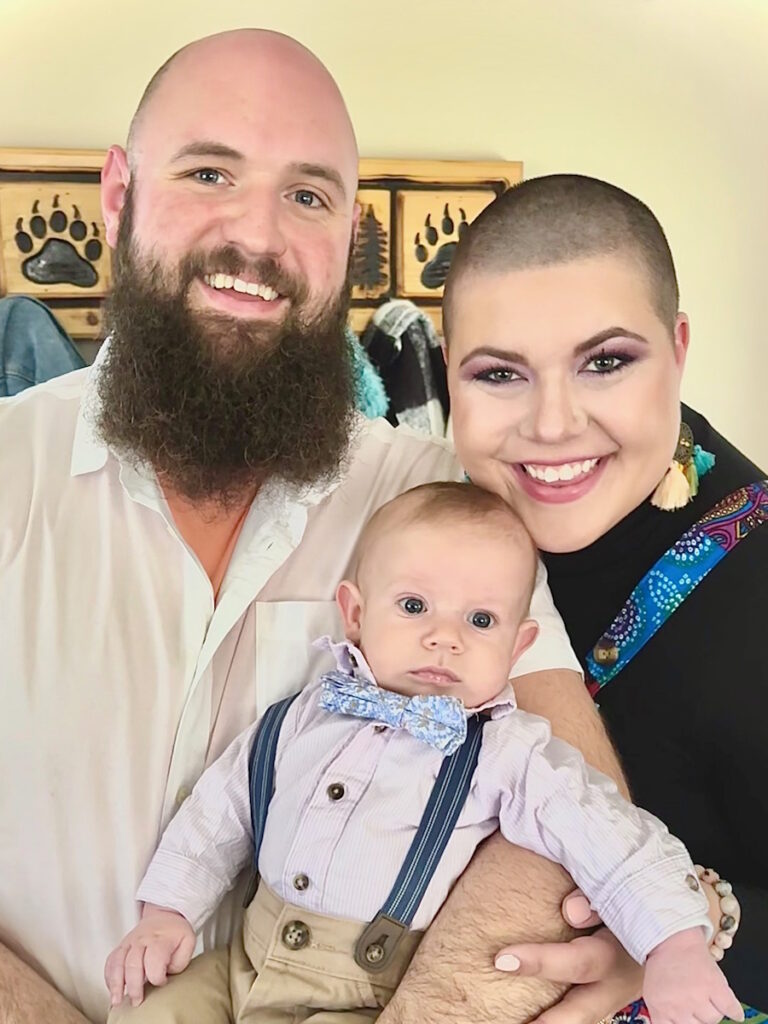
Non-Hodgkin Lymphoma at 29: How Ashley Navigated Motherhood and DLBCL
Ashley’s experience with diffuse large B-cell lymphoma (DLBCL), a type of non-Hodgkin lymphoma, began during a period that should have been filled with new beginnings and joy – the arrival of a new baby into her life. Instead, Ashley, now a mother of three, confronted a growing list of symptoms shortly after her pregnancy when dizziness, cardiac complications, and difficulties breastfeeding all led up to an unexpected, and life-altering cancer diagnosis.
Interviewed by: Keshia Rice
Edited by: Katrina Villareal
Being diagnosed with DLBCL weeks before her 30th birthday set Ashley apart from the typical patient profile, as most individuals face this diagnosis later in life. Her youth contributed to challenges in being heard by her medical team, intensifying her frustration as treatments like chemotherapy caused debilitating side effects. Emotional struggles compounded Ashley’s physical battles: fear of leaving her children, grief over lost moments with her newborn, and the continual responsibilities of motherhood that do not pause for illness.

Despite assurances from leading cancer doctors regarding advances in treatment options, Ashley’s cancer responded poorly to initial therapy, necessitating additional interventions, including CAR T-cell therapy, which required extended separation from her family. The transition from hope to uncertainty was difficult, but new developments with bispecific antibodies and ongoing research provide Ashley and other patients reasons to hold onto hope for recovery and better outcomes even amid refractory disease.
Ashley’s experience is marked by transformation, not just physically but emotionally and spiritually. She learned to lean on her family and faith for support, grappled with feelings of guilt and anger, and emerged with the conviction to advocate for herself and encourage others to trust their intuition. Her story is a testament to the unseen emotional dialogue cancer patients navigate, and to the importance of self-advocacy, community, and accessible innovations in cancer care.
Key Story Takeaways:
- Trust and advocate for your own body; patients know their symptoms best and should persist until they are heard.
- Emotional struggles, like fear, guilt, and anger, are often invisible but just as challenging as the physical aspects of disease.
- Family support and faith provided critical anchors for Ashley, helping her endure even the most difficult days.
- DLBCL can affect patients of any age, and younger individuals may face unique challenges in being taken seriously by the medical team.
- New therapies, including CAR T-cell therapy and bispecific antibodies, offer hope even in refractory cases.
- Advocacy and self-acceptance are vital; patients experiencing life-altering conditions deserve compassionate care and respect for their experience.
- Name: Ashley P.
- Age at Diagnosis:
- 29
- Diagnosis:
- Diffuse Large B-Cell Lymphoma (DLBCL)
- Staging:
- Stage 4
- Symptoms:
- Feeling like holding breath when bending down or picking up objects from the floor
- Waking abruptly at night, feeling “off”
- One episode of fainting (syncope)
- Presence of a large mass in the breast
- Treatments:
- Chemotherapy
- Bridge therapy of chemotherapy and radiation
- CAR T-cell therapy
Thank you to Genmab and AbbVie for their support of our independent patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Facing the Unexpected: Early Signs and Diagnosis
- A Young Mother and a Rare Diagnosis
- The Unseen Struggle: Emotions Behind the Experience
- CAR T-cell Therapy and Next Steps
- Advocacy and Self-Empowerment: Lessons Learned
- Advice for Others: Faith, Family, and Resilience
- Moving Forward: Transformation and Community
I didn’t realize how big the lump was. It was literally the size of a baseball. But it didn’t raise any red flags.
Ashley P., Stage 4 DLBCL Patient
Facing the Unexpected: Early Signs and Diagnosis
Ashley P.: I’m not afraid to die by any means. I would say I fear leaving my children and leaving them without a mom.
What should have been one of the happiest times in her life became filled with worry when Ashley was diagnosed with a cancer she hadn’t heard of before: non-Hodgkin lymphoma, specifically diffuse large B-cell lymphoma or DLBCL.
Ashley: I started having symptoms while I was pregnant. I had our baby in December 2023 and at the end of my pregnancy, I was having a lot of complications with my heart rate. In February 2024, I started to feel super lightheaded, as if I was hanging upside down for a very long time. It reached a point where I was getting concerned about being alone with the baby. I felt like I was going to pass out. What if I’m holding him and something happens?


Dizziness wasn’t her only concern. Ashley also started to have trouble breastfeeding. A trip to see her midwife helped lead to the diagnosis.
Ashley: I went to nurse him one day and I couldn’t extend my nipple. It was completely caved in. I tried everything to get it unclogged, like hot showers and massages, but they didn’t work, so I reached out to my midwife.
I didn’t realize how big the lump was. It was literally the size of a baseball. But it didn’t raise any red flags. When I saw my midwife, she looked at it and said, “Ashley, this is very, very large. You need to go to the breast cancer center,” which was wild to me.
I went in and they did biopsies on both breasts and the lymph nodes in my armpits, and that’s how I found out.
We have more FDA-approved medicines for lymphoma than for any other cancer… It’s awesome because it means we have more options for patients
Dr. Joshua Brody, Hematologist-Oncologist
A Young Mother and a Rare Diagnosis
The average age for a DLBCL diagnosis is in the mid- to late-60s. Ashley says being diagnosed at a much younger age made the treatment process even more frustrating.
Ashley: I found out I had cancer literally two weeks before my 30th birthday. They said that I was so young and that everybody they usually see with this cancer is in their late 70s. They told me that it was going to be an absolute breeze.
I had a very hard time being heard because I was so young. Chemotherapy rocked my world. I was extremely sick. I barely had time to recover between rounds. I kept telling my oncologist that I was so sick and miserable, and the response that I kept getting was, “You’re young. You shouldn’t be.”
DLBCL can be a devastating diagnosis. But top cancer doctors, Dr. Amir Steinberg from Westchester Medical Center and Dr. Joshua Brody from Mount Sinai, want people to know that there’s a lot of hope. Watch their discussion.

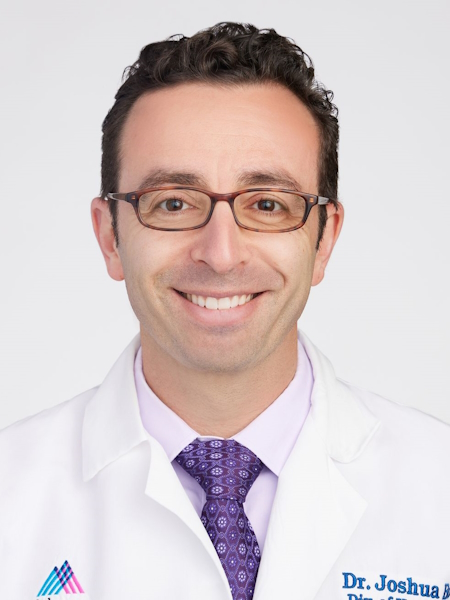
Dr. Joshua Brody: We’re very lucky because, even though lymphoma is technically the fifth most common cancer in America, we have more FDA-approved medicines for lymphoma than for any other cancer, even more than for breast cancer, which is so incredibly common. It’s awesome because it means we have more options for patients
Dr. Amir Steinberg: There’s so much that’s changed in the last 20 to 30 years, most especially in the last five years. Things are changing for the better so rapidly for patients. As doctors, we have so much to catch up on and stay up on in terms of the knowledge out there, but it’s totally worth it because it will make patients’ lives better and more fulfilling.
Despite assurances from doctors, treatment was daunting.
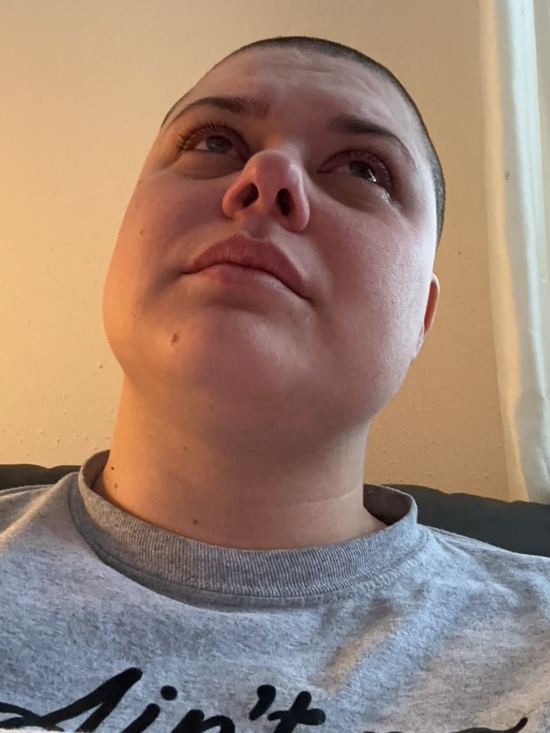
Ashley: I don’t think people understand that you can see all the physical changes. You can see the hair loss, the bloating, the puking, and even the literal color draining from their face. But you cannot see their inner dialogue. You can’t see them fighting for their lives. You can’t see the anger or the conversations with God about why. Questions of, “Did I do something wrong to deserve this?”
The world doesn’t stop… You still have to show up and be a mom and a wife… and that is such a hard challenge.
Ashley P., Stage 4 DLBCL Patient
The Unseen Struggle: Emotions Behind the Experience
As a mom of three, Ashley dealt with mixed emotions of guilt, stress, and sadness over the experiences she lost.
Ashley: I honestly think I got robbed of the joy. He’s my last baby and I had this huge goal of nursing. It was easy with him. I had all these plans, but I was in so much pain from my cancer.
Then I have a nine-year-old and an almost five-year-old, so it was difficult juggling that and trying to figure out the best way to tell them what I was going through. That was probably the roughest part.

The world doesn’t stop and that thought came into my head so many times while I had cancer. You still have to show up and be a mom and a wife. You still have to be all of these things while battling the biggest physical challenge that you’ll ever go through and the biggest emotional and mental struggle that you’ll ever have to battle. You still have to show up for everybody around you and that is such a hard challenge.
One of the hardest emotions Ashley had to deal with was anger.
Ashley: I knew that I was mad and not the best version of myself. Then you have this feeling of complete guilt. What if you die and this is who you showed up as and who you left as? This is how you treated your fiancé and your kids? Don’t you value life? Didn’t you say that you wanted to show up differently? Didn’t you say that you were going to be a completely different person because now you know the value of life and how it can be taken away? Now, you have this complete guilt trip of who you’re showing up as. But at the same time, you’re so mad. You’re so mad.
I thought, ‘What if I go through all of this and then I still have cancer?’ That was something that I didn’t want to face.
Ashley P., Stage 4 DLBCL Patient
During those moments, Ashley leaned into her family and her faith.
Ashley: I’ve seen other people talk about it, but there is a sense of peace and knowing that I have not experienced in my life. Definitely not the peace that carried me through. I had to be here for my kids. There were so many times when I thought that if I were doing this for myself, I wouldn’t have gone through it. It was too much. It was so hard that I truly don’t know if I would have shown up in the same capacity.


CAR T-cell Therapy and Next Steps
After six rounds of chemo, Ashley thought the hardest part was over. But her DLBCL was refractory, meaning it did not respond well to initial treatment.
Ashley: When I did my chemo, they didn’t even talk to me about the steps and what they would do. Again, age was a huge factor. We did have conversations about other things out there. It went from a 70% chance of beating this and the odds are good of going to Mayo, to my odds going down to 10%. The biggest concern was waiting for the CAR T-cell therapy. But after, they told me, “This is your last option. If this doesn’t work, there isn’t anything more out there for you to do.”
CAR T-cell therapy came with new challenges.
Ashley: When you go through CAR T-cell therapy, you have to be gone and by the hospital for 47 days, away from your family. I thought, “What if I go through all of this and then I still have cancer?” That was something that I didn’t want to face. I didn’t even want to have that be a possibility. I just wanted to be done.
Whenever possible, we try to offer trials because that’s how we advance the science and get higher cure rates. They’re essential.
Dr. Amir Steinberg, Hematologist-Oncologist
Ashley’s experience reflects the complexity of DLBCL treatment. It’s one of the reasons why doctors are constantly looking to new research in clinical trials for answers. One of the answers is a newer option in immunotherapy called bispecific antibodies.
Dr. Brody: Even for people who relapse in the first year or in their third line, there is great evidence for bispecific antibody plus chemotherapy. Overall, it certainly seems to be a bit safer than transplant, maybe even safer than CAR T-cell therapy, and it’s a lot more accessible to folks who are being treated in the community when they don’t have a CAR T-cell therapy center nearby. If you’re getting more options, then that can only be a good thing. People would rather have a clear answer. But they would rather have better therapies and better options.
Dr. Steinberg: Whenever possible, we try to offer trials because that’s how we advance the science and get higher cure rates. They’re essential.


Advocacy and Self-Empowerment: Lessons Learned
While Ashley eventually found a great and supportive medical team, she wishes she had advocated for herself more from the beginning.
Ashley: That is one thing I regret and one thing I always tell somebody. You have to advocate for yourself. I’m not that person. I’m very shy. I don’t want to make people upset. I want to make everybody happy. I struggled very much with advocating for myself.
Advocate for yourself. If something doesn’t feel right, if you know something’s wrong, or if you feel sick or in pain, talk about it until you’re blue in the face and somebody listens to you.
Ashley P., Stage 4 DLBCL Patient
Advice for Others: Faith, Family, and Resilience
Ashley’s advice to others? Advocate for yourself, lean into your faith, and learn to accept the changes.
Ashley: Be honest with how you feel. Have those hard conversations. Lean into God as much as you possibly can because at times, that’s literally all you have. You would be very surprised at what you’re willing to go through and what you’re willing to overcome for the people that you love. It’s almost like an adrenaline rush to make it through.
Advocate for yourself. If something doesn’t feel right, if you know something’s wrong, or if you feel sick or in pain, talk about it until you’re blue in the face and somebody listens to you. You know your own body. You have that intuition for a reason and you know when something is wrong.
Moving Forward: Transformation and Community
Ashley: You make it. You make it out alive. You will never be this version of yourself again and that is completely okay. Sometimes we have to go through something completely terrifying and life-changing to figure out who we want to show up as and what’s important to us. It’s going to suck so badly. But you find out who your people are. So many people love you. And you make it.


Inspired by Ashley's story?
Share your story, too!
Thank you to Genmab and AbbVie for their support of our independent patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
More DLBCL Patient Stories
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy


