Meghan’s Crohn’s Disease (IBD) Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

Meghan’s journey began with symptoms that are all too familiar to both Crohn’s disease and colorectal cancer patients: persistent diarrhea, blood in the stool, and severe stomach pain. Initially dismissed as stress-related by her doctor, it wasn’t until her condition worsened that another doctor suspected a more serious issue—possibly Crohn’s disease or colitis. This overlap in symptoms between inflammatory bowel disease (IBD) and colorectal cancer underscores the importance of thorough medical evaluation and early diagnosis.
After her diagnosis, Meghan tried various treatments. Initial oral medications didn’t work, so she switched to Remicade (infliximab), which put her in remission. Despite the medication’s risks, her symptoms improved and she was able to resume a normal life.
Five years later, her symptoms returned and after trying different medications, Entyvio (vedolizumab) helped manage her symptoms. In 2016, a routine colonoscopy revealed precancerous tissue, leading to the recommendation for a permanent ileostomy. Initially resistant, Meghan decided to proceed with the surgery after a pivotal conversation with her surgeon about her future. Despite initial concerns, she had two complication-free pregnancies and successful vaginal births.
Meghan’s husband has been incredibly supportive throughout her journey. She emphasizes the importance of finding a supportive community, maintaining a sense of humor, and living without regrets.
- Name: Meghan B.
- Diagnosis:
- Crohn’s disease (a type of Inflammatory Bowel Disease or IBD)
- Initial Symptoms:
- Persistent diarrhea
- Blood in stool
- Stomach pain
- Treatment:
- Remicade (infliximab)
- Humira (adalimumab)
- Methotrexate
- Entyvio (vedolizumab)
- Surgery: proctocolectomy

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
When I was in eighth grade, I started having diarrhea and it happened every single time I went to the bathroom.
Introduction
I’m from Charlottesville, Virginia. I love to travel. I love going to the beach, going on hikes, and being outside in general. I love spending time with my family.
I have Crohn’s disease as well as a permanent ileostomy. My biggest passion is disease advocacy and awareness.


Pre-diagnosis
Initial Symptoms
As a child, I was extremely active. I was an avid softball and basketball player, constantly going to camp. I spent tons of time outside. I was very active and very social.
When I was in eighth grade, I started having diarrhea and it happened every single time I went to the bathroom. Thankfully, my mom was very aware and thought it wasn’t normal. She told me we would go to the doctor because it was getting progressively worse.
I didn’t have any other symptoms. I went to the doctor and she said, “There’s nothing wrong with her. She’s just nervous and that’s why she’s having diarrhea.”
It felt like a punch to the gut because I never felt like a nervous child. It didn’t seem to be a good enough answer for what was happening. Thankfully, both of my parents advocated for me. They felt it didn’t sound right so we sought a second opinion.
I was in so much pain and my body was so weak. I was in and out of the hospital all the time.
Symptoms Worsen
I started having blood in my stool and horrible stomach pain. I went to see another doctor and at that point, they weren’t sure if I had Crohn’s or colitis. I continued to get worse. When I was a freshman in high school, I had to be homeschooled. I was too sick to get out of bed. It’s crazy to look back to see the 180 my life took. I was in so much pain and my body was so weak. I was in and out of the hospital all the time.
Diagnosis
I ended up having a colonoscopy and got diagnosed with Crohn’s disease. After getting a formal diagnosis, I began treatment. Compared to other people, I got diagnosed pretty quickly, but my health was rapidly declining.
Getting Diagnosed as a Teen
I turned lemons into lemonade. This was in 2006, so it was before social media and texting, but I could text 50 words a month. I was isolated from my friends. It was hard. I was homeschooled and a lot of people didn’t know where I was. All these rumors spread about me that I had died or had gotten pregnant and was sent away.
Meanwhile, I was in and out of the hospital and horribly sick, so it was hard. That was where the isolation came in plus not knowing anyone else going through this.


Treatment
I started various oral medications, but I wasn’t digesting them. I would take these medications, but they would go straight through me that I would see them in the toilet. Since the medications weren’t working, my symptoms weren’t getting better.
Remicade (infliximab)
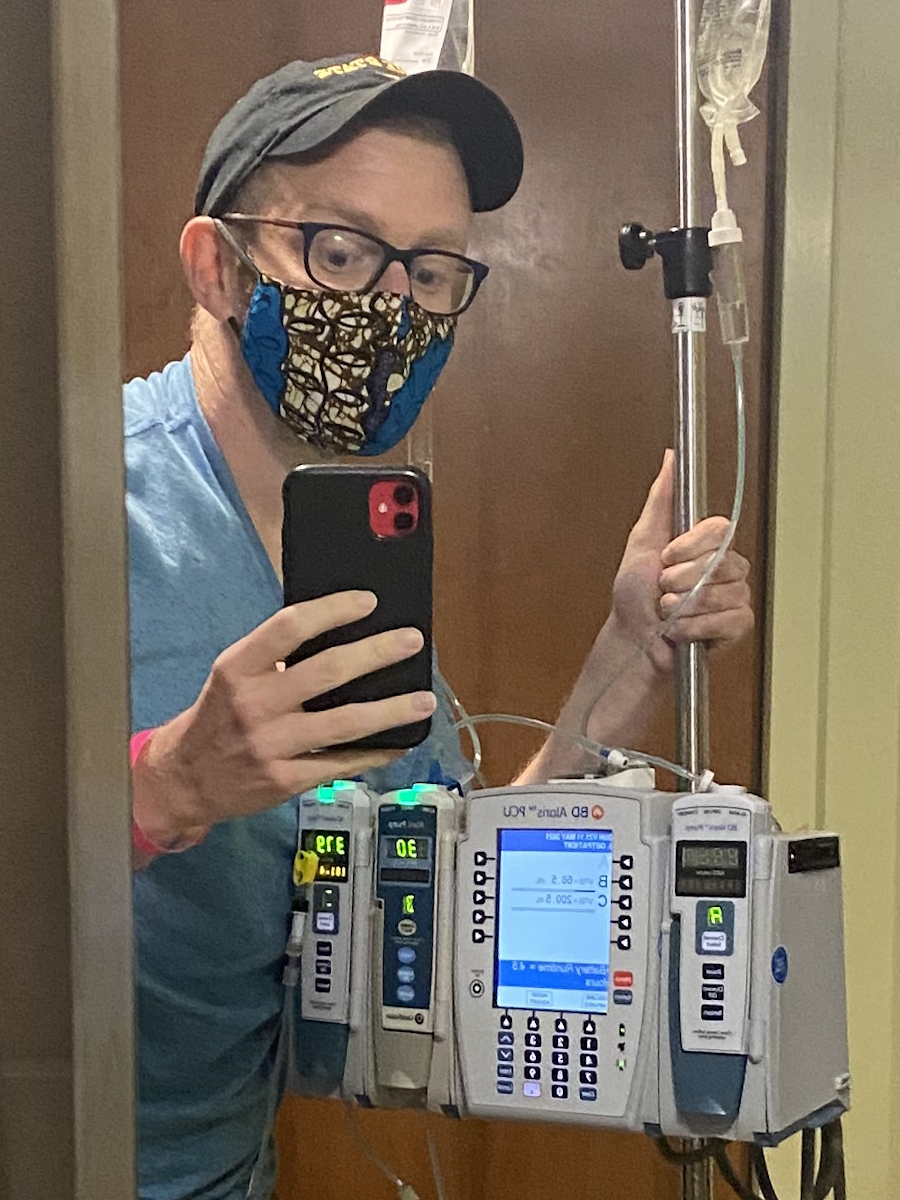
I started taking infusion medications and went on a drug called Remicade (infliximab). By the time I started my sophomore year of high school, I was in remission. I was on monthly infusions, but I was well enough to go to school. I was so excited to find some type of normalcy and feel good for the first time in a long time.
Everything was going great. My symptoms, for the most part, were at bay. The next question was: what do we do now? The infusions were eight-hour-long sessions. I would go to the hospital and stay for eight hours to get my medication.
I made it through high school and the beginning of college with symptoms at bay. Then in my sophomore year, I started to go downhill drastically.
Before I started treatment, while driving to the hospital, I could hear my parents whispering about how they were going to have to sign a waiver saying that they would not sue the hospital if I died by taking this drug. It was that serious, but they didn’t want to freak me out.
Remicade was a scary drug. When I was responding to it and doing well, they had to decide if they wanted to keep me on it. It’s a harsh drug and I was so young. We decided to get off of it.
Going Off Treatment
I went the homeopathic route for around five years. I took different supplements and probiotics. Those bought me five years.

Recurrence
Symptoms Return
I made it through high school and the beginning of college with symptoms at bay. Then in my sophomore year, I started to go downhill drastically. College is stressful and stress is one of my big triggers.
New Treatment
It was time to return to my doctor and go back on medication. I tried Remicade again because it worked well for me in the past. Unfortunately, I could no longer take it this time, so I went on a trial-and-error phase.
I tried taking Humira (adalimumab), which I didn’t respond to. I also tried methotrexate, which was a weekly injection that I had to administer myself. I drove home every weekend from college to give myself these shots.
Finally, after a lot of trial and error, I responded to a drug called Entyvio (vedolizumab). It didn’t necessarily send me back into remission, but my symptoms were kept at bay. Entyvio worked until I ended up having my colon removed.
My doctor said, ‘There is precancerous tissue deep within your colon. There’s a high chance that you’re going to need surgery.’
Getting a Colonoscopy
The conversation of having my colon removed was something I never had with my doctors. I didn’t know what an ostomy bag was when I was told that I needed one. It had never been mentioned, I had never heard of it, and I never thought I would be living with one.
At this point, I had graduated. I met my husband in college. We dated and right after graduating, we got engaged and got married at 23.
Eight months after we got married, in July, I went in for a routine colonoscopy. I had been feeling fine. There was nothing drastic or new. My symptoms had pretty much stayed the same. They were present but not how I had previously been in the past. I was able to function and have a life.
I went into this appointment excited because I thought they were going to tell me I was doing well. After all, I felt like I had been doing well. At the appointment, they came out and said, “We saw a few things. We’re sending a few biopsies off to make sure everything is fine.”


Getting the Biopsy Results
A week later, while I was home alone and my husband was at work, I got a phone call and my doctor said, “There is precancerous tissue deep within your colon. There’s a high chance that you’re going to need surgery.”
I vividly remember that moment. I collapsed in my kitchen crying because even though my colon was precancerous, all I could hear was the word “cancer.” Immediately, all I thought was I didn’t want to die. I was terrified.
I couldn’t believe this was happening to me. I was angry and upset. There was a lot of dwelling and processing.
Treatment-Decision Making
My surgeon and I talked about the different options I had. He said, “We can do nothing and hope for the best. We can remove part of your colon, but you’re going to have to come in for routine monitoring probably every three months or so, possibly have colonoscopies to check for any progression and make sure nothing is happening. Or we can remove your colon and your rectum, you will have a permanent ostomy bag, but you will never have the chance of colon cancer.” I left that appointment thinking, There’s no way I’m getting an ostomy bag. I’m not doing that. I’m not having surgery. I absolutely refuse that.
A week later, my husband had to deploy and I moved back home with my parents. I had a month to make this decision if I was going to have ostomy surgery or not. In the meantime, we went for a second opinion, which I always highly suggest because it never hurts. Unfortunately, it was the same response. This is what needed to happen.


I was still adamantly against it. I’m 24 years old. I’m not going to ruin my body. Thinking back, it’s wild that I was willing to live with the threat of cancer to have this unscathed body for the aesthetic side of it. I was willing to possibly have cancer and that blows my mind today that I would feel like that.
I fell into a dark tunnel. I don’t think it was depression, but I fell into a dark space. I couldn’t believe this was happening to me. I was angry and upset. There was a lot of dwelling and processing until finally, I went to my next surgery appointment where I was going to have to give my decision.
We had a conversation that changed my mind forever… He said to me, ‘Imagine being a young mom and finding out you have cancer.’
Deciding to Have a Proctocolectomy
I was ready to go into the appointment to say, “I will have part of my colon removed with the monitoring, but I’m not doing an ostomy bag.” That’s where I was at, even though my parents didn’t agree. They wanted me to do the ostomy bag because they thought this wasn’t something to joke with and we needed to be serious about this. I wasn’t ready to do that. My surgeon knew how horrified I was and how adamantly against it I was.
We had a conversation that changed my mind forever. I still get chills and goosebumps and tear up whenever I think of it. He said to me, “Imagine being a young mom and finding out you have cancer.” That put everything into perspective for me because he knew how important having a family and having children was to me. I left that appointment with my surgery booked to have my colon and rectum removed with a permanent ileostomy bag.


That conversation made me stop and realize that this wasn’t just about me. It’s also about my family. I want to be around for my husband and my parents. At that point, I didn’t have children, so it was also for my future children. I want to be able to have children, be there to watch them grow up, and be a significant part of their lives.
It made me realize it was worth it. It was worth it to have an ostomy bag to be able to be here with my children for every milestone and witness everything. It put everything into perspective. That’s a conversation I will never forget. I think about it every single day. That’s what led me to get my ostomy bag.
Going into it with an open mind, a more positive mindset, a willingness to learn, and a willingness to educate made a huge difference in my situation.
Mentally Preparing for a Permanent Ileostomy
There are two avenues to getting an ostomy bag: either it’s an emergency or it’s a planned surgery. I felt lucky because mine was planned so I had time to process beforehand. Even though I only had a month to figure everything out, I did what everyone else does: I went online.
This was 2016 and I was trying to find anything. There was social media, but I didn’t see a lot of ostomy on social media. I read a couple of blogs and there was one called The Stolen Colon, which offered more information and insight. Everything else I saw was the ostomy being associated with older generations. No one in their 20s had an ostomy bag.
All of the negative stigmas were popping up as well as the negative sides of having an ostomy bag. I tried to research and educate myself as much as I could beforehand. What helped was going into it with the mindset that it could only get better. I had been sick for so long. At that point, it’s been 10 years and my colon turned precancerous because of the intense scarring from Crohn’s disease. It could only get better, so why not try? It couldn’t get worse than it already is.
Going into it with an open mind, a more positive mindset, a willingness to learn, and a willingness to educate made a huge difference in my situation. Before having surgery, I felt very negative towards an ostomy bag. But as soon as I was rolled out after surgery, I never had any negative, upset, or harsh feelings. I always felt this was my second chance at life, so I’ll figure it out and get going. I felt like I missed out on so much when I was a teenager and in college. Now it’s time to make up for that.


What is an Ostomy Bag?
I always tell everyone that, essentially, my ileostomy bag is how I go number two. I have a stoma, which is a little round, fleshy pink-looking thing that sticks out of the skin on my abdomen, and it’s part of my intestines. My surgeons created a hole through my abdomen and brought a little piece of my intestines out. I wear an ostomy bag over it so you don’t see it and that’s what collects my stool.
I have to wear an ostomy bag at all times because I have no control. I don’t know when I’m going to the bathroom. It happens all the time. I have no urge to go.
I also don’t have a rectum. I had my rectum removed and that means I will have my ostomy bag forever because there’s no possible way to reconnect anything down there.
I always tell everyone to try everything. Once you find what works for you, it will be so much easier.
Ostomy Care
I’m biased because I’ve had this for almost eight years. At first, it’s very difficult to figure out. Once you get the hang of it and find the appliance that works best for you, it’s so much easier.
Overall maintenance is not too terrible. I change the complete system every three or four days. You buy an ostomy bag from the distributors and you get a prescription for ostomy bags sent to your house. You take it off and clean the skin around it. A lot of times, people will tell you not to use any soaps or perfumes because you can have issues with the adhesive sticking to your skin or an allergic reaction.
You have to empty your ostomy bag daily. I got into the habit of emptying it every time I use the bathroom even if it’s not full yet. I don’t like walking around with a full ostomy bag because it’s not comfortable.


There are certain factors that people have to deal with, especially if you have skin irritation. You can get skin irritation if your ostomy bag leaks because sometimes your stool can seep through under the wafer and it can sit on your skin. When that happens, it’s essentially burning your skin until you clean it off and change it. It hurts so bad because you have this rash. It’s difficult to get it to heal because you’re constantly covering it up.
They have different products to help treat different rashes. There are different adhesives because people may have an adhesive allergy. That’s where the trial and error comes in and that can be frustrating in the beginning when you’re trying to find out what works best for you. It can be very overwhelming, but I always tell everyone to try everything. Once you find what works for you, it will be so much easier.
Tips and tricks for ostomy bags change. Everyone asks, “How are you not pooping everywhere when you change your ostomy bag? You always have clean bag changes.” A big part of that is being mindful of when you last ate. I’ve had my ostomy for almost eight years. I have learned my body and my ostomy. I know that if I eat lunch at noon, I’m probably going to have output at around 1:00 or 1:30 PM, so I’m not going to change my ostomy bag after I eat.
I had my ostomy bag for a year and on the first anniversary, I posted a picture. I wouldn’t say I was hiding, but I wasn’t public about it.
A lot of times, people would change it first thing in the morning because you’ve been asleep all night and things have slowed down.
Another tip that I love and I’m always so surprised that more ostomates have not heard of this is eating marshmallows before doing bag changes. Marshmallows, bananas, and bread can slow down your output so you can have a small window to have a clean bag change.
Knowing how to have a clean bag change is important because, a lot of times, people are horrified to have a messy one. It sounds gross, but if you get output on your hands, it’s not a big deal. It happens. You can wash it off. Also, I have two kids, so it’s nothing.


Being Comfortable with Having an Ostomy Bag
I had my ostomy bag for a year and on the first anniversary, I posted a picture. I wouldn’t say I was hiding, but I wasn’t public about it. My husband and I saw it, but that’s it. I didn’t want to talk about it. That was my year to process and figure it out. I wasn’t trying to hide it, but I wasn’t the proudest of it.
A year into it, I made an Instagram account and made a post. I had come to terms with it and a big part of me said, “When I went through this, I didn’t see anyone else my age, so I want to put this out there.”
I had no idea what the response was going to be, but I felt okay and safe because I did this on Instagram. None of these people knew me. I had no idea who these people were. All I knew was they were people on the internet. To my surprise, I got an overwhelmingly positive response and that fueled the fire.
Having an ostomy bag did not take away from me as a person. Having that positivity helped me to become more comfortable.
Social media was a coping mechanism for me because it allowed me to express myself. I love to write. Before Instagram reels, Instagram was about posting pictures with captions, so I would post a picture and pour my heart out. That allowed me to cope.
The biggest thing was that it allowed me to accept myself and my body because other people were so accepting of it. I didn’t know any of these people. They were random people on the Internet, but people were so kind and genuinely wanted to know more. Having an ostomy bag did not take away from me as a person. Having that positivity helped me to become more comfortable.
I kept sharing and reached more people. People then started coming to me, asking for tips and advice. It quickly became my passion. That’s honestly how I became more comfortable with it. Finally, after seven years, I wore my ostomy bag out at the beach for the very first time. It was amazing.
I’m learning not to worry about what other people think and having the mindset that life is too short. Ostomy surgery was a huge experience. It made me realize that I don’t want to grow old and look back having these regrets that I didn’t do what I wanted to do because I was worried about what other people would think about me. It’s weird and funny, but I always tell people that I feel more confident with an ostomy than I did without because I had that life-changing experience that put everything into perspective.


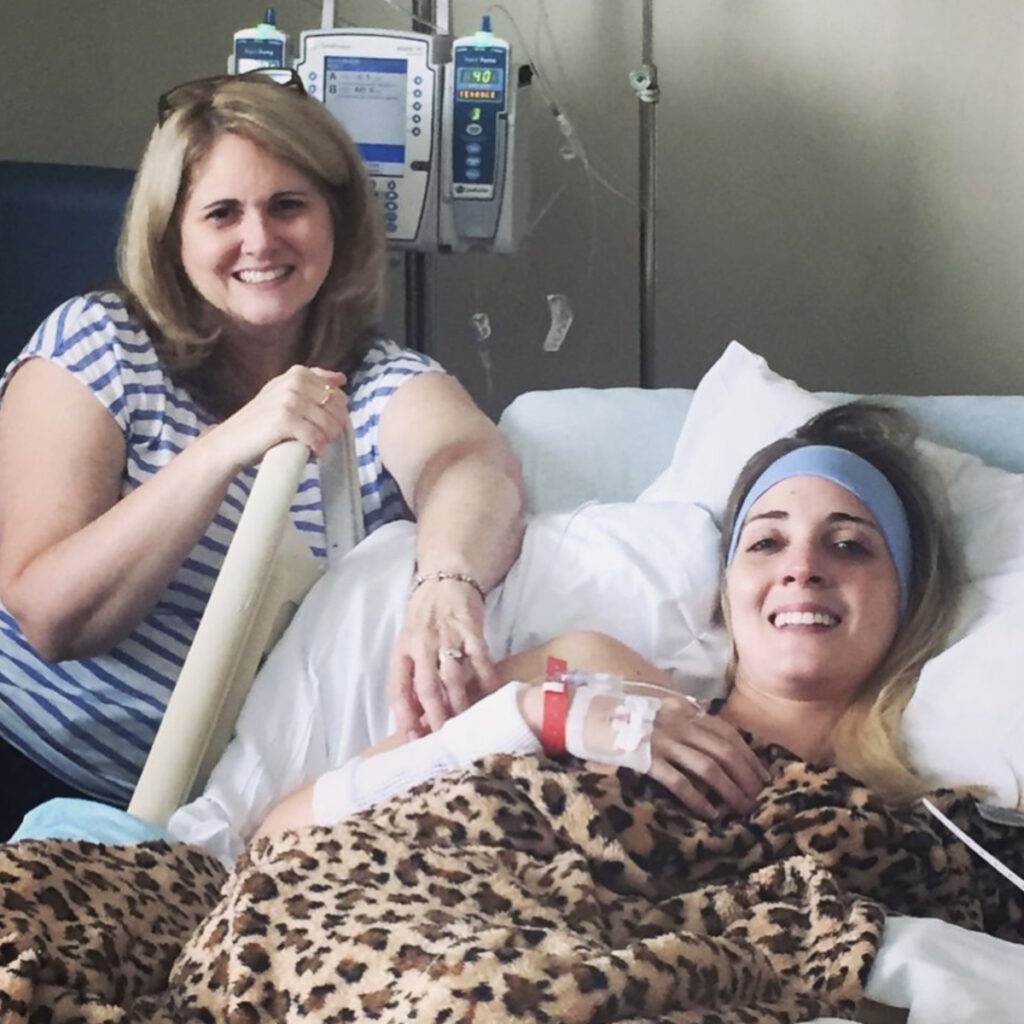
Being Pregnant with an Ostomy Bag
I had no idea what it was going to be like to be pregnant with an ostomy. There’s not a lot of research out there. With my first pregnancy, there weren’t a lot of other people who had been pregnant who were sharing their experiences. I was going to have to figure it out.
My doctors never said I wouldn’t be able to get pregnant, but I was concerned that it would be difficult because I had this massive surgery. I was worried there could be a lot of scar tissue. We tried for a year and a half, and while my husband was on his second deployment, I went to the fertility doctor to find out what was going on.
Thankfully, I only had a hormonal imbalance. It wasn’t ostomy-related at all. My husband had a short deployment, so he was gone for five months only. I did one round of Clomid (clomiphene) and got pregnant with our daughter.
On the ostomy side, there were a few changes but nothing crazy or out of the ordinary. As my belly grew, I had to switch ostomy appliances. I typically wear a convex wafer that helps push my stoma out, but because my belly was big and round, that wouldn’t fit anymore, so I had to wear flat wafers.
Everyone has a different situation and a different story, but pregnancy with an ostomy is possible.
My biggest concern was childbirth. Because I don’t have a rectum, I was scared to death that I was going to tear, which would cause issues with my rectum removal. My worst nightmare was having a baby and then going through “Barbie butt surgery” again and having to be stitched back up down there because that was by far more difficult than the ostomy recovery, in my opinion. I didn’t do the two surgeries at the same time.
Another concern I had was automatically assuming I was going to undergo a C-section, but thankfully, I had an incredible doctor who advocated for me. Dr. Bearling at Fort Carson was amazing. She asked, “Why do you think you’re going to have to have a C-section?” I said, “I don’t have a rectum and I have an ostomy.” She checked to make sure I still had muscle function down there and I did. I was still able to push, so she said, “You’re going to have a vaginal birth. You’re fine. You can do this.”
I am so glad I had that conversation with her. At the initial appointment when I first found out I was pregnant with my son, I gave them my history and told them that story. They said, “I’m glad you shared that because if you hadn’t, we were going to schedule a C-section for you.” There’s a difference in care.
Overall, I felt lucky with childbirth. I didn’t have any complications with my ostomy or during pregnancy. I’ve heard stories of people having stomach blockages and issues where they had to go in for surgery or deliver their baby early. People have said that the baby can kick inside where your stoma is located and that can be painful. Thankfully, my babies never did that. Overall, I had a great experience.


Postpartum with my son, our second-born, was wild. My hormones went crazy and, as a result, my skin broke out. Suddenly, I was reacting to the adhesive of ostomy appliances that I’d been wearing for five to six years at that point. My skin was an absolute nightmare. I had a 2-year-old and a two-week-old, and I am trying to get an ostomy bag to stick to my body. It wasn’t very pleasant.
My hormones readjusted after giving birth and the hormonal storm ended. My skin calmed back down and I was able to wear my appliance. Everyone has a different situation and a different story, but pregnancy with an ostomy is possible. It’s wonderful, it’s beautiful, and I’m lucky that I got to experience it twice.
I always think back to the conversation that I had with my surgeon because I’m at that age now. I’m that mom with young children. What if I did not have ostomy surgery? I could potentially have colon cancer right now with two young children. I’m so thankful every day that I made the hardest decision of my life to have surgery.
Ostomy surgery did not faze him. I’m sure he was freaked out and probably scared inside, but he didn’t let that show. He’d always been extremely supportive.
Having a Supportive Husband
Thankfully, I have a very wonderful and accepting husband. Before my ostomy, he had only ever known me as being sick. He’d never seen me healthy. I knew he was a keeper because I was sick all the time. There were numerous occasions where we’d been driving and we’d have to pull over to the side of the road because I was in excruciating pain and needed to use the bathroom or lay down in the car. He never batted an eye. He was always there to take care of me and help me with anything I needed.
Ostomy surgery did not faze him. I’m sure he was freaked out and probably scared inside, but he didn’t let that show. He’d always been extremely supportive. He fought tooth and nail to come home when I had surgery. They told him he couldn’t go home from deployment unless a close family member passed away. I don’t know how he did it, but he did and went back before I was discharged.
When he returned from his deployment, we had to navigate each other. We had been married, but it was like we were dating again. We had to relearn each other. He’d always been supportive, but deep down, I had these fears of being a different person compared to when he left. He took it with grace.


With intimacy, the best tip I can give is to have a sense of humor. Laugh it off. He’s my best friend and, thankfully, we can joke and laugh about things. Laughter and a sense of humor can be a great coping mechanism; it’s the best medicine. Nothing’s ever going to be perfect. Funny things are going to happen. They happen even to people who don’t have an ostomy bag.
He’s been so supportive since day one. Now he knows how to change my ostomy bag and we posted a video of him changing my ostomy bag. It’s so important to teach someone you know how to change your ostomy bag. If something ever happened to you or you were physically unable to do it, having someone close to you who knows how to take care of you and help you in that way is extremely important.
You can still live a long, beautiful, happy, healthy life with an ostomy bag. Try to keep a positive mindset and view this as your second chance in life.
Words of Advice
Finding a community is incredibly important. I turned to social media to find my ostomy community. You would be surprised at how many people in the world have an ostomy bag. People you know may have one, but you wouldn’t know it. Put yourself out there and be willing to find community.
I have made so many lifelong friends through social media. I’ve had the pleasure of meeting a couple of them in person. Being able to connect with someone who has gone through a situation like yours is earth-shattering. Someone could have all the empathy in the world, but it’s truly difficult to understand unless you have been through it. Having a community where you can talk about these things with other people who have similar experiences makes such a huge difference.


Ostomies save lives! You can still live a long, beautiful, happy, healthy life with an ostomy bag. Try to keep a positive mindset and view this as your second chance in life. You can do things that you didn’t get to do. This is what helped me and made me into the person that I am today. I’m a changed person since having an ostomy bag, but I’m so happy with where I am.
An ostomy bag is not the end. It’s all about how you perceive it and how you decide to live with it. I’ve grown to love and appreciate it. You can do everything with an ostomy bag. You can do anything that you want to do. It’s all about the decisions you make and how you decide to live with it.

Inspired by Meghan's story?
Share your story, too!
More Crohn’s and Colitis Stories
Kristen F., Crohn’s Disease (IBD)
Symptoms: Fatigue, abdominal cramps, blood in stool, loss of appetite, frequent and painful bathroom visits, perianal disease (open wound), mouth sores, joint pain
Treatments: Multiple medications, surgeries (temporary ostomy, total colectomy and permanent ostomy, Barbie butt surgery or proctectomy)
Jess G., Crohn’s Disease (IBD)
Symptoms: No appetite even when offered a favorite dessert, weight loss
Treatments: Steroids, blood transfusions, biologics, surgeries (colectomy, small bowel resection, colostomy)
Ariel D., Ulcerative Colitis (IBD)
Symptoms: Overactive bowel, heavy cramps in stomach area, abdominal pain
Treatment: Surgery (ileostomy)
Alli R., Ulcerative Colitis
Symptoms: Blood in stool, unexplained weight loss, stomach pain, constant defecation
Treatment: Surgery (ileostomy)
Sarah A., Ulcerative Colitis
Symptoms: Bowel irregularity, severe stomachaches, blood in stool
Treatments: Surgery (ostomy surgery), steroids, anti-inflammatory medication (mesalamine), biologic therapy
Dana D., Crohn’s Disease (IBD)
Symptoms: Abdominal pain, diarrhea, blood in stool
Treatments: Surgeries (colon resection, total proctocolectomy with end ileostomy,
abdominal perineal resection, myocutaneous flap), steroids, biologic therapy