Alison’s Stage 4 Triple-Positive Metastatic Breast Cancer Story
Alison shares her stage 4 triple-positive breast cancer story. She was diagnosed at just 34 years old after finding a lump under her right arm and breast area. She details undergoing chemotherapy, mastectomy, radiation, and targeted therapy.
In her story, Alison also highlights how she dealt with 2 relapses, how she parented with cancer, the impact of the diagnosis on her relationship with her spouse, and the support that helped her most.

- Name: Alison R.
- Diagnosis:
- Breast cancer
- Partially differentiated DCIS, triple positive at age 34
- Staging: 2 metastatic relapses
- Symptoms: Lump under right arm and breast area
- Treatments:
- Chemotherapy:
- 6 rounds of TCHP– Taxotere, Carboplatin, Herceptin & Perjeta
- Gemcitabine, Cisplatin, 5FU & Leucovorin
- Abraxane (paclitaxel), Adriamycin, Herceptin & cyclophosphamide
- Adriamycin switched out for Navelbine when lifetime dose was reached
- Capecitabine oral chemo during radiation
- Surgery
- Bilateral mastectomy with right axillary lymph node removal
- Radiation
- Right breast and axilla, 33 treatments
- To right neck after metastatic relapse, 33 treatments
- Targeted therapy
- Tykerb (lapatinib)
- Chemotherapy:
- Diagnosis
- 1st-Line Treatment
- What was your treatment plan?
- You underwent genetic testing
- What was your first chemo regimen?
- What were your side effects from chemo?
- How did you feel before the mastectomy?
- What do you remember of waking up from surgery?
- What was radiation like?
- Switching oncologists
- You had some more treatment after NED (no evidence of disease)
- How were you feeling after you finished treatment?
- Relapses
- Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
As much as you can, try to take it one day at a time. It can feel really overwhelming if you try to look at the whole picture. If you can keep focused on what’s going on today, it’s a lot more manageable.
Something else that’s helpful for me is journaling. I write about things that have worked out and things I’m thankful for. That helps me stay grateful in hard times.
Alison R.
Diagnosis
Can you talk about your first sign that something was wrong?
We had moved from Nebraska to California, but I was back home with my kids visiting family. I felt a lump under my arm. My mom is a nurse, so I had her feel it. She asked if I had anything on my breast. We started looking, and sure enough, I felt a long, flat spot on my right breast.
She said it was probably nothing but suggested I go ahead and check with my doctor when I got home. I was visiting for about a week, so when I got home, I went and saw my OB.
She said, ‘You’re young. It’s probably nothing, but we’ll check it out.’
We did an ultrasound first because I was breastfeeding and couldn’t do a mammogram. We did an MRI next. Then we did the breast and lymph node biopsy.
What was the biopsy like?
They were fine-needle biopsies, and it was an interventional radiologist who did them. They kept saying that the biopsies weren’t going to be bad, but it was actually more painful than I expected.
The one in my breast wasn’t that bad, but the one in my armpit (the lymph node biopsy) hurt. They hit a nerve the first time.
I still have some numbness in my ring and pinky finger from that. Under my arm was sore, and I had more swelling than I expected. The breast biopsy wasn’t a big deal.
How did you receive your diagnosis?
The doctor called and said they had my results, if I wanted to go ahead and come in. She told me it was breast cancer in the breast and the lymph nodes. My husband left work to head there. It was just me and my 18-month-old daughter when she told me.
I realized then that I was prepared for it to be breast cancer, but I wasn’t prepared for it to have spread to the lymph nodes.
I was a little bit shocked. I took in the information, and I was crying. My daughter was on my lap, and she was like, ‘Be happy, Mommy.’
About that time, my husband walked in. I let the doctor tell him. We hadn’t really told anyone that I was getting tested for anything when I got the diagnosis.
We wanted to gather all the information and handle our own emotions before taking on the emotions of others as well. I called my parents on the way home.
»MORE: Patients share how they processed a cancer diagnosis
You had boudoir pictures taken
A friend of ours takes all our family photos. Her mom died of ovarian cancer and had the BRCA gene. She’s had a prophylactic mastectomy.
I knew that even if it wasn’t cancer, there was a chance they’d have to remove it. Before I got the diagnosis, I had asked her to take boudoir photos for me.
I just wanted to capture my body how it was even if it wasn’t cancer because I knew it could still change it.
I don’t know why I thought of it at the time. It was for my husband. Then I found out it was really for me, too. I’m really thankful I did that.
Since then, I’ve had a mastectomy, but I’ve never had reconstruction, so I’m really glad I have those. Because of her history, I think it was special for her to do that with me.

1st-Line Treatment
What was your treatment plan?
I had a lot of testing, and we first met with the surgeon. He was friends with the oncologist. He messaged her when she was on vacation, and she called me. That was amazing.
They wanted to do surgery, but because of the size, they decided to go ahead and do chemo first to shrink it before surgery.
You underwent genetic testing
My HER2 test results came back equivocal 3 times, so it felt like a long time waiting in between getting diagnosed and starting treatment.
When we finally found out I was triple positive, we could start. That was about a month later.
What was your first chemo regimen?
I started with TCHP chemotherapy regimen — taxotere, carboplatin, Herceptin, and Perjeta. The first time I went in, it was a really long day. I got all of the pre-meds and chemo drugs on the same day. Then, 3 weeks later, you get the next round of them. I did 6 rounds.
After the first round, I ended up with a neutropenic fever. My white count got really low. I ended up in the hospital. Everyone who came in had to be gloved up. My husband thought I was going to die. I didn’t have that fear at the time, but he did.
After that, my white count came up, and we continued, but I took Neulasta after infusions. I used Benadryl, Claritin, and ibuprofen each time I got a shot, and that prevented the dreaded bone pain.
What were your side effects from chemo?
Summary: mouth sores, hair loss, taste changes, fatigue
I got mouth sores, and those were not fun. I tried the Magic Mouthwash. I tried a steroid paste. I tried viscous lidocaine.
The doctor started me on Acyclovir and I didn’t get mouth sores after that.
I lost my hair. I shaved my hair before chemo. I had my kids do it because I wanted them to have some control, and I figured it would make more sense to them. I went ahead and shaved it so I could donate it, because they wanted it pre-chemo. Plus, it made more sense to my kids.
My taste buds would be okay for a couple of days, then things would start to taste funny. By the time it started to feel better, it would be time to start the next treatment.
I had fatigue. I didn’t ever get nauseous really. They managed that well, and for the most part, I think my body tolerated the chemo pretty well, too.
I would do labs before doing chemo each round. After the 6 rounds, we did a breast MRI. I didn’t do a PET scan. I had actually begged for PET scans, and nobody would do it. On the breast MRI, it looked like it was pretty much gone.
»MORE: Cancer patients share their treatment side effects

How did you feel before the mastectomy?
I did a bilateral mastectomy and right axillary lymph node removal. I had my nipples removed, too. I just wanted to be really sure that I was reducing the chance of having a recurrence.
I was okay with all of that. It did feel weird to lose my nipples, but my doctor said it reduces the chance of recurrence, so I said okay.
To prepare, I was just in a fight mode. I wanted to stick around for my kids. I wanted to be more aggressive.
I have a friend who had been through breast cancer and a cousin in Texas, and they both shared their experiences with me. I talked to a few people who had been through it before.
Right before surgery, I remember feeling nervous about the anesthesia. I didn’t want to wake up during surgery. The nurse navigator reassured me that there were people whose only job was to keep me asleep.
What do you remember of waking up from surgery?
I was in some pain when I woke up. I had a compression garment over my chest. The surgeon wasn’t as empathetic as I would’ve hoped he would be after surgery. I wanted to see my chest after surgery. He was basically just like, “Well, it’s going to look freaky.”
The nurse navigator offered to look with me. I removed the garment, and I remember seeing the staples across my chest. I didn’t feel highly emotional about it or anything.
I had a lot of swelling. The mastectomy wasn’t really painful in my chest, but under my arm was really sore. I had drains in. I had a post-mastectomy bra that had pockets for them. I was nervous to get the drains removed, but it wasn’t as bad as I thought it would be.
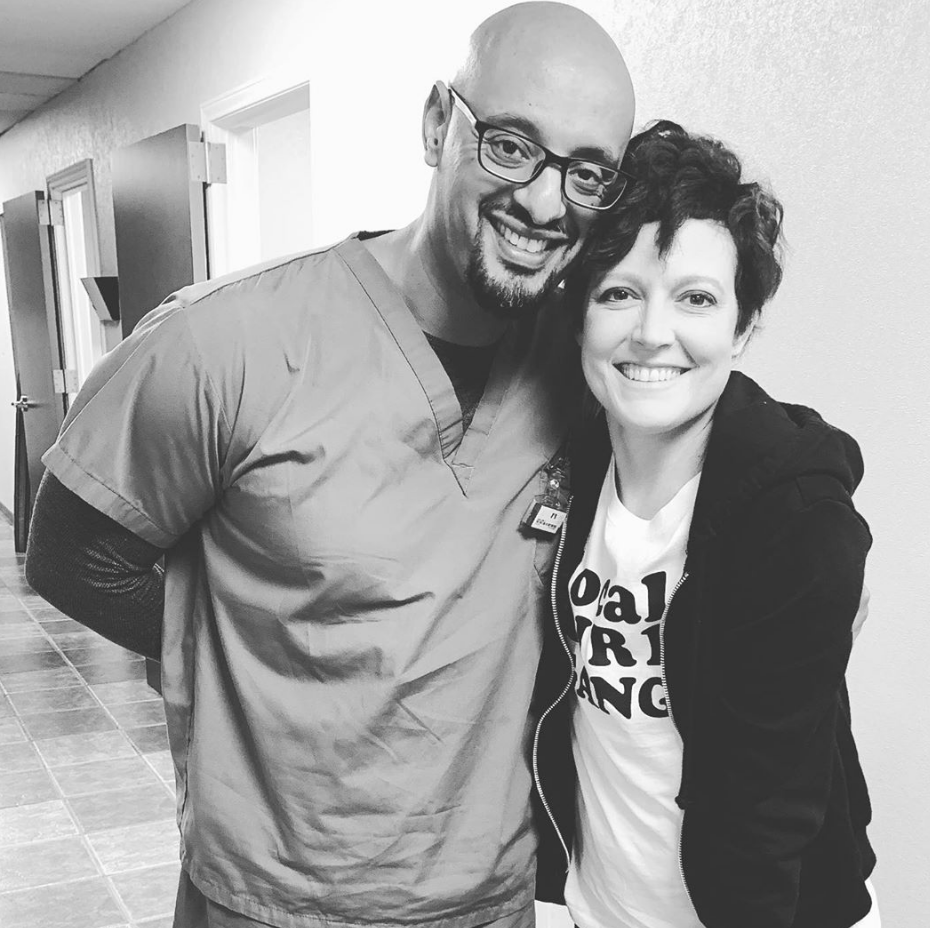
What was radiation like?
After recovering from surgery, it was time to start radiation. I met with the radiation oncologist. I went in, and they did an MRI and mapping. They planned out where they were going to radiate.
They would take me in, get everything lined up, walk out, and then radiation itself was so fast.
There was this picture on the wall of a lake scene. I think it was meant to be comforting, but it just made me feel like I was going to die. It wasn’t a terribly scary process, though.
I was mostly just tired. I had quite a bit of fatigue. That lasted a couple of months, even after radiation had ended. I also had some minor burning on my skin in the areas they radiated. I had Silvadene cream for that, though, and that helped.
Switching oncologists
We moved from California back to Nebraska, so I switched oncologists then. It is hard because you develop some trust with your team.
Luckily, my oncologist in California recommended a doctor she was on the ASCO board with. It was orchestrated seamlessly.
You had some more treatment after NED (no evidence of disease)
I had been on Lupron injections to shut down my ovaries since my cancer was ER+. After radiation, I started on Arimidex, which is an aromatase inhibitor to suppress any other estrogen. That’s just a daily pill. I also had to finish up 6 months of Herceptin infusions.
I had gotten my port taken out during my mastectomy because my daughter lays on my chest, and her head would always hit it.
That was okay, though, because Herceptin isn’t as hard on the veins, so I just got it infused through an IV.

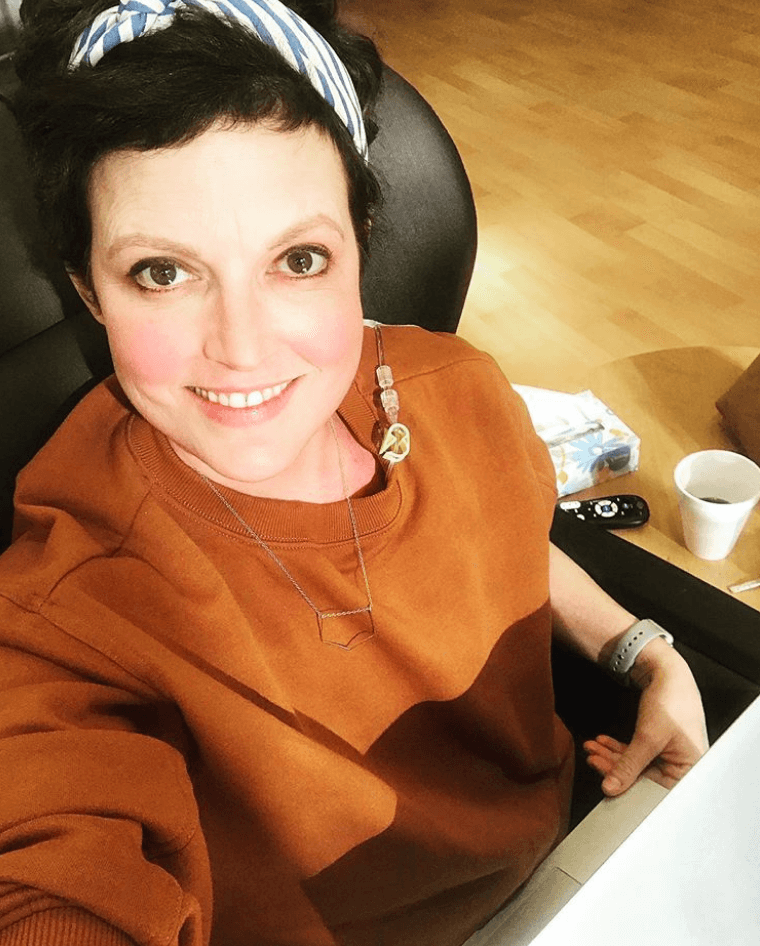
How were you feeling after you finished treatment?
I was getting back into my normal life, but that was a time filled with a lot of stress and anxiety for me.
I was seeing my counselor for my anxiety. He asked, “Has your mom or husband talked to you about taking anything for your anxiety?”
I would fixate or obsess over things during that time. I ended up started on a low-dose of Effexor XR, and that has helped tremendously.
Relapses
How did you find out you relapsed?
I felt something in my neck. There was something that felt familiar about it. It felt like what was in my armpit originally. We did an ultrasound and biopsy of that.
I was at the movie theater with my kids. My oncologist’s nurse called, and she said, “I’m so sorry. It is breast cancer.”
That was harder than the original diagnosis. I had the fear that it was going to come back, but I never expected it to happen that soon.
I had known enough to know that stage 4 was so much more serious.
My husband came over, and I said, “Well, I need to go to Houston to get a second opinion. I need to call the doctor.”
He said, “No. What do you want to do right now? The kids are about to walk out of the theater.” We agreed he would take the kids home, I would go for a jog, put the kids to bed that night, and talk after that.
I wanted to get a second opinion at MD Anderson and at Salem Oncology Center because my cousin had seen a doctor down there. He didn’t take insurance, but our cousins and godparents helped us financially so that I could start treatment with him.
What was your chemo like the second time?
I started treatment at Salem Oncology Center. My dad went down with me. We arrived on Sunday, and I went in to get a port put in again. I got wheeled straight into my new doctor’s office.
I did gemcitabine on Day 1. Then I did cisplatin on Days 4 to 6. He would fractionate it. He gave me the full dose over those 3 days. That wasn’t as toxic on my body.
A few days later, I’d get gemcitabine again. Then I’d get 5FU and leucovorin. The next week, I’d get gemcitabine again, and then I’d have a full week off.
I didn’t lose my hair on that regimen.
I had a few mouth sores, but we figured out a dental paste that helped. I used viscous lidocaine. I didn’t have a lot of side effects with this regimen.
After one round of chemo, we did a CT and PET scan. I had a 60% reduction. I stayed for one more round. Then I came back to Nebraska. I found an oncologist in Lincoln who was willing to do it, because it was working. I did a few more rounds with him.
I was in complete remission again after that.
What happened when you went into complete remission?
Once I was in remission, my doctor in Nebraska wanted to stop chemo and start radiation again. My doctor in Houston wanted to keep the chemo going. We had another decision to make.
I met with another oncologist here in Lincoln who happened to know my doctor in Houston. They worked together for 17 years. I made the decision to keep going with chemo. I had to find another local oncologist who would follow the protocol. I found one in Omaha.
He was comfortable working outside of the box. He said because patients aren’t standard, treatment doesn’t always have to be.
Relapse again
I found another tiny lymph node in my neck. I asked to push my trip to Houston for an early scan. The radiologist just thought it was an active lymph node. My doctor said he trusted my fingers, though, and the radiologist did a fine needle biopsy.
It came back positive for cancer. My doctor wanted to switch my protocol. I went for a month of treatment. I did another round of chemo down there.
Then I came back to Nebraska, did another round or 2, and I was in complete remission again.

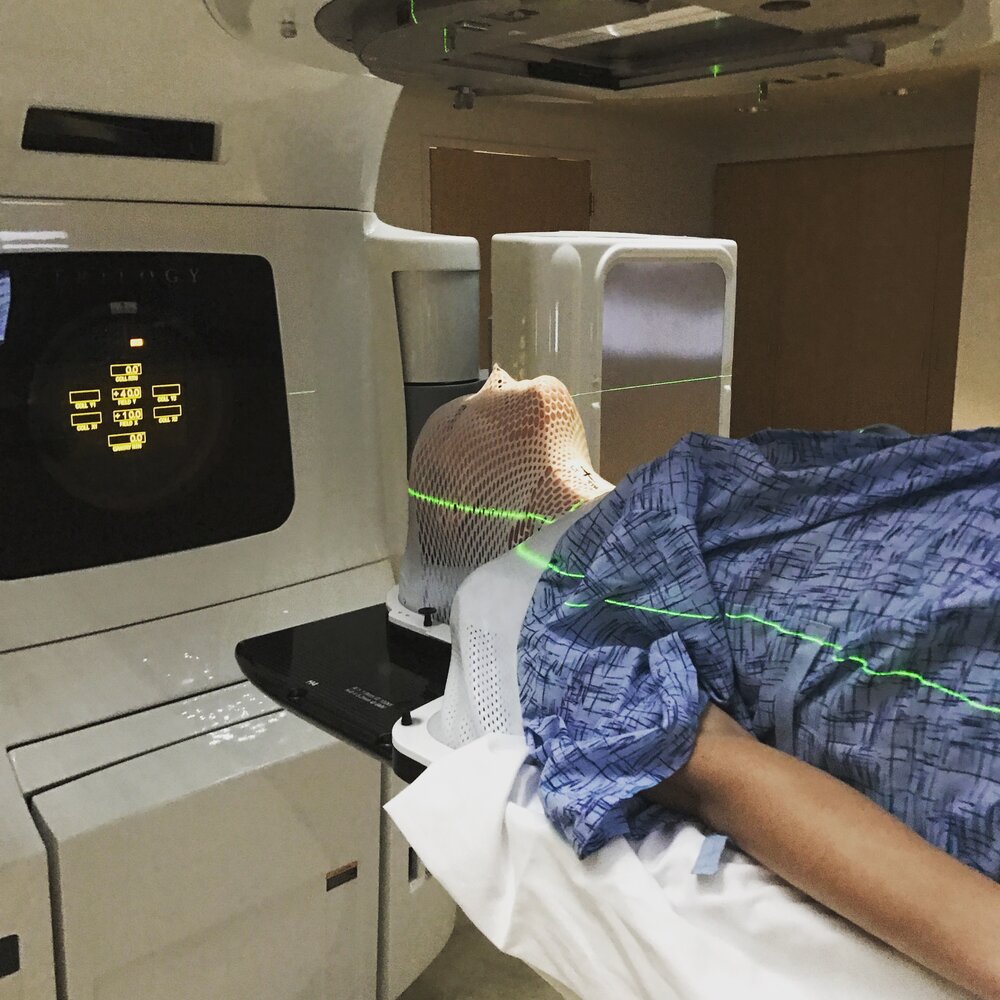
At that point, I did consolidation radiation. I did that here in Nebraska. They put the thin mask over you, and it hardens.
They’d hook me in, and I would panic a little until I could swallow the first time.
I lost 15 pounds or so during that radiation because it was just on the edge of my esophagus. Eating became difficult, so I was just doing a lot of shakes and stuff, so I think that’s why I lost weight.
I did chemo during radiation. That regimen was Adriamycin, cyclophosphamide and Abraxane. They added Herceptin back in as well.
During radiation, he took me off of Adriamycin and put me on capecitabine instead.
Are you in remission currently?
I was back in remission, but I did a couple of more rounds of chemo again. Then, once I was in remission, I would do a month of chemo on and then a month off. After a year of doing that, I moved to doing 1 month of chemo and 2 months off for a year.
At some point, I hit the lifetime dose of Adriamycin, so they switched that out for Navelbine. I’m currently still doing 1 month of chemo and 2 months off, but I’ve been in remission since August 2017.
If I stay in remission for a while, there might be a point where we spread it out even further or where I don’t have to do chemo at all, but for now, I’m just taking it one step at a time.
Reflections
How have you handled this mentally and emotionally?
I have wonderful friends and family, I see a counselor, that low dose of Effexor XR helps tremendously, and I’m a believer. I pray. I feel like God has given me the strength I need. He’s brought so many people into our lives. He’s been so faithful that I trust even if I do die, He’s taking care of this.
I used to worry about dying as it related to my kids. Then it clicked one day. I can’t worry about not being their mom later. I’m their mom right now.
I have to focus on right now. I accept grace for each day. I can’t know what’s coming, but when I get there, I’ll have grace for that day, too.
I’m not as fearful as I was in the beginning. Now, I feel like I’m able to be realistic about death, but I also know I could be around for a long time. I don’t know which one is my future, but I’m at peace with that now.
How is it being a parent with cancer?
They were so little when I was diagnosed. Now, my son is 8, and my daughter is 6.
About 2 years ago, my daughter’s friend’s mom died from breast cancer. That was the first time my son brought up death and cancer.
He said, “Mom, did she die from her chemo and her cancer?” I had to say, “Yes, she did.” My daughter said, “Mom, are you going to die when I’m a kid?”
I said, “I don’t know. I hope not, but if I do, you have Grandma, your aunts, and your dad, who all love you.” We have those conversations now. We talk about how some people die from cancer, but others don’t.
We’ve also been very sure to use the correct terms in order to not confuse them.
We’ve made it very clear that Mommy has cancer and has chemo. We don’t say, ‘Mommy is sick and needs medicine.’ We’ve made it clear that they don’t have cancer, Daddy doesn’t have cancer, and they can’t get it from Mommy like a cold.
»MORE: Parents describe how they handled cancer with their kids


How has cancer affected your marriage?
It’s brought us a lot closer. We’ve had to get even clearer in our communication. It’s given us the opportunity to have some really deep and hard conversations.
He’s really good at bringing me back to the moment. One time, I relapsed, and I said something about wanting him to get remarried but would wish it could be me.
He said, “That’s not happening right now. Let’s think about what’s happening right now.” He brings me back to the present moment a lot.
We talked about how it was a hard thing at first to let people help. He still has to work through some of that, and I do, too.
»MORE: 3 Things To Remember If Your Spouse/Partner Is Diagnosed With Cancer
How has the financial aspect of treatment been?
Thankfully, we have insanely generous cousins, who gave us the money to be able to start treatment in Houston. That was hard on my husband because he felt weird accepting that. He wouldn’t even buy himself a candy bar for a while.
When I do treatment in Nebraska, it’s covered by insurance. My doctor here said that insurance could decide at any point to not cover it, but my medical team works really hard.
We have a high deductible, so we just save in other ways and are careful with our money.
Can you talk about hair loss?
You never know if it’s going to bother you, but thankfully it didn’t bother me. Except there were times when I didn’t really know how to dress and be bald.
The second time, when the kids shaved my head, they were really mad. They didn’t want me to lose my hair. They were mostly okay with me going bald.
I did have wigs and hats, though. I posted a picture on social media of me in all the different options. That way, if I saw someone, it wouldn’t be awkward for them.

Then the third time I lost my hair, my kids wanted me to wear the wig. I’d ask if they wanted me to have hair or no hair, and they’d always choose the wig.
I was a little bit bummed when I lost it the second and third time because I looked sick. When I was going through treatment and didn’t lose my hair, it was nice because people didn’t necessarily know.
My hair thins now, but it’s nice to still have it. It’s better than not having it. I’ve gotten to try out all the short hairstyles I was always too scared to try before cancer.
»MORE: Dealing with hair loss during cancer treatment
How people have supported you
Some of our friends distanced themselves because they didn’t know how to handle it or deal with it. Other people stepped up.
Now, I think everyone is more comfortable with it. People brought meals, care packages, and offered to help with the kids.
One thing that happened when I relapsed was one friend had a bunch of people dress up in superhero shirts and send me pictures. That was nice because it was so encouraging, anyone could do it, and it didn’t cost them anything.

The care packages were always so nice. I got a lot of lotion made for someone going through chemo, scarves, blankets, and so many helpful things.
Even just a text or note of encouragement went such a long way. Having someone just say something is great. I think sometimes people don’t know what to say, so they just don’t, but just say something.
Ask, “How are you today?” I think, “How are you?” is a hard question.
»MORE: What kind of support cancer patients say helped the most
What advice do you have for someone who has just been diagnosed?
As much as you can, try to take it one day at a time. It can feel really overwhelming if you try to look at the whole picture. If you can keep focused on what’s going on today, it’s a lot more manageable.
Something else that’s helpful for me is journaling. I write about things that have worked out and things I’m thankful for. That helps me stay grateful in hard times.
Advocate for yourself and ask a lot of questions. Find an oncologist you’re comfortable with. Especially if you have late-stage cancer, keep going until you find someone who’s willing to fight as hard as you want to.

Inspired by Alison's story?
Share your story, too!
Ductal Carcinoma In Situ Stories
Erica C., DCIS, Stage 0
Symptoms: Indeterminate calcifications found on a routine mammogram
Treatment: Double mastectomy
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
Alison R., Partially Differentiated DCIS, Stage 4 Metastatic
Symptom: Lump in underarm/breast
Treatments: Chemotherapy, surgery, radiation, targeted therapy


One reply on “Alison’s Stage 4 Triple-Positive Metastatic Breast Cancer Story”
Thank you for sharing your story Alison R., Partially Differentiated DCIS, Stage 4 Metastatic. I was just diagnosed, and have a small team to help. I too am a believer.