Kayla’s Stage 3A Refractory Hodgkin’s Lymphoma Story
Kayla was first diagnosed with stage 3A Hodgkin’s lymphoma, but after undergoing ABVD chemo, found out cancer was still there. It was possible she actually had gray zone lymphoma, so they treated her like a relapsed patient, undergoing more chemo and a transplant.
Now in remission, Kayla highlights dealing with 2 diagnoses, losing hair from chemo and using naturopathic medicine.
- Name: Kayla T.
- Diagnosis:
- Hodgkin’s lymphoma
- Classical
- Refractory cancer
- Diagnosed as gray zone lymphoma, treated like relapsed patient
- Staging: 3A
- Symptoms:
- No real symptoms, pulled muscle in chest that prompted doctor visit
- 1st-Line Treatment
- Chemotherapy:
- ABVD
- 7 months
- Gemcitabine, dexamethasone & rituximab
- ABVD
- Chemotherapy:
- 2nd-Line Treatment
- Busulfan & cyclophosphamide
- High dose for 1 week just before SCT
- Radiation targeted to chest
- Stem cell transplant
- Busulfan & cyclophosphamide
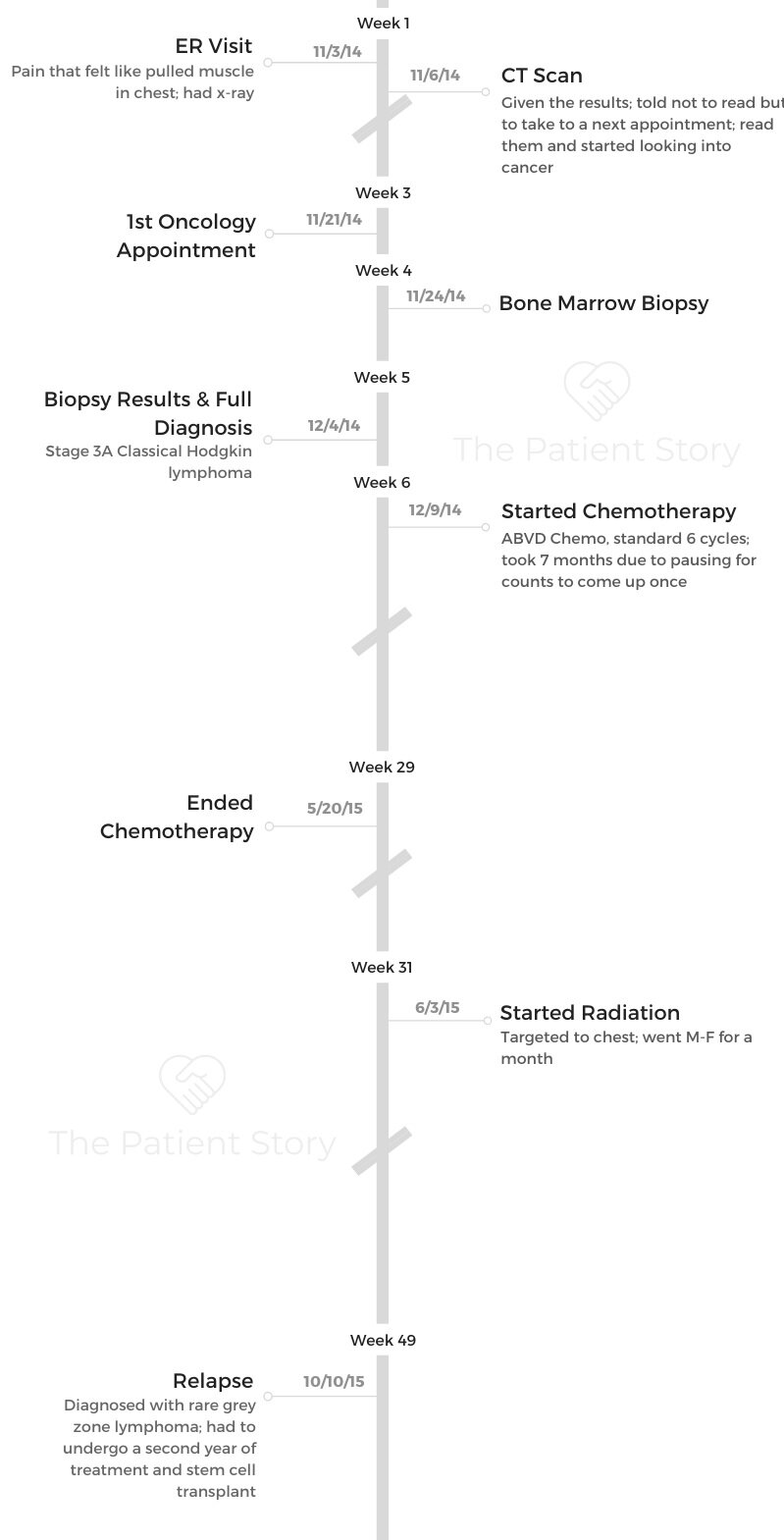
- Diagnosis
- 1st-Line Treatment
- Refractory Cancer & 2nd-Line Treatment
- Reflections
- Did you celebrate being in remission?
- Going in-depth about the hair loss and emotional impact
- Advice for someone who’s about to lose their hair
- Using naturopathic medicine as a complement to western medicine
- Being a student with cancer
- Finding your cancer community
- How did cancer shift your perspective?
- What would you say to someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

I don’t like to bullshit. This is going to be a shitty experience. [That’s] probably the first thing.
You are going to get through it, though. It might take you longer than other people. Your recovery might look different from other people.
But you are not alone.
Kayla T.
Diagnosis
What were your 1st symptoms?
Just before Halloween, I was vacuuming behind my TV at a weird angle. I felt a rip in my chest. I thought I pulled a muscle.
I felt okay, but there was an immediate tearing sensation. A few days later, I was at the movies with my friend and then-boyfriend.
I remember so distinctly — when I went to sit down in the seat, all of a sudden, it felt like there was a vacuum in my chest. It was hard to breathe, and it was cramping.
I didn’t want to cause a fuss, so I pushed through it for the movie. I was drinking water and taking shallow breaths. From them on, for about a week or so, I just struggled.
I continuously had that ripping and cramping sensation. If you were sitting close to me, you could hear what sounded like a water bottle being crushed.
That was the sound my lung was making.
After about a week and a half, my mom said, “Enough is enough. I’m taking you to the ER because that doesn’t sound normal.”

Hospital walk-in clinic visit
We actually wound up at a walk-in clinic next to the hospital first. The doctor had no idea what was wrong, but I could tell it was freaking him out.
He said I needed to go to the hospital and get X-rays. We did that. They did the scan and some blood work.
I get bronchitis every year, so he compared my X-rays to ones I had a year before.
He did say my lymph nodes looked a little swollen, so he wanted to take it to the radiologist just to be sure. I didn’t have a pulled muscle or anything.
3 days later, I was sitting at the art gallery I worked at. I got a call saying I had been scheduled for a CT scan.
They didn’t really tell me why. I just knew I was scheduled to get it.
How did you get the initial diagnosis?
I took my CT results — which they told me not to look at, but of course I did — to my doctor. I had looked up some of the things on the sheet, so I kind of already knew what was going on when I went in.
The respirologist (pulmonologist) who did my biopsy told me I needed to see an oncologist because he was pretty sure I had lymphoma.
I said, “Oh. Okay.”
I was very unemotional about it. It didn’t really affect me as I thought it would.
My mom was like, “Are you okay? How are you feeling?”
I said, “I don’t know. I just know I have a test tomorrow.”
I was so focused on my studies, and that really distracted me from the whole thing. I’m the kind of person who just does stuff. When he said it, I was just like, “Okay, what’s next? Let’s do it.”
Tests and scans you underwent to get the official diagnosis
I did the CT, lymph node biopsy, another CT scan, a PET scan and a bone marrow biopsy.
After all that, I got the final diagnosis. The bone marrow biopsy was able to tell if it was stage 3 or 4.
Stage 3 for me meant I had tumors above and below my diaphragm, but I was 3A because I was asymptomatic.
I still didn’t freak out. I just wanted to know what I had to do.
Describe the bone marrow biopsy
What they have to do is get your bone marrow and plasma out of your bone. They go into the biggest bone in your body, which is in the femur and hip area, and extract from there.
Your skin all feels frozen in the area. It sounds awful because it really is, but they stick a giant needle down into your bone through your back.
If you’ve ever put your hand to a vacuum hose, it feels like that times 100 in your back. Since they’re going into your bone, it feels like the entire surrounding area is being sucked into a tube.
At the end, they showed me their sample, and it’s so tiny! I was like, “All of that just for that?”

1st-Line Treatment
Discussing your treatment plan
After all the results came back, my oncologist and I had a discussion. She said typically, they treat it with ABVD chemo over a 6-month period.
Then I’d get a scan and see if I needed radiation or something. She asked when I wanted to start, and I told her I wanted to start the next week.
Right before, they did a bunch of blood work and breathing tests. I had a bunch of tests to make sure I was healthy enough for chemo.
Getting a PICC line
For the first chemo, I didn’t have any external IV, and that was excruciating. They made me an appointment to get a PICC line put in before the next one.
The PICC line basically goes into your arm and up to your chest cavity. It makes blood work and everything so much easier.

How was your first ABVD infusion?
I wasn’t too nervous. I’ve never been squeamish around hospitals. I really didn’t know what to expect.
You see all these cancer movies, so you think you might know, but it’s really not the same.
The nurses all pay special attention to you because it’s your first day. They just want to make sure you and your body are handling everything okay.
They go over each drug in detail, what the side effects might be, and how long each drug should take to infuse. Then a resident came and told me more about the side effects of chemotherapy.
I was told what to expect and what was normal. She also gave me some hospital support network resources, should I want to use them.
Because I didn’t have a PICC line the first day, my infusion took a long time. It took 6 hours for all the drugs. Some of them hurt as they go through your veins, so they had to slow the infusion rate and add saline every time.
That’s another reason I opted for the PICC line afterwards, because I didn’t want to go through that pain every time.
It was weird because I was 21, and I was here in this room with all these old people. I was like, ‘Cancer doesn’t discriminate!’
I would say it was more uncomfortable than anxiety-inducing or awful.
Side effects of ABVD chemo
When I was finished, I felt fine. I didn’t feel sick or weird. I felt a little heavy, but that’s about it. Then later that night, I puked everywhere. I ate a big bowl of soup and puked it all up.
I also started having really bad upper body pains. I had to get some morphine the next time I went in because of it.
The side effects came in different stages for me. For the first 2 months of my treatment, I had a lot of upper body pain, and it was also very cold.
I did have some vomiting, but the anti-nausea medicine is actually what was making me nauseous. I figured it out after the second time.
I told my nurses I was going to stop taking it, and they were fine with it. The nausea stopped. Never puked again.
After the first couple of months, the fatigue really started kicking in more. It’s harder and harder on your body the longer you’re in treatment.
I was still in school, and I was working a part-time job. I was able to maintain a normal life to some extent.
The biggest side effect I had was weight gain. I was on steroids for both years I was in treatment. They make you want to eat more, and even though I wasn’t eating that much more, they made me swell.
I was pale and swollen, and I was gaining 2 to 3 pounds consistently every week. I really wasn’t eating a lot, but it just kept adding up.
I gained 25 pounds during my first year of treatment. That was a really big blow. I had never weighed that much before, and I was normally very active.
That weight gain also caused quite a bit of pain because my body wasn’t used to supporting that much weight. I wasn’t working out at all at one point because I was just too tired.
Hair loss
My hair fell out, but I kept about 30% of it. That was the worst for me besides the weight gain. I thought, “If I lose my hair, I can’t do this.” My hair was what defined me.
Even now, if I had to ever go through treatment again, losing my hair would be the worst part because you look at yourself in the mirror, and you don’t even know who you are. It just makes you feel worse than you already do.
»MORE: Dealing with hair loss during cancer treatment

What was radiation like?
Halfway through my chemo, they did a scan. Some of my tumors had shrunk, but they hadn’t shrunk enough.
At the end of chemo, they decided to do the radiation. I did one month of radiation targeted to my chest.
You go Monday through Friday. It’s really quick. I would hold my breath, and the machine would draw lines over my body. They made me a custom head mask that kept me in the same place every time. It took all of 15 minutes every time.
The only side effects I got from radiation was a dry throat and mouth and a mild sunburn on my chest.
Radiation was a walk in the park compared to chemo. I would take it over chemo any day.
I finished my chemotherapy and radiation treatment in June of 2015. In September, I went back for a follow-up and found out that my cancer was (still there).
Refractory Cancer & 2nd-Line Treatment
Processing the news of refractory cancer
I was really focused on losing the weight. I wanted to get control of my life again. Throughout most of my university, I took summer classes, but this year I didn’t. I just focused on recovering and losing weight.
I thought I was getting back to normal. I went in for a follow-up appointment.
That’s when they told me my treatment hadn’t worked and the cancer was still there.
I was really frustrated because my radiation oncologist told me there was a possibility the original treatment plan didn’t work because they had misdiagnosed me with the wrong cancer.
That really boiled my blood. He said he couldn’t prove it, but that’s what he thinks happened.
We had a conversation about what to do moving forward. We didn’t want to do the same chemo regimen. They were going to treat me as a relapsed patient even though I was never officially in remission for those 4 months (refractory).
As a relapsed patient, my new treatment plan was high-dose chemotherapy and a stem cell transplant. He told me I was going to have 3 months of really high-dose chemo that would kill everything in my body.
Then they were going to harvest my stem cells, give me more chemo for a week, and then they were going to give me my stem cells back.
He also said they would probably go ahead and do more radiation after the stem cell transplant just to be safe. He wanted to start right away.
»MORE: Read more relapsed/refractory cancer stories

2nd-line chemotherapy
I started chemo and got it once every 3 weeks. The first week afterwards, I couldn’t sit up or get up at all. I was horizontal for 7 days. The next few days, I was slowly able to walk again. It was really hard to go to school.
I had more weight gain because I was on steroids, but I didn’t have an appetite because I was so tired. I lost all my hair this time. I had a rash, and I got a lot of mouth sores.
What was the stem cell process like?
I went into the hospital, and they hooked me up to what looked like a dialysis machine. Blood goes out, stem cells get taken out, and it gives your blood back. They collected a lot of cells and stored them in the freezer.
That’s when I was referred to the stem cell transplant unit. I was in the day hospital since I was using my own stem cells for an autologous transplant.
I would wake up, go spend all day there, go home to sleep and head back the next morning. I did that for about a month.
They were prepping my body for the transplant. I had a lot of IV drugs. I also got the strong chemo. It’s a 2-day process for this one.
SCT chemo side effects
When I got it the first time, I instantly threw up. I had really bad upper body pain, so they sent me home with more morphine.
I got 2 days of rest after that. They pumped me up with saline and hydration. On the fourth day, I got my stem cells back. It took like 3 minutes.
It’s gross because the whole room starts to smell like creamed corn and garlic. Your sweat smells like that. I stunk for about a week.
Recovery after transplant
I had to be careful for 100 days. I got an infection at one point and had to go to the hospital to get a carry-out bag of antibiotics to carry around with me.
They told me no physical contact with other people, no going to the mall, no takeout. I had to go to the hospital pretty much every day.
It wasn’t that bad. I’m pretty sure I went to school still. I don’t think I was supposed to, but I went when I had to.
One day, I went in for a blood work check, they told me my numbers were going up. There was one point where my nurse wanted to give me a transfusion, and I said absolutely not.
I’m really into natural healing and nutrition, so I asked my naturopath and started Googling how to bring my platelets up.
I read that papayas are really good for that, so I was eating a papaya a day. The next time I went back, my platelets were much higher.
I hate when people tell me I can’t do something or that naturopathic ways of living don’t work. You have to be open-minded about these things.
There has to be some kind of compromise in treating your body with natural and conventional medicine.
I personally think I had a better success rate and recovered faster because I was eating healthier food.
Reflections
Did you celebrate being in remission?
I was so over cancer at that point that I was like, “Okay, whatever.”
I was graduating university at the same time, so that was my reward. I also planned a trip with my friend to San Francisco a few weeks after they released me from the hospital.
I don’t really remember celebrating necessarily because I still had so much shame. To the outside world, I was like, “Okay, let’s get back to my life,” but inside, there was chaos.

Going in-depth about the hair loss and emotional impact
My doctor told me all of my hair would probably fall out, but I’m stubborn. I basically willed my hair to stay in my head. I lost a lot of it, but I still had a thin amount.
When it started falling out, I remember one morning waking up, and it was just all over my pillow.
A few days later, I was brushing my hair in the shower, and clumps just started coming out. That shower alone probably took out a good 20% of my hair.
I had this weird ritualistic moment, and I was like, “Should I keep this hair? What would I use it for?” I was studying art, so I thought I might use it or something, but I never wound up using it.
I had an issue with showing people how I really felt at the time. Even though I was telling everyone I was fine on the outside, it really brought me to a dark place. I felt very disassociated from who I was.
I lost all of my self-esteem. It was really hard for me to tell other people that. When I showed my mom the trash bag full of hair, she freaked out and asked if I was okay. I was like, “Yeah, it’s no big deal.”

It was very devastating for me. I did everything I could to keep the hair I had left.
I wore caps at night, I bought protein shampoo, and I was also taking some naturopathic supplements to support my hair and skin.
During my first year of treatment, I was taking curcumin, vitamin D, BioSil and a green protein I would put in drinks. I had bought hair extensions and sewed them into a hat.
Advice for someone who’s about to lose their hair
It’s gonna suck. You have to somehow be ready for that “oh shit” feeling to hit. Some people embrace it and shave their head.
I was never that brave because I was so ashamed about having cancer. I wasn’t able to be proud of my fight.
My advice is: if you’re like me, go buy yourself a wig and some fun hats. Come up with a creative solution that allows you to express yourself.
I couldn’t afford a wig at the time, so that’s why I did hair extensions. You can sew them into just about anything. If I could have afforded a wig, I would have definitely gotten one.
Do something for yourself within your means that gives you your control back. Being able to style something on your body, even if it’s not your own hair, is really important.
When you look in the mirror and don’t recognize yourself, it’s really hard. If you can do something to make yourself feel better, do it.
»MORE: Dealing with hair loss during cancer treatment
Using naturopathic medicine as a complement to western medicine
Everything started kicking off when I was 18 or so. I was having a lot of chronic pain, headaches, and just generally feeling unwell all the time. I didn’t know what was going on. I got an allergy test done, and it revealed some allergies I knew about and some I didn’t.
I was like, ‘Okay, I’m an adult now. I need to take care of my body.’ I’d always taken care of my body, but I wanted to be more conscious and aware of what I was putting in my body and how to support myself more holistically.
I saw a naturopathic doctor, and we came up with a plan together. I ended up getting diagnosed with fibromyalgia, which is a chronic pain condition that they really don’t know anything about.
I was at the rheumatologist, and she said, “If you’re not sleeping well, I can give you a pill.” I thought, “I don’t want a pill. I want to figure out the reason I’m not sleeping and the cause of the pain and fix it.”
I told the naturopath what was going on and asked if she could help me. I’ve been seeing her for 8 years now. We’ve worked really hard to support my adrenals and focused a lot on the foods I was eating.
I had been eating a lot of nightshade vegetables. They’re very inflammatory. I was already dairy-free, and I went gluten-free. I started implementing little changes in my life. I felt night and day better within a few months.
She has always listened to everything I have to say. She never discredits anything I say or makes me feel unheard. I trust her so much. She’s helped me more in 6 months than any doctor has in my whole life.
Being a student with cancer
It was definitely weird. When I got my official diagnosis and everything, I emailed all my professors and told them what was going on.
I told them I wasn’t planning on dropping or anything, but I asked if I could do more work from home if it was okay with them. They were all super cool about it and so understanding. I went in when I could, and if I had chemo or didn’t feel well, I didn’t go.
Because I was in my fourth year at the time, I had a lot more days where I didn’t have classes. I tried to schedule my classes around that. I studied fine art and art history.
I was in my sculpture class presenting my project for the semester, and I had to tell everyone, “I’m sitting for my presentation not because I’m lazy, but because I just had a bone marrow biopsy.”
It was awkward telling my classmates more than my teachers. I feel like they all treated me like an alien after that.
I had this one teacher who told me it was okay if I needed to take a year off, and I was like, “No. I’m in school because it’s keeping me going.”
School helped motivate me. I almost treated school as a metaphor for myself.
Going to class, doing my projects and handing them all in on time was like me showing cancer that I was going to beat it.
I wasn’t very emotional. I didn’t talk about cancer because I didn’t want to. I think I really took what I felt and put it all into my schoolwork. I treated school as a metaphor for my body.
I thought, “If you just go to this lecture, if you just do this next project, you’ll be okay.” I equated graduating with me making it and living.
Finding your cancer community
In the summer, I was watching TV with my mom. I turned to her and said, “I think I need to talk to somebody because I hate everything and everyone. I’m angry all the time.”
I fully admit it. I was an asshole to everyone. We talked to my oncologist, and he set me up with a therapist who deals with cancer patients and survivors.
Going to see her for the first time was the first time I had openly talked about how I felt.
I was still staying on a very surface level. I wasn’t getting to the nitty gritty or anything. At that first session, she introduced me to Young Adult Cancer Canada. They are an organization who help young adults with or after cancer connect with other young adults who get it.
She told me they were having a retreat a few weeks later. I told her I didn’t feel like sitting around a fire with a bunch of people with cancer.
She said, “It’s not like that, but I understand where you’re coming from. Go on the website and just see what happens.”
I went home and looked into it, so I filled out the form. They accepted me, and the next thing I knew I was on a flight to Vancouver to hang out with a bunch of strangers. I’ve never felt more connected in my entire life.
I still wasn’t very open because I didn’t know how much I was allowed to feel. Even without sharing as much as I should have or wanted to, being able to hear these stories of other people who had been through what I had been through was enough for me.
That retreat pretty much changed my whole life. I go to all their events. I help people who are in the same place I was, so it’s very rewarding. Joining that community has changed me forever.
How did cancer shift your perspective?
I have a perspective now that says, “Live your life and take in moments.”
I feel like everyone is always in a rush to get to the next place, to get the next big thing, or to be better at this or that. That’s fine, but in doing that, you miss all these nuances in life that are never going to happen again.

Having cancer really taught me to slow down, appreciate what I have now, and notice the moments.
I don’t take what I have for granted, and if I have a goal, I don’t say, “I’ll start tomorrow,” anymore. I start today because I might not have tomorrow.
It also really taught me a lot about mental health in general. Suppressing your emotions is only going to hurt you and people around you more in the long run.
By not being honest with yourself, you lose that connection with what you’ve gone through, and it makes it harder to heal.
I never talked about how I felt when I was sick, and I didn’t want my parents to talk about it with anyone because I was ashamed. Now, I’m like, “Tell the world!” By sharing your story and what you’ve gone through, you can not only help heal yourself, but others going through something similar as well.
Being brave isn’t always about smiling through the pain. It’s about being vulnerable and sharing how you’re feeling.
What would you say to someone who has just been diagnosed?
I don’t like to bullshit. This is going to be a shitty experience. [That] is probably the first thing.
You are going to get through it, though. It might take you longer than other people. Your recovery might look different from other people, but you are not alone.
There are people around you who want to help you. You just have to take that step and ask for help. I never thought there was a light at the end of the tunnel for me.
It’s taken me years to realize that there is light. It just takes time. We don’t want to wait as human beings, but this is something that only time will heal.
Effort from you being honest is what will help move that along.
If you’re having a hard time, connect with someone online. Find a social worker who can give you resources.
If that’s too much for you, try doing something to connect with yourself. Write in a journal and accept your feelings.

Kayla’s YouTube
Thank you, Kayla, for sharing your story with us!
Inspired by Kayla's story?
Share your story, too!
Gray Zone Lymphoma Stories
Kayla T., Hodgkin's Lymphoma, Stage 3A
Cancer details: Possibly misdiagnosed the first time; later diagnosed as grey zone lymphoma
Symptoms: Pulled muscle in chest
Treatments: ABVD chemo, radiation, high-dose chemo, stem cell transplant
Hodgkin’s Lymphoma Stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s Lymphoma, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s Lymphoma, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta
Brescia D., Hodgkin's Lymphoma
Symptom: Swelling in the side of her neck
Treatment: Chemotherapy: 6 rounds of ABVD





