“I’m Still Affected 25 Years Later”: Maria’s Experience with Kidney Cancer as a Child and Colon Cancer as a Young Adult
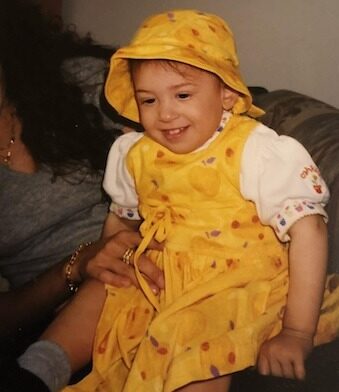
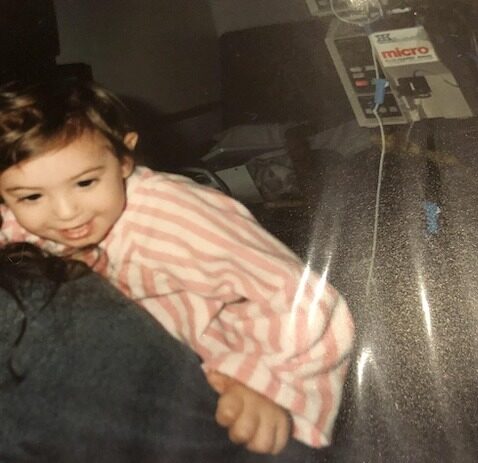
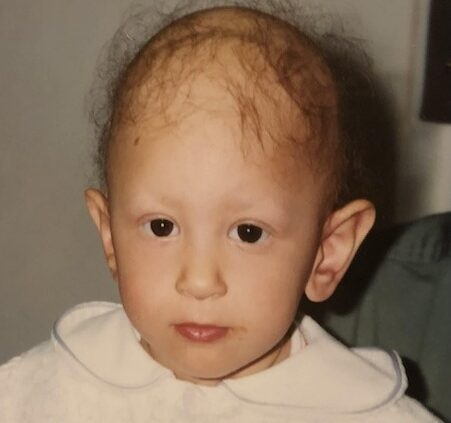
Maria’s cancer experience began when she was just 15 months old, when she was diagnosed with Wilms tumor, also known as nephroblastoma, a pediatric kidney cancer. Growing up, she was in and out of hospitals in Ottawa, Canada, for countless appointments, treatments, including surgery and radiation, and a gastrostomy tube or G‑tube that stayed in place for 12 years. She says that as a young child, all she knew was that she was sick and assumed everyone else lived that way, too. She adds that she felt confused and in denial about the seriousness of her cancer.
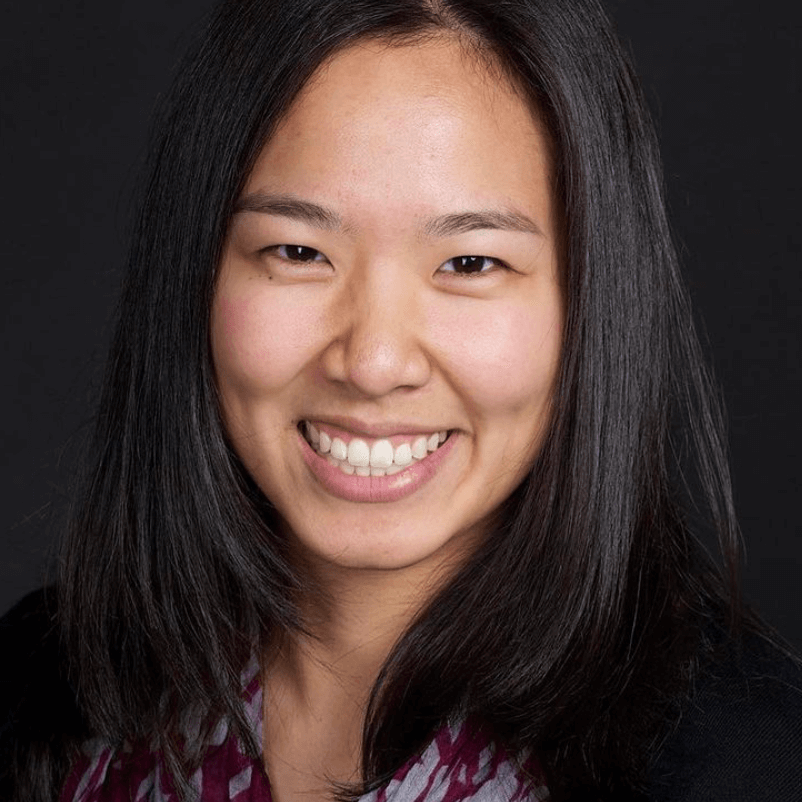
Interviewed by: Ali Wolf
Edited by: Chris Sanchez
As a teenager, Maria says she started experiencing bleeding in her stool and stomach issues, but when she told her pediatric oncologist about these symptoms, she wasn’t taken seriously. Eventually, a colonoscopy revealed early-stage colon cancer, which was removed with a small surgery. Even then, Maria’s instinct was to think, “It’s gone, so everything is good now.”

In her 20s, Maria faced new challenges, including bowel obstructions and recurrent polyps requiring colonoscopies every six to 12 months. For about half a year, clinicians suspected she had Bloom syndrome (BSyn), which can carry a significantly shortened life expectancy. Later results confirmed mosaic variegated aneuploidy syndrome 3 or MVA3, a rare genetic disorder where some cells have an abnormal number of chromosomes. MVA3 is associated with increased cancer risk, especially Wilms tumor.
That diagnosis transformed Maria’s outlook. During the months when she thought she had Bloom syndrome, she believed her life might be very short. She focused on Brazilian jiu-jitsu and spent time with her cats. After learning about MVA3, she was told she would likely live much longer. She began planning her career, and today Maria works as an educational assistant supporting students with disabilities. She continues to heal emotionally through therapy, peer cancer communities, and her own evolving understanding of her experience as a childhood cancer survivor.
Watch Maria’s video or read the edited interview transcript below to know more about her story.
- Maria explains how her rare condition has affected her physical and mental health decades later
- She highlights the importance of self‑advocacy in healthcare, especially as a young adult whose symptoms were dismissed or minimized
- The importance of connecting with other young adult cancer communities and doing therapy to recognize that long‑term emotional and physical effects are common and valid
- A universal truth in Maria’s experience is that patients often know their bodies best and deserve to be heard and believed when they describe symptoms
- Her perspective shifts from denial to healing, helping Maria to envision a bright future that includes work, hobbies, and ongoing healing
- Name: Maria F.
- Age at Diagnosis:
- 15 months
- Diagnosis:
- Kidney Cancer (Wilms Tumor)
- Mutation:
- Mosaic Variegated Aneuploidy syndrome 3 (MVA3)
- Symptom:
- Back pain
- Treatments:
- Surgery: nephrectomy
- Chemotherapy
- Radiation
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Hi, I’m Maria
- New job and working as an educational assistant
- Living with disability and wanting to support others
- Childhood innocence and realizing life was different
- Family silence, denial, and wanting more information
- Learning the word “cancer” and truly understanding it as an adult
- Denial, early colon cancer, and not being believed
- ER experiences, advocacy, and pain
- Early colon cancer removal and initial denial
- G‑tube, long‑term pain, and waiting for help
- Feeling like a burden and hearing my mother’s pain
- Cancer camp, Young Adult Cancer programs, and therapy
- Finding connection with other survivors
- Bowel obstruction, polyps, and finally getting coordinated follow‑up
- My thoughts on genetic testing and Wilms tumor features
- My experiences at different ages and PTSD from procedures
- Minimization of pain and struggles in the ER
- Early signs as a baby and port, surgery, chemo, and radiation
- Self‑advocacy, mental health, and healing from childhood cancer
Hi, I’m Maria
I had Wilms tumor, which is a kidney cancer, when I was 15 months old. I live in Ottawa, Ontario, Canada.
I am 27 years old. I just turned 27 last week, and I’m a big enthusiast of martial arts, and I do Brazilian jiu-jitsu. I’ve been doing this sport for about eight years, I believe, and I did kickboxing in the past, and I compete once or twice a year. I’m really interested in that. That’s one of my biggest passions.
I love Brazilian jiu-jitsu because it makes me feel more empowered and able to do things in my own body. Even though what I’ve been dealing with as a child, I’m still able to use my body and to perform with my body. It’s very physical, but it’s also challenging to the mind, and it’s very close contact, so you make friends for life, and you’re in very close contact with them. You have to trust them, and through jiu-jitsu, I’ve been able to feel a bit more confident in myself. I’m still trying to increase that, and I’m also trying to increase more positivity in my life, and I have a lot of great people there that help me get through that and help support me.
I help support them as well in what they need in life.
New job and working as an educational assistant
I actually just had an interview yesterday for a job, and I got the job today. So I’m happy to see in the new year what that will lead to. Currently, I’m also a casual EA at the school, but starting in the new year, I think I will have a more stable position at the school.
Right now I’ve been helping a lot with people with disability or in wheelchairs. I did that in the past as well, but now I’m in the schools with that, so I help them with education as well. It’s an EA. Yes, it’s an educational assistant.
Living with disability and wanting to support others
I think because I’m also a person with disability, and I don’t think I really understood that when I was a kid, and understood all the possibilities of help that I could have had. I had my mom advocate for me for some help as well. But now I see the amount of help that you can ask for. Now it might be different because of the difference in generations.
I think just trying to support kids now, and also adults, when I used to work with adults, just to be able to fulfill their life and make their life easier in education, that’s why.
Childhood innocence and realizing life was different
I think I was very innocent as a child. I didn’t really think of anything at all. Later on, as I aged, I noticed that not all my friends were dealing with the same stuff. I thought everyone dealt with it. I thought having millions of appointments a year would be normal for people. I just knew I was sick when I was younger, and that’s all I knew.
When I tried to ask my parents when I was more curious and I turned a bit older, they would tell me, “Oh, well, your brothers are going to do the same thing when they get your age,” since my brothers are younger than me. For me, I thought, “Haha, they have to deal with this stuff when they’re older.” But it was definitely not the truth. I think they did that to protect me, and they weren’t sure what they wanted to tell me or how to tell me yet, because I was still a young child.
I also felt, because of the cancer stuff too, that I did feel like a normal child, but I knew that I didn’t really develop as much as the other children, learning‑wise. I realized that some kids knew a lot more than I did, and it was just, “Okay, well, I don’t know what I’m supposed to do. I don’t know why I’m in school, but I don’t know.”
I didn’t know that there was a life after. So after you graduate, you can start working, you can get married, you can have kids, and all that. I just went day by day, not really understanding a lot.
Family silence, denial, and wanting more information
I think it would have been nice to know a bit more. We’ve never really spoken truly about things. It was always if someone came by to visit, sometimes my mom would tell some stories to them, and that’s how I knew a bit more about myself or what happened when I was younger. But we never had an open discussion. It always felt like a closed door. So it would have been nice to have a bit more.
Also, knowing what’s happening, why things are happening like this. I think I was always left in the dark. That led me to denial when I was older, too. “Okay, well, everything is fine, it’s fine,” because when I was a kid, my parents didn’t cry or anything. They didn’t seem like they were upset. They just said, “Okay, it’s okay.” But I think that was just in front of me, and behind my back, they would probably say more than that.
Learning the word “cancer” and truly understanding it as an adult
I think that was more towards when I was a teenager. I think I knew the word when I was maybe an early teenager, but I didn’t really understand everything fully until maybe even adulthood.
I think that I really understood also because I was able to go to camp, and I was seeing other adults who were diagnosed as a kid and really able to talk to them and really understand a bit more. I think mentally as well, learning‑wise, it was easier for me to understand then, because I couldn’t really develop well even as a teenager. Maybe I thought I understood, but now that I’m older, I think it’s mostly when I was a young adult that I really understood, “Okay, this is happening, this happened, and now I’m continuing trying to survive this and understand and knowing that this happened when I was a kid, but now it’s still affecting me over 20, 25 years later.”
Denial, early colon cancer, and not being believed
I think I knew maybe when I was a teenager, I was more in denial because I was a little bit rebellious against the healthcare providers as well. Because of that, I had symptoms not of recurrence, but symptoms from colon cancer, and it turned out to be an early stage of colon cancer. But the doctor, my oncologist at the time in pediatrics, didn’t really believe my symptoms. Then, when I told her, “Okay, then I don’t have this symptom,” she would say, “Okay, well, you did tell me you had that.”
So it was very confusing, and I was very in denial, like, “Okay, maybe I’m just making things up.” But it was a pretty big symptom, and I knew that symptom. I had some bleeding in my stool for months, and I felt like, “Okay, maybe it’s not as important as I think it is.” When I was older, I got sick as well. I kept having some stomach issues, so I think from then on I knew, “Okay, I’m still affected by this. I’m still affected by the chemo, by the radiation, and by the surgeries from when I was younger.”
So it was an early stage of colon cancer, and that’s because I got sick later on. Eventually, I did get a colonoscopy. They finally figured out it was that, and they were able to remove it. But my oncologist at the time didn’t believe me or didn’t really help me at the time.
I’m not sure. She asked if I had any bleeding in my stool or anything like that, and I said yes. Then I said, “It’s a bit too much information,” but she asked if I was bleeding in my stool or just when I’m wiping or anything, and I said both. She said, “It can’t be both, so you have to pick one.”
Then I told her, “Okay, well, it’s none,” and then she said, “Well, you told me it’s both, so which one is it?” I don’t remember what it was at the end, but it was just a weird encounter. I haven’t seen her since then. I didn’t want to see her again. I was 17.
ER experiences, advocacy, and pain
I think I definitely felt disappointed, but I wasn’t shocked because there were a lot of times before that that doctors either ignored me or didn’t believe me. I really thought that was going to be the norm from then on.
So now every time I go to the ER, I make sure I’m in like a ten‑out‑of‑ten pain before I go, and I make sure I have my mom or a friend with me, because if I go alone, I get treated really poorly, and I’m in too much pain to advocate for myself.
My mom usually has the energy to push, and she’s been through it with me, so she knows how to push doctors.
Early colon cancer removal and initial denial
I think that was in 2018. I was probably around 18 or 19 during that time. It was either 2018 or 2019, but it was a very early stage, so they were able to remove it during the colonoscopy.
When the doctors told me about that, my instinct was, “Okay, it’s gone, so everything is good now.” I think I was still in denial, not understanding that now there’s a very big chance of recurrence and things like that. I find that I’m very lucky that that one was caught really early, and I just needed a small surgery to remove it.
G‑tube, long‑term pain, and waiting for help
Obviously, I can’t remember the very early years. I do remember being around four to ten years old. In those years, I knew I had a lot of appointments, and I was in school.
I also had a G‑tube, and I’m struggling with the pain from that till now. I’m supposed to go to the pain clinic, but I’ve been waiting for eight months now, and I’m still on the waiting list for that.
Feeling like a burden and hearing my mother’s pain
I think with my mom telling the story a few times, and she did have a few speeches at her school since she’s a teacher as well, just knowing that when she tells the story that she’s in pain, she’s still in pain, or she’s still tearing up — and that’s been over 25 years now — I feel a bit of a burden. I felt that a long time ago as well, and now I’m trying to heal from that.
I definitely do feel guilty putting her through all that, even though I know it’s not my fault. I know she’s been there a few times, at least. She’s always been on my side in the hospital. I’ve been in the hospital, I think, about a year at a time, and sometimes in and out, and I’ve been in the ER over 300 times at the children’s hospital.
She mentioned how it was difficult to go through treatments because I wasn’t eating, and that’s when they decided to put the G‑tube, the feeding tube. I had that for 12 years. A few times, I was in a Code Blue situation, so she mentioned how scary that was.
Since I was young, for radiation, I had to be put under. They don’t do radiation in the children’s hospital, so in Ottawa, we have the children’s hospital, and there’s a tunnel that goes to the General, which is for the adults. They had to run all the way there to do the anesthesia, get the radiation done, and run back before I woke up.
She mentioned that even from a young age, I had a very high tolerance to pain and a very high tolerance to medication. Sometimes I was in a Code Blue because they gave me too much morphine, even though I wasn’t falling asleep or acting the way the anesthesia was supposed to act.
Cancer camp, Young Adult Cancer programs, and therapy
Now it’s much better. Being able to go to the Ottawa Cancer Foundation and YACC (Young Adult Cancer Canada) and the cancer camps as a child and as an adult really helped. YACC as well, because there are some conferences, and they talk about things like that. It was nice to see that those are normal things that people who are surviving or have survived cancer feel too, that you’re not the only one.
It’s nice to see that in the community. It helped a lot. I started doing therapy as well to help with things like that and to heal from the past. I hope these videos help, too, for other people to know that they’re not alone and that there are a lot of things we don’t talk about or doctors don’t tell you about. Those other survivors really — it felt kind of like a relief, like, “Okay, okay,” and there are also strategies to try to understand and try to heal from it in Canada.
Finding connection with other survivors
I think just meeting those people, it felt so easy to meet them. There was just this type of bond that’s already connected, and this type of empathy. You don’t need to say anything, but you just understand each other. It was so nice to meet all these people.
For years, I thought I needed to get over this — these fears, everything like that — because it’s been so long since I had cancer and this shouldn’t be affecting me now. But knowing and seeing them, it really did really well for me.
Bowel obstruction, polyps, and finally getting coordinated follow‑up
When I was an adult, maybe in 2022, I had another obstruction in my bowel. A non‑surgical oncology doctor from gastro came in to see me and started to really follow up with me, really started the ball moving because I kept having a lot of polyps reappearing every year. I keep having colonoscopies every six months to a year and endoscopies as well.
She really pushed the ball to see genetics and to see another gastro as well, to keep following up, and just to see all these different doctors to really keep me in the loop. I hadn’t had a good follow‑up since I didn’t want to see that oncologist as a child, and that oncologist as a follow‑up in adulthood, too. I didn’t want to see her.
Genetic testing, Bloom syndrome scare, and mosaic variegated aneuploidy syndrome 3
In the genetics department, they were able to assess me, and they were able to test for a genetic disorder for polyps in the colon, but it tested negative. They kept doing those tests. They really thought I had Bloom syndrome. So I did the bad thing of searching it up and noticing how little the life expectancy is, and because they were pretty much 99% sure I had that, they kept retesting me when it was negative.
Because there was a low life expectancy, for, I think, half a year, I was thinking, “Okay, I’m still in school, so I don’t really need to get a job because I’m not going to live that long.” I wanted to get more into jiu-jitsu, really get better at it because I like that, and to spend time with my cats and maybe travel if I can. That was really my goal. But then they noticed it was something else, and it was called mosaic variegated aneuploidy syndrome 3, and there’s just a high risk of cancer, and there’s no danger to life expectancy.
Then my perspective kind of changed, like, “Okay, so I actually need to get a job, and I need to figure out everything else, but also monitor my health,” because this year has been a bit more downhill. I’m going to live longer than I expected, which is nice to know, but I need to rethink, because I was trying to accept death at an early stage. I’m happily living now. I’m trying to do the best I can to do what I can.
My thoughts on genetic testing and Wilms tumor features
For me, it was a bit of a shock, because usually it’s kind of odd to have cancer below the age of two or even below the age of five. So I feel like they should have or would have tested me then. But at the same time, the genetic testing that I did at the end, because they realized it’s definitely not Bloom syndrome, is like a sister disorder to it, because they have very similar traits.
It was due to Wilms tumor and also short stature, learning disability or developmental disability, microcephaly, and trouble feeding, which are all things that I had as I was diagnosed with cancer. So all these things, it just seems like it would have been a normal thing to do to test. But the testing pool for MVA3 was still being developed, so there are still some false negatives. I was just really lucky.
Yeah, that’s what I’m thinking. It’s nice to know. Right now, I’m still having a lot of stomach issues, but I know what’s going on, and I’m still following up.
My experiences at different ages and PTSD from procedures
I think it was a mix when I was very young. I didn’t know anything, so I was just like, “Okay, okay.” My mom would play games with me when I was waiting for appointments. The floor was very colorful, so I had to jump from one color to another, and they were fun games. I did have this one scan that I was really terrified of, and I think even as an adult, I’m scared of it. I noticed with therapy that I might have a bit of PTSD from that and the sound of it.
I also had a favorite nurse. I could only get blood work with this nurse and no one else. Anyone else — it was no. I would throw a fit.
As a teenager, I think mentally everything was just… as a teenager, your mental state is a bit wonky. It was very difficult back then, because I think I was also rebellious. As an adult, I think I had one good encounter because the doctors I followed up with were really nice, but my ER visits were always very difficult.
Minimization of pain and struggles in the ER
I’ve never felt believed. I always felt like I was just a child being a spoiled brat and just whining because of menstrual pain. That’s what doctors would ask me all the time, like, “Are you on your period?” if I came in with stomach pain, which is all the time, I had obstructions. They would always say, “Do you have menstrual pains? Do you have your menstrual cycle right now?” It was hard because I’m not going to go to the ER just because of that.
Also, because I have a high tolerance to pain, it’s difficult to demand more pain meds, even for my mom to do that. In my last visit, I was very sleep deprived, and I was in a lot of pain, but they were not giving me the amount of painkillers I needed. I was a bit delusional too because of lack of sleep and pain. I told my mom, “Okay, we’re leaving because they’re not helping, they’re not doing anything.” Eventually, my mom was able to get someone from anesthesia, an anesthesiologist, to try to help me with the pain.
There’s always this type of situation. It was never very smooth. If it was, there was just one time it was good in the ER, but when I went to the floor, it was a disaster. Other times it’s the opposite way around. It was just difficult to go through the medical system in that case.
Early signs as a baby and port, surgery, chemo, and radiation
That’s what my mom would say. They would say that I kept rocking myself, throwing myself on my back, and the doctor said that was my way of trying to relieve the pain from the tumor.
I had my port installed first. My port was actually under my armpit instead of on my chest by accident. Then I’m not sure what happened first, either chemo or surgery. I believe it was surgery first, and then chemo, and then radiation.
No recurrence, just monitoring.
Self‑advocacy, mental health, and healing from childhood cancer
I think I’d like to say how important it is to try to advocate for yourself, because I always thought, “Okay, I’ll listen to the doctors,” but also, you know what’s best for you. You know your body the most.
In the mental health aspects, I’m seeing a therapist right now, but especially if you’re diagnosed at an early age, I would recommend, the earlier the better. I think I’m still trying to go through some of the trauma from my cancer journey when I was a kid, and also recognizing that it’s there, even though I thought I was just a kid and didn’t really notice until now.
I’ve learned from therapists that there’s someone else who was diagnosed at an early age, and they mentioned how they have some PTSD from sounds as well, but they were so young that they don’t really see or notice why. It lives through your body as the pain lives through your body. I think it’s very important, if you’re not going to therapy, to talk to someone you can relate to or do some exercise or something to help yourself.

Inspired by Maria's story?
Share your story, too!
More Kidney Cancer Stories
Maria F., Kidney Cancer (Wilms Tumor)
Symptom: Back pain
Treatments: Surgery (nephrectomy), chemotherapy, radiation
...
Mia H., Kidney Cancer (SMARCB1-Deficient Renal Cell Carcinoma, Non-Sickle Cell Trait), Stage 4
Symptoms: Bad cough, fatigue, nausea
Treatments: Chemotherapy, radiation, immunotherapy
...
Alexa D., Kidney Cancer, Stage 1B
Symptoms: Blood in the urine; lower abdominal pain, cramping, back pain on the right side
Treatment: Surgery (radical right nephrectomy)
...
Bill P., Kidney Cancer (Papillary Renal Cell Carcinoma), Stage 3, Type 1
Symptoms: Kidney stone, lower back pain, sore/stiff leg, deep vein thrombosis (DVT) blood clot
Treatment: Nephrectomy (surgical removal of kidney and ureter)
...
Burt R., Pancreatic Neuroendocrine Tumor (pNET) & Kidney Cancer
Symptom: None; found the cancers during CAT scans for internal bleeding due to ulcers
Treatments: Chemotherapy (capecitabine + temozolomide), surgery (distal pancreatectomy, to be scheduled)
...
Bill P., Kidney Cancer (Papillary Renal Cell Carcinoma), Stage 3, Type 1
Symptoms: Kidney stone, lower back pain, sore/stiff leg, deep vein thrombosis (DVT) blood clot
Treatment: Nephrectomy (surgical removal of kidney and ureter)
...
Laura E., Type 2 Kidney Cancer (Papillary Renal Cell Carcinoma), Stage 4
Symptoms: Profound fatigue, hypertension, high red blood cell count, severe back pain, badly swollen legs
Treatment: Chemotherapy (Cabometyx (cabozantinib) assigned under S1500 PAPMET clinical trial)
...
Nina N., Kidney Cancer (Chromophobe Renal Cell Carcinoma), Stage 2
Symptoms: Blood in urine, blood clots, intense abdominal pain
Treatment: Partial nephrectomy (surgical removal of right kidney)
...