Together in Treatment: Strengthening Your Myeloma Care Team
Edited by: Katrina Villareal
The relationship between a patient and their doctor can make all the difference. A strong partnership leads to more informed decisions, personalized care, and a greater sense of control. Myeloma patient advocate Michelle and her doctor and myeloma expert Dr. Caitlin Costello discuss what makes their patient-doctor teamwork truly effective.
Learn how to build trust and open communication with your healthcare team. Understand the role of shared decision-making in multiple myeloma care. Hear first-hand experiences of navigating a chronic cancer with your doctor by your side. Discover practical tips for advocating for yourself or a loved one in the treatment process. Explore how teamwork fosters a supportive environment for long-term care.

We would like to thank The Leukemia & Lymphoma Society for its partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- Initial Multiple Myeloma Symptoms and Diagnosis
- Explaining Multiple Myeloma to Patients
- Common Questions After a Multiple Myeloma Diagnosis
- Getting Involved in the Decision-Making Process
- Factors to Consider in Shared Decision-Making
- Multiple Myeloma Treatment Journey
- Coordinating Care with Multiple Healthcare Providers
- Managing Patient Care From Afar
- Importance of Quality of Life in Driving Treatment Decisions
- Data That Looks at Quality of Life for Multiple Myeloma Patients
- Approaching the Clinical Trial Conversation
- Key Takeaways
- Conclusion

Introduction
Tiffany Drummond: I’m an advocate who has worked in cancer research for 20 years, but more importantly, I became a care partner advocate when my mom was diagnosed with endometrial cancer in 2014. Her journey led me to find out as much as I could to help with her care. Information wasn’t easy to find, so I’m honored to join The Patient Story in putting on programs to help people navigate life after diagnosis.
This program is hosted by The Patient Story, where we aim to help people navigate life before, at, and after diagnosis through empowering patient stories and educational discussions where we focus on how patients, caregivers, and their partners can best communicate with their doctors as they go from diagnosis through treatment with myeloma.

We want to thank The Leukemia & Lymphoma Society for its partnership. The LLS offers incredible free resources, like their Information Specialists, to help you communicate with members of your healthcare team and provide information about treatment options.
The Patient Story retains full editorial control over all content. I hope you find this information helpful, but please keep in mind that this program is not a substitute for medical advice.
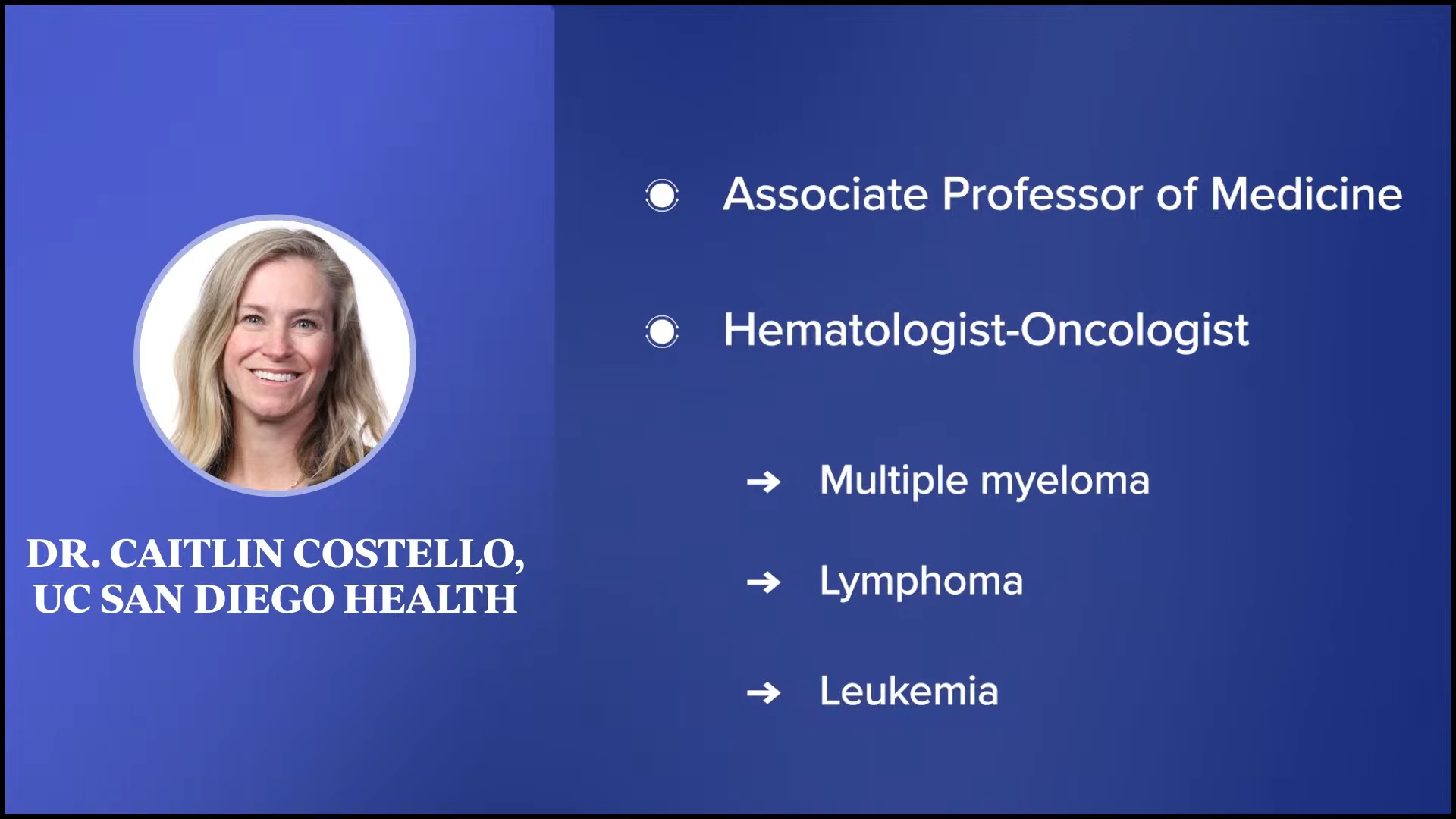
We have two special guests from whom we can learn more about the patient-physician partnership. We have Dr. Caitlin Costello, an associate professor of medicine at UC San Diego Health and a hematologist-oncologist specializing in blood cancers, including myeloma, lymphoma, and leukemia. We also have our patient advocate, Michelle, who is a multiple myeloma fighter and a survivor.

Initial Multiple Myeloma Symptoms and Diagnosis
Tiffany: Let’s start back to your initial diagnosis. What was that experience like for you?
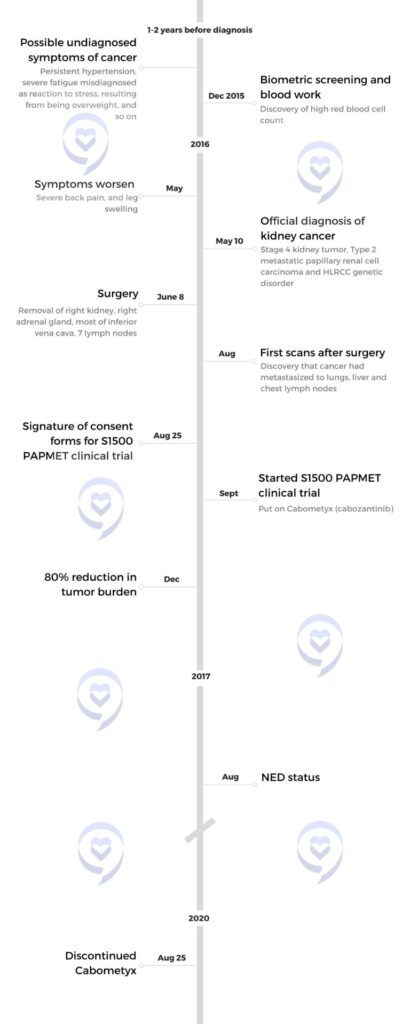
Michelle: I was diagnosed in 2016 at the age of 35. I had a five-year-old and a one-year-old at the time. The year leading up to my diagnosis, I had on-and-off back pain, which they said was because my muscles weren’t strong after having a baby. I was starting to lose weight, which they attributed to breastfeeding. I ended up having other symptoms that led me to go to the doctor more.
But then I ended up having severe stomach pain, which at times made me want to drive myself to the ER. I also ended up having itchy scabs all over my body. I went to the dermatologist and my general physician. They both started digging, and my general physician started ordering lab work, which eventually led to the diagnosis of multiple myeloma.
Tiffany: You knew in your gut that something wasn’t right. What did it take for you to advocate for yourself? And when you were referred to a specialist or a hematologist-oncologist, what was your initial experience like?
Michelle: My husband travels for work. was at home with my one-year-old and five-year-old when I was having stomach pains. I didn’t know what to do. I almost drove myself to the ER one day. I took a breath, pulled over, and the pain stopped. I called my doctor and told him he needed to see me the following day. I had already seen the dermatologist about the scabs all over my body. She looked into things and I didn’t know if any of my symptoms were related.
The doctor called and said, “You need to come in right now.” My husband was home, so we picked up our one-year-old and drove to the doctor’s office. My husband stayed with our one-year-old so I could listen to what the doctor was saying.

When we got home, we started making calls…. They all led us to Dr. Caitlin Costello… She fit me in right away, and we never looked back.
Michelle
He said, “You have multiple myeloma.” I asked, “Is that cancer?” He said yes, explained what it was, and sent me to a hematologist-oncologist in their group, who was not at UCSD then. They got me in that day, and the hematologist-oncologist did a bone marrow biopsy.
When we got home, we started making calls. I called my boys’ pediatrician, who I loved and whose opinion I valued, and we reached out to several other people. They all led us to Dr. Caitlin Costello, so we gave her a call. She fit me in right away, and we never looked back.

Explaining Multiple Myeloma to Patients
Tiffany: Doctors all explain myeloma differently, so Dr. Costello, how do you explain myeloma to your patients?
Dr. Caitlin Costello: For many people, when they hear of and think of cancer, they think of a lump, like breast cancer, or there are symptoms associated with a tumor. But when you’re talking about blood cancers, no tumor can be picked up on routine screening tests, of which there aren’t any for myeloma.
With more “typical cancers,” we’re so used to having public health initiatives for screenings like mammograms and colonoscopies. Multiple myeloma, however, while it’s the third most common blood cancer, doesn’t come anywhere near number-wise in terms of how many patients are affected in the United States each year. For that reason, for better or for worse, I don’t think we have good epidemiologic advances to say that everyone should have a blood test screening looking for this.
There’s ongoing interest in screening wide groups of populations. In Iceland, they’re screening the entire country for all patients over the age of 40 to see if they can figure out how many patients have what looks like the beginnings of multiple myeloma. And if they’re not myeloma at that point, they want to understand if it makes sense to screen patients.
Patients are going to live with this for the rest of their lives, so there’s no greater importance than understanding and knowledge.
Dr. Caitlin Costello
For the most part, that means that most patients are diagnosed with multiple myeloma when they develop a symptom of some sort. Many people have not heard of myeloma. When a doctor says to a patient that they have multiple myeloma, they ask, “What does that mean?”
When I describe multiple myeloma to a patient, I say, “What we have identified is a form of a blood cancer called multiple myeloma based on your blood tests and your bone marrow tests.” A lot of my consultations with patients are to explain that diagnosis because.
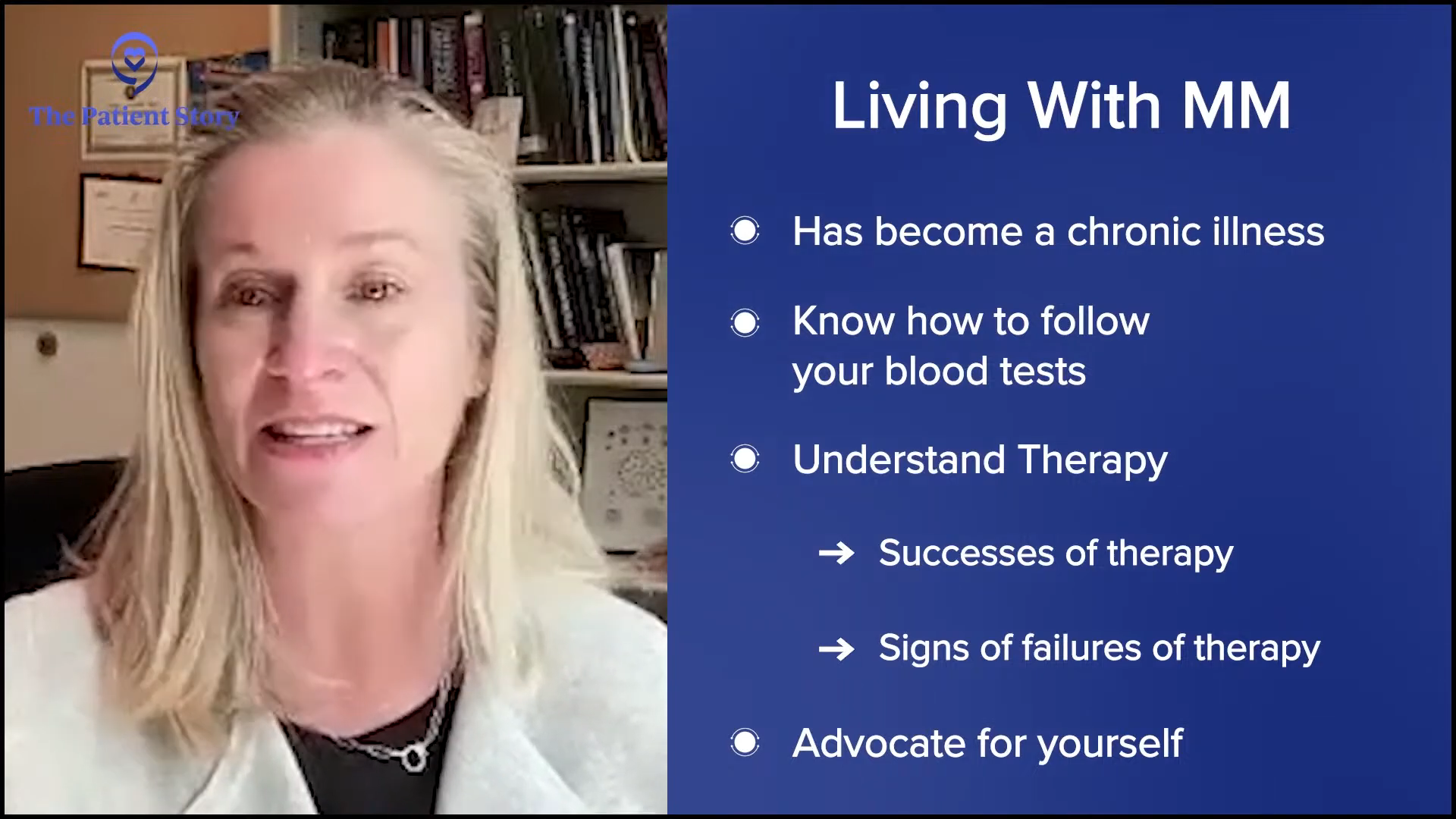
We have a wonderful problem with myeloma. This has turned into a chronic illness. Patients are going to live with this for the rest of their lives, so there’s no greater importance than understanding and knowledge so that patients know what it is that we’re talking about, know how to follow their blood tests, understand the successes of therapy or perhaps early signs of failures of therapy, and advocate for themselves.
There’s so much to say of the educated patient, which doesn’t mean Doctor Google. There are very good patient advocacy groups and platforms like The Patient Story, where patients can get great information to help them understand their disease and their journey with it.

When I explain myeloma, I explain that it’s a form of blood cancer that comes from a plasma cell, which is part of your immune system. The plasma cell is designed to produce the weapons needed to protect our body. The bone marrow is like the armed forces. We have an army, a navy, an air force, and all these different branches with different weapons designed to protect you. One branch went rogue when one plasma cell went rogue and started producing extra bad guy weapons that don’t work well and cannot protect the body and cause damage.
Bones are the most common way that myeloma can affect a person’s body, and therefore, that’s one of the most common ways that patients are eventually diagnosed because they come seeking help for pain. As Michelle experienced, back pain is one of the most common ones. We think the bones in the middle of our body are more often affected than elsewhere. The classic story is someone had back pain, their doctor did X-rays, but they didn’t see anything, or they were referred to physical therapy, but the pain got worse.
Everyone’s allowed to hurt, but pain that doesn’t go away, came on for no good reason, and is persistent needs to be evaluated. Michelle did all the right things because she had what we can say are typical symptoms with pain, some atypical symptoms with the skin and the belly discomfort, but she asked all the right questions to get her to the right people who could help her.

Common Questions After a Multiple Myeloma Diagnosis
Tiffany: I love that you talk about patient education. I believe that part of patient education is learning all the medical terms you probably weren’t familiar with before. How receptive are your patients in terms of wanting to learn all that? What are the top three common questions you get after someone is diagnosed with myeloma?
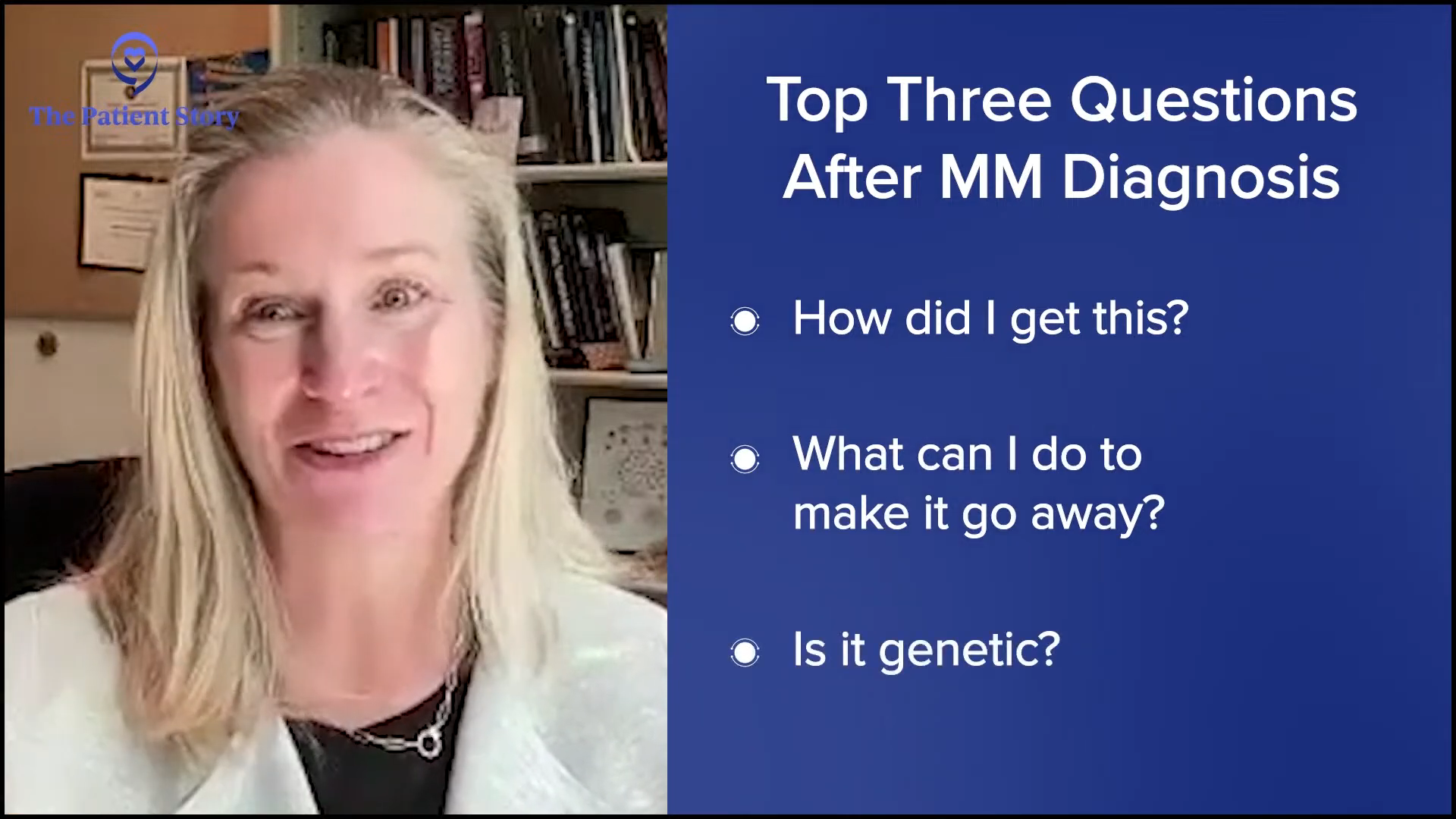
Dr. Costello: The top three questions are: How did I get this? What can I do to make it go away? Is it genetic?
Everyone wants to feel empowered that they can make some lifestyle change, for example, to make things better or help rationalize this to some degree to say X caused Y. It would be fair if there was some culprit, but it’s unfair because there is no culprit. We think this is a random thing that happened for no good reason, by no fault of anybody’s. Nature changed the makeup of your bone marrow and the part of your immune system.
Getting Involved in the Decision-Making Process
Tiffany: Michelle, when you first met with Dr. Costello and as she was explaining your treatment options, how involved were you in the decision-making process? What did that experience look like?
Michelle: Dr. Costello presented me with what the standard of care was for multiple myeloma at the time. I was very receptive. I sought a second opinion and reached out to another multiple myeloma specialist in the vicinity. She confirmed the same thing, so we went with what everyone was recommending.
Factors to Consider in Shared Decision-Making
Tiffany: Dr. Costello, when you approach your patients about their treatment options, what are your thoughts? How do you approach shared decision-making with your patients? What factors do you consider to help them come to that process with you?

Dr. Costello: Every person is different. People process information differently. People hear information differently. Some people want to know more, and some people don’t want to know more.
An important part of any conversation is to level set and say, “What do you want to get out of this conversation? What is it that you want to know?” More often than not, the patient has something in mind, and the family members have something different in mind. It’s important to gauge the group to determine what it is that they’re hoping to get out of the appointment so that I’m not overstepping boundaries.
Once we are able to establish how much will be shared, my job is to give the information. What is the standard of care? What is the typical approach? Once we’ve laid the groundwork, then we can determine treatment recommendations based on the patient and the details of their health, caregiver support, and the biology of their disease. Very specific details can make treatment recommendations slightly nuanced for any individual person.
My job is to help them be as informed as possible so that they can make the best decision for themselves.
Dr. Caitlin Costello
I love that Michelle got a second opinion. I have no ego. When you are diagnosed with something life-changing, you need to feel very confident in what your next approach is going to be. The more people think about you, the better. Like many myeloma specialists, this is what we do day in and day out, but it’s nice to have a fresh set of eyes so nothing’s missed. Yesterday’s information may have been different from a month ago’s research.
The approach is standard, but the shared decision-making is where things may be slightly different. I can make all of my recommendations and say, “This is what’s standard. These are the slight modifications I would make for you.” Sometimes, the patients will take that information and say, “I’ll get back to you.” Some people will say, “Let’s do this. Whatever you say, doc.” Some people will say, “No.”
I’m not in their body. I’m not making decisions for them. My job is to help them be as informed as possible so that they can make the best decision for themselves. I may not agree with their decision, but that’s not my job. My job is to help them arrive at the best decision that’s for them.

Tiffany: You said everything that I wanted to hear personally, especially when it comes to seeking a second opinion. For a lot of patients, especially if they like their physician in the first meeting, they feel like they’re turning their back on their physician. Thank you so much for encouraging patients to seek a second opinion.
Multiple Myeloma Treatment Journey
Tiffany: Michelle, where are you in your treatment journey?
Michelle: I did four months of the initial treatment regimen and went into an autologous stem cell transplant. Unfortunately, it wasn’t successful and the myeloma returned within the 100-day mark. We regrouped, went back on one treatment for the summer, regrouped again, and did a more aggressive approach.
The MRD testing at the beginning of 2024 showed that the myeloma was slightly coming back. It was affecting my quality of life and I was ready for something different, so we regrouped again. The doctors agreed that I could take the summer off. We did a repeat bone marrow biopsy, so I would have some initial data to compare against when I start my new treatment plan.
Tiffany: Did the pandemic affect your treatment at all?
Michelle: It gave me a lot of anxiety, but I had to be persistent. Even when everything closed down initially, we were on the phone asking, “Am I coming in?” She said yes, so I went in. I went in every other week all through the pandemic.
Coordinating Care with Multiple Healthcare Providers
Tiffany: When it comes to cancer, you have more than one healthcare provider. Your healthcare team is very vast. Is that specific to UC San Diego or do you have local providers that you also go to? You’re always receiving a lot of information, so how do you coordinate that among yourself and your medical team?
Michelle: I don’t live in San Diego anymore, so I have a local hematologist-oncologist in Sacramento where I now live. This is my disease and my choice. I’ve always sought second opinions, especially when making big decisions about changing treatment plans and what to do next.
Thankfully, the multiple myeloma world is small, so they all know each other. I’ve always been able to discuss with each physician. Even if I don’t agree with a treatment plan, I can seek a different opinion. They have been very kind and take into account my quality of life and what I would like.
Getting the information is best. I seek opinions, weigh out what I want to do and how the treatment is going to affect my life, especially with raising two active boys, what I can handle as far as raising them and having a great quality of life, and then make my decision of how I want to proceed based on their recommendations.


Managing Patient Care From Afar
Tiffany: Dr. Costello, for someone like Michelle who doesn’t live in your area, how do you approach seeing patients from afar? Is that something that you do? I had a conversation recently about how large academic centers are more specialized and how you share information with local providers who may not have the same knowledge that you would have. How does that work for you?
Dr. Costello: I don’t feel like Michelle gives herself enough credit. From everything that she said, while raising two young children amid a pandemic, I told her to jump, and she said, “How high?” She has such a commitment to her health and her family.
She got her care at UCSD where we have myeloma-dedicated physicians, but most myeloma patients are taken care of in the community. They see an oncologist, who is possibly a general oncologist who’s seeing them right after they see someone with breast cancer and right before they see someone with lung cancer. Often, they’re good with myeloma, but it’s hard to be a jack of all trades also, and that’s where the importance of a myeloma specialist comes in. I don’t know how they do what they do, seeing so many different cancers. I have difficulty keeping track of one, let alone all of them.
The importance of the connection between the community oncologist and the academic myeloma specialists can’t be underlined enough because we have different tools at our disposal.
Dr. Caitiln Costello
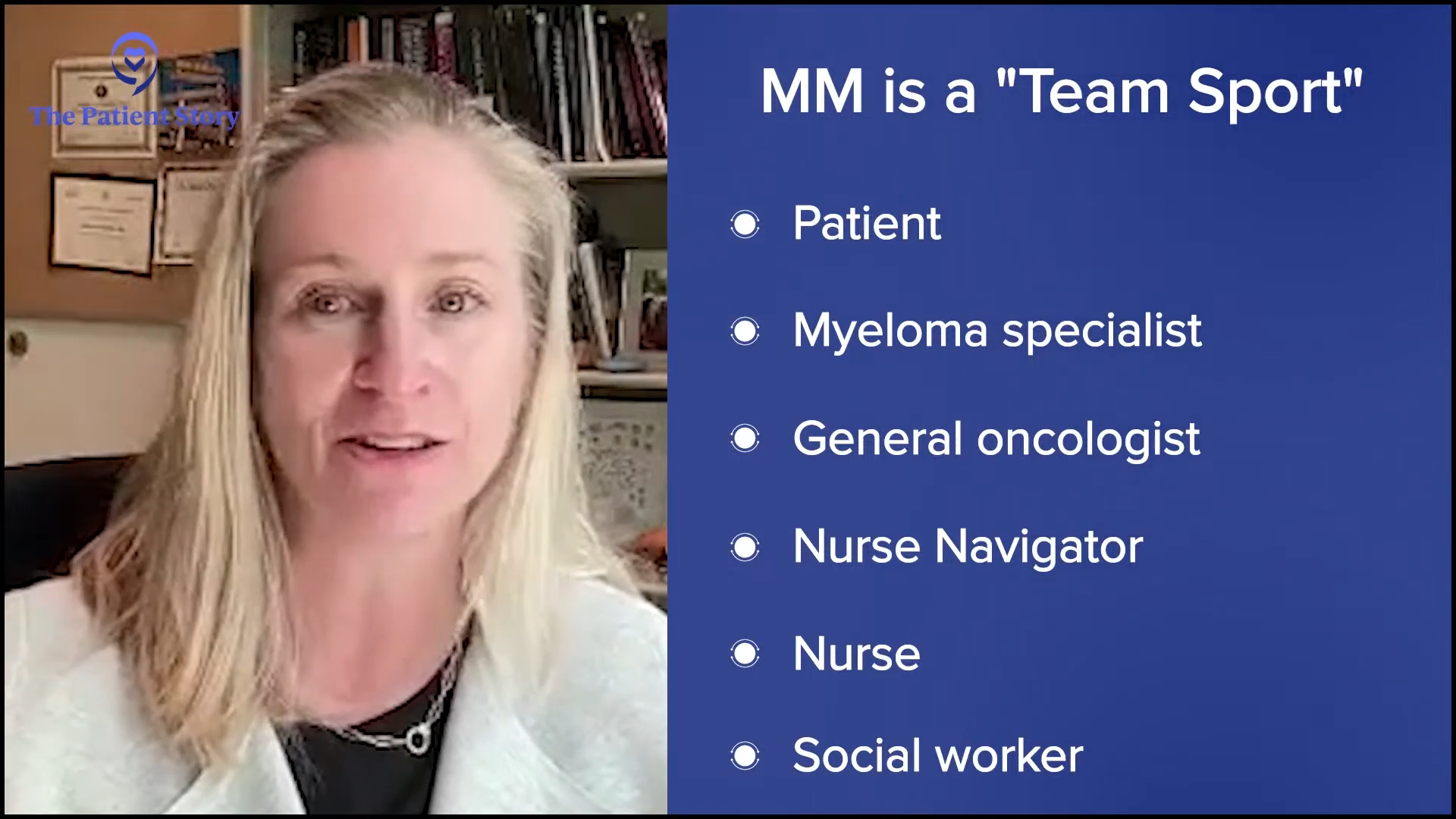
Myeloma is a team sport. Your team includes the patient, myeloma specialist, general oncologist, nurse navigator, nurse, and social worker. There’s a whole team of people who are trying to come together to hold hands with our patients to get them through this whole process.
I can’t speak for other places, but a lot of that can be a little insurance-driven, especially in California. Some insurers will require you to stay with your community oncologist and if that’s the case, the patients get referred for their stem cell transplant, CAR T-cell therapy, or whatever treatment we have to offer at the academic center that perhaps the local oncologist cannot offer. That allows us to maintain that relationship with our patients as well. I have a list of phone numbers of all my local community oncologists down here because we are constantly talking about our patients behind the scenes.

The importance of the connection between the community oncologist and the academic myeloma specialists can’t be underlined enough because we have different tools at our disposal. Myeloma is complicated. There are so many drugs, which is a wonderful problem, but that means that it can be complicated to understand which drug to use and in what order. The connection between the oncologist in the community and the myeloma specialist is absolutely paramount to navigate this whole thing.
I want to be well and healthy to see my boys’ future, and I want to do that with a great quality of life.
Michelle

Importance of Quality of Life in Driving Treatment Decisions
Tiffany: I used to be a caregiver, so I understand the importance of quality of life. Michelle, you were able to take some time off treatment. How important was your quality of life in driving treatment decisions?
Michelle: I want to be around for my children. That’s my top priority and however I’m going to get there, I will get there. I will cross that finish line no matter what it takes. I want to be well and healthy to see my boys’ future, and I want to do that with a great quality of life.
I started not feeling well after treatments. I was dragging myself and making myself nauseous before even getting to treatment. It was psychosomatic. I realized this wasn’t good and I needed to switch things.
I’m very fortunate where I have a lot of flexibility in my time, so I’m able to make doctor’s appointments and do my treatments during the day when my boys are at school. I try to lead my life in a way that doesn’t affect my children. I’m not in the infusion center when they’re home and going to bed, and I’m very blessed to have that opportunity.
Data That Looks at Quality of Life for Multiple Myeloma Patients
Tiffany: Dr. Costello, is there increasing data that looks at quality of life when it comes to myeloma and treatment options?
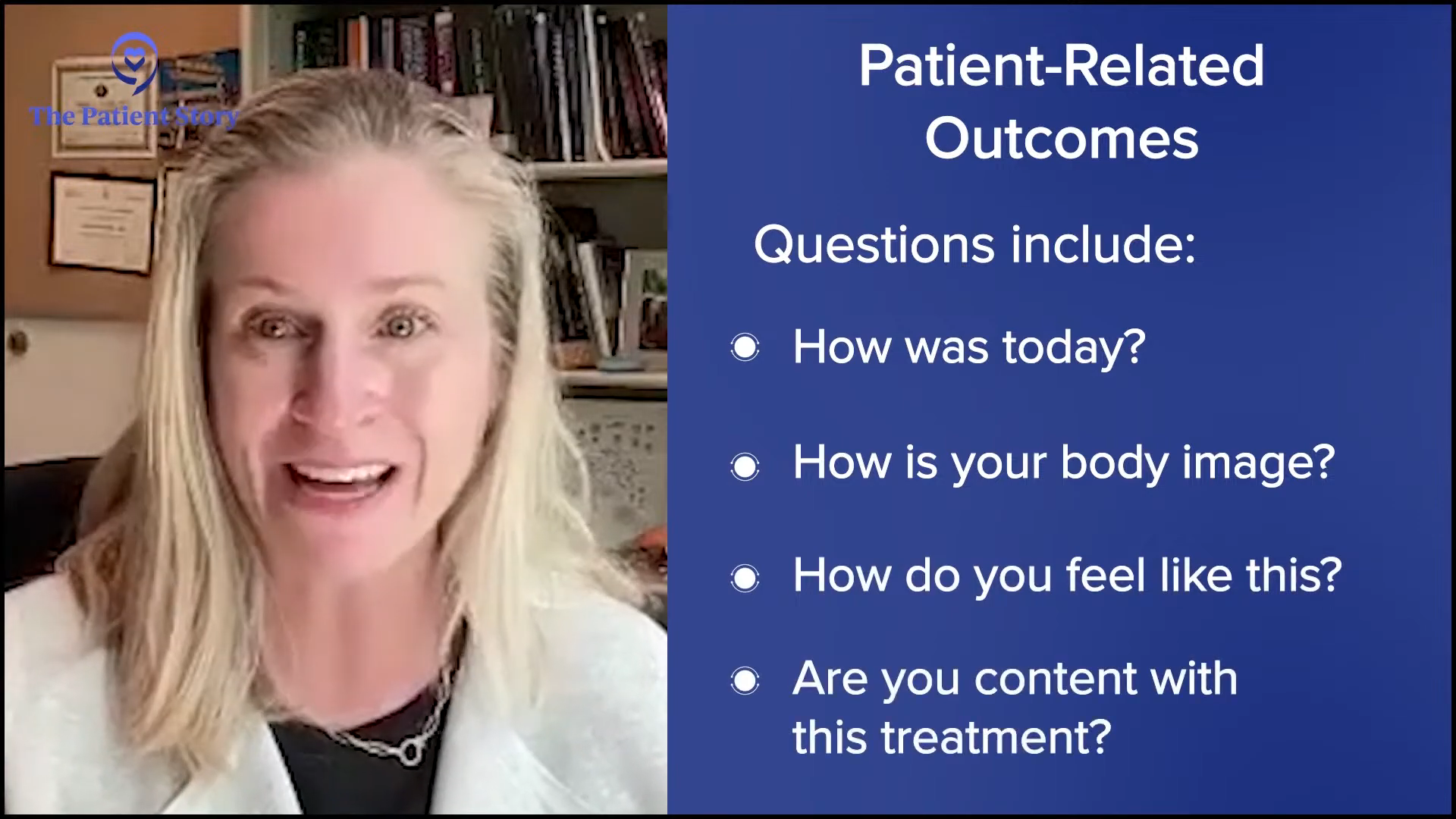
Dr. Costello: I don’t even know how to emphasize quality of life enough. People ask, “Is it quantity of life? Is it quality of life? Is it both?” I ask that to some degree to find out about their goals. People’s goals are different. It’s realistic though to say that some of our treatments are not that great. They’re inconvenient and take up a lot of time even though they work. We need to have a conversation to find out their deal breakers. Some patients don’t want to be in an infusion center and only want to take a pill, even if it means it’s not as effective because that’s what’s meaningful to them.
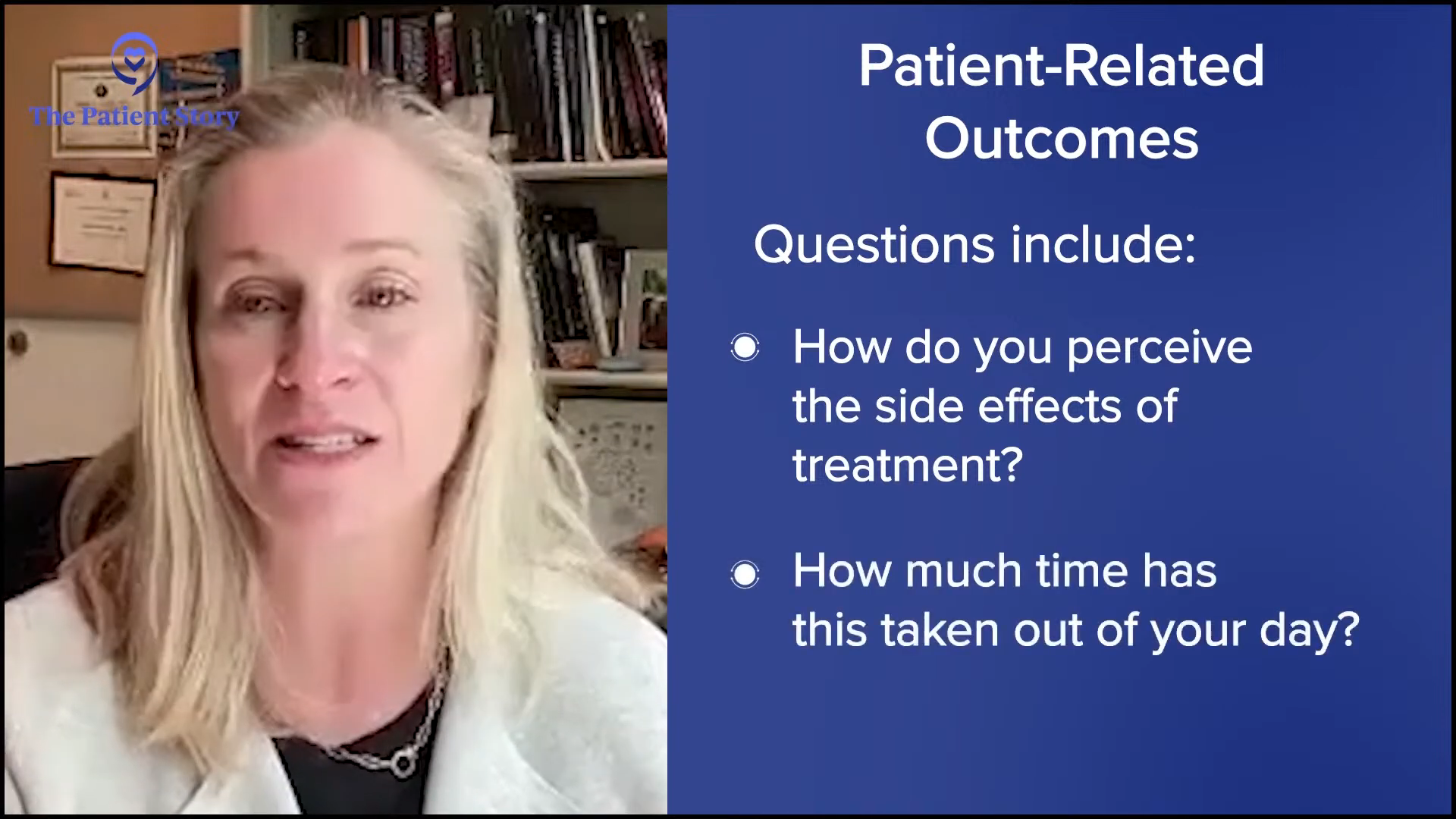
As far as research goes, fortunately, a lot of different studies are looking at new drugs or new drug combinations, including what we call patient-related outcomes. People may hate it because there’s a lot of surveys that happen in the midst of clinical trials asking them, “How’s today? How’s your body image? How do you feel like this? Are you content with this treatment? How do you perceive the side effects of treatment? How much time has this taken out of your day to do this?”
There is more interest in expanding on what we’ve always relied on to evaluate the safety and efficacy of drugs, to incorporate how these drugs can change people’s lives positively and negatively, and to help guide doctors in making treatment decisions and help patients understand if that’s a deal breaker.
Approaching the Clinical Trial Conversation
Tiffany: You brought up clinical trials, which is one of my favorite topics. Oftentimes, I’ll hear patients say they don’t want to go on a clinical trial because they think that’s the last resort. Dr. Costello, how do you approach the clinical trial conversation with your patients?
Dr. Costello: I first dispel the myth that placebos still exist. Some people still have it embedded in their mind. I always say that it isn’t ethical. We don’t do that anymore. Clinical trials are designed to give you what we consider the best available treatment right now and/or compare it to something that we think is as good or potentially better. I tell patients they’re potentially getting the best of both worlds no matter what they get assigned to at clinical trials.
Part of clinical trials is to help patients understand that there are various phases. Some are randomized where we don’t get to say in what treatment the patient will get. They get assigned to one or the other, but both are great options. There’s an earlier phase trial, which evaluates the safety or efficacy of these treatments and every patient will get the exact same treatment.
There are great benefits that can be reaped by participating in trials, which include getting access to cutting-edge therapies.
Dr. Caitlin Costello
There’s a thought that participating in a clinical trial is purely altruism and to some degree, yes. You are helping the future of myeloma therapies, but you’re getting the benefit yourself from it. Clinical trials are not always designed to be testing the next best thing when a patient has no other options. It’s improving all the steps of treatment that currently exist because we can always do better.
When the conversation about clinical trials comes up, a lot of it is dispelling myths and helping people recognize that it’s not just for others. There are great benefits that can be reaped by participating in trials, which include getting access to cutting-edge therapies that I otherwise cannot write a prescription for.
Seek other opinions and make the best informed decision for yourself.
Michelle
Key Takeaways
Tiffany: Michelle, what would you tell a patient who is newly diagnosed? Honestly, it seems like you did everything right, so I want to commend you.
Michelle: You are your best advocate. Do your research. Seek other opinions and make the best informed decision for yourself.
Tiffany: Dr. Costello, how do you help a provider to be an active participant and proponent of informed decision-making and shared decision-making, especially junior providers who are coming into the fold? What advice would you give providers to be the kind of person who has relationships with their patients like you and Michelle have?

Dr. Costello: Thank goodness that the paternalistic approach to medicine is a thing of the past. While there may still be a bit of it out there, there has been such an important message about customer service with medicine. You have to understand that this is a give-and-take relationship to some degree. The patient deserves to hear all the information and it’s the physician’s role to give all that information.
There’s been such an important emphasis on compassion and communication. If the physician can put themselves in the shoes of a 35-year-old newly diagnosed mom walking into a cancer center, we can all step out of our bodies and our egos to understand that there is more that can be improved in terms of developing that relationship and the importance of communication. We need to understand that we have much to offer, but our patients have so much to offer us as well.

Conclusion
Tiffany: Thank you, Michelle and Dr. Costello, for such an engaging and empowering conversation. I learned a lot about both of you personally and professionally. What you’ve had to say is going to resonate with our audience.
Dr. Costello is truly a testament to what makes a great physician partner. Witnessing her and Michelle interact was refreshing since we know the patient-physician conversation isn’t always light-hearted when it comes to cancer care. It is important to be empowered so that you and your caregivers can make informed decisions about your care.
Thanks again to our partner The Leukemia & Lymphoma Society. Check out the links on their website, including their information resource center, which provides free one-on-one support.

Special thanks to The Leukemia & Lymphoma Society for its partnership.
Multiple Myeloma Patient Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...