Living with the Mental Health Aspects of Waldenström Macroglobulinemia (WM)
Edited by:
Katrina Villareal
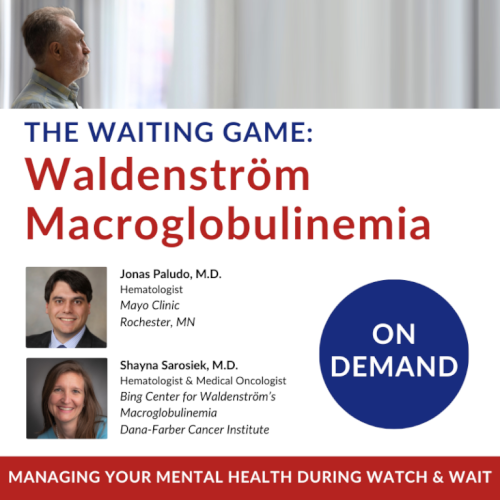
WM patient advocate Pete DeNardis leads the discussion as two experts in the field of cancer care, Dr. Jonas Paludo from the Mayo Clinic and Dr. Shayna Sarosiek from Dana-Farber Cancer Institute, dive deep into the crucial topics of watch and wait and mental health. Gain insights that could transform your understanding and approach to cancer treatment.

Thank you to Blood Cancer United for their support of our patient education program. The Patient Story retains full editorial control over all content
We would also like to thank the International Waldenstrom’s Macroglobulinemia Foundation for their partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Introduction
Stephanie Chuang, The Patient Story Founder
Stephanie Chuang: I’m the founder of The Patient Story after my non-Hodgkin lymphoma diagnosis. The goal of our platform is to help patients, care partners, and anyone in the support circle navigate life after a diagnosis. The Patient Story does this primarily through in-depth patient stories and educational programs.
It’s especially important in a space like Waldenstrom’s where patients and families are told many times that there will be no immediate treatment and that they’ll enter a period known by most as watch and wait. This discussion is all about support and getting through something as difficult as hearing that.
We want to thank The Leukemia & Lymphoma Society for supporting this independent educational program, which helps us host more of these and always for free for our audience. The LSS has invested over $1.5 billion in blood cancer research and provides free educational resources and support, like information specialists on hand who provide one-on-one support on everything from questions about treatment to social and financial challenges.
Thank you also to our promotional partner, the International Waldenstrom’s Macroglobulinemia Foundation (IWMF), which also provides free resources specifically to the Waldenström’s community, from wellness resources to peer-to-peer support.
While we hope you walk away with more knowledge, this discussion is not meant to be a substitute for medical advice. Please speak with your medical team about important decisions.



Stephanie: I’m lucky to know Pete DeNardis, who has been an incredible part of the IWMF as someone who was diagnosed with Waldenström’s and an advocate. Pete, thank you for taking the time.
Pete DeNardis, WM Patient Advocate
Pete DeNardis: I’m a WM patient myself. I was diagnosed in 2003 at the age of 43. I’ve been a volunteer for the International Waldenstrom’s Macroglobulinemia Foundation (IWMF) since 2005 and have been a board member for a long time and currently serving as the chair of the board of trustees.
I’ve been in multiple periods of treatment and watch and wait, so I understand the physical and mental impact of Waldenstrom’s when you’re navigating through those various periods.
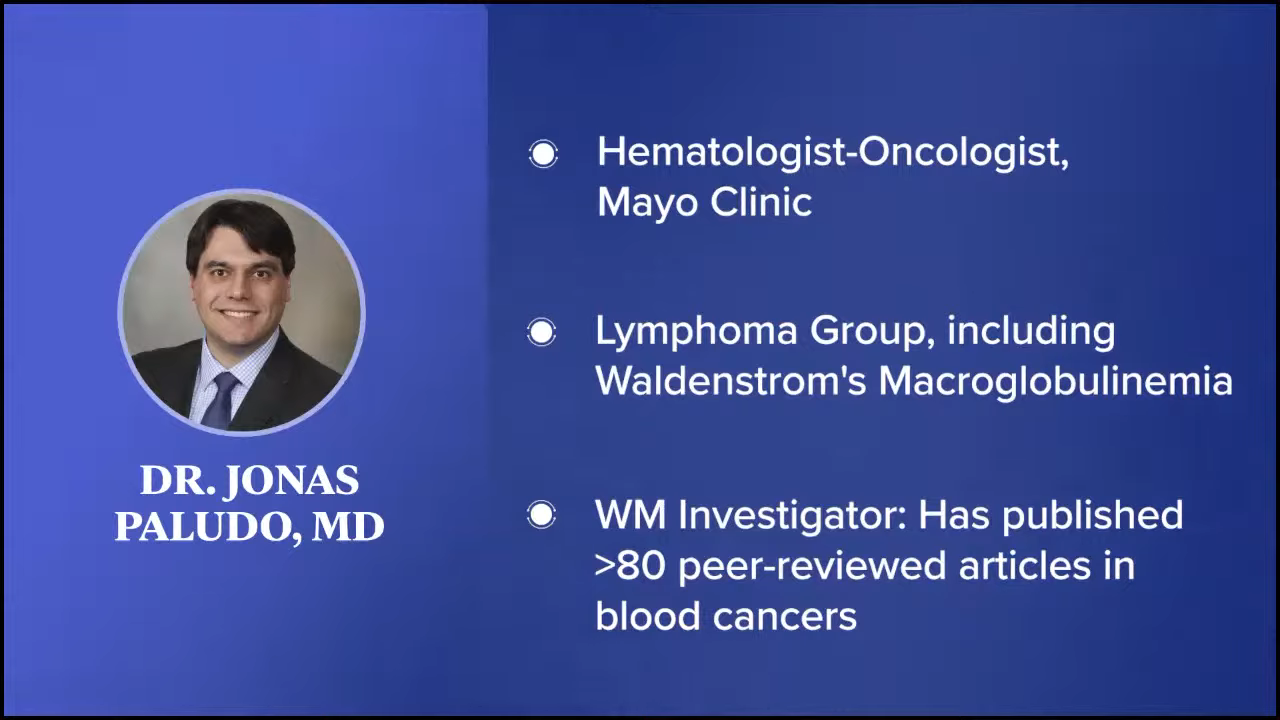
Dr. Jonas Paludo, Hematologist-Oncologist
Pete: Dr. Jonas Paludo is a hematologist-oncologist at the Mayo Clinic and part of their lymphoma group, including Waldenstrom’s Macroglobulinemia. He also investigates the effectiveness of various treatments for WM, examines the outcomes of patients with the disease, and studies the genetic mechanisms associated with the development of this malignancy. Dr. Paludo, what drew you to becoming a doctor?
Dr. Jonas Paludo: I had the first-hand opportunity to experience the difference that a good doctor can make in the lives of patients and families when they go through a cancer diagnosis. I thought my calling was to help patients and people when they’re struggling with a difficult diagnosis. I always thought I was going to be an electric engineer because I enjoyed math and physics. I changed my mind, applied to medical school, and never looked back.

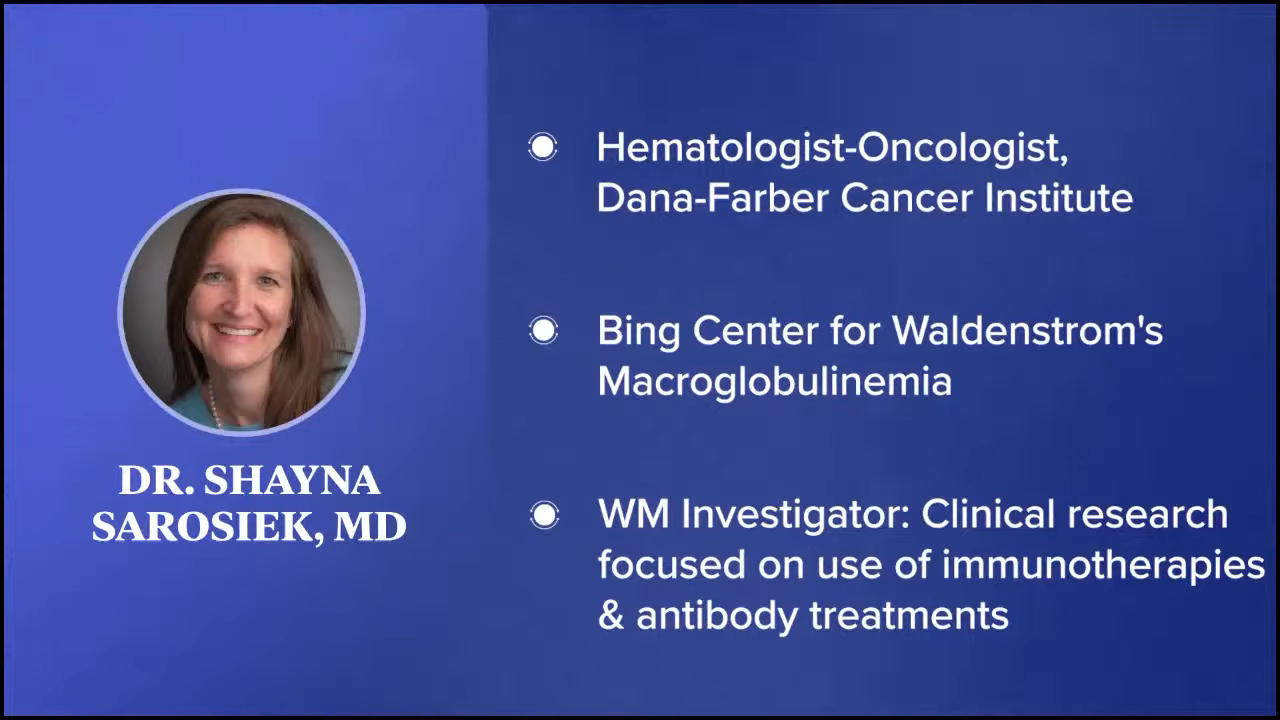

Dr. Shayna Sarosiek, Hematologist-Oncologist
Pete: Dr. Shayna Sarosiek is a hematologist-oncologist at Dana-Farber Cancer Institute, specifically at The Bing Center for Waldenström’s Macroglobulinemia, the largest center in the world dedicated to the study and development of new targeted therapies for Waldenstrom’s. She’s involved in clinical research focused on the use of immunotherapies and antibody treatments. She also sees patients on a day-to-day basis and deals with patients who have both WM and amyloidosis. Dr. Sarosiek, what drew you to becoming a doctor?
Dr. Shayna Sarosiek: I was very young when I decided I wanted to be a doctor. I was interested in biology. Instead of pictures of bands on my bedroom wall, I had a poster of every system in the body. I had anatomy setups around my room so that I could study the human body. I also had a close family member with cancer when I was a child and that’s what drew me to cancer care specifically. I’m very happy that I’m in this field.
Understanding Waldenström Macroglobulinemia
What is Waldenstrom’s Macroglobulinemia?
Pete: Let’s talk about understanding WM. Dr. Paludo, can you describe Waldenstrom’s Macroglobulinemia?
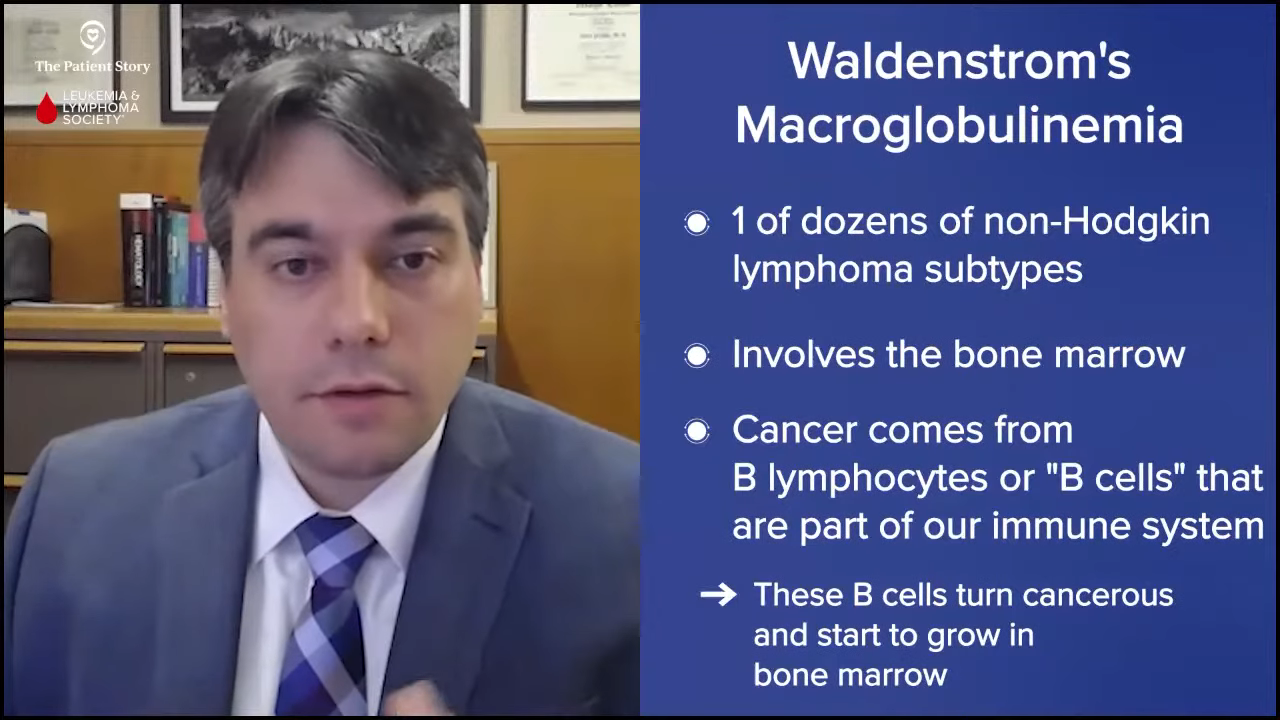
Dr. Paludo: Waldenstrom’s is a type of lymphoma. There are many different types of lymphomas, several dozen to be honest, and they behave in different ways. They come from different cell types and different classifications. Waldenstrom’s belongs to the non-Hodgkin’s lymphoma category, which has several dozen different lymphoma subtypes.
Waldenstrom is also sometimes called lymphoplasmacytic lymphoma as it involves the bone marrow of the patients. This type of cancer comes from B cells or B lymphocytes that are part of our immune system. For reasons that we don’t understand exactly why or how, when one of those normal B cells or B lymphocytes becomes a cancer cell, it starts to grow and take up space in the bone marrow.
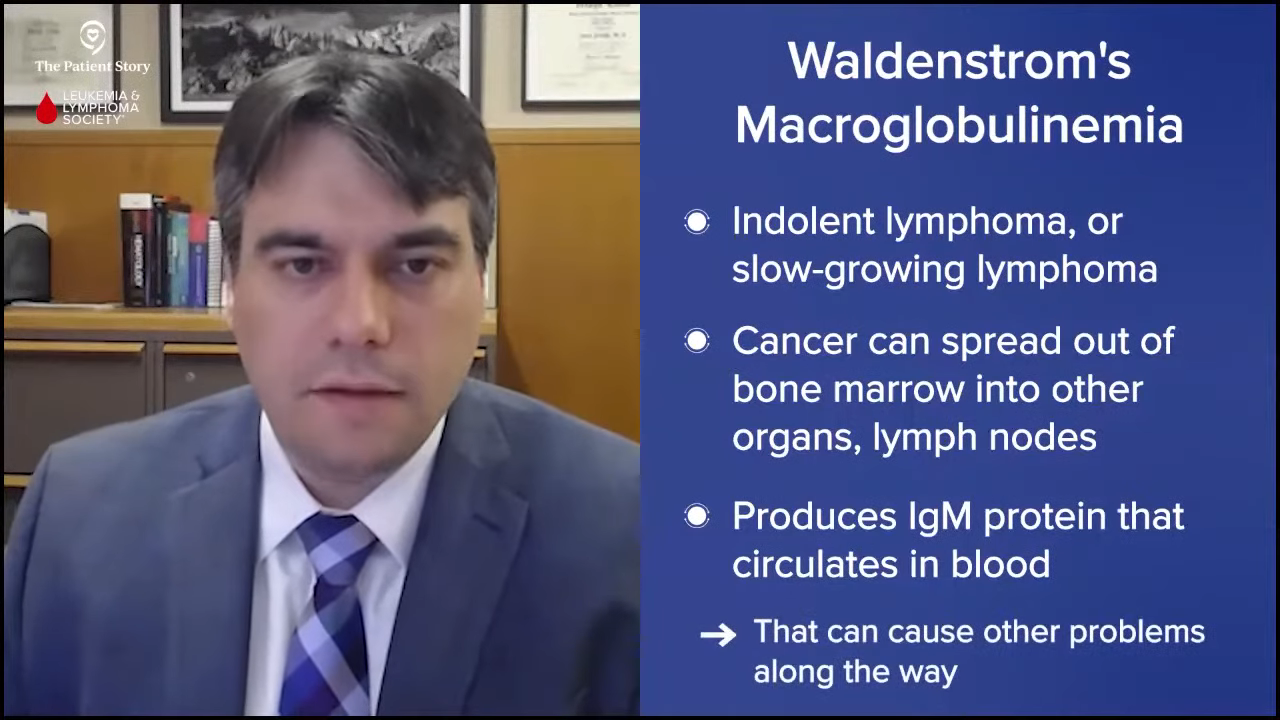
But it does grow very slowly and that’s why we also classify Waldenstrom’s as indolent lymphoma or slow-growing lymphoma. It’s an indolent lymphoma that comes from B cells and belongs to the category of non-Hodgkin’s lymphoma.
Waldenstrom’s is very unique in that not only is the cancer cell in the bone marrow, but these cancer cells can go to other organs, like lymph nodes and the spleen. It also produces a protein called IgM protein that can circulate in the blood and can cause different types of symptoms along the way.
Most Common Symptoms of Waldenstrom’s Macroglobulinemia
Pete: Dr. Sarosiek, we know that WM is rare as Dr. Paludo just mentioned, but what are common ways people find out that they have Waldenstrom’s and what are the symptoms when they’re diagnosed?
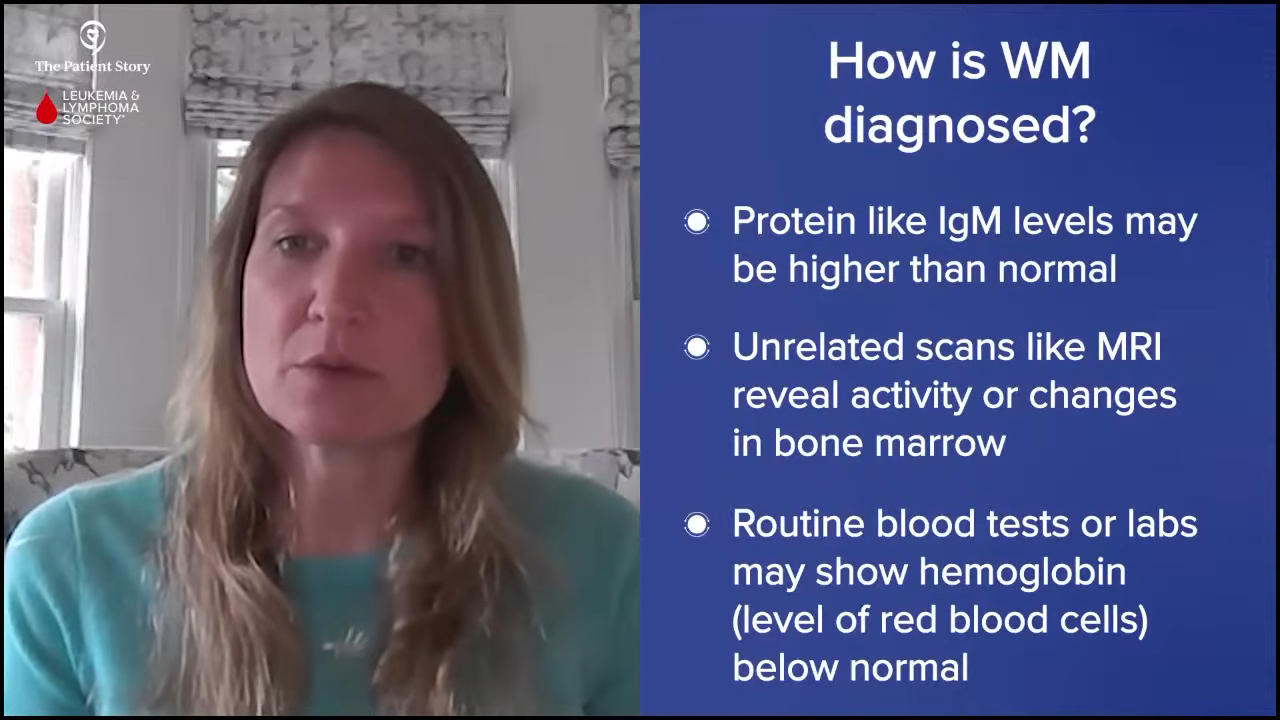
Dr. Sarosiek: Patients find out that they have Waldenstrom’s in a multitude of different ways, but a lot of patients don’t have any symptoms and it’s picked up incidentally when they have other testing done.
One of the most common things I see in my clinic is that during normal primary care follow-up, patients are noted to have a high total protein on routine blood tests. The IgM antibody that you heard from Dr. Paludo is made in Waldenstrom’s and is a type of protein. Often, the protein level in a patient’s blood might be high if they’re making a lot of IgM.
For some patients, it’s picked up because they had an MRI done for other reasons and the bone marrow looks active or looks like it has some changes.
Some patients are noted to have anemia in routine labs. Even if they don’t have symptoms, their doctor notices that their hemoglobin or red blood cell level is a little below normal. Sometimes it’s picked up incidentally; other times, patients have symptoms.
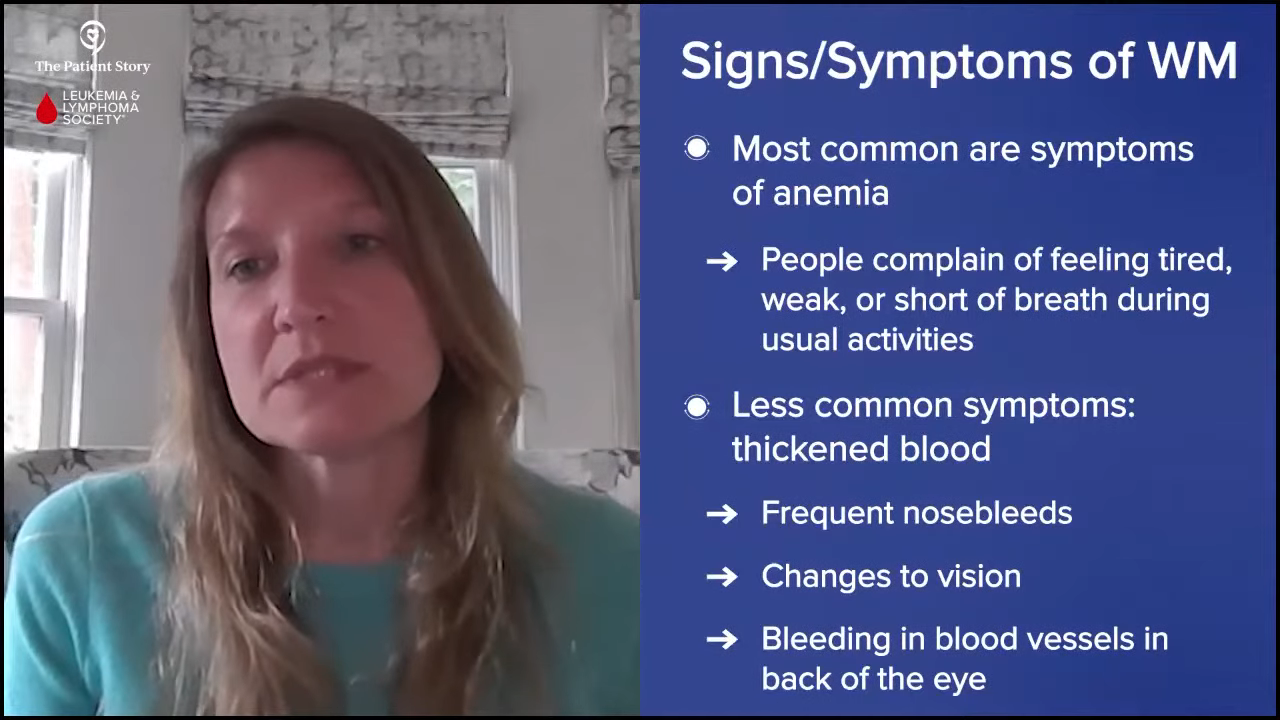
The most common symptoms we see with Waldenstrom’s, both at the time of diagnosis and the time of treatment, are symptoms of anemia. Some patients notice that they’re feeling tired, weak, or getting short of breath doing their usual activities. More commonly, patients attribute their symptoms to aging when in reality, it’s because they’ve developed anemia and their disease has progressed. When symptoms of anemia are present, it might be a cause for a workup.
Another symptom that isn’t as common is hyperviscosity or thickened blood. They might have frequent nosebleeds or visual changes and their eye doctor notices some bleeding in the blood vessels in the back of the eye. Sometimes, they might have symptoms from thickened blood, but it can be a variety of different things that happen and lead to the diagnosis.
Pete: My diagnosis came as a result of a blood test I had for another reason. The doctor said I had elevated protein levels and I thought I needed to cut back on my red meat to lower the protein level. I didn’t know anything about it.
Watch and Wait Process
What is Watch and Wait?
Pete: I’ve had Waldenstrom’s for almost 20 years now, so the definition of watch and wait has evolved and continues to evolve depending on the stage of the disease that I’m at. Initially, it was to see how well the treatments were working but in between treatment periods, watch and wait turns more into a waiting process.
Each time there’s a blood test, you have a little bit of anxiety as to what the results will be. I learned over the years to watch the trends and not focus so much on one blip up or down and that’s helped me relax a little bit. It’s not easy and it can lead to a lot of anxiety on the part of the patient and the caregiver. It’s important to watch those trends and stay in close contact with your doctor.
From the doctor’s perspective, can you describe the watch and wait process?

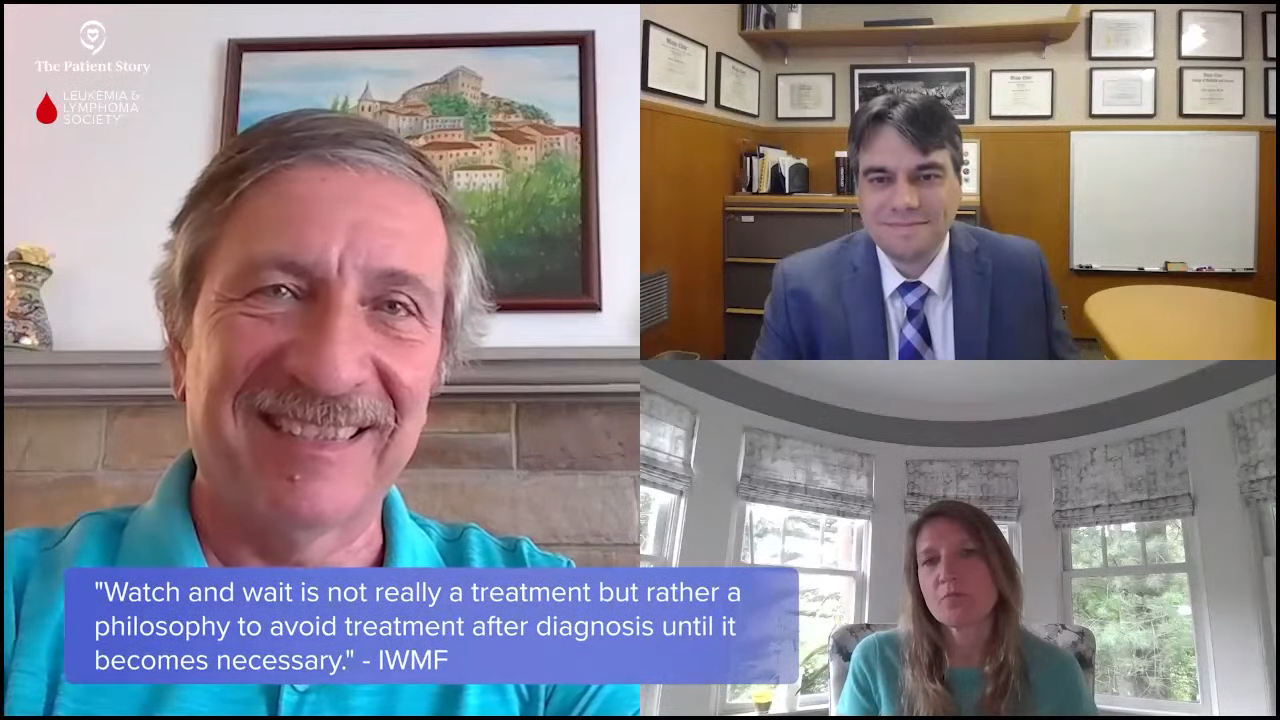
Dr. Paludo: The watch-and-wait process is the time between diagnosis and when we have to do something or start treatment. It’s the period when you’re monitoring the disease and waiting for symptoms or changes that would require treatment.
Pete, as you mentioned, you were diagnosed when they found an abnormal protein level in your blood. I’m assuming you weren’t having any symptoms at that time and that’s the case for a good number of patients diagnosed with Waldenstrom’s. As Dr. Sarosiek mentioned, a patient could have a test done that eventually led to a Waldenstrom’s diagnosis, but they were feeling well and not having symptoms at that time. Because Waldenstrom’s is a very slow-growing disease, we know that a lot of patients can go for many, many years without having any symptoms from this disease.
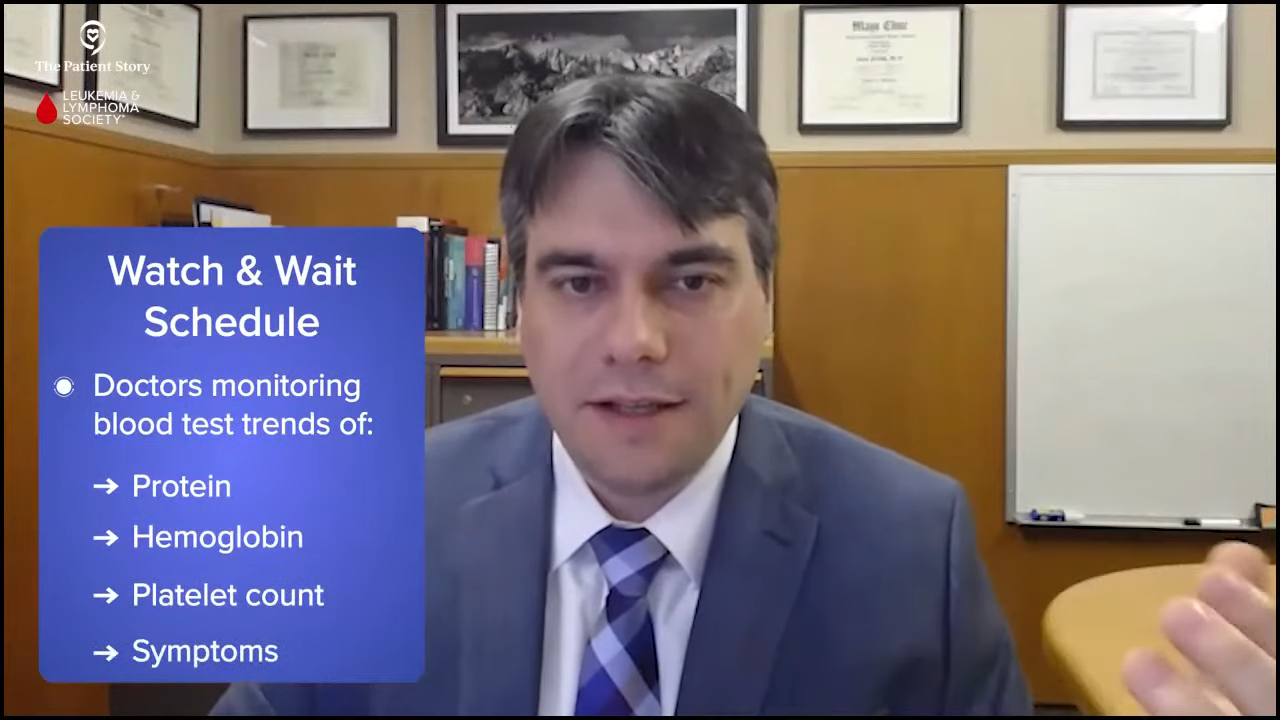
During watch and wait, we are keeping an eye on things and monitoring labs, like the trends of the protein level, hemoglobin, and platelet count. Some people call it active monitoring because we’re doing frequent follow-ups with labs and doctor visits, looking for symptoms or changes that would suggest treatment has to be done.
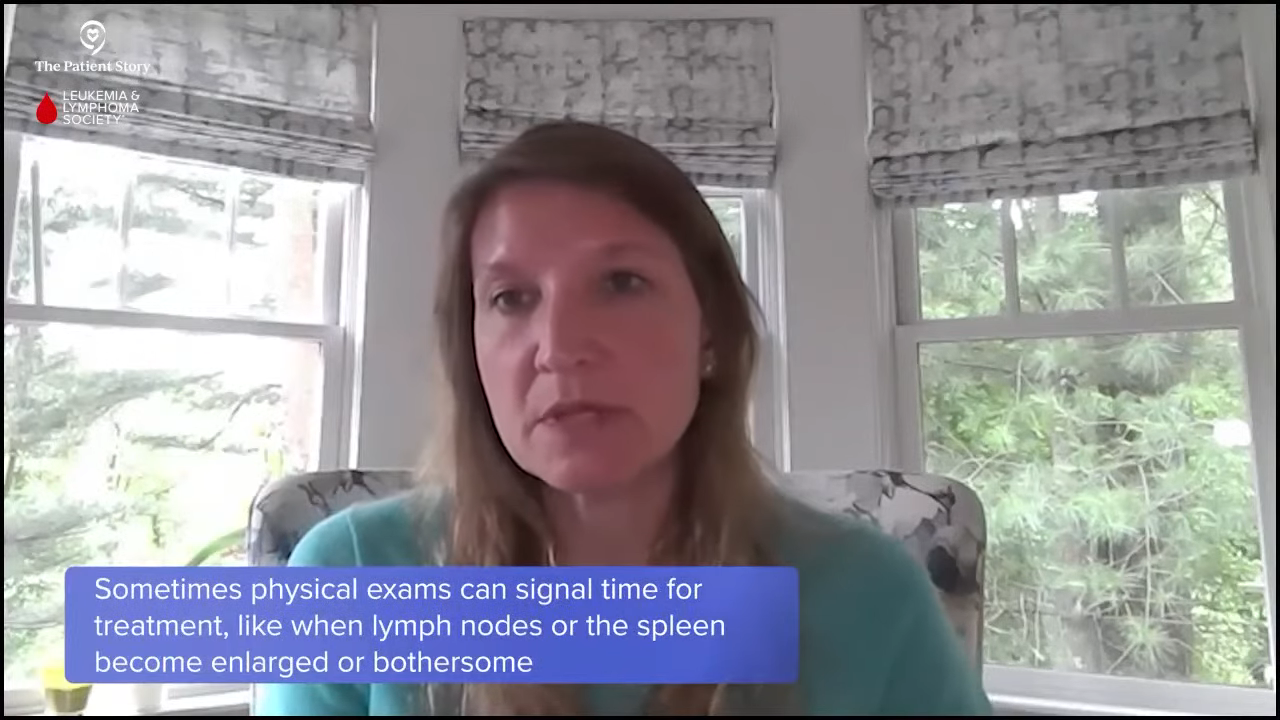
Dr. Sarosiek: I agree with everything you said. Generally, the process of watch and wait, active surveillance, or active monitoring is keeping an eye on a few key things, most importantly patient symptoms. Often, symptoms will align with a patient’s lab results or physical exam, but sometimes they don’t.

We’re trying to maintain a patient’s quality of life, so during that period, we’re monitoring the patient’s symptoms and blood work because if there are changes that are concerning or could become dangerous, then that’s the other thing we want to watch. Sometimes patients develop enlarged lymph nodes or an enlarged spleen.
Pete, you hit the nail on the head by saying that watching the trend is important because there can be some natural fluctuations. The IgM might increase or decrease a little bit. If a patient had a viral infection, it could affect the lab results. It’s more about the trend over the course of time rather than one lab value.
The same thing is true for symptoms. If a patient is sick, they might feel more fatigued but feel better the following week. We like to see the trend over some time during watch and wait.
Pete: I used to keep a spreadsheet to track the trends. My doctor used to expect that and wait for me to hand the sheet that I put together so we could look at the trends together. Thanks to technological advancements, I don’t have to do that anymore.
How Often Do Patients See Their Doctors?
Pete: When someone is in watch and wait, is there a standard frequency of doing blood tests or does it vary?
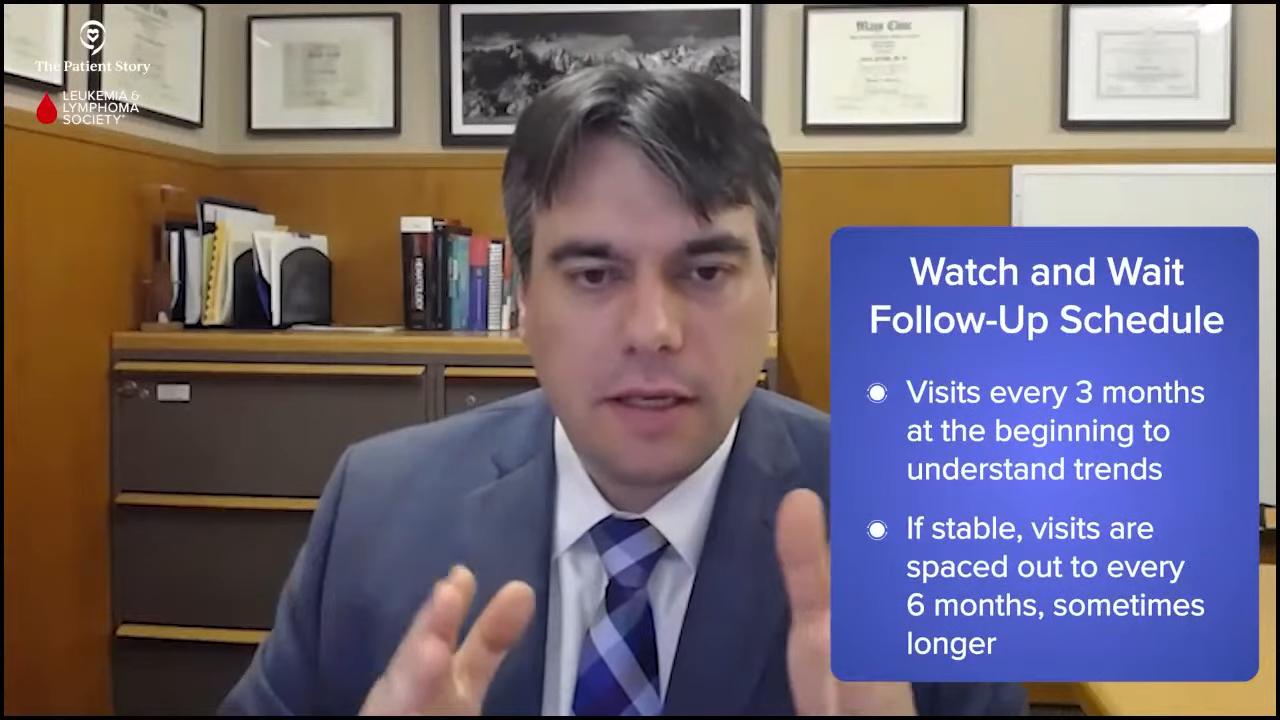
Dr. Sarosiek: It varies from patient to patient. On average for most of my patients, we follow up every three months. A lot of patients have a very slow progression of the disease, but it depends on the patient. Sometimes we have patients who have been stable for years, so we might extend that follow-up to align with what we know is happening with their disease.
In the beginning, patients are adjusting to their diagnosis and learning more about the disease and probably have more questions, so more frequent follow-up sometimes happens. Even if we don’t feel like we need it from a lab perspective, more frequent follow-ups allow us to check in with patients and allow them to ask questions and get used to having this disease. It can be important from a mental health perspective.
I don’t want any of my patients to be at home thinking they wanted to check at two months and spending the last month of the three-month period waiting anxiously. Sometimes, we’ll check in a little more frequently, especially around the time of a new diagnosis, but on average, it’s every three months.
Dr. Paludo: We have a very similar schedule. We tend to follow up with watch-and-wait patients approximately every three months, especially at the beginning as we have a better idea of how the disease is changing and what the trends look like initially. Assuming that everything is stable or mostly stable, then we start to space those visits about every six months, sometimes even a little longer depending on the patient, what they might be experiencing, and where they’re coming from.
Pete: I hadn’t considered the mental aspect behind the timing. You’re not just focused on the physical aspects of what the patient’s going through but also mentally. Looking back, I guess that did happen to me also. I appreciate that that’s part of the art of being a doctor as it’s not just science, so I compliment both of you on your ability to do that.
Top Tips for Getting Through Watch and Wait
Pete: Are there mental health issues surrounding being on watch and wait? I’ve been in various phases of watch and wait as I’ve been through multiple rounds of treatment. Fortunately, I have a strong support network with my wife, my kids, and my family. Through my involvement with the IWMF, I’ve talked to a lot of patients and not every patient has that support. Patient support is important. Talking to other patients and being part of a support group helps.
All that being said, there are still periods where you have rough patches. You don’t know what’s going to happen next and you’re either anxious about where your disease is heading or when the other shoe is going to drop. It’s important to take advantage of your support network, talk to your doctors, and seek mental help if you need it. There’s no shame in seeking help. You’re to be commended for doing so because you’re taking active control of your disease and your condition.
Doctors, what are the most common questions and concerns you get from your patients when it comes to watching and waiting? What are the top tips you provide them when they’re going through that process?

Dr. Sarosiek: Mentally, for a patient who has cancer, something changes in terms of the way that you think about new symptoms that come up. If you don’t have cancer or haven’t had a major medical issue and you have a little bit of back pain, you might think you hurt your back and move on with your day. But once you have an underlying diagnosis, you start to interpret symptoms differently. I see that very commonly and it’s very normal for that to happen with patients with Waldenstrom’s and other cancers. You start to see your symptoms through a new eye.
From my perspective, it’s important to have an open line of communication with your provider to relieve your anxiety, especially at the beginning when you don’t know exactly what to expect. Many patients will reach out to me and say, “I know this probably isn’t related, but I want to reassure myself. I have this new pain or new symptom. Do you think it’s part of the Waldenstrom’s or something bigger to worry about?”
The important part of active monitoring and surveillance is having that open line of communication to be able to ask questions to put into the context of your Waldenstrom’s, which otherwise you might have ignored. Don’t be afraid to ask to allay your anxieties and be able to enjoy your quality of life without having to worry every day about the small things.
Dr. Paludo: Another common thing is being concerned about watching and waiting. A patient is told they have Waldenstrom’s and now that patient is told that we’re not going to do anything about it. I discuss the rationale and the quality of life component, and reinforce that we do not forget about it. We’re going to have frequent regular time points to check and monitor things.
As Dr. Sarosiek mentioned, have an open line of communication and tell the patients to ask questions. If you have any concerns, contact your doctor to discuss them because there could be a great deal of anxiety, especially at the beginning as patients are getting used to living with Waldenstrom’s and not starting treatment right away.
Dr. Sarosiek: It’s important to find support and resources that work best for you. A lot of people have families and friends to support them and though some patients don’t have that, they might find support in other places. A lot of institutions have great social work care or psycho-social teams that can help deal with anxieties and mental health issues surrounding a cancer diagnosis. There are resources like the IWMF.
Some patients benefit from talking with other patients and being active participants on online forums. Other patients may find that overwhelming and don’t want to necessarily get all that information in the beginning. They might want to learn on their own through patient-directed education. Patients should use the resources available to them and find support in ways that they find most helpful. They don’t need to feel like they have to use everything available. It’s about finding a balance of what they feel most comfortable in.
Pete: Those are very insightful responses and hopefully, people find some help and guidance. I’ve been on this journey for a long time and I’m at a point where my disease is behaving itself and has been so for a while. I’m at the point where I’m worried more about my children and my grandchildren. If they have a bruise or some strange thing, I think, Could it be Waldenstrom’s or something related? It’s a different level of anxiety and I hate to admit that, but it’s true.
What Factors Impact the Watch-and-Wait Process?
Pete: Do different patient profiles, like age, gender, geographic location, and other considerations, impact how you work with patients on the watch-and-wait process? Does it matter where they are in terms of what type of patient they are or even where they live?
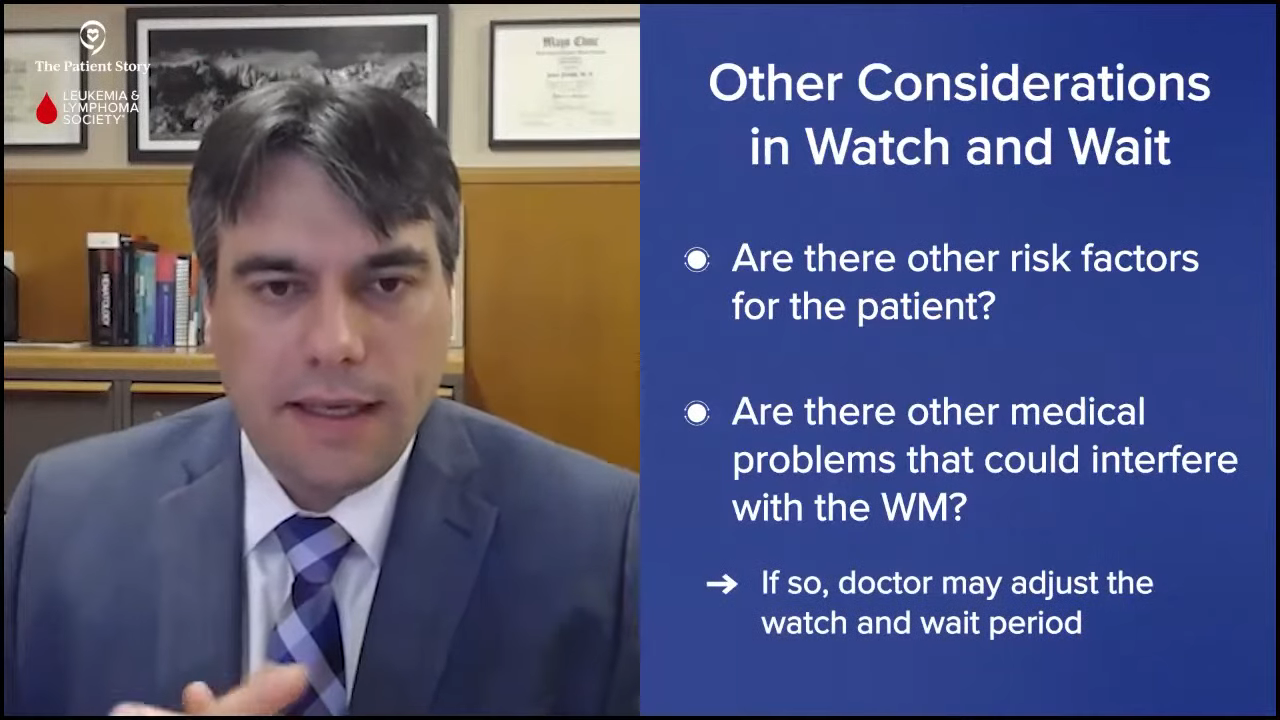
Dr. Paludo: They certainly influence the approach to a certain degree. I think about the interaction of Waldenstrom’s and other medical problems patients may have. For example, am I concerned about a potential kidney problem in a specific patient because they may have other risk factors for kidney problems or am I concerned about something else, like a big spleen?
Depending on how a patient presents, depending on what other medical problems they may have that could interfere with Waldenstrom’s, I may look at that and adjust a little bit of how we watch and wait. At the end of the day, it’s all about the trends in their labs and how the patient is feeling, but depending on other medical issues they may have, we may keep a closer eye or adjust the watch and wait period.
Dr. Sarosiek: You mentioned urban versus rural in terms of where a patient resides. That also can impact continued care. Dr. Paludo and I are both very fortunate to work at larger academic centers where we get to have more experience with specific diseases. If a patient is in a rural area, their local doctor might not see as much Waldenstrom’s.
Connecting with someone at a larger academic center could be helpful in terms of continuing to follow the disease. I work with a lot of local oncologists in terms of developing watch-and-wait plans and seeing what they’re comfortable with and what the patient is comfortable with. In some settings, in terms of developing a plan for active monitoring, it’s not just me and the patient, but it’s me, the patient, and their local oncologist.
Approaching the Mental Challenges of Watch and Wait
Pete: If a patient’s going through a mentally difficult time, do you do anything different in the treatment? How do you work through that process when they’re on watch and wait and they’re particularly anxious?
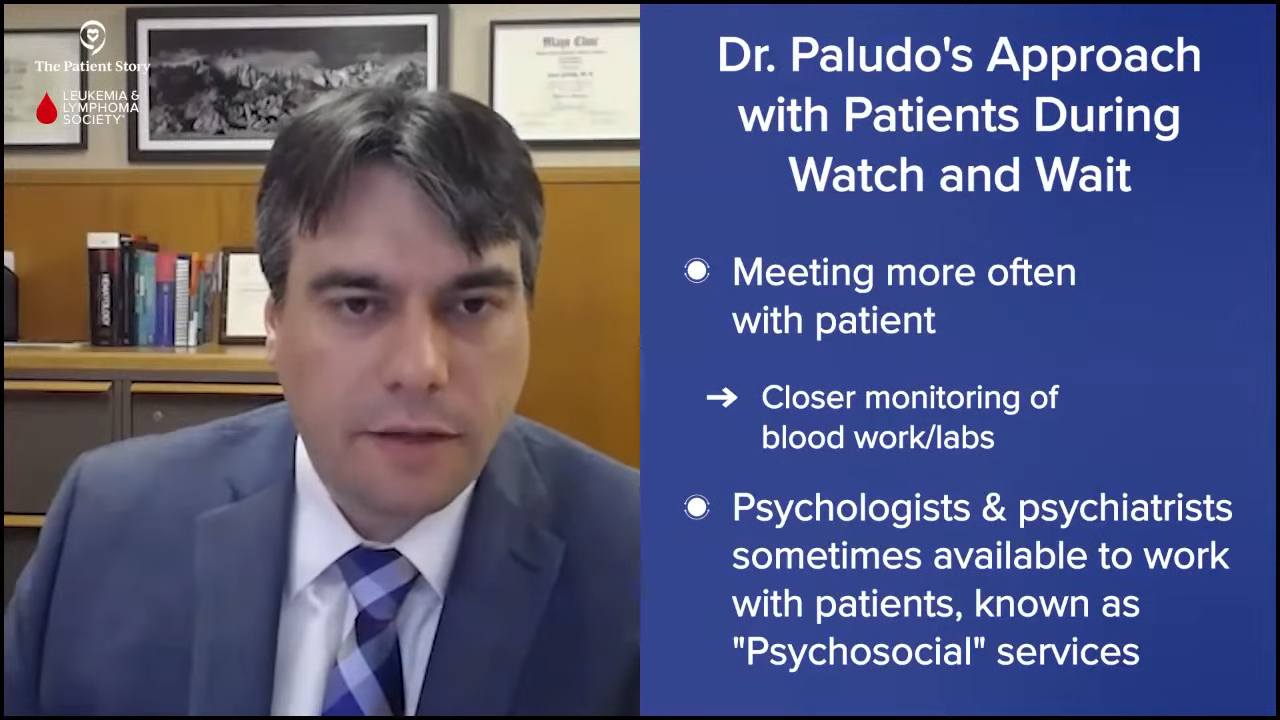
Dr. Paludo: A component of our discussions at patient visits is talking about stressors and anxiety symptoms. I tend to meet more often with patients who may have a higher anxiety level, which is not uncommon. The shorter intervals between appointments allow us to monitor labs a little closer. I found that usually helps a lot with those patients.
More important than that, we’re fortunate to have a very large group of psychologists and psychiatrists at Mayo who are experts in cancer patients. We tend to make a referral earlier in the disease process, so patients would have other professionals to speak with. We also share the different resources available outside of our institution.
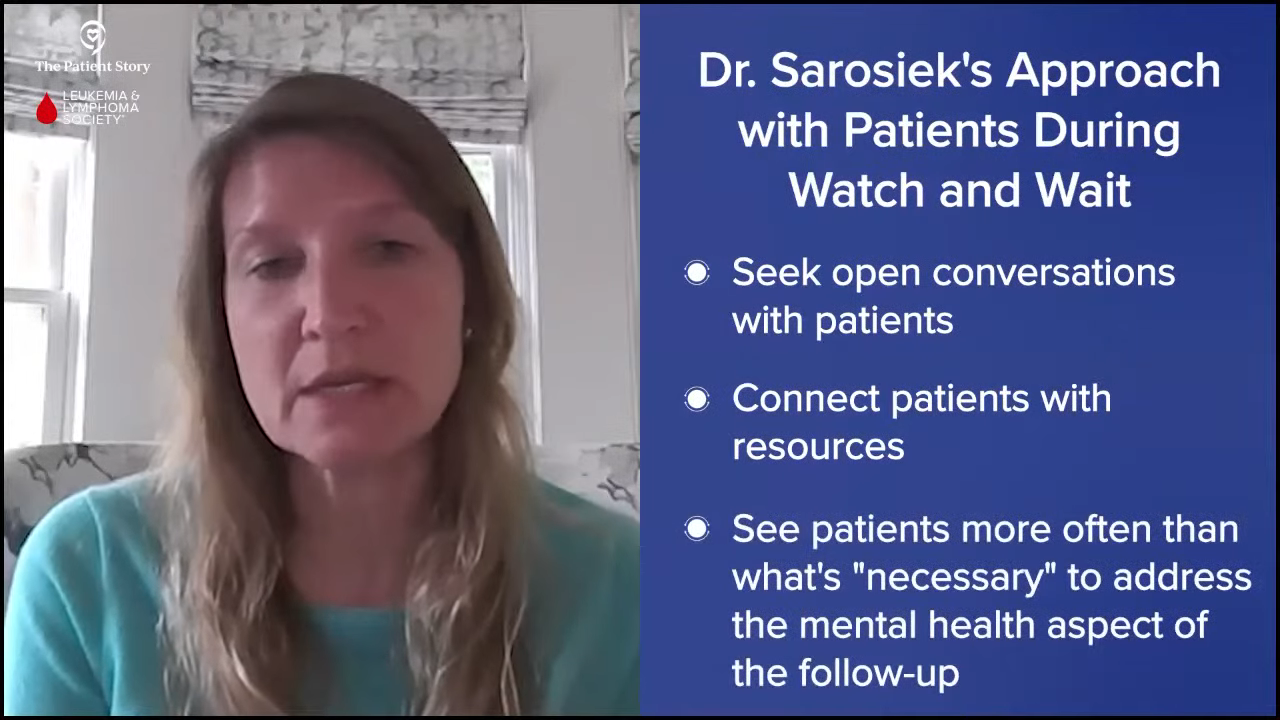
Dr. Sarosiek: Part of the beauty of Waldenstrom’s is since our patients do well and we get to know them very well, we can have open conversations when they’re feeling more anxious or when they would like to be connected to more support systems. Based on our conversations, if they have anxiety about specific things happening with the disease, we can connect them to resources or see them more often.
I have many patients who I would feel comfortable seeing less often from a medical perspective, but the mental health perspective is also very important, so I continue to follow them a little bit more closely to manage that part. Keeping both mental and physical health in mind is an important part of the follow-up.
Importance of WM Caregivers
Pete: I’m a patient, but I also happen to be a caregiver. My wife has a related blood cancer and it’s strange to find myself wearing the caregiver hat. Do you work with caregivers in this regard? Do you have advice for them, specifically when a patient is going through the watch and wait period?
Dr. Sarosiek: Caregivers carry a big portion of the burden of the disease. We have a great social work team and they’re quite wonderful in terms of working with the families and seeing what needs the caregiver or the family member might have.
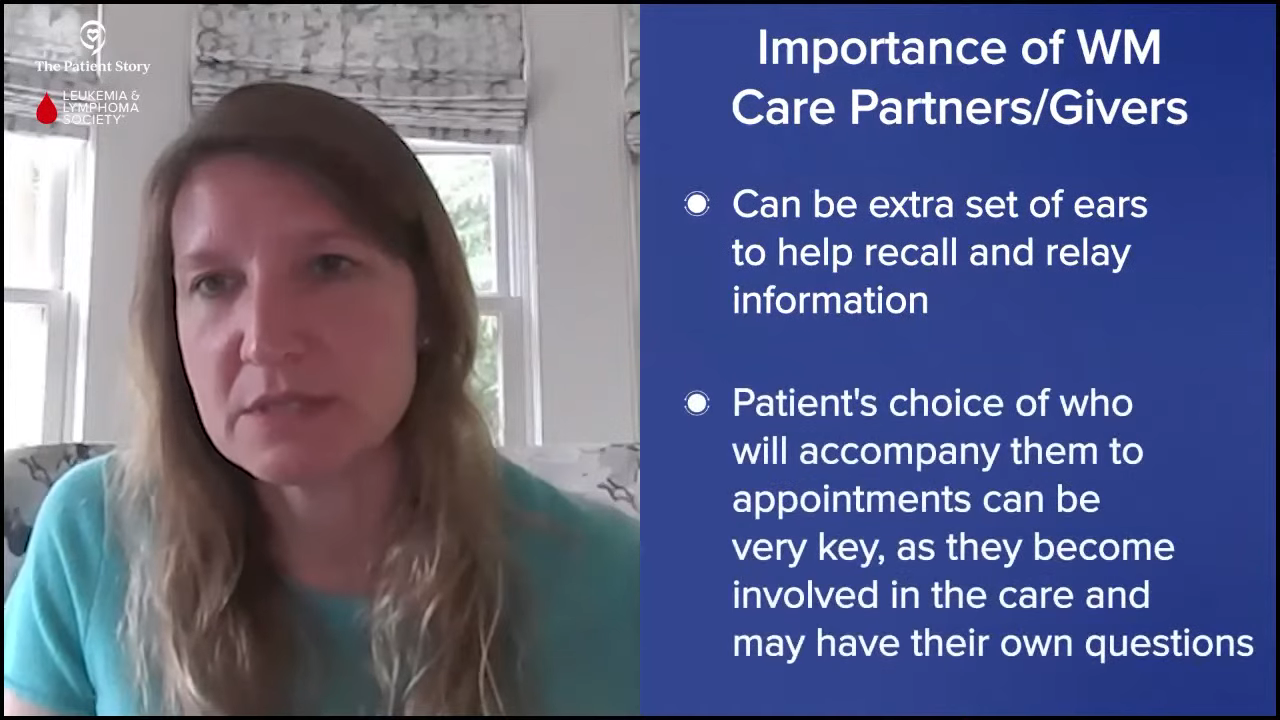
A patient needs to bring someone to an appointment. I always try to address if the family member or caregiver has other questions too because they’re quite involved. They’re often an extra set of ears, help quell anxieties the patient may have later, and can report back information that might have been too overwhelming at the time of the appointment.
A key part of caring for the patient during a visit is whoever they bring along is someone important and involved in their care, so I make sure their questions are answered too.
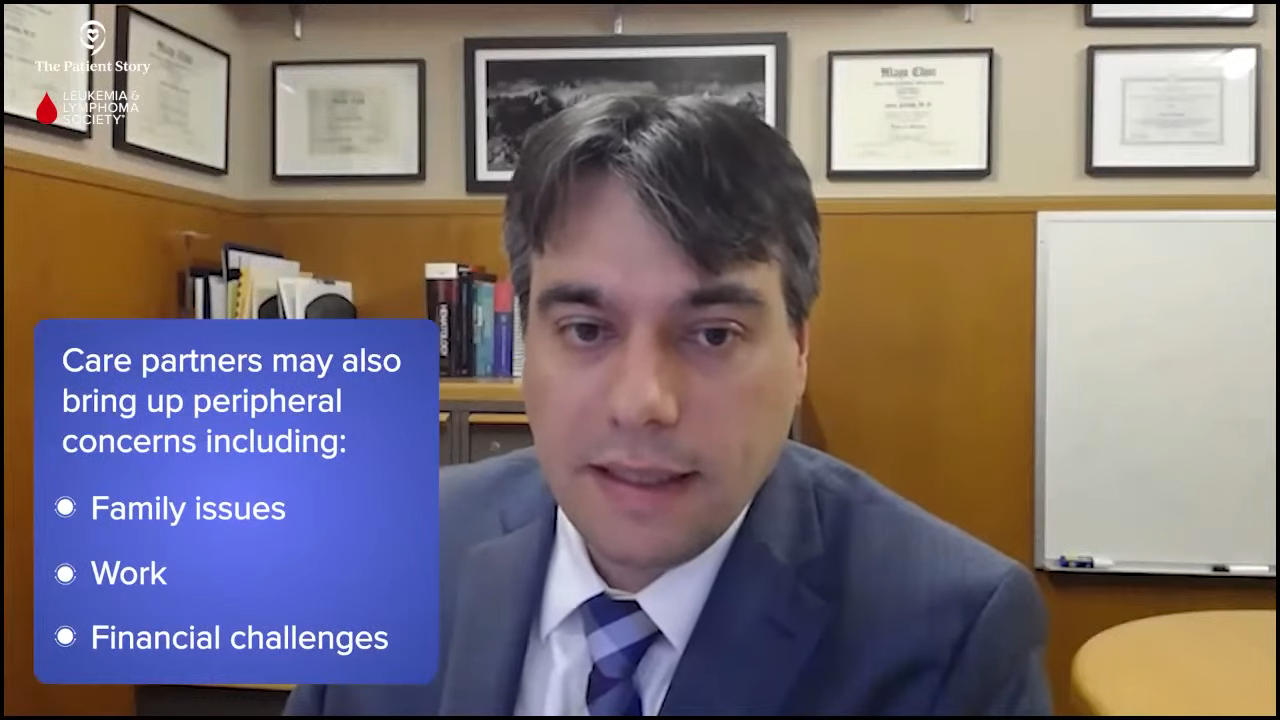
Dr. Paludo: Caregivers are very important, especially in Waldenstrom’s. I include them and check with them because they might be experiencing different types of anxieties and concerns. Caregivers are also looking for other things that we may not discuss, like family, work, and finances, which are important topics that don’t take center stage in the discussions but are important to address. They provide a lot of support to the patient, so it’s important to make sure they’re supported as well.
Pete: Having to wear the caregiver hat, I had a newfound respect for what my wife had been through for years. In some respects, it’s harder than being the patient. I have a lot of appreciation for all the caregivers and physicians who are working with us, trying to help during these difficult periods, whether we’re in treatment or watch and wait.
Latest Treatment Options for Waldenström Macroglobulinemia
Pete: We want to touch on the current treatment landscape or what treatment is like for Waldenstrom’s patients and where we might be headed. When I was diagnosed in 2003, Rituxan (rituximab) was a fairly new treatment paradigm and there were concerns about whether it was safe to take long-term. We know much better now, but back then, we weren’t sure.
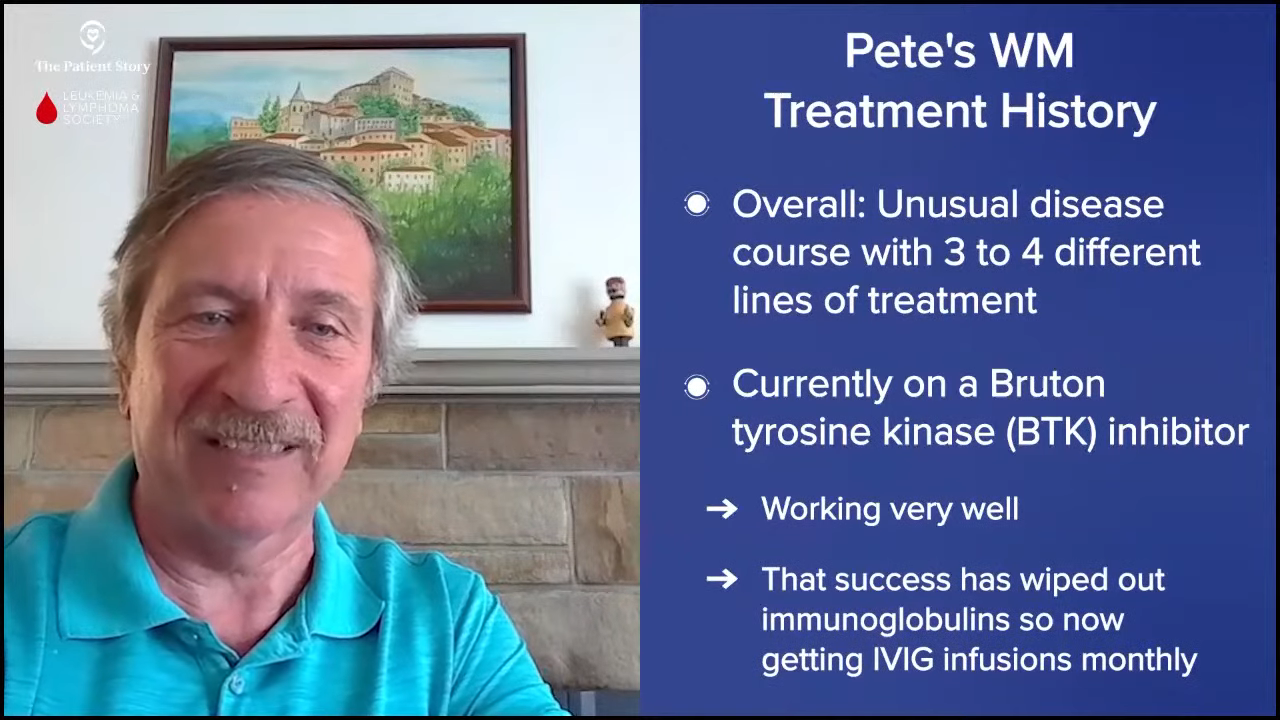
One of my initial treatments, which was fludarabine, cytoxan, and rituximab, isn’t used anymore. I have an unusual disease course, so I’ve had different courses of treatment. I’m currently on a BTK inhibitor, which is working well for me. Because I have a different manifestation of the disease, I also get monthly IVIG.
Every patient is different. What are the current treatment options for patients? If they’re newly diagnosed, what do they have to look forward to in terms of options?
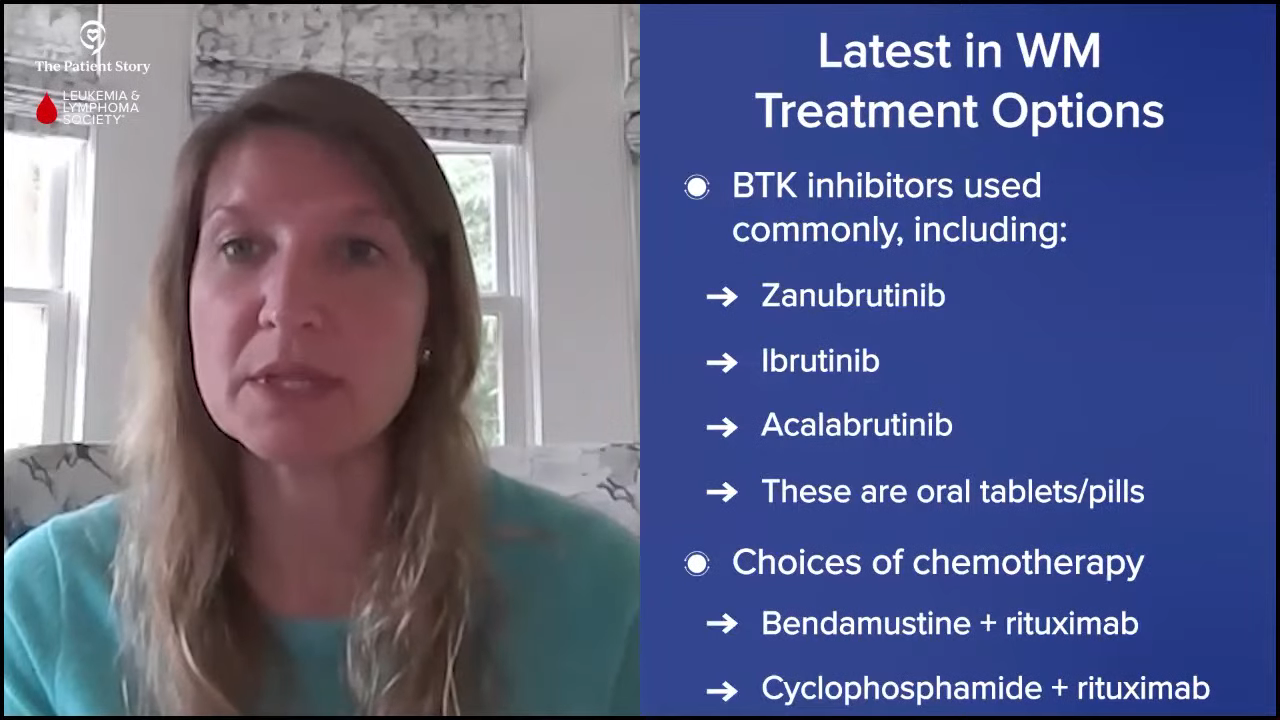
Dr. Sarosiek: Over time, if a patient’s disease progresses or comes back, we have a lot of different treatment options, which is wonderful. Most commonly for a treatment-naïve patient, which means they’ve never had treatment for their Waldenstrom’s, we think of two big categories for first-line therapies.
We often think about BTK inhibitors, like zanubrutinib, ibrutinib, and acalabrutinib. There’s also chemotherapy with rituximab. There are quite a few different chemotherapies. Fludarabine is one of the older ones, but we don’t use that as frequently anymore. In the US, we often use bendamustine with rituximab, but there’s also another chemo called Cytoxan (cyclophosphamide) that can be combined with rituximab. I would say the two most common are rituximab with chemotherapy or BTK inhibitor.
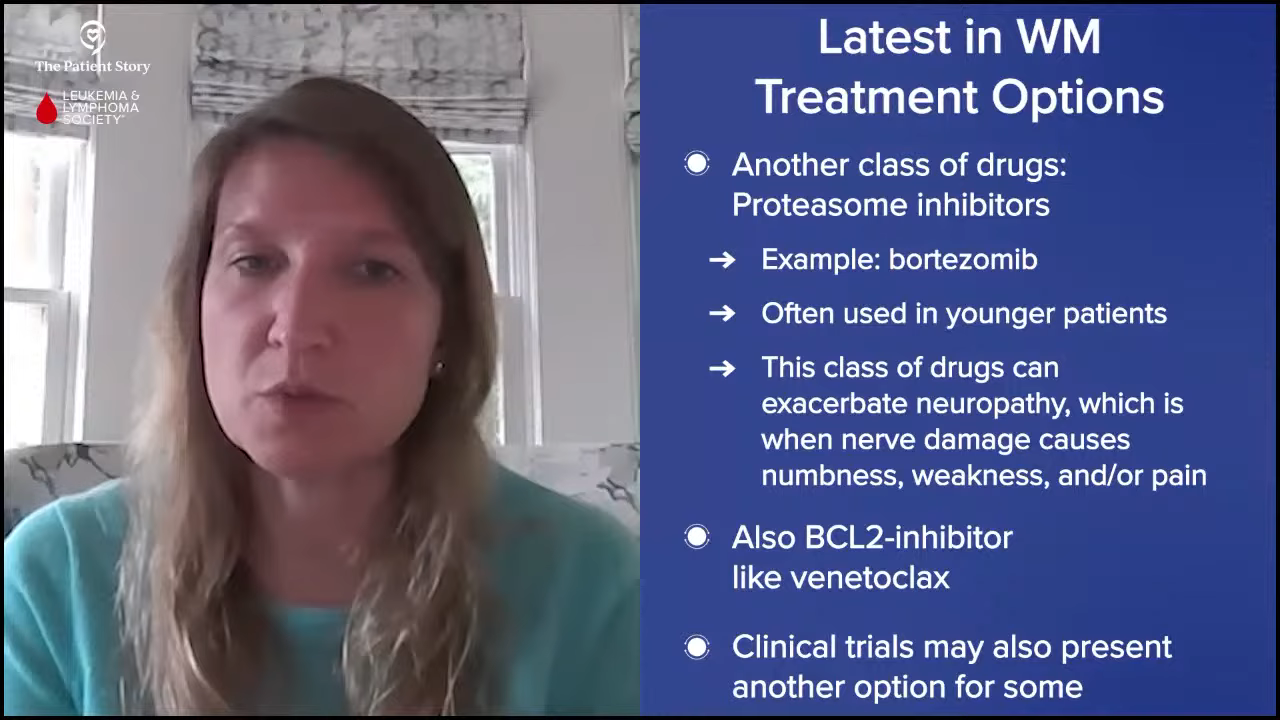
There is another class of drugs called proteasome inhibitors, like bortezomib, or related drugs that we can also use. I tend to use those in younger patients. A lot of patients with Waldenstrom’s have neuropathy, so we don’t use those drugs as frequently because neuropathy can happen with that group of drugs.
There are other oral therapies like venetoclax or the newer BTK inhibitor ibrutinib. There are also different options available as well for patients who have had their disease come back. Clinical trials are also an option, which is the way that we move therapies forward.
We have so many different options and we’re lucky enough to have a conversation with our patients about what might fit their disease and their preferences. Some patients don’t want to take a pill every day, some people don’t want chemotherapy. In most cases, we can tailor therapies to patient preferences and what we might expect to be best for their disease.
Pete: Dr. Paludo, can you talk about fixed-duration therapy versus continuous therapy? What are the differences and what are the advantages and disadvantages?
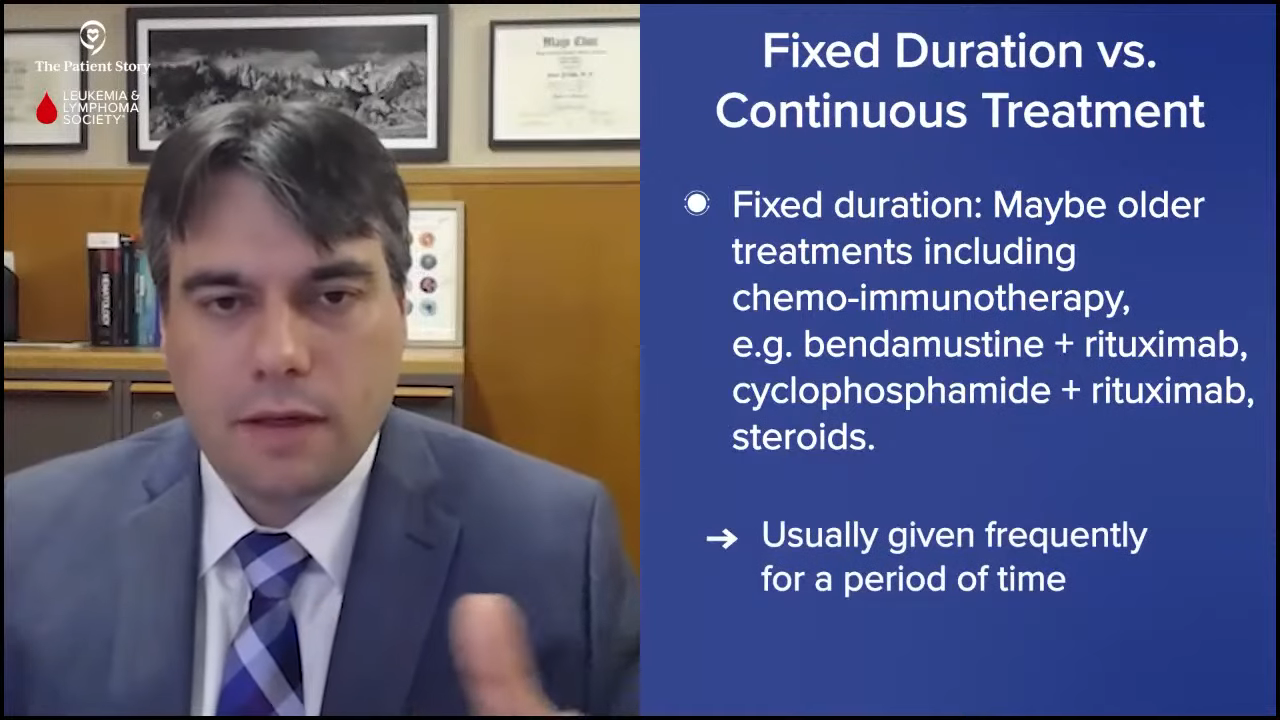
Dr. Paludo: As Dr. Sarosiek mentioned, we are very lucky to have so many different options, a lot more options than we had 20 years ago, Pete, when you were diagnosed. We can divide the different treatments into fixed-duration treatments and continuous treatments.
With fixed-duration treatment, there’s a start date and an end date. Those include chemoimmunotherapy regimens, like bendamustine and rituximab, and cyclophosphamide, rituximab, and steroids. Treatment is usually given at frequent intervals for a specific amount of time.
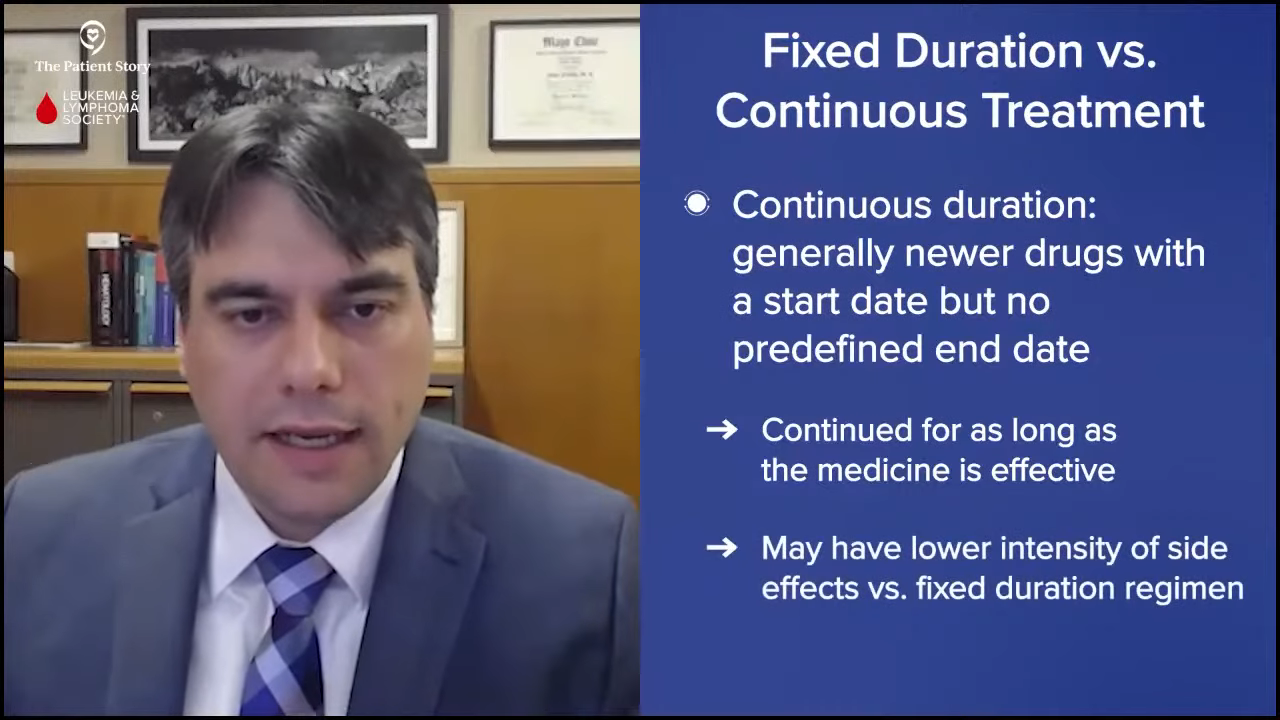
Continuous treatments include newer drugs, like targeted therapy. They have a start date but they don’t have a predefined end date. Treatment is continued for as long as it’s working and not causing side effects that require us to stop treatment. That’s where BTK inhibitors come into play, like the one you’re currently taking, Pete. You’re going to continue on it for as long as it’s working and not causing enough side effects to impact your quality of life to justify stopping treatment.
We usually think of fixed-duration treatments as having more side effects at a higher intensity and that’s why they’re given for a certain duration. Continuous therapy tends to have a lower level of side effects so patients can continue on treatment for a long time. Patients can choose what fits them better, whether it’s fixed-duration treatment or continuous treatment.
Promising Clinical Trials in Waldenström Macroglobulinemia
Pete: What’s always interested me was when it was time to decide, the doctor would tell me my options and ask which one I wanted. We’re fortunate as WM patients to have so many different options available regarding treatment, which is a testament to the amazing research being done to move the ball forward.
We look forward to the newer agents down the road and better treatments in the future for improved quality of life for all. With that in mind and looking at the future of treatments, what’s exciting at this point? What are some of the studies you’re most interested in, and why should patients and care partners be interested in participating in a clinical trial specifically?
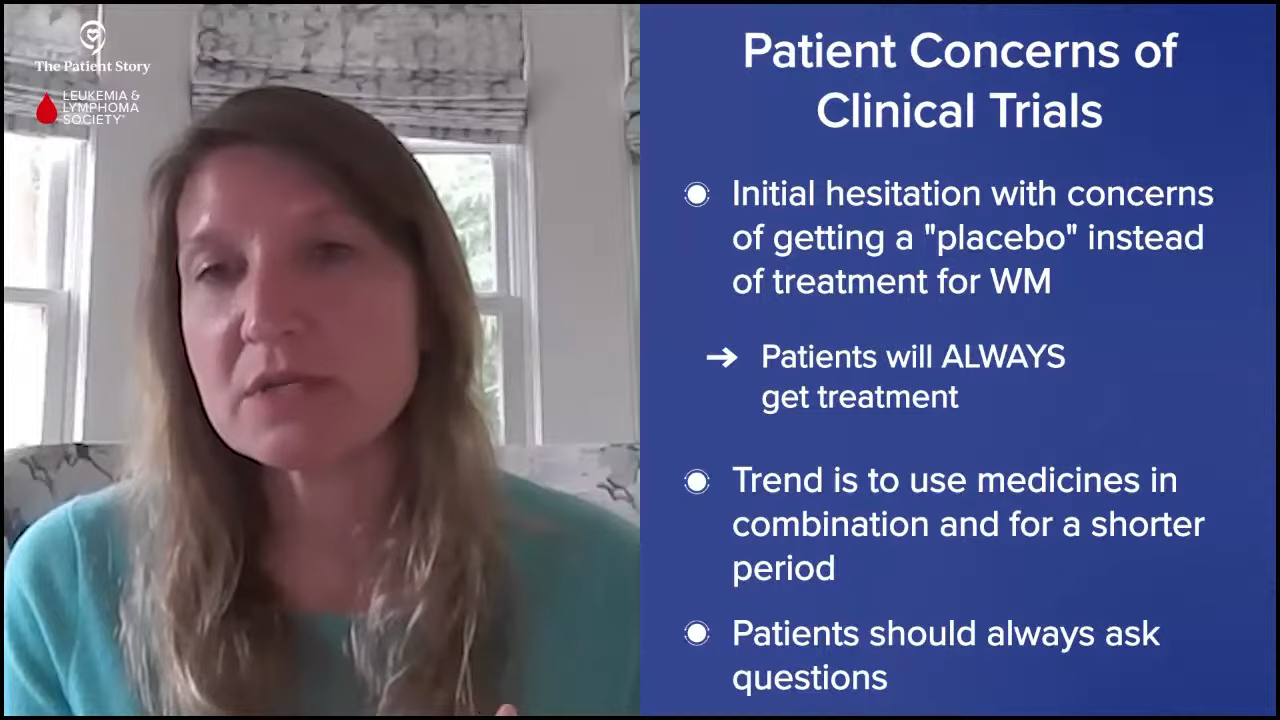
Dr. Sarosiek: Clinical trials are how we move forward in the field. We’re in an exciting time with the number of clinical trials that we have available for Waldenstrom’s and there are quite a few that I’m interested in. When I bring up Waldenstrom’s clinical trials to patients, there’s an initial hesitance because of concern that a patient would get a placebo and not get treatment for their disease.
An important thing to remember is that we’re certainly treating our patients and what the trials do is try some of the treatments in a new way. Maybe a specific treatment was effective for other types of lymphomas and we’re seeing if it would work in Waldenstrom’s or if a combination of two effective therapies has been used before, we’re studying if we could use both for a shorter duration.
Patients should always be open to asking questions about clinical trials if they have any hesitancy, are worried that they’re not going to get active therapy, or are worried about side effects. Some trials offer an opportunity to get something new and different that might be more effective based on some encouraging background data.
We have a couple of ongoing clinical trials for patients with Waldenstrom’s, a precursor of Waldenstrom’s, or who don’t quite meet the criteria for Waldenstrom’s but have an abnormal IgM antibody. Patients can develop neuropathy that affects the lining of the nerves We have a clinical trial open for exploring that neuropathy differently by treating the underlying abnormal IgM and then following the patient’s nerve damage over time and hoping to find something that’s effective. That trial used rituximab with acalabrutinib to see if that regimen can protect the patient’s nerves.
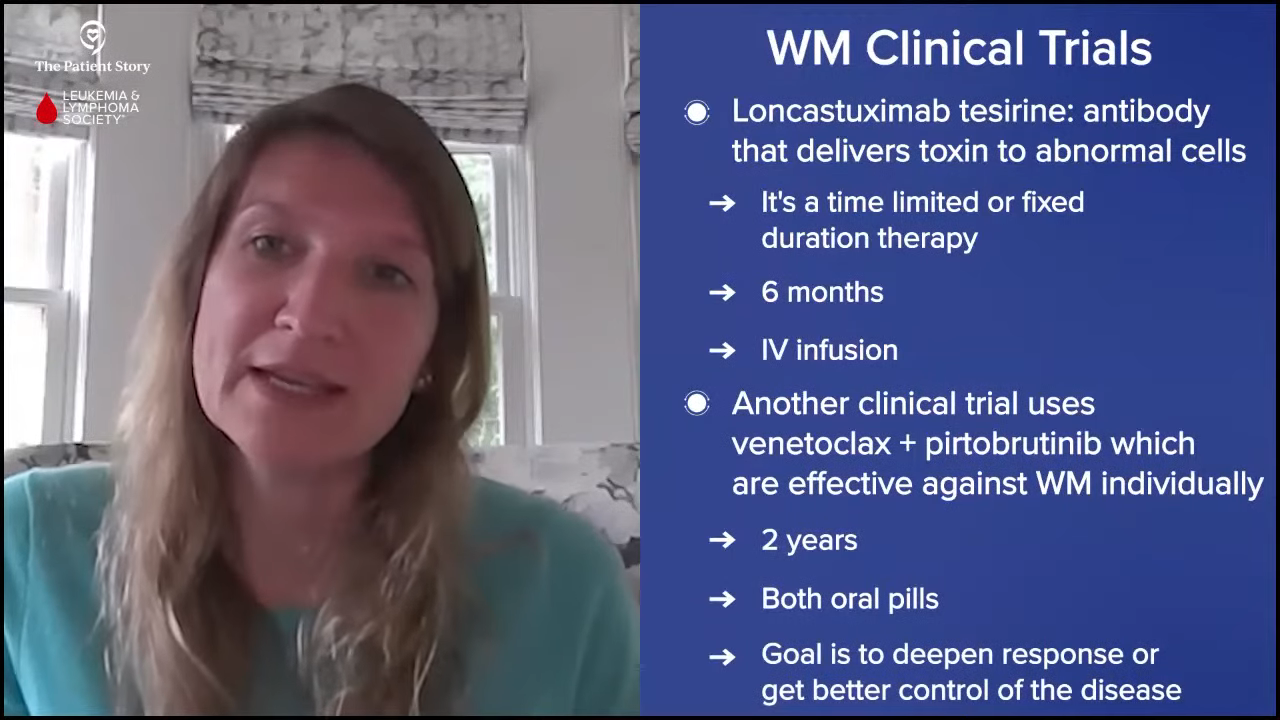
Another clinical trial we have is using a drug called loncastuximab tesirine, an antibody that delivers a toxin to the site where the abnormal cells are, and that’s a limited-time therapy of six months. The trial is ongoing and it’s for patients who have had at least two other types of therapy in the past.
We have another clinical trial that’s using two oral therapies, venetoclax and pirtobrutinib. We know both of those drugs are effective in Waldenstrom’s on their own, but this trial is using a combination of both for two years in hopes of deepening or getting better control of Waldenstrom’s, and also in hopes of allowing patients to come off treatment after two years.
I could go on and on about many other clinical trials available for Waldenstrom’s, but those are some of the more exciting ones that we’re talking about. Dr. Paludo, do you have other thoughts about clinical trials for patients with Waldenstrom’s?
Dr. Paludo: Participating in clinical trials is very important for patients and the community. Participating helps patients have new and other different treatment options available and that’s how we got where we are right now. Often, the first patients to benefit from a new treatment are the ones in the clinical trials, so the ones in the ibrutinib clinical trial are the first ones to benefit from that drug and become the standard of care. Hopefully, loncastuximab will become part of the standard treatment in those patients in clinical trials who are the first ones to benefit from that.
There are several clinical trials available for Waldenstrom’s. There are a few that are very interesting and seeing results and I hope they will be available soon. There are some trials comparing differences in the treatment regimens and classes that we were talking about earlier, trying to see if one is better than the other, or which situation to use one or the other.
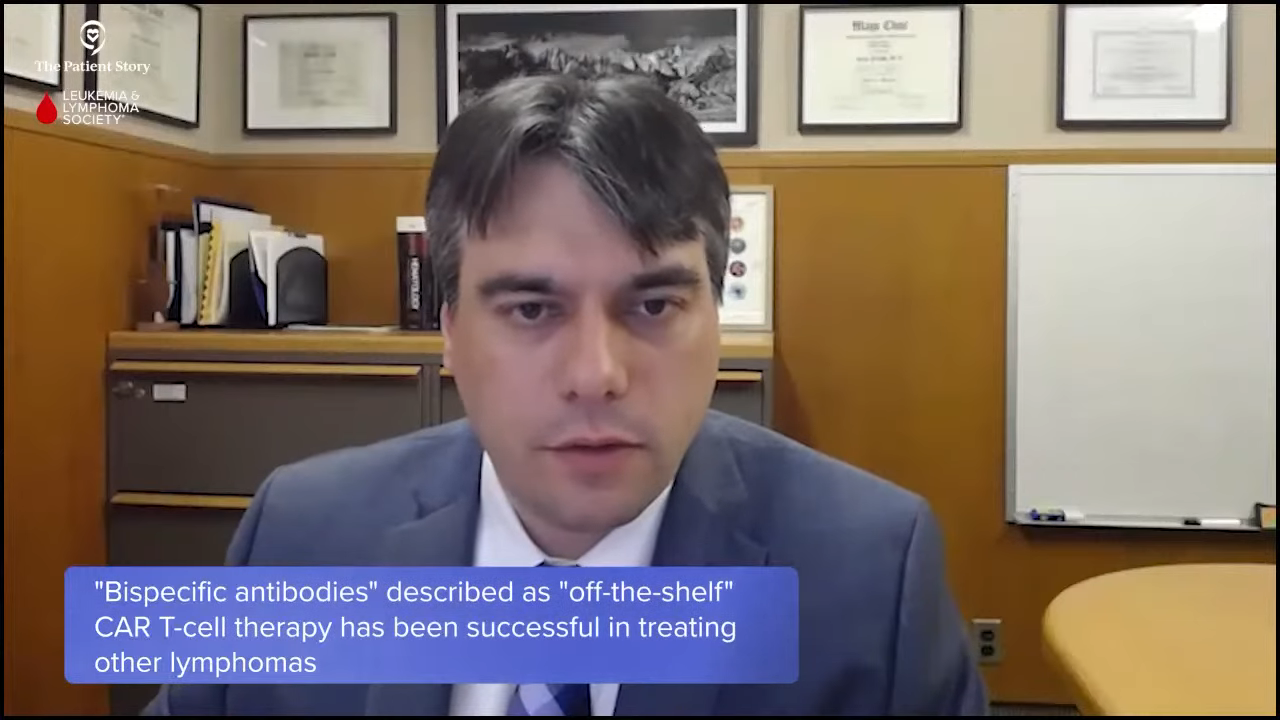
We don’t have the specific trials yet, but I’m looking forward to seeing what novel types of immunotherapy drugs will bring to Waldenstrom’s field. I’ll be very curious to see what we’re going to find with bispecific antibodies in Waldenstrom’s. We have seen excellent results in different lymphomas similar to Waldenstrom’s and I’m hoping that we’ll have clinical trials soon that will be able to investigate if those treatments are helpful in Waldenstrom’s as well.
Pete: With the clinical trials, what it comes down to is that it’s an opportunity to be on the cutting edge in a sense of what treatments are out there and find something that will work well for you.
Correct me if I’m wrong, but the thing that people should take away is that if you are in a position where you need treatment, you will get treatment whether it’s from a clinical trial drug or another treatment.
Dr. Sarosiek: That’s correct. No matter what, patients need to understand that if their disease needs treatment, they will get treatment for their disease. If they qualify for a trial and want to participate, they can do that. We would never advocate for a clinical trial that wouldn’t provide the treatment that the patient needed.
Dr. Paludo: We also look for clinical trials that make sense for the patient. If the patient needs treatment, do the new drugs in clinical trials make sense for that patient or do they have potential side effects that will cause more trouble? If so, we would avoid those clinical trials. When looking for a clinical trial or treatment, it has to fit the patient.
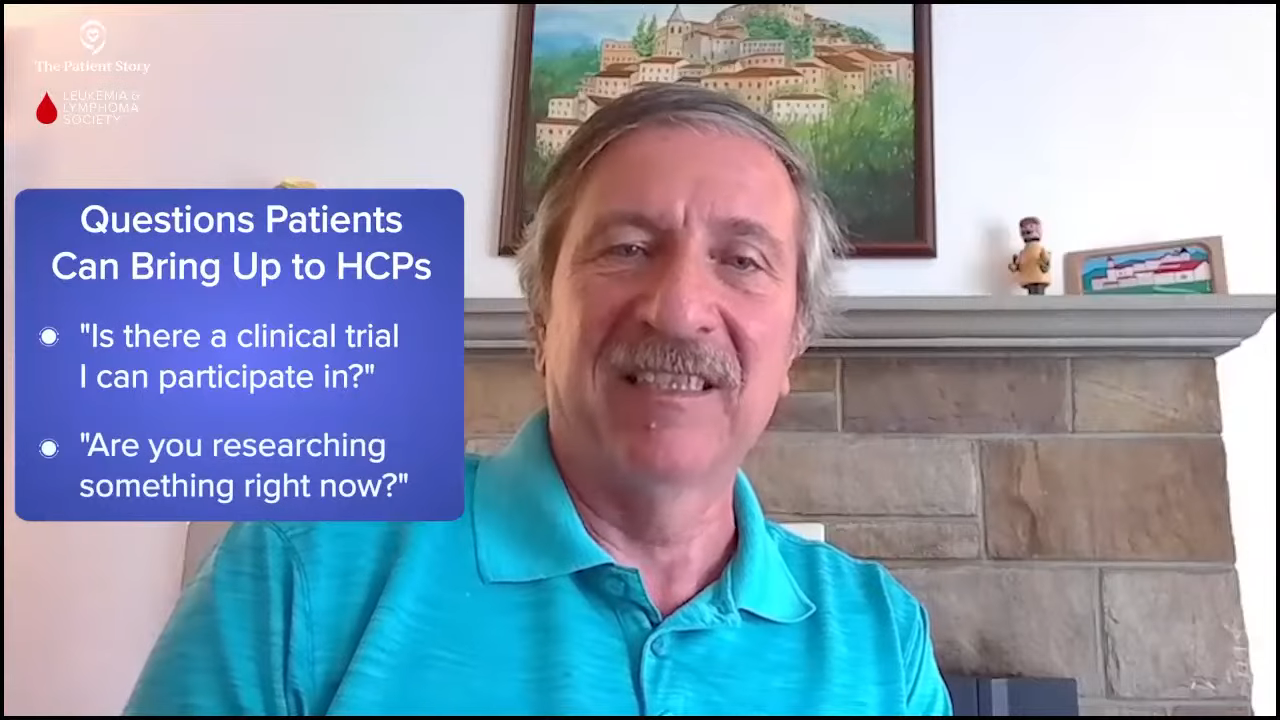
Pete: Patients could always ask if there’s a clinical trial that they can participate in. Depending on where they’re located, they may have to reach out to people, like at Mayo Clinic and Dana-Farber, to see if there are trials available. They may have to travel, but they have an option. I encourage patients to always look at clinical trials and see if any of them are the right fit for them because you help yourself and you also help other Waldenstrom patients in the process. It’s a win-win situation.
Final Takeaways
Pete: Dr. Paludo, as a final message to any patient who’s in watch and wait, what would you tell them to alleviate their anxiety and mentally dealing with being on watch and wait?
Dr. Paludo: I always try to convey to my patients that being able to watch and wait is very positive. It’s an excellent situation to be in where you don’t need treatment. You want to kick that can down the road only when you have symptoms. Work with your hematologist. You need to follow up. Despite all the anxiety that comes with it, being on watch and wait is an excellent position to be in.

Dr. Sarosiek: Watch and wait or active monitoring is a personalized process. It can be adjusted and will be adjusted as needed for each patient in terms of what to follow up on and how often to follow up. I encourage everyone to find a physician who they’re comfortable with, who they can go through that process with, and who they feel is supporting them.
Pete: As a patient myself, I always appreciate my doctor and the advice that he gives me. Having a good working relationship with your doctor and having your caregiver involved is important, so make sure to have someone come to your appointments with you.
It’s okay to let your emotions out. Be upset, yell, and cry if you need to. Don’t hold it in. But if you find that that doesn’t help, reach out to your doctor, to your care professionals, to social workers, and to whatever support is available to you. Take advantage of that support network. You don’t have to suffer alone. There are people who can help you through the process.

The Leukemia & Lymphoma Society
Stephanie: Before we wrap up this discussion, I’d like to spend time on a very great hands-on resource at your fingertips, The LLS’ Information Resource Center, which features specialists who work with people one-on-one. Joining us is Jennifer Wilson, a senior information specialist with The LLS. Jennifer, can you share the basics of how you are helping patients and care partners in general?
Jennifer Wilson: We want to make sure that whether someone calls us for the first time or the 40th time that we hear what they need. Sometimes people can identify it, but sometimes they can’t. We want to make sure that they have good, up-to-date information on their disease and treatment options and how to get support because we know that what your needs are from day one can be very different over time.
Stephanie: For Waldenstrom’s patients and care partners in particular, what are some of the common questions and topics that come up, and how do you help the people who approach you?
Jennifer: When someone is newly diagnosed, oftentimes they may be told that Waldenstrom’s is a chronic illness so they’re going to watch and wait, but to hearing that can be completely overwhelming. We prefer to use the phrase “active surveillance” because that indicates that they’re keeping an eye on things. They’re not waiting to see what happens. They’re very deliberately monitoring to manage the disease.
Then we look at what supports are available. We have the First Connection® Program, a peer-to-peer program so that someone with Waldenstrom’s would have the opportunity to speak with someone else who has been in watch and wait to find out what that felt like and how to communicate with their friends and family.
We have an online non-Hodkin lymphoma chat. For the caregiver, we have a caregivers chat. We have a community with a designated group for Waldenstrom’s patients and family members. We have local support groups and education programs because knowing about one’s disease and treatment options is essential.
A lot of times, we help patients figure out what they need to ask at their next appointment to ensure that when they leave the doctor’s office, their top five questions have been answered.

Conclusion
Pete: Thank you again to both of you, Drs. Paludo and Sarosiek. We look forward to future discussions and further advancements in the clinical trials and the future of Waldenstrom’s research.
Stephanie: Thank you, Jennifer, for the work that you’re doing to help patients and families everywhere, including those who are dealing with Waldenstrom’s. We want to thank both Blood Cancer United and the IWMF for being incredible partners.
Thank you, Pete, for leading an incredible discussion, spending the time, and your advocacy in general. You have made an immeasurable impact in this space.
Thank you, Dr. Sarosiek and Dr. Paludo, for the work that you’re doing both in the clinic with the people you’re helping directly in Waldenstrom’s and beyond, and also all the research that you’ve contributed to lifting the possibilities for everybody with Waldenstrom’s.
I hope that this discussion was helpful and that you walk away feeling more confident. We hope to see you at a future program.
If you read and/or watched our program, we encourage you to take our program survey to help us improve future programs and answer your questions.

Special thanks again to Blood Cancer United for its support of our independent patient education content and the International Waldenstrom’s Macroglobulinemia Foundation for their partnership. The Patient Story retains full editorial control.