Michael’s Relapsed Diffuse Large B-Cell Lymphoma (DLBCL) Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal
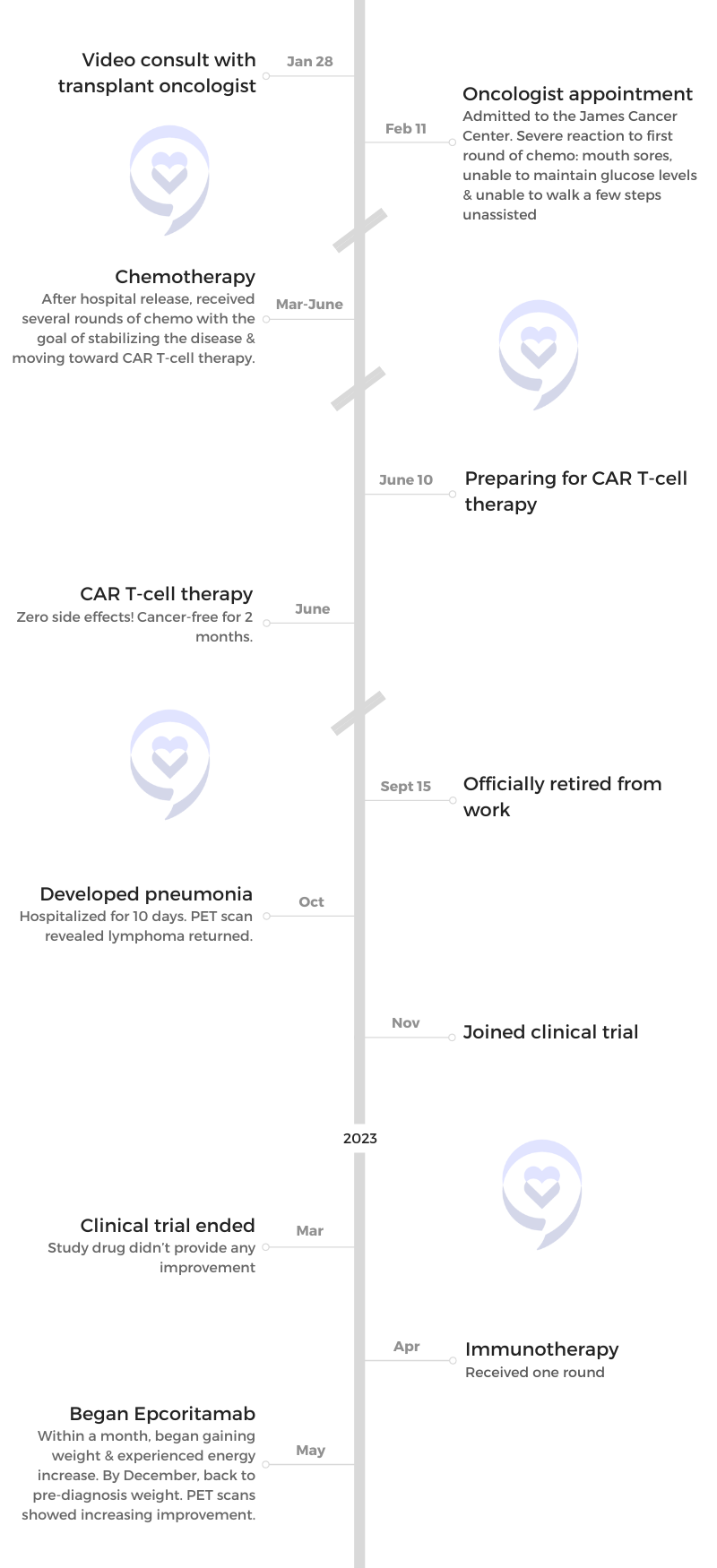
Michael recounts his journey with diffuse large B-cell lymphoma (DLBCL) alongside his wife and care partner, Kimberly. He was initially diagnosed in 2016 but after experiencing pain in his lower back and leg coupled with severe itching, it led to a diagnosis of a relapse.
After undergoing chemotherapy, he faced severe side effects including weight loss, itching, and pneumonia. He then underwent CAR T-cell therapy, experiencing a brief remission. Michael tried a drug through a clinical trial but saw limited success. Eventually, he turned to epcoritamab, which has brought about significant improvement without notable side effects and improved his quality of life.
Michael emphasizes the importance of advocacy, seeking multiple opinions, and maintaining hope throughout the challenging journey. His wife Kimberly stresses the crucial role of care partners in managing and supporting treatment and well-being. She emphasizes the significance of self-care for caregivers and persistence in seeking answers and treatment options.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
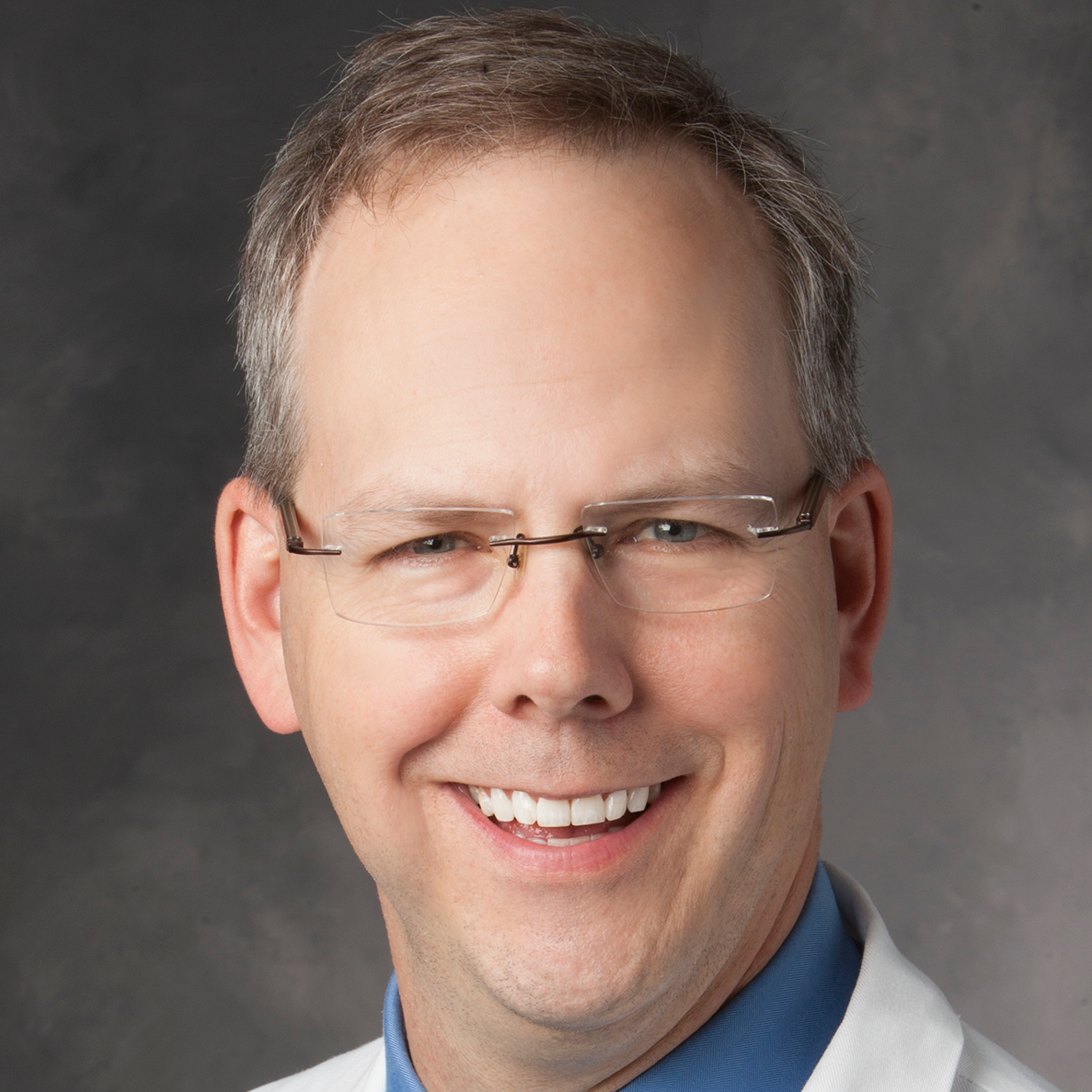
- Name: Michael E.
- Diagnosis:
- Relapsed Diffuse Large B-cell Lymphoma (DLBCL)
- Initial Symptoms:
- Back & leg pain
- Rash
- Severe itching
- Decreased appetite
- Weight loss
- Treatment:
- Chemotherapy
- CAR T-cell therapy
- Clinical trial (no improvement from study drug)
- Immunotherapy: epcoritamab

I was having lower back pain and an incredible amount of pain down the front of my right leg.
Michael
We knew two issues were going on, but we had no idea that they were pointing to the same thing.
Kimberly
Introduction
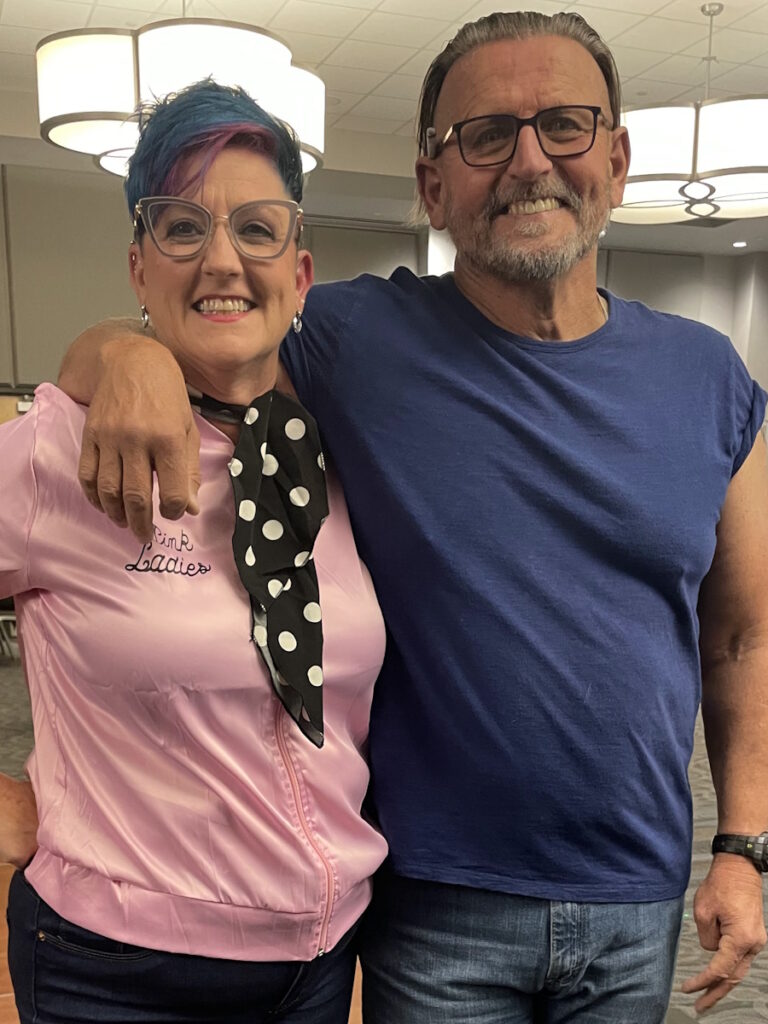
Michael: I was born and raised in Ravenna, Ohio. My wife Kimberly and I have six daughters and 10 grandchildren.
Kimberly: I didn’t know I would be a care partner when we got married, but it was a role I took on. I did it willingly, but it was a rough road.


Pre-diagnosis
Initial Symptoms
Michael: I was having lower back pain and an incredible amount of pain down the front of my right leg. I thought it was a pinched nerve or I’d done something wrong while working out.
Kimberly: We thought it was back trouble. That was coupled with severe rashes and itching. At that time, the two didn’t seem related. We knew two issues were going on, but we had no idea that they were pointing to the same thing.
Testing
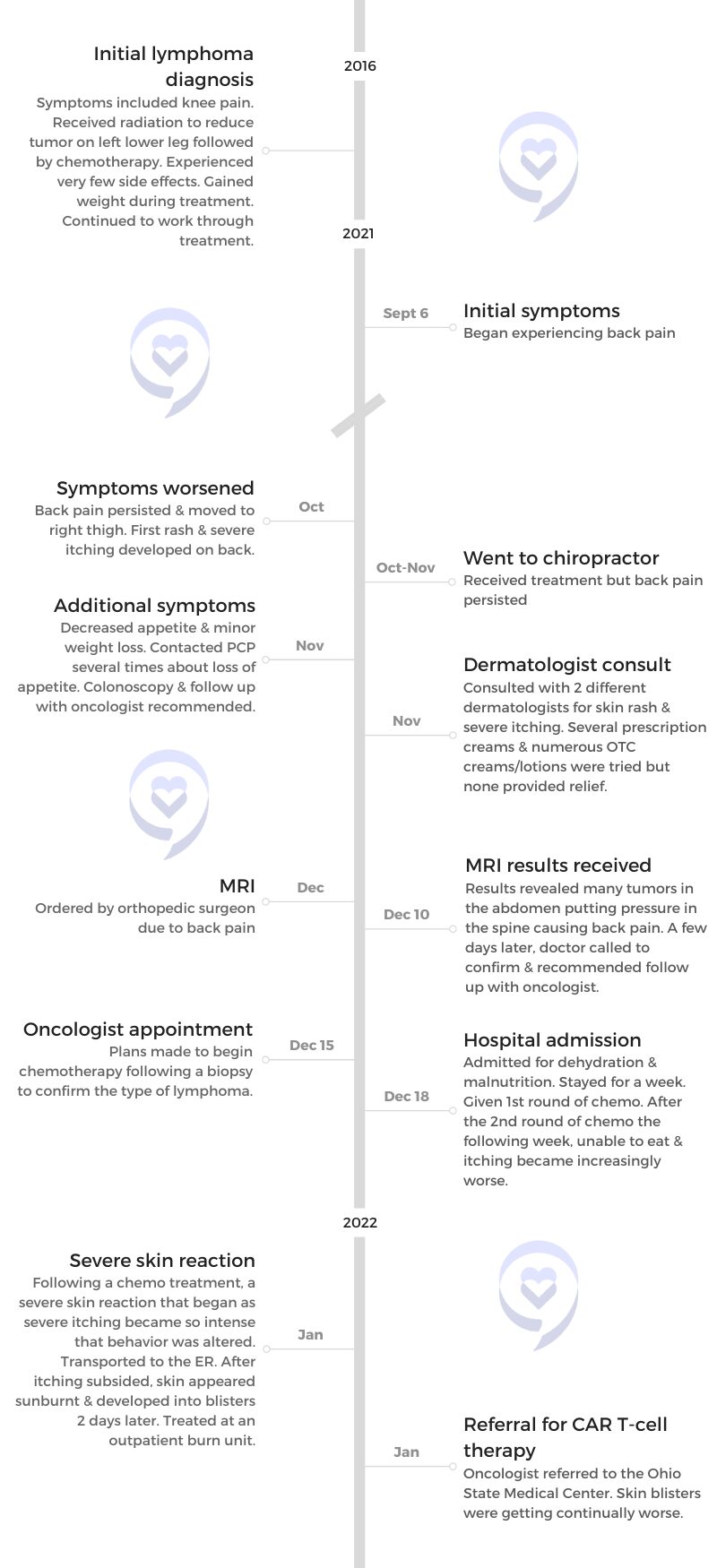
Kimberly: The back and leg pain started around Labor Day and the rash started in October. By November, we noticed weight loss.
The Friday after Thanksgiving, he consulted with an orthopedic surgeon since we presumed it was back trouble and the surgeon ordered an MRI.
Michael: My wife pushed, so we got in sooner than scheduled.

They began treatment with the inclination that it probably was going to be diffuse large B-cell lymphoma.
Kimberly

Diagnosis
Kimberly: Based on Michael’s previous history, the doctor said, “We’re seeing enlarged lymph nodes. You have a lot of tumors pressing on your spine and that’s why you have this pain. We’re pretty sure your cancer is back.”
After the MRI, we saw the oncologist he had previously worked with.
Michael: I was diagnosed with DLBCL in 2016.
Kimberly: They ordered a biopsy, but because it was so severe, they began treatment with the inclination that it probably was going to be diffuse large B-cell lymphoma. They didn’t want to hold off on treatment. He had two rounds of chemo when the results of the biopsy came back and confirmed that it was DLBCL.
Michael: We didn’t find out what was going on until we went to Columbus. I will always be grateful to the oncologist in Akron because he had the wherewithal to say, “This is beyond me and I don’t know what to do with this.” He put us in contact with the hospital in Columbus and we met Dr. Voorhees, who took the ball and started running with it.
Kimberly: He was malnourished and dehydrated because of severe weight loss. The majority of the weight loss happened within three weeks.


Reaction to the Diagnosis
Michael: We were not expecting to hear that. When you hear something like that, it sets you back on your heels.
It’s scary because you don’t know what’s going on. Most people who get a cancer diagnosis start by looking for answers and don’t expect it to be serious. Most people think, I’ll get this taken care of and then we’ll move on the next day. Our next day turned into a 2 ½-year journey.
Kimberly: In the beginning, you don’t process because you’re on autopilot and doing everything you can for your loved one, like getting them to treatments and making sure they’re comfortable. Oftentimes, the reality of what’s happening doesn’t sink in.
An example is when we spent Christmas Day in the hospital. That was his initial stay from being dehydrated and malnourished and when he received his first round of chemo. I cooked him a quasi-Christmas dinner in the visitors’ lounge of the hospital.
Looking back at pictures of him, he was on the edge, but because I was so in the moment and going through everything a day at a time, I didn’t realize it then. A lot of the processing didn’t happen until later on.
One of the side effects I had was some of the worst itching of my life.
Michael
Treatment
Chemotherapy
Michael: We started with chemotherapy. I received a high amount of chemotherapy and I about died twice from it. Looking back, it was necessary to save my life.
I wasn’t in very good shape at all. I started at around 240 lbs. By the time we got to Columbus, I was down to 150 lbs. Being in that state physically is not a good place to start.


Side Effects of Chemotherapy
Michael: One of the side effects I had was some of the worst itching of my life to the point where it was causing me to have a different outlook on things. It was horrible. I’ve never experienced anything like that in my life.
Kimberly: When they started a second round, the reactions got worse. That’s when his skin started to blister and he was treated as a burn patient.
At that point, his doctor said, “This is way more than I can handle. I want you to go to the James Cancer Center.”
Michael: They had to come up with other treatment options. Thankfully, they got us through. It was like going through stages. Everything we went through got us to the next step. Then from there, we’d go to the next step. It went on down the line like that for a while. They kept me alive and kept me moving.
CAR T-cell Therapy
Michael: Our main goal was to get to CAR T-cell therapy, but we had to choose interim treatments in order to keep the cancer at bay long enough.
I asked Dr. Voorhees, “What do I have to do to be eligible for CAR T-cell therapy?” He said, “You have to be able to walk into my office.” Ten days later, by the grace of God, I was able to walk into his office. I went from being flat on my back to walking into his office.
I didn’t know anything about CAR T-cell therapy. We learned quickly, especially my wife. She’s a detail-oriented person and because of who she is, we learned quite a bit about how CAR T-cell therapy works. She has a curious mind and doesn’t accept not knowing things whereas I’m more of a big-picture guy. Tell me where we’re going and I’ll be there to do my part.

At the 100-day mark, I had a PET scan and they told us that my cancer had returned.
Michael

Post-CAR T-cell Therapy Monitoring
Michael: At that time, we thought CAR T-cell therapy was our cure-all. We believed that. But it turned out to be another step to get us to where we needed to be.
Relapse
Michael: At the 100-day mark, I had a PET scan and they told us that my cancer had returned. I didn’t feel any symptoms. My energy level was starting to increase. My weight was starting to come back. I was feeling good.
Reaction to the Relapse
Michael: When I receive information like that, I go quiet. I’m an internal processor and I think things through before I comment. I felt angry and frustrated. That was a bad day.
We believed that CAR T-cell therapy was a cure-all. We didn’t know that it only had a 47% success rate. Nobody told us. I don’t know if it was an oversight or nobody thought about it, but to be honest, there was some bitterness on my part because no one told us. But there comes a point where you have to accept things, move forward, and start looking at other options.
The next time we met with Dr. Voorhees, the first thing I asked him was, “Why didn’t somebody tell us that the success rate was less than 50%?” He said, “I don’t know why that didn’t happen.” He didn’t dodge the question. He was very honest with us about it. You don’t want to hear bad news, but you need to hear everything so that you can make good decisions.
I never allowed myself to think that there would be anything negative coming from that. We did everything that’s been asked of us. We trusted it and believed it would work. For 100 days, it was great.


Joining a Clinical Trial
Immunotherapy
Kimberly: We’re thankful that in today’s world, multiple options are available. His oncologist, who we started working with prior to and after CAR T-cell therapy, is always great at providing options. He felt that our best chance for controlling the lymphoma and giving Michael a quality of life would be to go on a trial.
There was a trial that he was aware of, which had some results, and he thought that would be best. We’re very adventurous and very aggressive, so we said, “All right, let’s do the trial.”
He was trying to keep my cancer under control until we could get to the point where we could find something that would work well.
Michael
Michael: I took eight pills a day and had to be monitored. Thankfully, I didn’t have any side effects.
Kimberly: Every day, I’d say, “Oh, you look a little better,” or, “Oh, you gained a little weight.” After several months, it was obvious that it wasn’t having an effect.
Michael: A PET scan showed that the disease progression slowed down but not to the degree that they had hoped. He was trying to keep my cancer under control until we could get to the point where we could find something that would work well. He said, “We’re going to try to move on to some other things because that wasn’t working.”
Kimberly: The good news is that it wasn’t necessarily worse, but there was no change, and there definitely still was active disease so we had to do something else.


Bispecific Antibody
Kimberly: Dr. Voorhees presented us with three options, but he felt that two of them were not viable.
His number one option—and the one I wanted Michael to pick—was another round of chemo because that’s a sure thing. We knew that it would control the lymphoma but not sure how it would play out.
A second option was to have a round of immunotherapy, which he responded to before but wasn’t a sure thing. Michael chose immunotherapy because he said, “Why would I want to be alive if I can’t have a quality of life and actually live?”
That was hard for me as a care partner because I wanted the sure thing. We knew that chemotherapy would knock out the lymphoma and keep it under control, but as a care partner, I also had to respect his wishes.
Michael: I love Dr. Voorhees dearly. He’s a good man. He makes you part of the process. If you start getting off the path a little bit, he’ll gently steer you back on, which I’ve always been grateful for and appreciated.
Kimberly: Based on Michael’s previous response to CAR T-cell therapy and the information from ongoing trials, epcoritamab seemed like it would be our best hope. Dr. Voorhees was confident that we would see at least some response.
Michael: He laid out the options. It was my choice. The choice I made was something that I thought would work best for me because of how my body handled CAR T-cell therapy. Bispecific antibodies were very similar so we went in that direction.
Kimberly: I read about the trial on epcoritamab and I felt that everyone who participated was identical to Michael. They had been through very similar things and that was very encouraging at that point.
We had to apply for compassionate use from the FDA because it was still waiting for approval. Michael had to have some additional treatment.

I thank God every day for the people who came up with the medication that saved my life.
Michael
Michael: I’m on epcoritamab (EPKINLY). One of my greatest hopes and prayers is that people have the opportunity to continue on to tomorrow, to enjoy life, and to enjoy their families.
Right now, I take epcoritamab once a month. I started with one a week and that went on for a while, then it went down to one every two weeks, and then we got to the point where I’m at now. The process takes 30 minutes. I used to take a couple of pills before I received the injection, but I don’t have to do that anymore. I go there, they give me my injection, then I go home.
From where we live, it takes between 2 ¼ to 2 ½ hours each way to drive to Columbus for a five-minute injection. It’s a very small price to pay for the results that we’re getting. Compared to everything else that we’ve been through, that is a very easy solution.
I thank God every day for the people who came up with the medication that saved my life. It was a very long ordeal for us and, thankfully, because of a lot of very intelligent people, epcoritamab was developed, is working for us, and makes a big difference.
Response to Epcoritamab
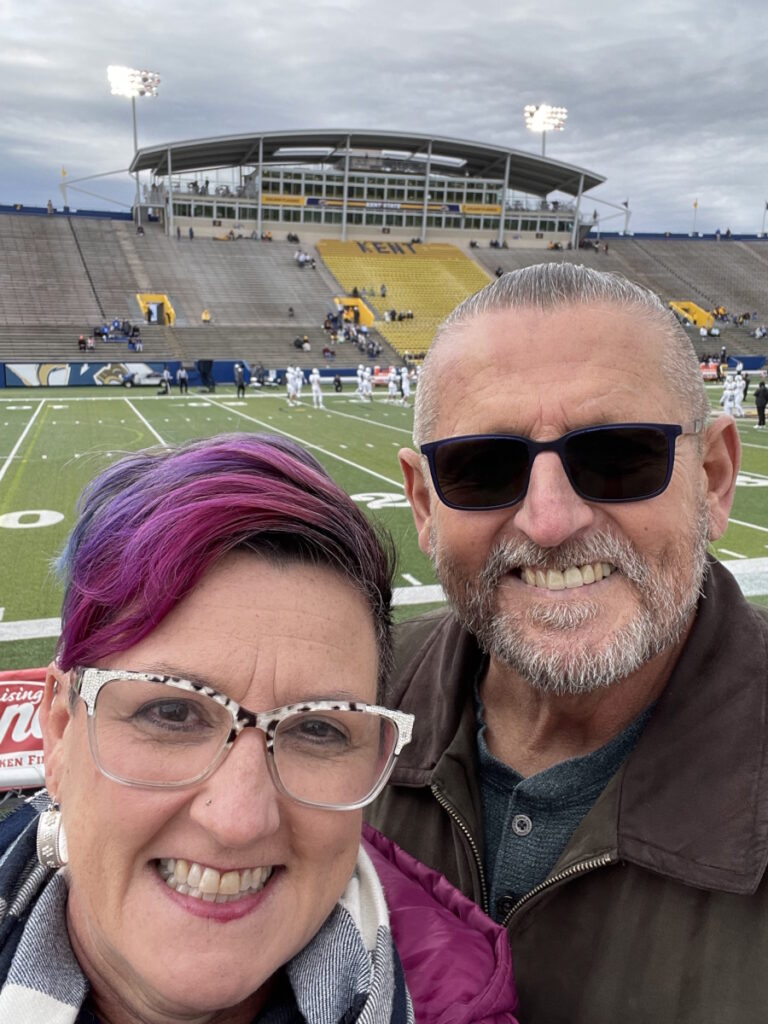
Michael: Within a month of receiving epcoritamab, my weight started coming back. My strength returned and I was able to do things that I hadn’t been able to do in quite a while. I’m back to 238 lbs and getting to do things that I never used to do.
I’m back to working out a lot, which I enjoy. My wife and I ride bikes, kayak, and play with the grandkids. We love to ride roller coasters and we like to travel. We live life and that’s something that was taken from us.
A lot of things were stripped from me when we went through cancer. I like to have the right to make my own choices and that was very hard for me to accept. To this day, when I think back on what happened, it doesn’t sit well with me. You have to learn to deal with it and get to the point where you find the goodness in things.


Kimberly: The immunotherapy did its job. It was almost as if I could see him transforming weekly. His energy level was up. He was able to resume his activities.
The day that I knew that we had hit a turning point was when he worked for about 10 hours in our yard. He loves landscaping. He’s an arborist by trade. He came inside and said, “I’m exhausted.” The red flags went up and I said, “Oh, no, here we go.” And he said, “No, I’m not cancer fatigued. I’m exhausted from working hard in our yard.” That was the moment I knew that we had turned a corner.
Side Effects of Epcoritamab
Michael: There were supposed to be some side effects, but I didn’t have any. It operates in a similar way as some of the medications that worked well for me, so I thought, If that worked really well, we’ll go ahead and have a go at this. It was a medication that my body accepted and that worked well. I have been at full tilt ever since. It’s a true blessing for us.
Don’t be afraid to ask all the questions that you want to ask. Make sure that you’re getting the information that you need.
Michael
Words of Advice
Michael: Part of the reason why my wife and I are doing what we’re doing is to help. We don’t want anybody to go through what we did. If there’s anything that we can do to help somebody look in another direction, hang on one more day, or give them a little hope that there is a better tomorrow out there, then that’s what we’re doing. We want to help and this is one of the ways that we’re doing it.
Don’t wait. Go see a doctor. If the physician that you are seeing now is not the right one for you, don’t be afraid to switch. At the end of the day, it wasn’t just about me. It was about my family and continuing on to be with them.
When you get to a hurdle that you need to cross, be your own advocate. Be involved in your own care. Find a doctor who will talk to you, not at you. Find a physician who will work with you.


The oncologist that we were seeing in Akron said that this was beyond him and what he was accustomed to dealing with. Once he got the PET scans, the test results, and the first attempt at chemotherapy, he said this was beyond him. I admire him for that because he could have said, “We can try this, this, or this,” but he cared enough about us to say, “This is beyond me.” I have always appreciated that about him.
I’ve always been grateful that he had the courage to say that he wasn’t the person who could do this for me. He could have been prideful and said, “I can handle this,” but he didn’t. He had my best interest at heart. We got pointed in the direction we needed to go, so I’ll always be grateful to him.
Before going to the James in Columbus, we did some research and, for us, it’s one of the premier centers in the United States for cancer treatment so we were very comfortable with that decision.
Everybody we met at the James was wonderful—the doctors, the nurses, the people who make the food, the people who clean the rooms. They were all wonderful people, very kind, very loving, very patient, and not afraid to answer questions. I can’t tell you what a really good organization they have down there so I have no regrets going there. Because they took care of me, I’m here today and I get to enjoy my wife, my family, and my friends. I get to enjoy life. Two years ago, that was not the case.
Don’t be afraid to ask all the questions that you want to ask. Make sure that you’re getting the information that you need. You owe yourself that much.
Don’t be afraid to change. Don’t be afraid to try things. Rely on your family and friends because they want to help. They may not always know how, but they want to help. Allow them to be part of the healing process. It makes a big difference.
There has been some goodness that came out of all this and we’re trying to focus on that now. I’ve tried to forget some of the things that happened because they were so bad. I’m trying to look toward the future and enjoy life the best way I know how.
Have things to hold on to, whatever it takes for you to hang on for one more day. For me, it was religion. If you’re a religious person, God is your rock. We’re a religious family and that was something that helped us get to the next day.
Have hope. I know that’s going to be hard at times, especially if you’re getting bad news after bad news after bad news. Sometimes that happens. Don’t give up. Everything that we did that didn’t work was a stepping point for us to get to the next step, to the next day, and to where we are today. Do everything in your power to not give up.
You and the people around you are a lot stronger than you realize.
Michael

There’s nothing to be ashamed of when it comes to talking to a mental health professional. They can help make a big difference. Sometimes you need to talk things out. You and your family are under a lot of pressure and stress.You have a lot of questions and maybe wondering if you’re going to have tomorrow. That is another avenue that you can take to help you clarify and focus on what you have to do to get to the next day. Being prideful that you don’t show your emotions is not a good thing. No one can do that. Sometimes things come out and that’s okay.
Value your family, the day that you have, and the life that God has given you. Be glad to get up in the morning and see the sun come up. Be happy with small things.
You and the people around you are a lot stronger than you realize. I learned that about my children. You try to protect your children by keeping things from them because you don’t want them to feel pain, but I learned that you don’t have to keep things from them to protect them. They’re there to help you and they will help you in ways that you never thought would happen.
My grandkids would always write me little notes and tell me, “You can do this!” They were right. Family is everything and everything like that matters. The things that used to matter to me are not very important anymore. It helps you focus on what matters.


It has been an experience, but at the end of the day, it’s been a good one. I’m grateful for everything that everybody has done for us and for where we are in life right now. It’s good to be alive, so I’ll do the best I can to enjoy life every day and be happy.
We want to help and that’s why we do what we’re doing. If this makes one person’s day a little better, then we’ve accomplished our goal.
Figure out a way to take care of yourself. It may look different to you than it does for other people, but it’s important and it’s okay to think of yourself.
Kimberly
Kimberly: Advocate for yourself and for the person who you’re going through this with. We all assume that medical providers know everything. They know a lot and we’re thankful for them. However, they’re not with our loved ones day in and day out. They don’t see the subtle changes that happen day in and day out. There are things that you can bring to their attention that they may not catch. It’s not that they don’t know their job. It’s not that they don’t care or that they’re in a hurry. They’re just not with them.
Ask questions. If something doesn’t seem right, ask. The worst thing that’s going to happen is the doctor is going to say, “No, this is correct,” or, “I’ve already taken that into consideration.” The best thing that’s going to happen is you’re going to bring up something that they were unaware of and that could make a difference in care.


I encourage care partners, whether you’re a spouse, a family member, or a friend, to figure out a way to take care of themselves. They say to get rest and ask for help because you can’t give if your tank is empty. All of those things are true, but no one tells you how to go about that.
It’s different for each person. Oftentimes, it’s difficult to think of yourself because you’re healthy and not the one going through treatment or constantly wondering what’s going to happen tomorrow. It’s important that you figure out a way to take care of yourself. It may look different to you than it does for other people, but it’s important and it’s okay to think of yourself.
We were dealing with a recurrence so there were things that we needed to be aware of that someone who is getting a first diagnosis may not.
All the little things matter. If something is persistent, you might think it will go away and it might, but it’s better to find out. If something is persistent and you can’t get any answers, keep asking and keep looking. Don’t defer to, “This is the best we can do,” “We’re not sure,” or, “Try this.” Keep asking.
On this side, it’s easy to say, “You have to have hope. Hope is what got us through.” It’s true. Having hope keeps you going. However, when your husband’s glucose levels are so low that he shouldn’t be able to open his eyes or breathe and you’re not sure how many more breaths he has, hope is hard, but you have to find something to hold on to.
With a terminal diagnosis, that hope may be that you get to spend five more minutes with that person. It might be that you get to spend one more day with that person. Our mantra through the whole thing is that life is good as long as we’re breathing the same air. It didn’t matter if it was hospital air, Hawaii air, bedridden air in our home, but as long as we were breathing the same air, there was hope and that’s what got us through. Find whatever hope is for you.


Special thanks again to Genmab for its support of our independent patient education content. The Patient Story retains full editorial control.
Inspired by Michael's story?
Share your story, too!
More DLBCL Stories
Anna M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: a rRapidly growing, painless lump on the breast
Treatment: Chemotherapy
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant