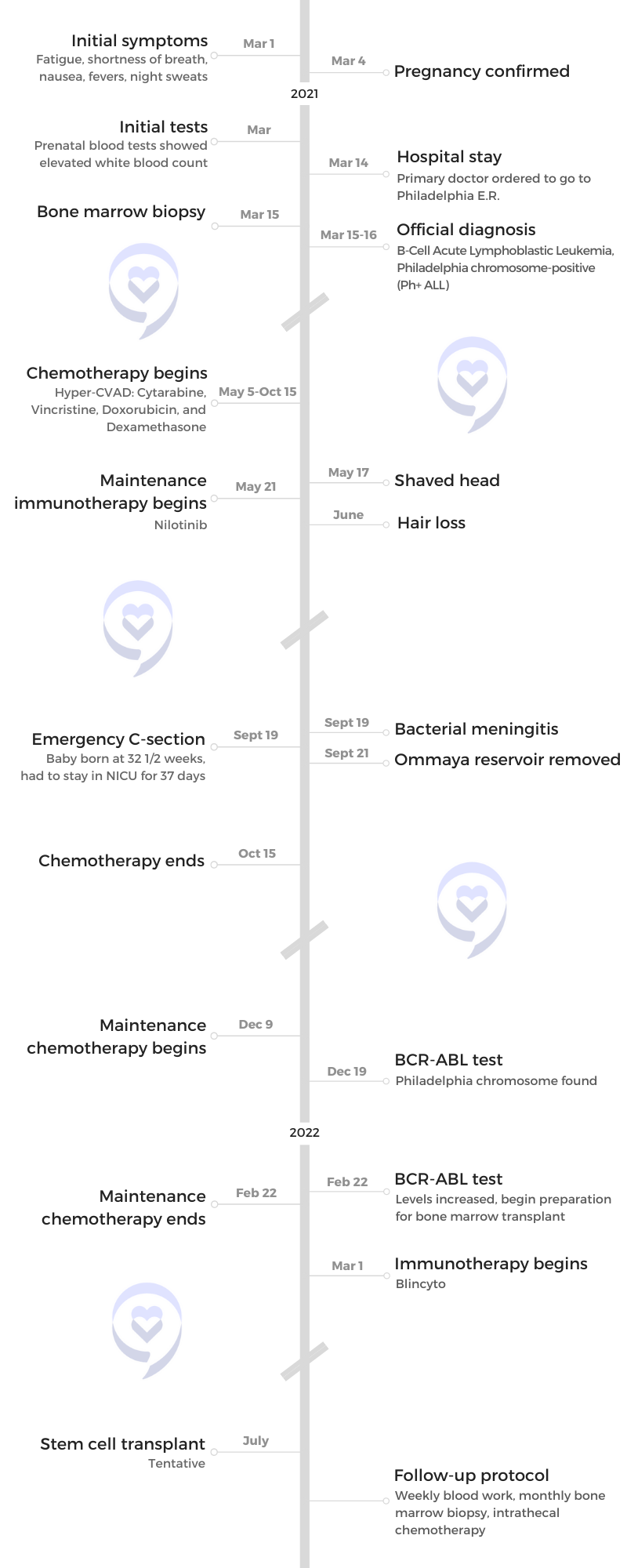
Renata’s Ph+ B-Cell Acute Lymphoblastic Leukemia Story
Renata was diagnosed with B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ ALL) shortly after finding out that she was pregnant.
She shares how tricky it was to be undergoing treatment while carrying their first child, giving birth via emergency C-section, and now waiting for her stem cell transplant.

- Name: Renata R.
- Diagnosis:
- B-Cell Acute Lymphoblastic Leukemia
- Ph+ (Philadelphia chromosome-positive)
- Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
- Treatments:
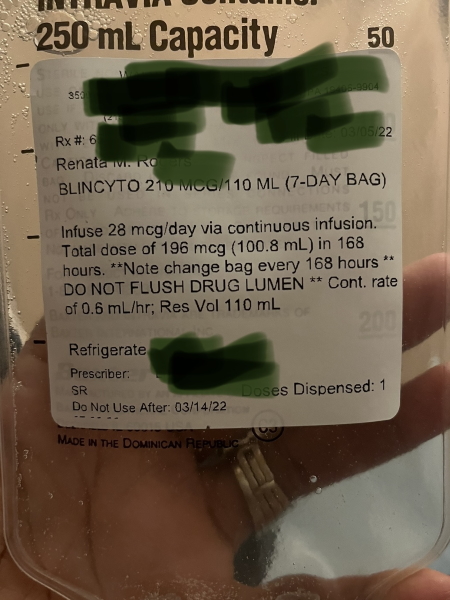
- Immunotherapy: Blincyto
- Chemotherapy: Hyper-CVAD (Cytarabine, Vincristine, Doxorubicin, and Dexamethasone)
- TKI: Nilotinib
- Stem cell transplant (tentatively scheduled for July 2022)
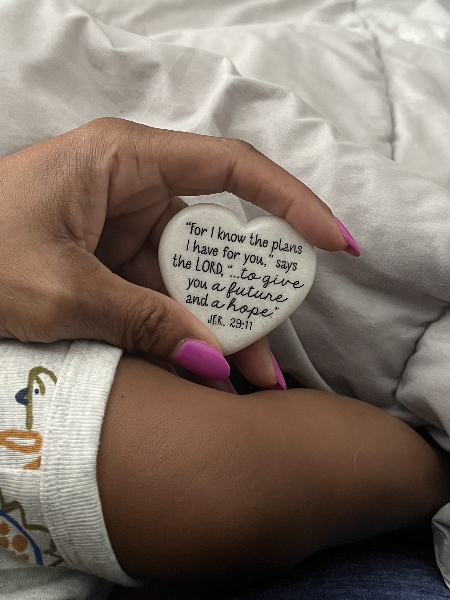
When you feel that urge to quit, you have to have something to hold on to, something to look forward to in the future.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I had this feeling, even when I found out that I was pregnant, that something wasn’t right. It was just this weird, foreboding experience.
Pre-Diagnosis
Tell us about yourself
I live in New Jersey. I work as a research scientist in bioanalysis. In my spare time, before cancer, I was really into working out, jogging, traveling, [and] just living life. I do a lot of things. I like to go out with my friends. That was pretty much my life before cancer.
Initial symptoms
Around the end of February [2021], I started to get tired. Symptoms like fatigue. I thought maybe [I’d] been working too much. I also became short of breath a few weeks later.
 On March 4th, I found out that I was pregnant, so that kind of put everything together. But I had this feeling, even when I found out that I was pregnant, that something wasn’t right. I couldn’t put my finger on it but it was just this weird, foreboding experience. I think that was due to fatigue.
On March 4th, I found out that I was pregnant, so that kind of put everything together. But I had this feeling, even when I found out that I was pregnant, that something wasn’t right. I couldn’t put my finger on it but it was just this weird, foreboding experience. I think that was due to fatigue.
My body was just out of it. I kept telling my OB-GYN I’m having nausea [and] fevers, what’s going on? I got diagnosed with [an] ear infection once.

I remember, one night, saying to my husband, “I feel like I’m dying.”
They put me on anti-nausea medication and it didn’t seem to help. It just got worse. I didn’t know pregnancy was this bad. I got to the point where — usually I walk my dog every day — I was out of breath walking him.
My work suffered because I could not concentrate and I was tired all the time. It just snowballed. It just got worse and worse. I chalked it up as just pregnancy.
I remember, one night, saying to my husband, “I feel like I’m dying.” He probably thought I was being a little melodramatic but that’s how I felt.
I was just so tired and I couldn’t get enough rest. Even if I would sleep 10 hours, it felt like I didn’t sleep at all. I would have night sweats, but I attributed that to the pregnancy hormones.
Testing
Initial tests
I didn’t find out until I went to my OB-GYN. You know how they do a whole battery of tests? They took 15 [to] 20 vials of blood. The next day, they called me back. It was a very weird conversation.
The nurse [said], “Your white blood count came back high and we can’t deal with that here.” It was just the way she said it and her voice, it kind of told me that something wasn’t right. She said it should be, I think, 4 to 11. Mine [was] 37.8.
While I’m talking to her, my primary doctor calls and [said], “Renata, I just got a call from your OB-GYN.” At the time, I didn’t have time to Google anything because I wanted to Google what is this? The doctor [said], “You need to go to the hospital. I’m going to call a hematologist.”
Hematologists, I know what they do, like blood disorder. “Could this be an autoimmune disease? Maybe I have lupus?” And he [said], “No, I don’t think it’s that, but we’ll call you back.” He called back and he was like, “Go to the E.R. in Philadelphia,” and I’m an hour from Philadelphia.
Diagnosis
Getting the official diagnosis
As we drove there, I did Google “high white blood count.” The first thing that came up was leukemia. But I said, “I know I don’t have leukemia, so I’m not worried.”
They redid the test at the hospital and it confirmed that it was high. That night, I had a doctor come in and it was just like in a movie. She sat next to my bed and I’m [wondering] what is she about to tell me.
She [said], “You have some type of blood cancer.” I couldn’t believe it. I said, “No. I’m pregnant.” And she’s like, “Yeah, you have some type of blood cancer. You’re going to meet with an oncologist.” I was in shock. I met with the oncologist and my oncologist was phenomenal
Reaction to the diagnosis
Disbelief because [with] cancer, I think the statistics are [that] 40% of us will get it. I know that. But I felt that I took care of myself. I didn’t eat red meat. All of the things that they say help you to stay healthy. That went through my mind. I did this and that, I don’t smoke. I can’t have blood cancer. I didn’t believe it. I just couldn’t connect.
I’ve never felt that feeling before and I never want to feel it again. I don’t think that I cried because I just stared at her, “Are you serious?” It was just disbelief and panic a little because of the baby.
I didn’t want to think too much about it because I didn’t believe the diagnosis. [I was] ten and a half weeks [at that point].
I took care of myself. All of the things that they say help you to stay healthy. I didn’t believe it. I just couldn’t connect.
Meeting the oncologist
One of the first questions: was this a planned and wanted pregnancy. I didn’t realize the significance of that at the time. I [said], “Yes, no question. Yes.” She [said], “We’re going to consult with maternal-fetal medicine and we’re going to see what we can do.”
At that time, she told me that I had B-Cell ALL. She did not know at the time if I had the Philadelphia chromosome or not so she wouldn’t know that result until the next day.
The next day, she told me I did have the Philadelphia chromosome.
[My oncologist] told me that 25% of patients get it. She said it makes it harder to treat and it makes it a high risk for relapse. I was still in disbelief.

Finding the right oncologist
The nurse told me who my attending doctor would be. I Googled the doctor and I read her reviews. She’s a pretty good doctor. Then once I talked to her, it was almost like she was a friend. She fit me well.
When I read the reviews, I saw what type of cancer she treated and she’s also a professor at Thomas Jefferson University; that was a plus, too. I think the biggest thing was how many years she’s been in practice.
The bedside manner, [with] a few other oncologists that worked in the same group, I didn’t get that same feeling. I just got the feeling that she really cared.
It was a very tricky situation, to be completely honest. It would have been easier to treat me if I weren’t pregnant, if I had decided to terminate.
One doctor told me, ‘We’d rather wait to start chemo when you’re in the second trimester. But we talked to oncology and they said you would not make it that long.’
Cancer and pregnancy
Video

Working with maternal-fetal medicine
I met with maternal-fetal medicine and they were phenomenal as well. One doctor told me, “We’d rather wait to start chemo when you’re in the second trimester. But we talked to oncology and they said you would not make it that long.”
That was another moment I’ll never forget because I was potentially weeks away from dying. It was just crushing. I don’t think I’ll ever forget that moment because it made it real.
It also made me say, “Okay, what do we have to do? Because I have a baby and we need to get across this finish line.” I’m a very straightforward person because I have an experience in that field. I’m not a doctor or anything. I understand a lot of what they’re saying. Sometimes that’s not such a good thing because sometimes it’s too much.
She told me, “We’re going to do everything that we can to get you and the baby through this pregnancy.” They work very well with oncology. They had meetings. She said, “We talk about you every day. We’re trying to make up the best plan for you.” [Those were] the scariest moments of my life.
I have a baby and we need to get across this finish line.
Discussing treatment plan with your partner
They gave me statistics and I knew that I would be harder to treat because I’m pregnant. They assured me that they believed that they could get me through this pregnancy.
My husband was there as we were discussing this. He and I didn’t have to talk because he knew that we wanted the same thing. We planned this baby. This is our first child. I said I want to carry.
The tough thing was there was a risk. They wanted to wait until I was in the second trimester because there’s a risk of bleeding to death, of a spontaneous miscarriage, in the first trimester.
I couldn’t wait [so] they were able to put me on steroids that calmed the cancer down until I got to the second trimester. My husband and I knew that because this is acute cancer, it’s fast-moving [and] you can’t wait.
My son pretty much saved my life. As long as I can get through this, then I want him with me.
You didn’t want to explain this to people. Especially now, this is a big thing. But if I had got to that point where I couldn’t continue the pregnancy… I’m glad that at the time, I had the option to say, yes, I want to or no.
I remember the doctors telling me I had up to 24 weeks to terminate and that just stayed on my mind a lot. They were just doing their job but my husband and I were on the same page because my son pretty much saved my life.
As long as I can get through this, then I want him with me. I know it would be easier if he wasn’t, but no. And I had this faith that he was going to be completely okay. I was afraid, but I just knew that he would be fine because I felt that I was doing the right thing for both of us at that time.
Giving birth prematurely
I was due in November, but I got to 32 and a half weeks. What happened was I ended up getting meningitis. My port got infected so I got meningitis and I was sick. His fetal heart rate dropped.
Everything [happened] at exactly the right time to make sure that he was here. There was a nurse in oncology who had the sense to call the OB-GYN. They rushed me upstairs. I had to have an emergency C-section. They couldn’t find his heartbeat for a couple of minutes.
I had this faith that he was going to be completely okay. I felt that I was doing the right thing for both of us at that time.
I’m just laying there and I’m in shock again but still feeling that he’s going to make it through the pregnancy. I’m not going to say it was an easy pregnancy but he met every milestone. He was growing at the right rate. He was perfect.

There was guilt on my part because I’m like, this is my fault because I have meningitis and now, he has to be born prematurely but he was completely healthy. They got him out. I think I went into the E.R. at 12:09. He was out by 12:33. He was 3 pounds, 8 ounces. Completely healthy.
You know how they said there’s a pot of gold at the end of the rainbow? That was my pot of gold.
He stayed in the NICU for 37 days. That was hard. But now I realize it was almost for the best because I was very sick then, too. I was in and out of the hospital myself. I was neutropenic. I wouldn’t have been able to take care of him.
Now, he’s nine months. He’s met every milestone. He’s perfect and it’s through all of the worst. You know how they said there’s a pot of gold at the end of the rainbow? That was my pot of gold. I forgot that I had cancer. I know all mothers feel that way, but it was just different.
Listen to what the oncologist and the maternal-fetal medicine say because sometimes, it’s the difference [between] life and death.
Support from family and friends
Be honest and upfront. They came to me after the fact. One person thought that maybe I had to terminate the pregnancy. Most people mean well but that’s not helpful to new mothers that went through that. If you can’t be positive, then don’t say anything at all. That’s usually the best thing.
Treatment plan
Sometimes Dexamethasone works, sometimes it doesn’t. But it worked just as she hoped for me. I did it for two weeks and then I checked back into the hospital for them to place my PICC line and start the Hyper-CVAD.
I was taking 40 milligrams [once a day for two weeks]. I got the munchies, but I felt better than I had felt in months because, for the past few months, I’ve been declining. I was able to walk the dog. It was almost scary because I didn’t feel like I was sick and that feeling is tricky because when I had to check into the hospital, I don’t feel bad.
My blast had gotten down to maybe 32 or something and I think they were at 82. So [the Dexamethasone] did take it down significantly.

Pre-chemotherapy scans
They did a bone marrow biopsy. They did the lumbar puncture but they had a hard time doing it. I have a rod in my back, so I had to get an Ommaya reservoir put into my scalp. It’s a little reservoir that goes right into your scalp and they can actually access your spinal fluid. So instead of getting the puncture, they would do it here. It was totally painless. When they would do it, it was painless, but 10 minutes later, I was just really, really sick.
[It’s] a one-time surgery where they put it in and usually, they keep it in for life. Mine got infected, so they took it out seven months later. I had that done so I didn’t need the lumbar punctures.
They also did an echo of my heart. They did CT scans just for a baseline before they started the chemo.
Chemotherapy
[My treatment plan] was altered. They omitted Methotrexate because that’s known to cause fetal issues with the baby.
Also my TKI for the Philadelphia chromosome, they wanted to put me on Ponatinib, but that was known to cause fetal defects. They tried me on Nilotinib. The data was mixed for that particular drug but at that point, I had to get on a TKI for the chromosome.
The Hyper-CVAD was divided into two parts, part A and part B. Part A, you got four drugs. Cytarabine, Dexamethasone, Vincristine, and Doxorubicin. Usually, it would be four nights in the hospital because you would get the Cytarabine every 12 hours. The B part would just be Cytarabine, but it would be a higher dose [of] Cytarabine.
I would be in the hospital for three days now at both A and B cycles. They checked my spinal fluid. I got chemo [through the reservoir], too. Each time, they had to do that.
Chemo was the hardest part. I believe that was Cytarabine, too, that I would get so sick 10 minutes after they would give it to me because I was just pregnant.
They would puncture [the reservoir] with a butterfly [needle], like what they would use to take blood. Then they would put a syringe on the end to take out some of the CSF. Then they would have a little syringe and they would push the Cytarabine through.
They took the CSF and gave the chemo [through the reservoir]… to ensure that the leukemia cells don’t go to my spinal fluid. Leukemia actually hides there a lot. They didn’t find any there, but they just want to make sure each cycle that it’s clean and get the Cytarabine in hopes that it doesn’t spread there.
You get a three-week break [in between part A and part B]. Sometimes that could extend if your counts didn’t bounce back. But for me, I was on time, luckily, each schedule. I was supposed to do it eight [times], but I had the baby that’s why I only did seven.
I [also] did Rituxan [at the same time]. I did eight cycles of that and that was pretty simple. You would just go to the infusion center. It took about 3 hours.
Side effects of chemotherapy
When they first gave me [the Rituxan], I had an allergic reaction to it. I started having an asthma attack. They jumped into action [so] I was fine. Each time I would go — and I think that one was once every 21 days — they would give me Benadryl before they would start.
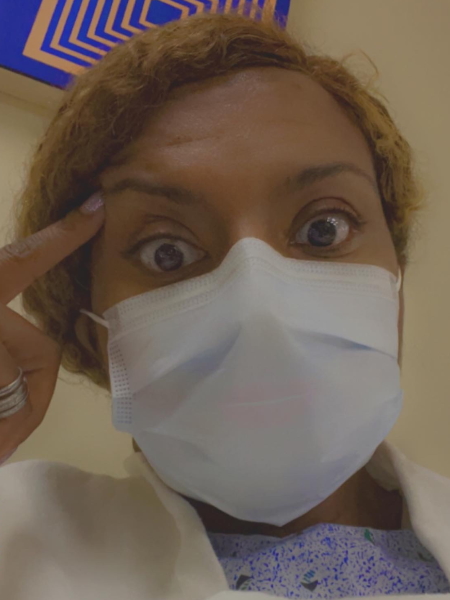
Hair loss, that one hit. I think I started chemo [on] May 5th. By about May 19th, my hair started coming out. I had my husband give me a buzz cut and probably by June 1st, most of my hair was gone. A few of the drugs caused that hair loss. It wasn’t just one for that.
I do know that the Cytarabine, the main thing was fevers. I would get fevers every single cycle. Sometimes I would end up back in the hospital because I had a fever and they thought it was an infection, but it was from the Cytarabine.
The fatigue was pretty bad but again, I was pregnant, so I don’t know how much was from the pregnancy and how much was from cancer. I noticed during the B cycles, the high-dose Cytarabine made the fatigue worse. So Cytarabine for me was tough.

I had food aversions. I didn’t have an appetite. I think that was a combination of the drugs, too. It was tricky for me because I started losing weight, but I was pregnant. One month, I lost 20 pounds and it was hard to balance. I have to eat because I have a baby, too. They actually gave me medicine to help with my appetite.
Brain fog. When I think about that whole experience, it’s almost like a fog because everything went by. I couldn’t remember things. I had to set alarms to take my pills. That was tough, too. I actually had thought about working. I was working from home while I was going through this therapy. I’m so glad I did not because I couldn’t think.
Joint pain. I also had a lot of joint pain. That actually may have come from the Nilotinib but because I was pregnant, I couldn’t take anything. They gave me a low-dose Oxycodone. The joint pain was a big one.
Vincristine gave me neuropathy but the doctor put me on Lyrica and that cleared it up completely. Lyrica definitely helps for the neuropathy.
With nausea, Compazine definitely helped me. I also use these anti-nausea patches behind my ears; that helped a lot. Zofran helped too, but it gave me headaches.
Immunotherapy
I finished active chemo in October. I had a bone marrow biopsy done in November. I was MRD negative [and] in the clear. [With] the Philadelphia chromosome, my BCR-ABL levels were at zero. But my doctor wanted to do blood tests every month to check those levels to make sure.
The first month was fine. Around Christmas, the nurse calls me. “Your BCR-ABL levels came back elevated. It’s 0.02.” We thought it was because we lowered my dose. We cut it in half from 30 to 15. My oncologist did not believe it was from that. She thought that it was coming back. But I said, “Can we increase the dose and maybe it’ll go down again?” We did that the next month. That was 0.01.
I have a conversation with my oncologist and [she said], “For long-term survival, this needs to be negative. If this comes back positive again, you’re going to need a stem cell transplant.” [It] was really devastating to know that the treatment, as much as we tried, wasn’t enough.
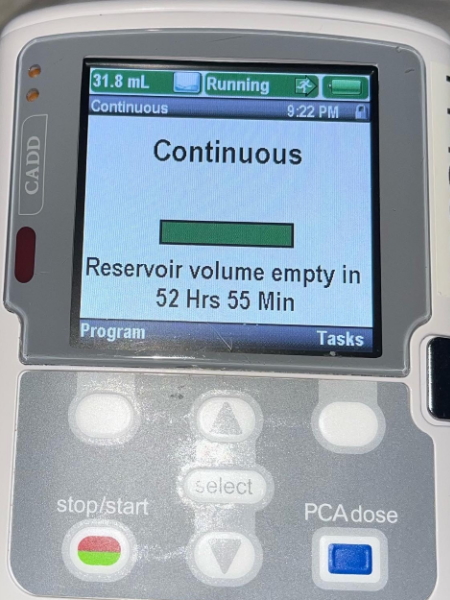
All of January and February were just stressful because I’m waiting for these test results to come back. After 0.01 in January, February [was] the big month. This has to be negative. It comes back at 0.153, so it increased. When I saw those numbers, I knew that I would be getting a stem cell transplant. My oncologist [said], “We need to get rid of that trace amount so I’m going to put you on Blincyto.”
I started Blincyto, the immunotherapy drug, the [following] week. That was originally supposed to be a three-day stay, but I actually stayed for five because I had an adverse reaction. My liver enzymes were off the charts. I had really high fevers [and] joint pain. It was so bad. They had to give me Dilaudid to calm the pain. We thought this would be an easier treatment because she said most people tolerate it well. I didn’t tolerate it well at all.
[It] was really devastating to know that the treatment, as much as we tried, wasn’t enough.
Stem cell transplant
Video
Getting the news
It was really tough. I never thought about dying before. But seeing those numbers, everything kind of flashed through my head. I went through so much and it wasn’t enough.
I knew there was no doubt that I’m going to get the transplant. I asked my doctor, “If I don’t get the transplant — and let’s just say the Blincyto gets rid of it — what are my chances of being cured?” She said zero. Not 50%. It would come back eventually and I wouldn’t live a long life.
As soon as she said that, I thought about my son. I have to do it. The main thing was knowing that I was going to be away from my son. I’ll be away from him, but it’ll be worth it because I’ll be able to be with him. That was really hard.
Also just the fear of the unknown. I’ve heard horror stories about stem cell transplants and all of this just kind of flashed through my mind when I saw those numbers. That’s why I said sometimes it’s a gift and a curse to understand things because I actually saw the numbers before my oncologist did. I saw the results and I knew what she was going to say that it was time to switch to a different treatment, to go more aggressive.
I thought it would be easier because I know what chemo felt like but it’s not because I know how bad chemo was for me.
I spent so much time researching outcomes. We, as humans, try to find a way out. We want to make this easier. Maybe there’s a treatment, maybe there’s this. But everything that my oncologist was doing, that was the latest, that was what should be done, so I knew that there was no way around this. I just have to go through it again. It took a while.
To me, it might have been more devastating than my original or just as devastating as the original diagnosis. I thought it would be easier because I know what chemo felt like but it’s not because I know how bad chemo was for me. You think about that and it’s tough.
It’s really hard to keep your mind focused on something other than that. But for me, I still keep my focus on Michael. He’s trying to crawl now. In a couple of years, I want to get him T-ball and things like that. I think about that and I said, “Okay, let’s do this.”

It’s been an uphill battle from February till now because I’m actually allergic to the Blincyto so my eosinophils have been really, really high. I’ve been having asthma symptoms. I haven’t been able to breathe for weeks but Blincyto’s saving my life right now. It’s a risk versus benefit thing. But it takes a lot out of me.
I’m fatigued. Sometimes it’s hard to take care of the baby. I actually went back to work and I had to stop because it was too much. Now we’re just waiting for the stem cell.
Blincyto was the latest and the best. We hoped [there] would be no side effects but sometimes you get the long end of the stick.
Preparing for allogeneic stem cell transplant
[Depending] on how my numbers rebound, my doctor told me to expect to be in the hospital [for] 4 to 6 weeks. There’s a week before you get the cells and then you have to stay until your counts recover.
[For] the first 100 days, I need to isolate [myself] because I’m going to pretty much be like a newborn baby. I’ll get to see Michael within that time because luckily, he doesn’t go to daycare.
We’re going to stay in Philadelphia for a month so that we’re close to the hospital. I probably won’t get to see him at all then, which is tough.
I’m going to go through intensive chemo and full-body radiation. [Radiation is] for four days then the chemo is for three days. They’re going to completely wipe out my immune system.
I’m going to get the cells from my brother and hope that I don’t run into graft versus host disease (GvHD). My brother’s actually a half match so I believe I’m going to have chemo a few days after the transplant, too.
My transplant specialist, she’s amazing. She’s been very positive about the experience. She’s told me I definitely would get diarrhea [and] I’ll probably have nausea. But she told me, “If you got through being pregnant and chemo, I’m not worried about you.”
Statistically, 30% of transplant patients don’t make it through the first year. But reading [the] literature, I found that most of those people are older people with pre-existing conditions, which is why before you get the transplant, you have to get so many tests to make sure that you’re fit for it.
We automatically assume because I’m relatively young that I’m fit for it. They did an echocardiogram of my heart and found that my ejection fraction had dropped from 65% to 45% within the year. I saw a cardiologist. He said he didn’t think it was from chemo. He thinks it was from the pregnancy. I had to get more tests done on my heart.
Then you have to go and do a pulmonary test. I failed that and that’s because I’m on Blincyto and I’m allergic to the Blincyto so it’s hard for me to breathe.
I was actually supposed to get this transplant [on] June 13th but because of the heart issue and the lung issue, everything has gotten pushed. That actually scared me because I know I need this transplant.
They did another echocardiogram of my heart and the ejection fraction is back up to 62%. I have my pulmonary function test again, so hopefully, I’ll pass that.
[They also make you take a] mammogram. You have to get a pap smear. Anything that you can think of, they make you do it.
I’ve only had one cavity in my whole life. After chemo, you have to get clearance from a dentist. I couldn’t get clearance because I needed two root canals and I had three cavities. The dentist told me that’s most likely from chemo. It does a number on your teeth.
I had to spend quite a bit of money to get the root canals and crowns, but that’s something that you have to get. You can’t have bacteria just floating around in your mouth after [the stem cell] transplant because you don’t have an immune system [so] I had to get that done.
They’re very thorough and even though I want to get this over [with], I’m glad that they are so thorough. A stem cell transplant [is] almost like a factory reset of your body. It takes a lot out of you.
I appreciate them wanting to make sure that they get to the bottom of everything and make sure I have the best chance of getting through it. My doctor did say there’s a 70 to 85% chance that they’ll secure it so I think that those are good numbers compared to me not getting the transplant. In that aspect, I feel blessed.
I want to get it done and over with so I can move on. My doctors are positive. They haven’t scared me. My oncologist, she’s been positive. She’s glad that we figured out where this allergy was coming from. So that’s kind of where I’m at, just waiting.

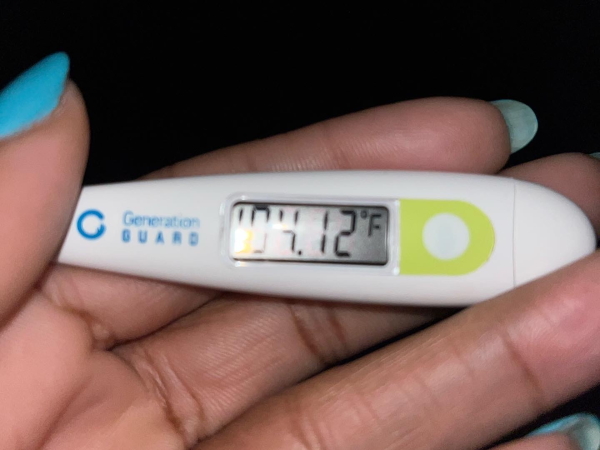
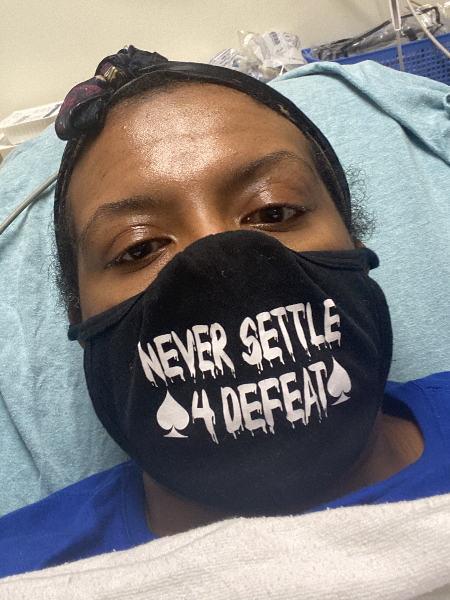
Waiting for the stem cell transplant
Right now, I’m on steroids. It’s like night and day. I would be running fevers from the Blincyto. Two weeks ago, I had a 104-degree fever. I went to see a pulmonologist and he [thought it was] just asthma and kind of dismissed me. I knew it was something else. I thought he would put me on steroids but he didn’t. He put me on inhalers and those didn’t work. This is week after week, I’m sick. Then finally, my oncologist says, “I’m going to put you on Prednisone,” and the Prednisone is working.
Post-stem cell transplant regimen
I’m not sure what chemo [I’ll be on]. This just came up. The doctor was saying you might have to get more, but they never broke down what type yet. We haven’t gotten that far because of all the things that came up, but I think it’s just for a few days.
I also need two more intrathecal chemos but because [the reservoir] isn’t in my head anymore, I have to get it in my spine. They [will] put me under twilight so I don’t feel it. I have to get two more intrathecal chemos and that’s Methotrexate.
Words of advice
The main thing is to focus on this child that’s growing inside of you and that this too shall pass. Once you have that baby, you’ll forget all about the things that you went through. People told me that and I didn’t believe it. I forgot about all of that because you have this baby, against all odds.
People were afraid to ask about my pregnancy because they knew I had cancer. It was almost like they pitied you but that bothered me. You have to rise above that and focus on the baby, focus on life after cancer. That’s what kept me going.
What I’ve learned was to focus on [Michael]. My sole purpose was to bring him into this world. I cared about myself, but thinking of him — thinking of taking him to Disneyland, going on trips with my husband and the dog and the baby, all of these things that I’ve always dreamed about — kept me going. It helped.

Focus on life after cancer. That’s what kept me going.
You can’t be around negativity. With cancer, you have to really be positive. People say to me all the time, if I were you, I would be depressed. Why would I be depressed? That’s not going to fix this cancer.
There are a lot of things that knock you down, like side effects, and sometimes you want to quit. When you feel that urge to quit — I don’t know if it’s your dog, your kid, your spouse — you have to have something to hold on to, something to look forward to in the future. That got me through.
Stay off of social. I joined these Facebook groups and they scared me to death. It was too much. I had to leave the group or just go in when I was mentally okay with doing it.

Another big thing: you have to listen to what the oncologist and the maternal-fetal medicine say. Everything. Sometimes it seems like they’re overbearing, but you have to listen to them because sometimes, it’s the difference [between] life and death. You might know someone else who had ALL that did this regimen — no. Just listen to your oncologist.
If you’re not comfortable with your oncologist, go somewhere else. I’ve come across people who said they had horrible oncologists. This is something that’s too precious. Your life is too precious. Just go somewhere else.
Drinking a lot of fluids, proteins, [and] things like that helped me, especially because I was pregnant. Chemo dehydrates you and you have to replace that. I would drink like a gallon of water a day. I don’t know if it made a difference, but I didn’t have any issues with being dehydrated.
I look at it as I want to get through the first year. Step by step. Try not to look too far into the future and just take things as they come.
Keep with friends and family. If you need help, don’t be afraid to ask for help because you need a good support system around you.
Remember it’s a marathon, not a sprint.
Another big thing is your social worker. I never really knew what a social worker did until I had cancer. I have a phenomenal social worker and she’s helped me because a lot of this is mental.
You have to have this strength that you’ve never had before and you know you have to do things that you’ve never done before. Different ways of coping. I got on Wellbutrin [and] that helped me. You can’t be afraid to ask for help because it’s a lot.
Find something that you like. Try to do things that you like doing. I love going for walks, so if I’m feeling up to it, I walk [and] I get on the bike. I keep moving. That helps a lot too.
Usually the two treatments for ALL, either you go to maintenance chemo for two years or you do the stem cell transplant. Neither one of them are easy. I did maintenance chemo for two months and it was hard. It wasn’t easy on me and I would have to do that for two years.
I know [it all] sounds daunting right now, but it’s a lifetime thing. Remember it’s a marathon, not a sprint.

Inspired by Renata's story?
Share your story, too!
Acute Lymphoblastic Leukemia (ALL) Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)


