Danielle’s Stage 4 Metastatic Colon Cancer Story
After overcoming stressful family matters, Danielle assumed her gastrointestinal issues were her body’s response to stress. But with ongoing constipation and abdominal pain, her husband encouraged her to go to the doctor. Her primary care physician referred her to a specialist which led her to get a colonoscopy that revealed she had a 7-centimeter tumor in her intestine.
Many scans and tests later, Danielle was officially diagnosed with stage 3 colorectal cancer, thus beginning her cancer journey. Having received breast cancer screenings since her 20s due to a family history, Danielle later discovered that she was able to get additional cancer screenings which she now advocates for.
Danielle shares her cancer story with us, including her thoughts on working while undergoing cancer treatments, the importance of getting examined for new symptoms, how she reacted to learning she had metastasis, her ileostomy experience, and her advice for those on their own cancer journeys.

- Name: Danielle A.
- Diagnosis (DX):
- Staging:
- Stage 4
- Symptoms:
- Abdominal pain
- Constipation
- Treatments:
If you don’t feel well, if something is wrong, you know your body better than anybody else does. Go to the doctor. If the doctor doesn’t pay attention to you or blows you off, go to somebody else. Do not wait.
Danielle A.
The interviews have been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Symptoms & Diagnosis
- Treatment
- Getting tests and deciding on a treatment plan
- Having surgery to remove the tumor
- What was your staging and official diagnosis?
- Was your cancer diagnosis related to a genetic predisposition?
- Starting chemotherapy
- What did your follow-up scans show?
- Did you have side effects from chemotherapy?
- Are you on any clinical trials?
- Living With Cancer
- Ileostomy
- Quality of Life
- Were you working throughout your cancer treatments?
- Working through insurance and the cost of cancer treatments
- Do you have advice for those on cancer treatments who want to work?
- Do you still get scans?
- Coping with scanxiety
- The difficulty of having age requirements to get cancer screenings
- Missing cancer diagnoses in young people
- Reflections
Symptoms & Diagnosis
Tell us about yourself
My name is Danielle Archer. I am a wife, a mom, and a mental health therapist. I live in central Florida by way of New York. I’ve been in central Florida since January of 2004. In my spare time, when it’s not blazing hot outside, we like to go to the amusement parks. My husband and I like to go to concerts, hanging out at home. We’ve got really great neighbors and we like to do stuff with our neighbors. Watch movies, listen to music, things like that.
What were your first symptoms?
I was having pain in my abdominal area. I would have to go to the bathroom and I would go, but nothing really would happen. It felt like I was hitting a wall and it was painful.
I want to say it was around September of 2018, I started having some, of what I thought were, gastrointestinal issues. Years back, I lived in California for a couple of years and when I lived in California, I was diagnosed with IBS.
There was a lot of stress in my family. My daughter, who’s now 21, was diagnosed with gastrointestinal stuff. We had just gotten through all of that. I had thought at the time that because everything had calmed down in the family, my body was responding and I was just feeling really off.
It was September or October and I was having pain in my abdominal area. I would have to go to the bathroom and I would go, but nothing really would happen. It felt like I was hitting a wall and it was painful. I would get up and I’m like, No, I still have to go, and nothing would happen. This was repeated.
»MORE: What Does Cancer Feel Like?
Did you tell your doctor about your symptoms?
I called my primary care physician. They said to try this and that. Finally, my husband was like, “Just go to the doctor. Go get checked out, and see what she says.”
I’m not really a doctor person because I don’t like doctors. Thankfully, up until now, I’ve never really been sick so I haven’t had to go other than my physical exam.
I went to see my primary care physician and she’s like, “All right, what’s up? You never come here other than for your annual exams. I know something is wrong.” I’d made a list of all the symptoms that I was experiencing. She was like, “All right, it’s probably nothing, but some of these symptoms I’m not comfortable with. Let me send you to a specialist.”
I went a couple of weeks later to a specialist in November of 2018. He listened to my symptoms, He’s like, “You’re a little bit older.” I was in my early 40s at the time. “You’ve had a couple of kids. It sounds like you may have pelvic floor disorder.” I looked it up because I didn’t know what that was, and I looked at the symptoms. I’m like, that kind of tracks, cool. He’s like, “But just to be on the safe side, just to rule everything out, I’m going to do a colonoscopy and endoscopy for you. I want to make sure we’re not missing anything.”
Getting colonoscopy prep
I scheduled the colonoscopy and endoscopy for December 31st of 2018. My husband’s an attorney. I knew it was a day that he wasn’t going to have to be in court. I was like, let’s just do it and we went at 6:00 in the morning.
I did the prep before. If you haven’t had a colonoscopy, if you do a prep, you don’t go anywhere that day, ever. But nothing happened when I did the colonoscopy prep. I did [go to the restroom] a little bit, but not very much. Not like what’s supposed to happen when you do a colonoscopy prep.
Family history of cancer and getting preventative screenings
It was just painful and excruciating. I couldn’t figure out what it was. It was really hard to describe what the feeling was to anybody, even to my doctor. Because of my age, I was 42 at the time, so they didn’t really look at it. I know now that I was eligible for screening for other types of cancer.
If you have a family history of cancer, it’s not just this type of cancer you can be tested for. You can be tested for everything. I found that out the hard way.
My mom passed away from breast cancer when I was 16, so I had been getting MRIs, CTs, and mammograms since I was 29 years old. I wasn’t aware that because of my mom’s family history of breast cancer, I was actually eligible to be tested for other types of cancer early. If you have a family history of cancer, it’s not just this type of cancer you can be tested for. You can be tested for everything. I found that out the hard way.

»MORE: Genetic Testing For Cancer
Receiving a diagnosis post-colonoscopy
When I did the colonoscopy, I woke up and I was throwing up, which I never do under anesthesia. The doctor came in. He was a very wonderful doctor. I’m still kind of out of it, and he’s like, “You have this bleeding, festering 7-centimeter mass in your rectosigmoid junction.” Without telling me I had cancer, he’s like, it looks like it’s cancer.
I’m waking up thinking he’s going to be like, you’re a hypochondriac. Get out. Go home. It wasn’t a Hallmark movie where there was a big dramatic reveal. I wasn’t crying. It was like, okay, then I was just checking out. They gave me a We were driving home, I looked at my husband and I was like, “Did he tell me that I have cancer?” He’s like, “Yeah.”
“You have this bleeding, festering 7-centimeter mass in your rectosigmoid junction.” Without telling me I had cancer, he’s like, it looks like it’s cancer.
Treatment
Getting tests and deciding on a treatment plan
It wasn’t until later in my journey that I thought about getting a second opinion. It was just like, you have cancer, here’s a doctor’s number, and start making appointments. Just start doing the things, and that’s what I did. I met with a colorectal surgeon. I scheduled all my appointments with the colorectal surgeon. I had a CT scan done and a rectal MRI done, which is amazing. That is an experience for the books. They need to come up with a better way to do those.
In between meeting with the surgeon and the oncologist before getting my official diagnosis, I had all these tests done, and then I met with the oncologist. They decided the best course of action. There’s something called a tumor board where the doctors get together and they decide this is what we’re going to do. They decided that surgery was going to be my best route first.
If you’re looking at a picture of your body, right before everything passes out of your body, there’s this final curve in your intestines right before the end. This is where my tumor was, which is why I wasn’t going to the bathroom. It was completely blocked.
Having surgery to remove the tumor
They said that it had spread to 9 of 26 lymph nodes, so I would have to start chemotherapy.

The surgeon was like, “We have all these different options, but because of where your tumor is, there’s a possibility that you will have an ileostomy, but probably not.” In February 2019, I went in for surgery. When I woke up from surgery, my husband was like, “They bagged you.” Because of the size of the tumor and where it wound up sitting, the height of it, they had to go in and they had to give me an ileostomy. I was supposed to have that for 6 weeks for my stitches to heal.
They sent me home with a PICC line in my arm, and then I had to sit on hydration every day for 8 hours. They gave me this fantastic plastic pole to hold this big bag of saline. It was like this plastic pole that didn’t hold the saline. It kept falling over and there were no wheels. I’m carrying this thing. It was a mess. I had a home health nurse come and they taught me how to change my saline and to keep myself hydrated.
One of our daughters was getting married in the middle of all this, so I had to try to hide my huge PICC line in my arm, when we were doing pictures. It was a lot going on, but during that process, we had gotten a call back from the doctor. They did the surgery, they did the tumor removal, and then they tested my lymph nodes. They said that it had spread to 9 of 26 lymph nodes, so I would have to start chemotherapy. I said, “Well, what about my ileostomy?” And he goes, “You have to keep it in until after chemotherapy is over because we can’t risk doing surgery on a lowered immune system.”
What was your staging and official diagnosis?
I put in all my symptoms and the first thing that popped up was colon cancer. I was like, I don’t have colon cancer…Even though that’s what it said it was, I didn’t put any stock in it. Who self-diagnoses themselves with cancer? You just don’t.
Stage 3 colon cancer. Some of my records said colorectal cancer, some said rectal cancer, but it’s essentially colon cancer. I was stage 3 at the time I was diagnosed.
The symptoms that I was having were really explainable. You don’t think that you have cancer. I don’t recommend anybody go on WebMD to diagnose yourself, but I was like, I need to figure out what this could be to try to give myself some relief until I go to the doctor and find out what it is. I put in all my symptoms and the first thing that popped up was colon cancer. I was like, I don’t have colon cancer. That’s stupid, I don’t have that. I was always like, I’m going to get breast cancer. I’m not getting anything else. Even though that’s what it said it was, I didn’t put any stock in it. Who self-diagnoses themselves with cancer? You just don’t. If I had waited any longer, who knows at that point?
Was your cancer diagnosis related to a genetic predisposition?
After they did all the testing, my oncologist basically said you got cancer because of bad luck. It’s not hereditary. There were no genetic markers. There was nothing. I downplay it, but I have a fantastic oncologist.
Starting chemotherapy
They started me on chemotherapy. I went in March 2019. They put a port in my chest because they do the chemotherapy intravenously. I would go to the cancer center and sit for 4 hours. They pump me full of chemo and then they would give me chemo to go. At the end, they would give me 1 to take home for 48 hours, and then I would go back and they’d flush it.
»MORE: Chemotherapy FAQs & Patient Stories
I tolerated chemotherapy really well. I would leave chemotherapy, go back to work, pick my kids up from school, and take my kids to school…Our lives weren’t really stunted by it.
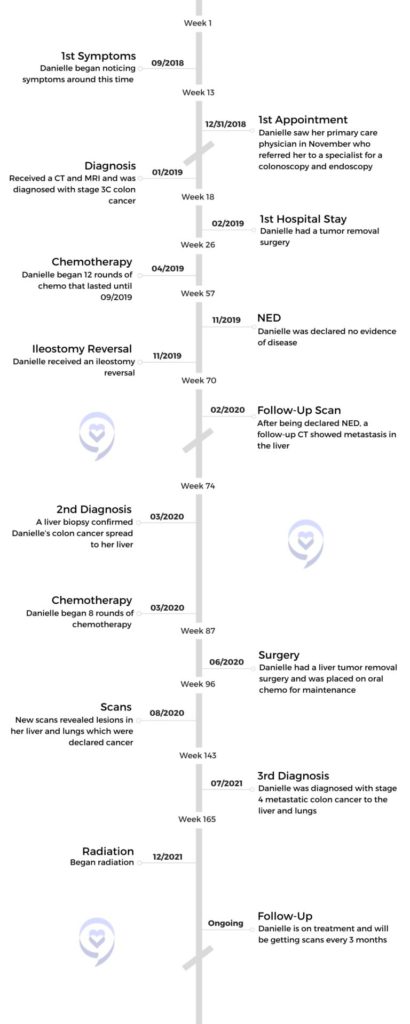
I started chemotherapy on April 1st of 2019, about 3 days after my husband went in for emergency open heart surgery. There was a lot happening. I did 12 rounds of chemotherapy. In September of 2019, I had my ileostomy reversal. In November 2019, I was declared no evidence of disease.
What did your follow-up scans show?
My first follow-up scans were 3 months later in February of 2020 and they showed metastasis to my liver. I went in for a biopsy in March 2020 and got diagnosed with metastatic colon cancer in my liver. It meant it was the same kind of tumor, not a new one, it just traveled.
They put me back on chemotherapy, which was a higher intensity for 8 weeks, then I had a tumor removal surgery in June of 2020. They put me on oral chemotherapy for maintenance purposes. I had my first follow-up scan in August of 2020, and it showed lesions in my liver and my lungs. They pulled me off the oral chemotherapy and put me back on IV chemotherapy. But at that time, we were just monitoring it. They weren’t saying it was cancer. My doctor was like, “People have lesions in their chest. It could be from anything, but we’re putting you back on chemotherapy just to be on the safe side.”
I went in for a biopsy in March 2020 and got diagnosed with metastatic colon cancer in my liver.
Did you have side effects from chemotherapy?
I was very lucky. I tolerated chemotherapy really well. I would leave chemotherapy, go back to work, pick my kids up from school, and take my kids to school. We were going out, we were doing stuff. Our lives weren’t really stunted by it. I was very lucky in that regard because not everybody reacts that way.
Are you on any clinical trials?
I don’t qualify for any right now based on the type of tumor that I have and what the genetic makeup of it is. I went to the colorectal cancer conference in September as a volunteer for the Colorectal Cancer Alliance. I met some great people there and they were able to help me out and give me some different ideas. I’ve been genetically tested. I’ve been blood tested. I’ve gone through all of the testing and all of the things, so right now I don’t qualify for anything else.
Living With Cancer
Getting caught up in making the “right” choices for your health
It’s been recommended to go plant-based. On the flip side, a lot of oncologists are like, “We just want you to eat. We want you to keep your nutrition up.” That becomes a difficult task as a cancer patient because once you start learning about all these different things you could be doing for yourself and doing for your body, it becomes, what if I don’t do this? I should do this. Well if I do this, is this going to help, or is this going to hurt me? Even 4 or 5 years later, I’m still in that position of, I’ve got Dunkin Donuts coffee. Should I not be having my iced coffee? Should I? It becomes a very difficult situation because you don’t know what the right thing is, but everybody’s body is so different.
Remembering that everyone is affected by cancer differently
When I see somebody pass away from the same kind of cancer and the same kind of diagnosis that I have, it’s like, why them and not me?…It’s a really weird space to be in.
I’m on a treatment right now that most people are on for 5 or 6 months before it stops working. I’ve been on it for almost a year and it’s still working for me. For the oncologists, it’s a really hard thing to predict because you’re dealing with individual body chemistries and so many other factors. Which is why, when I see somebody pass away from the same kind of cancer and the same kind of diagnosis that I have, it’s like, why them and not me? But it’s like, that’s them. It’s a really weird space to be in.
How much time passed between being NED and having metastasis?
There were 3 months in between when I received my scans. In this day and age, you’ve got access to everything. I pulled up my medical records and went to Dr. Google. I showed it to a friend who’s a nurse and she’s [shaking her head]. Then my follow-up with my doctor was in March. He’s like, “This is what it looks like, but we’re going to go do a biopsy just to make sure.” When the biopsy came back, he’s like, “Yeah, this is what it is.”
How did you process having metastasis?
Again, it wasn’t like a Lifetime movie. It was just like, all right, now what do we do? I live my life in 3-month increments because I get scans every 3 months without fail. What do my scans say? What does the doctor say? Okay, now I can plan the next 3 months. That’s just how I’ve learned to operate.
»MORE: Reacting to a Cancer Diagnosis
I live my life in 3-month increments because I get scans every 3 months without fail. What do my scans say? What does the doctor say? Okay, now I can plan the next 3 months.
What have the results of your most recent scans shown?
I had my most recent scan in July. Everything seems stable, so I’m very lucky. Everything right now is staying in my lungs and my liver. I did a month of radiation in December of 2021 to my lungs and my liver and then resumed oral chemotherapy. I’ve done everything, so I feel lucky in that regard because it’s just in these 2 places and I’m not getting new tumors. They’re not spreading and they’re not necessarily getting bigger to where there’s a major concern. It’s so weird when you have cancer, the things that you take as a win.
Ileostomy
Do you still have an ileostomy bag?
No, I got that reversed in November 2019. I’ve got a decent quarter-sized scar on my abdomen, on my right side from that.
Describe what an ileostomy is
The ileostomy is, they basically reroute your intestines to the outside of your body. It’s this very small piece that is probably a half inch that sticks outside of your body. It’s covered by a special bag, and that’s where you go to the bathroom. It doesn’t make it down your intestines. That reroute was done to bypass my stitches so my stitches wouldn’t get infected.
There are people that have a permanent ileostomy depending on their individual situation. It’s also different from an ostomy. It’s nicknamed Barbie butt because they sew your butt shut and then you never go to the bathroom again. That’s, I believe, lower in your intestines that they do that one.
»MORE: Navigating Life with an Ostomy
Do you have recommendations for anyone new to having an ileostomy?
Ask a lot of questions. They taught me and my husband how to change it when I was in the hospital. I didn’t grasp a lot of it and I didn’t ask. My husband was like, “It’s cool. I got it,” so he was doing it for me. But then he went in for open heart surgery. Luckily his office was next to a home health office and we had a very good relationship with them. I went over to them when he was in the hospital, like, “Can somebody help me here?” One of the nurses would help me change it until I figured out how to do it myself.
There are times that I miss it because there was a level of convenience. Everybody’s experience, of course, is different. But for me, it really wasn’t that bad once you learn to live with it.
I always had extra stuff with me, just in case. Making sure you’re staying hydrated, and keeping up the nutrition. Eating corn is a whole new experience when you have an ileostomy. It’s like popping popcorn. It’s the weirdest thing.
There are times that I miss it because there was a level of convenience. Everybody’s experience, of course, is different. But for me, it really wasn’t that bad once you learn to live with it. I mean, it still sucks, but I also think that things could have gone a lot worse for me.
Quality of Life
Were you working throughout your cancer treatments?
Fortunately for me, my husband and I are both self-employed. It was very helpful because when I got diagnosed and you’re doing 8000 tests and 8000 doctor’s appointments and you’re going in and out, I was able to work around that and take time off whenever I needed to. I don’t have to work. I love what I do for a living. That piece of it was really convenient for me.
About 3 years ago, I took a virtual position working for an online mental health company. It’s a weird thing because you don’t know if you should tell people that you have cancer or not. You never know how anybody’s going to react. Technically, nobody’s supposed to discriminate against you because you have a disability, which cancer for some reason is listed as a disability. But I took this job and we had requirements, just like any other company that you work for, especially mental health. You’re supposed to meet with so many clients a month.
I told her I had to do radiation for an entire month. I messaged my supervisor, who was really responsive. She’s like, “Well, I’ve got to run it up the chain.” I said, “Just for this month, I need to see 5 less clients a week.” I made every meeting, every training, and all my other appointments. I barely missed anything. She hadn’t gotten a response from anybody and it was a couple of months before somebody messaged me. Finally I messaged her and said, “Listen, if I’m going to get in trouble, I’m gonna get in trouble. I’ve got to do this. If the higher-ups want to come at me with it, that’s fine. I have no problem getting in trouble for this.”
»MORE: Working During Cancer Treatment
A couple of months after my radiation ended, I finally got a response, “Okay. If it goes any longer, we may have to talk about you going from W2 to 1099 as a contract employee because that may be better for you.” I found out after I separated from the company that they had a supervisor’s meeting. In the meeting, one of the higher-level people said, “She’s made this request to see 5 less people a week. We’re just going to tell her she’s got to be at 1099 instead.” The corporate attorney was like, “You can’t do that.” Just for 5 hours a week, like really? I’ve got cancer. I get great reviews from my clients. I got great reviews from my supervisors I’ve met. I’ve taught workshops. I’ve done all of the things. That was a really difficult thing for me.
Working through insurance and the cost of cancer treatments
I’m paying almost $1,000 a month on payment plans and that’s with insurance, so the cause of cancer is very expensive.
On the flip side of that, because I’ve been self-employed, I don’t qualify for disability. I don’t qualify for Medicaid because I haven’t paid enough into Social Security to get any disability, so that becomes part of it too. Now we have health insurance, which is great but even with that, there are co-payments. We have a very high deductible that we have to meet. I’m still paying for my surgery from 2019. Since I spoke to you last, I got 3 new medical bills that I’ve got co-payments for. I’m paying almost $1,000 a month on payment plans and that’s with insurance, so the cause of cancer is very expensive.
Then you fall into the category of working versus not working. I can’t work a regular job because I have to take time off. I go to treatment twice a month on Mondays. And what if I have a couple of unexpected hospitalizations? You’ve got that. It’s really hard for cancer patients, especially those who are still able to work. Disability doesn’t pay a lot of money, not enough for somebody to live on. That becomes really difficult as well. It makes me think of the people who are not in my position who are struggling. We’re able to make this work but there are so many people who can’t.
»MORE: Financial Toxicity of Cancer Treatment
Do you have advice for those on cancer treatments who want to work?
I guess, being in a place where it’s more accepted by people. People are more flexible for people that have not just cancer, but other chronic diseases that are still able to work and that want to work.
One of my best friends, she’s young, she’s 34, and she’s got all these post-cancer medical issues, but she wants to work. She’s in a position where it’s either she’s on disability or she works. She can’t do both. She’s got to be on state health insurance because she can’t work. It really makes it difficult for people to still be functional.
Do you still get scans?
I would go for MRIs on occasion. The MRIs were the worst for me. At first, they weren’t bad, but I call it being strapped to the table Silence of the Lambs style because they don’t want you to move. You’re strapped to this board and your head first in a closed MRI, and you’re in there for 45 minutes. The last time I did one, an Ativan was fantastic. It was fantastic for it. Fortunately, I haven’t had to do an MRI in a little bit.
I’m fortunate because my scans are like 5, 10 minutes. I go in feet first. They do my chest to my abdomen. They hook me up to an IV. They pump the contrast through my arm so that they can get a different visual. I think it takes me longer to drive there and get the contrast hooked up than it does for them to do my actual scans.
Coping with scanxiety
Again, I’m very fortunate because I don’t have all of the things, but I have anxiety because it’s like, okay, I got to do this again, what are my scans going to say? And then I check my electronic chart every 5 minutes, I get my results, and I don’t see my doctor after 2 weeks. I sit with these results for 2 weeks and what do they mean? There are those pieces of it that are difficult as well.
You do become sort of a pseudo-medical expert. We learn way more about blood tests and blood types and what blood levels mean. Me and my friend in California compare our blood panels with each other all the time. There are things that you learn about yourself and your body and medicine in general, because all of a sudden you have to be cognizant of these things and you have to become an expert of these things.
What’s happened is we have symptoms that we blow off. Our body betrays us because you think it’s one thing and it’s like, nope, it’s this. At least for me, I became hyper-vigilant. With a headache, I’m like, okay, do I have a brain tumor? My chest hurts. Have the tumors grown in my chest? It’s that constant background noise. I have a white noise machine that I use when I’m working with clients. It’s like a white noise machine. It’s always there in the background.
The difficulty of having age requirements to get cancer screenings
That’s the hard part about it. They just changed the age for colonoscopies from 50 to 45. I think you’re able to get it at like 43 or 42 if you’ve got a family history of cancer, but a lot of the people that I know that have colon cancer are in their 20s and 30s. If it were me, I would say stop with these age requirements because the age requirements are BS.
We’re living in a society where our environment sucks. The amount of wildfires happening in Canada that have polluted the air down in New York and beyond, and now the stuff in Hawaii. You’ve got 911 from 911.
I’m from New York. I’ve got friends that were first responders. One of my friends just finished breast cancer and had a double mastectomy. You have all these different factors. Our foods are genetically modified. Girls who are 12 and 13 do not look how I looked at 12 and 13 at all. There are all of these other factors that are involved. To have a minimum or an acceptable age where insurance starts covering these tasks I think is a bunch of crap. My friend is 34 years old. She cannot have children. I’m having colon cancer and cannot have children because of all the treatments.
If it were me, I would say stop with these age requirements because the age requirements are BS.
Missing cancer diagnoses in young people
That’s the thing too, is a lot of times if you’re younger or if something doesn’t fit into a medical model or a symptom checklist they say, oh, this isn’t this. You have that with WebMD. You put in the symptoms and this is what they tell you that you may have. If it doesn’t fit those categories, then you get dismissed. You’re too young for this or, oh, you just have this or that, or you get blown off completely. A year or 2 later, something happens. There are stories you hear all the time about 18, 19, and 20 years old.
The cost of food, the cost of living and eating healthy is way more expensive. Fresh fruits and vegetables don’t last as long so you have to go to the store more often. People can’t afford that.
Reflections
Getting checked when new symptoms arise
I tell people this all the time. If you don’t feel well, if something is wrong, you know your body better than anybody else does. Go to the doctor. If the doctor doesn’t pay attention to you or blows you off, go to somebody else. Do not wait. It may be nothing, but if it’s something, maybe you can catch it early enough to get it taken care of.
There are so many treatments out there. There are so many options out there. Not every diagnosis is a death sentence. Not everything is going to be tragic. But putting it off because you’re afraid of what may happen can be more detrimental to you than addressing it now. Make sure you’re taking care of yourself and identifying the best way for you to achieve that.
How to be supportive and unsupportive towards cancer patients
Dealing with cancer is hard enough without being browbeaten or judged about how we choose to handle it.
When you get diagnosed with cancer, you get all sorts of advice, all sorts of unsolicited advice. I’ve gotten copper water, essential oils, you name it, I’ve gotten it. People mean well, they really do. I remember when I first got diagnosed, I was working with a client and she’s like, “Oh if I got diagnosed with cancer, I wouldn’t do chemotherapy. That stuff’s just poison.” Cool. Not the thing that I wanted to hear, but I get what she was saying. Or, my sister’s cousin’s uncle got that kind of cancer and he died. Not helpful, not helping me.
The best way to support someone is to say, I’m here if you need anything, just let me know what it is that you need. Period. We shouldn’t be judging each other’s journey or the choices that we make. There are people who don’t get chemotherapy and try to go a natural route, and that works for them. There are people who do both and there are people who just go traditional. That’s fine. Again, everybody’s different. Dealing with cancer is hard enough without being browbeaten or judged about how we choose to handle it.
Do you have any advice for those on their cancer journeys?
Take advantage of the times that you feel good and honor your body when you don’t.
Joining a cancer community is great. If you’re on Twitter, cancer people are the funniest people on the planet. We’ve got the best sense of humor because we’re very twisted. We use a lot of dark humor to cope. If you ever need to be amused, go follow cancer patients on social media. There has to be some levity with the seriousness of it.
Having a cancer community is important because there is a level of understanding that you’re not going to get anywhere else. Not that your friends and family are not supportive, I’m not saying that at all. But people who go through it are in the trenches with you and go through the treatments and the surgeries and all the side effects. They can identify and assist you in a way that other people can’t. I think that’s really important.
More Colorectal Cancer Stories
Sydney S., Colon Cancer, Stage 4 (Metastatic)
Symptoms: Constant stomachaches that only went away after bowel movements, pain after eating, changes in bowel size and shape
Treatments: Surgeries (colectomy, temporary ileostomy, ileostomy reversal), chemotherapy (FOLFOX, FOLFIRI, trifluridine and tipiracil), monoclonal antibody (bevacizumab), radiation therapy, hormone therapy
Kristie C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: None per se that she noticed; she experienced constipation and passed narrow stool, but had been experiencing constipation most of her life, and thought that these digestive issues could also have resulted from perimenopause
Treatments: Chemotherapy (including adjuvant chemotherapy), radiation therapy, ablation therapy (liver ablation), surgeries (colectomy, temporary ileostomy, ileostomy reversal, scheduled liver resection)
Briana H., Colorectal Cancer, Stage 3
Symptoms: Periods of constipation initially lasting one week and then extending to two weeks, nausea, pain in lower left abdomen, lack of appetite, vomiting and inability to keep fluids down
Treatments: Surgeries (colon resection, tumor removal, colostomy placement, colostomy reversal), chemotherapy
Kailee O., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Sensitive stomach sometimes leading to vomiting after eating, bleeding during bowel movements, persistent fatigue, back pain, abdominal pain, anemia, significant symptom flare-up during second pregnancy
Treatments: Surgery (colectomy), chemotherapy, targeted therapy
Starr S., Colon Cancer, Stage 4 (Metastatic)
Symptom: Abdominal pain
Treatments: Chemotherapy, surgeries (colectomy, hepatectomy, lymphadenectomy), targeted therapy
Jackson L., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach pain, fatigue, lack of motivation, anemia, blood in stool, thinning stool
Treatments: Surgeries (emergency bowel obstruction surgery with temporary colostomy, possibility of HIPEC in 2026), chemotherapy, immunotherapy