Kate’s Stage 4 Hormone Positive Breast Cancer Story
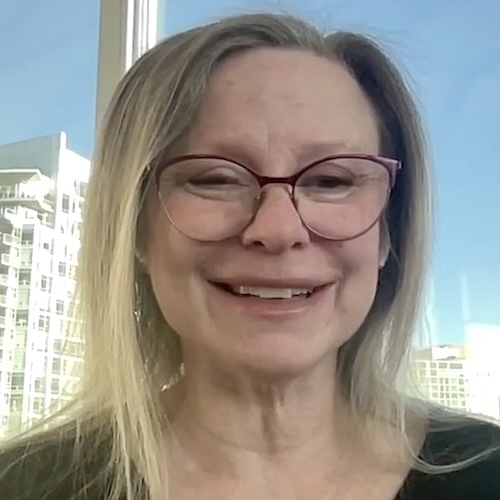
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez

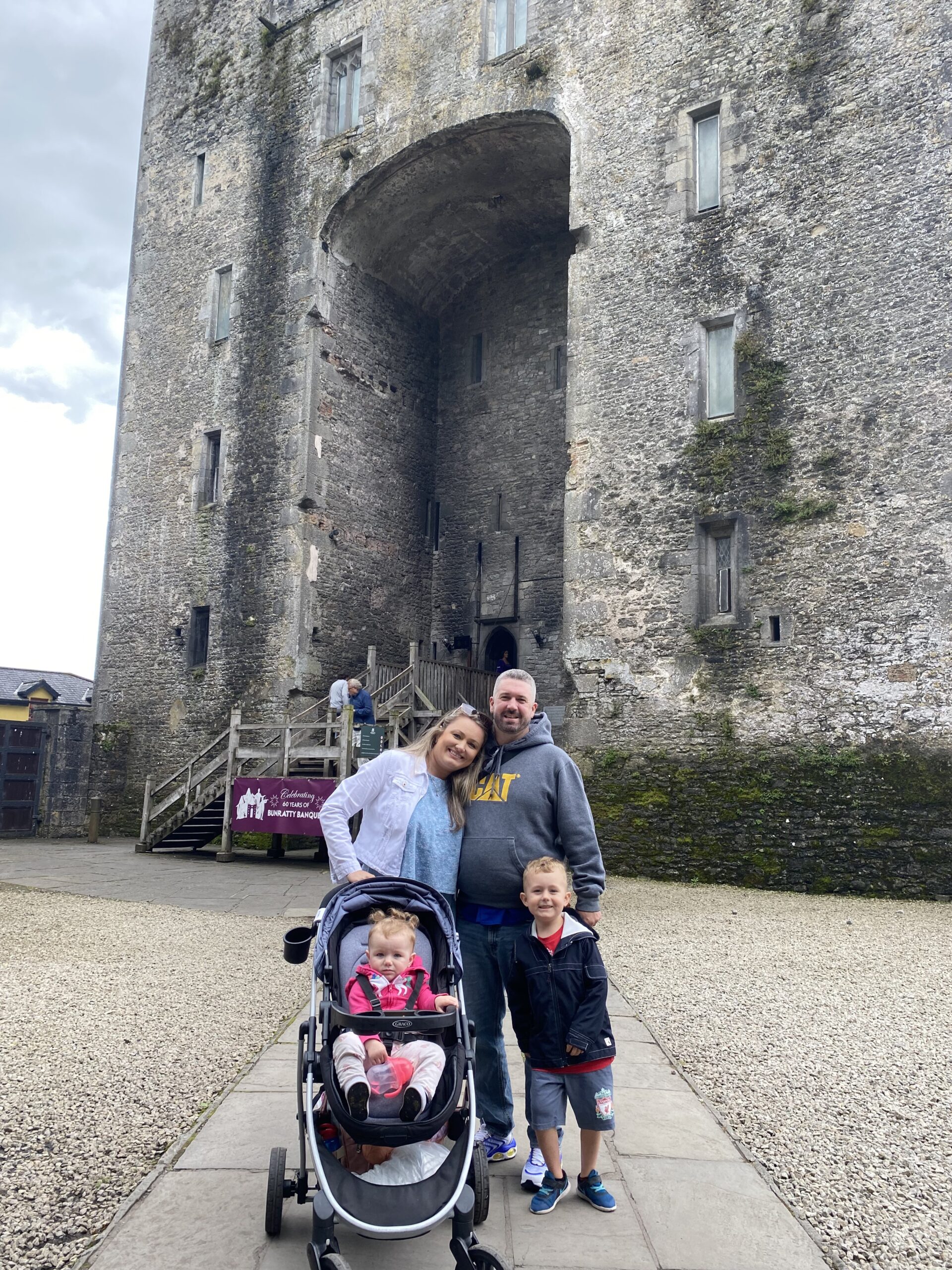
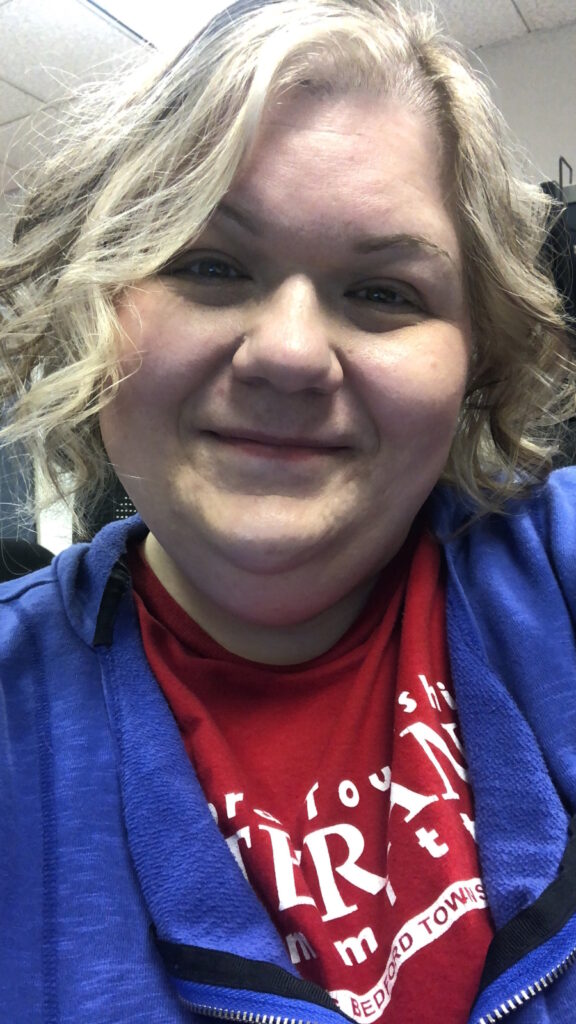
Kate, a 35-year-old mother of two from Brantford, Canada, was diagnosed with stage 4 hormone-positive breast cancer in late 2024.
Kate’s journey began in 2022, when she discovered a lump while breastfeeding her daughter. At the time, doctors dismissed it as a cyst, stating she was too young for a mammogram or biopsy. Over the years, doctors repeatedly disregarded her concerns, despite the lump growing significantly.
Balancing her roles as a mother, wife, and student pursuing a master’s in applied disabilities, Kate experienced severe anxiety, insomnia, and high blood pressure. She and her doctors had chalked these symptoms up to her hectic life, but later realized that they were signs of her advancing cancer. After she finally underwent a mammogram, ultrasound, and biopsy in July 2024, her hormone positive breast cancer was diagnosed as stage 3. However, additional scans confirmed that it was instead stage 4, after it had been found to have spread to her hip bone and some lung lymph nodes.
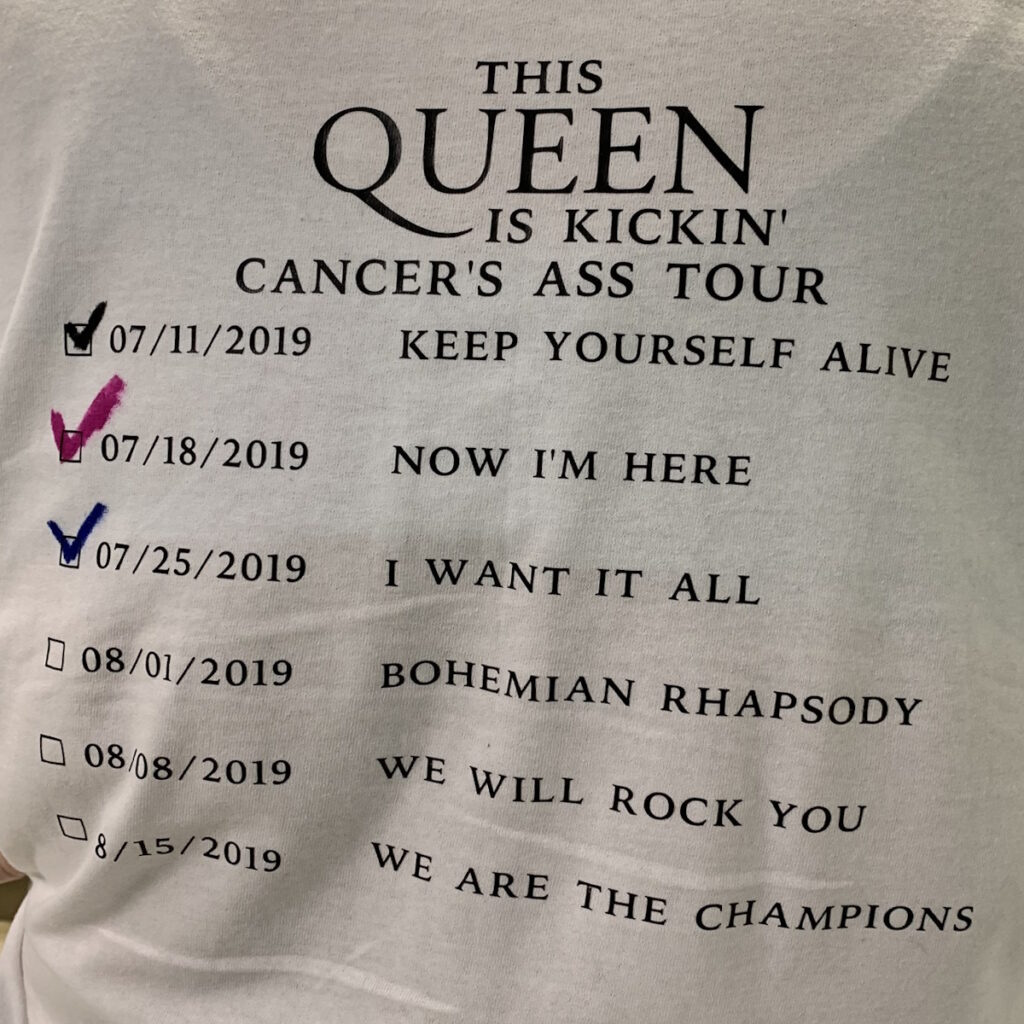
Kate quickly began an aggressive treatment plan, consisting of chemotherapy, a planned double mastectomy, and radiation. Despite the option to transition to palliative care, she chose to continue fighting for her family, especially her young children. Kate faces the physical and emotional toll of treatment, including exhaustion, chemo fog, and hair loss. Losing her hair was particularly difficult, but she found solace in the support of her husband and children, who embrace her unconditionally.
Her children, a 6-year-old son and a 2-year-old daughter, keep her motivated, though she struggles with guilt over their missed activities due to her treatment. Kate stays active in their lives, ensuring normalcy while relying on her strong support system, including family and friends who celebrated her birthday with a surprise party before her chemotherapy began.
Though she mourns the loss of aspects of her femininity, including the prospect of a hysterectomy due to her hormone positive breast cancer subtype, Kate prioritizes survival for her family. She and her husband chose not to freeze her eggs, feeling content with their 2 children.
Kate remains grateful for her oncologist, who has been thorough in diagnostics and treatment planning. She has not sought a second opinion, trusting his expertise. While the road ahead is uncertain and involves continued treatments, Kate draws strength from her determination to see her children grow and her close-knit circle of loved ones. Despite the challenges, her resolve to fight for more time with her family, to live her life to the fullest, and to help others advocate for themselves defines her journey.
- Name:
- Kate C.
- Age at Diagnosis:
- 34
- Diagnosis:
- Breast cancer (hormone receptor positive)
- Staging:
- Stage 4
- Symptoms:
- Rapidly growing tumor in right breast
- High blood pressure
- Insomnia
- Anxiety
- Treatment:
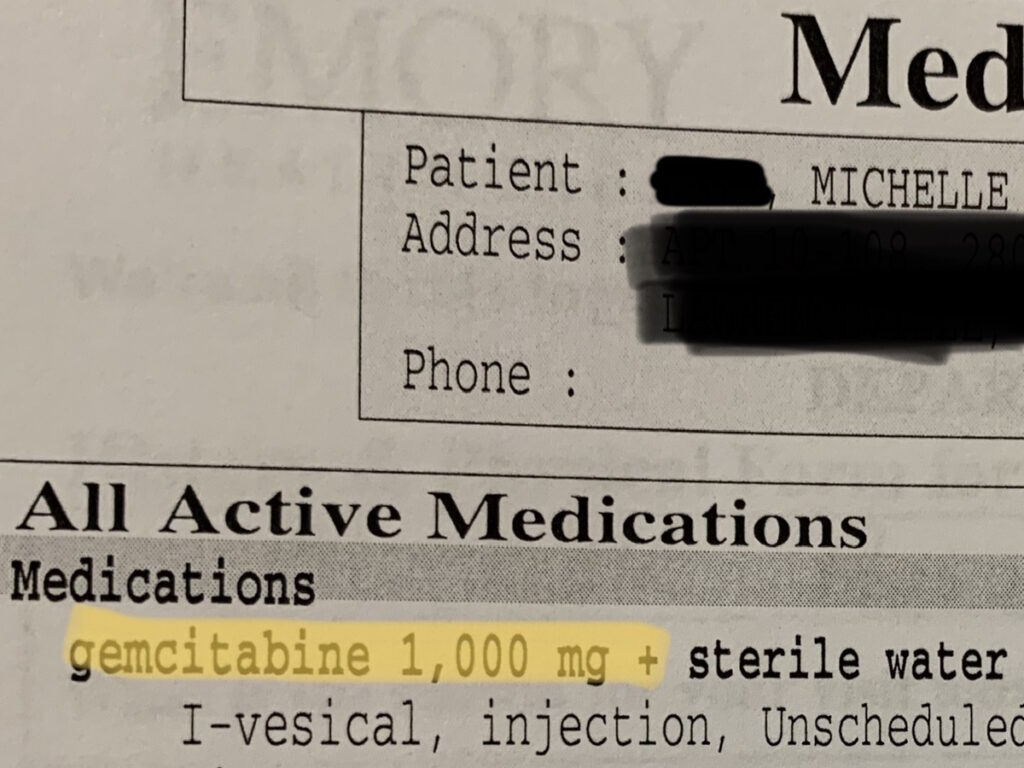
- Chemotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.

Inspired by Kate's story?
Share your story, too!
Related Cancer Stories
More Breast Cancer Stories
Deb O., Breast Cancer (De Novo Triple Positive and ER+ HER-)
Symptoms: First instance: appearance of lump that later on increased in size, orange peel-like skin around inverted nipple, persistent ache under right arm; second instance: appearance of lump
Treatments: First instance: chemotherapy, targeted therapy, hormone therapy; second instance: surgery (mastectomy), chemotherapy, radiation therapy, CDK 4/6 inhibitor
Tammy U., Metastatic Breast Cancer, Stage 4
Symptoms: Severe back pain, right hip pain, left leg pain
Treatments: Surgeries (mastectomy, hip arthroplasty), chemotherapy, radiation therapy, hormone therapy, targeted therapies (CDK4/6 inhibitor, antibody-drug conjugate)
Nicole B., Triple-Negative Metastatic Breast Cancer, Stage 4 (Metastatic)
Symptoms: Appearance of lumps in breast and liver, electric shock-like sensations in breast, fatigue
Treatments: Chemotherapy, surgeries (installation of chemotherapy port, mastectomy with flat aesthetic closure), targeted therapy (antibody-drug conjugate), hyperbaric oxygen therapy, lymphatic drainage
Dalitso N., IDC, Stage 4, HER+
Symptoms: Appearance of large tumor in left breast, severe back and body pain
Treatments: Surgery (hysterectomy), vertebroplasty, radiation therapy, hormone therapy, clinical trial
Marissa T., ILC, Stage 4, BRCA2+
Symptoms: Appearance of lump in right breast, significant fatigue, hot flashes at night, leg restlessness leading to sudden, unexpected leg muscle cramps
Treatments: Chemotherapy, hormone therapy, PARP inhibitor, integrative medicine
Janice C., Triple-Negative Metastatic Breast Cancer, Stage 4
Symptoms: Appearance of lump in left breast near sternum, fatigue, bone and joint pain
Treatments: Surgery (lumpectomy), radiation therapy (brachytherapy), chemotherapy
Dana S., IDC, Stage 4 (Metastatic)
Symptom: Appearance of large lump in left armpit
Treatments: Targeted therapy, hormone blockers, bone infusions
Maria S., Breast Cancer, Stage 4
Symptoms: Intermittent but severe pain including a burning sensation on the side of the breast, appearance of a cyst and a lump, abnormally warm and pink-colored breast, nipple inversion, strangely liquid menstrual periods, unusual underarm odor, darkening and dimpling of the nipple, severe fatigue, night sweats
Treatments: Chemotherapy, surgeries (mastectomy, lymphadenectomy), radiation therapy, targeted therapy
- 1
- 2