission. I went on a date last night.
I’m still trying to live my 20s, even though I have leukemia restricting me in certain ways. That’s the best that I can do. That and continuing to take care of myself.
I try to use this as a learning experience every time it comes up, because cancer is a period in my life that will end. I just don’t know when.
How important was it for you to have a support system?
I had support and help from a lot of people. I got really lucky in that department. One thing my mom and I talked about a lot was having to go through that fight alone or without a lot of support. I felt like I had this whole family behind me. That includes not just my actual family, but family friends who are now family.
I had this group of people who surrounded me and gave me hope. They loved on me and prayed for me. Whether you’re religious or not, it doesn’t really matter to me. I’ll take any spiritual mojo I can get. I love it.

While I was getting my treatment, someone gave me a rosary. I’m not even Catholic, but they gave it to me. They said, “Even though this isn’t your thing, we just want you to know we’re here for you and praying for you.”
I’m probably going to make a necklace out of it because I think it’s something that goes so much further than the spirituality of it.
I’ve had so much love and support, and one of the key figures in that is my mom. She was with me every step of the way.
She was also the one that was head honcho in all the research. She looked up everything. She looked up scientific studies on everything that was happening and all the treatments I was on.
She prepared and knew all the best questions to ask the doctors. She was a staple throughout my whole treatment and easily a pillar of strength for me in my lowest time.
My therapist has been one of the most helpful people I’ve ever known. He’s helped me keep my head in the game.
As for life outside of cancer, I have my best friend. He’s the one that got me into real estate, and he’s been helping me continue on in my life. He and his family have been there through the whole process, and it’s just made our friendship even stronger.
My good friend I met out in Baltimore. She helped us enjoy our time as much as possible while we were there. I’ve been there so much that it’s like a second home to me now. She’s invited me into her network and introduced me to a lot of people.
She’s a little older than me, but that’s great with me because I’ve been forced to mature because of all of this. She’s been a beacon of light for my mom as well. Seeing someone help my mom out helped me out a lot. I can’t imagine being a parent in all of this, so that was a big help to us.
How was the financial aspect of treatment?
I’m on my stepfather’s insurance. He works for GM. They have been incredible. I seriously give props to them because I know a lot of people face a lot of insurance issues. That’s not to say that we haven’t had our fair share of hefty costs. Living out there during treatments has cost us upwards of $10,000.
Financially, as a student, it’s really difficult. I’m lucky to have my parents. My best friend and his family started a GoFundMe for me, and that helped so much. We opened a bank account specifically from that and had a “cancer card.” Any donated money went in that account.
One thing I did not expect and something I think students need to be aware of is student loans. I had to take a year off from school, but my student loan payments were expected to start 6 months after I stopped school. I had to get a deferment plan going there.
Make sure you check your student loans and get that squared away. I’m on a small disability check right now, so there’s no way I could’ve afforded them to start.

The “new normal” after cancer
Right now, I’m living by the mantra ‘YOLT.’ There’s YOLO, but then there’s also ‘you only live twice.’
My perspective has changed a lot. I value spending time with my family a lot more than I did previously. I don’t know why it wasn’t something I valued much, but it just wasn’t.
After I got diagnosed, that changed dramatically. I love spending time with my family. I’ve never been one to get attached to animals, but I’m the biggest sucker for my dogs now.
I’ve always had a strong mental game, so that’s been pretty consistent with some obvious ups and downs, but staying on top of that has definitely been a priority.
My new normal is probably a lot more emotional, which I don’t think is a bad thing at all. People tend to bottle emotions up a lot. That’s where a lot of anxiety and depression comes from, I think.
I feel a lot more wholesome. I feel more genuine. The way I see and think about things is different. The time I spend with people is far more quality.
I’m able to help a lot of people, surprisingly. It’s been kind of neat to see an impact in people’s lives.
I’m a lot more emotionally and mentally strong, while still being vulnerable. I’m a lot more willing to accept challenges now. I’m more open to opportunities that present themselves.
Do you have any advice for someone has just been diagnosed?
Most of the people I speak to say, ‘Wow, you really went through a lot.’ Well, yeah, I did, but at the end of the day, we have the same diagnosis.
One of the best things you can do is stay active in some way, shape, or form. I don’t care what that is. Just move. Do anything to help the chemo in your blood move around and do its job.
In addition to that, the food you eat is really important. My mom is a hippie. She’s plant-based vegan and eats whole foods. I call myself a flexitarian because after having this experience, I also see the value in eating things that you love. I have no problem with enjoying cake and ice cream.

Try to focus on eating a little more healthy if you can. Watch your diet a little more. Try to drink some more water. Even before I got diagnosed, those are 2 things I really lived by. Seeing how they helped me after diagnosis really just drove them home for me.
Do you have a message for someone reading this?
First, I’d be realistic. It’s a long process, and it sucks. Welcome to the show. You’ve got tons of people who have already gone through it. You’re not the only one.
If we’re talking about leukemia, it doesn’t have to be a life-or-death thing by any means. We’re very fortunate these days with the medical advancements we’ve made. It’s a very treatable cancer.
Regardless of how this might affect your life in the short-term, don’t worry too much. Your social life isn’t over. Your life isn’t over. Make a story out of it and document it if you need to.
Play the hand that you’re dealt. If this is the hand that you’re given, all you can do is the best that you can with them. I really tried to live that out. If leukemia happens to be in your hand, play it, and don’t quit. If you quit, you’re going to be miserable.

Inspired by William's story?
Share your story, too!
Acute Lymphoblastic Leukemia (ALL) Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)



