Rich’s Stage 3B Melanoma Story
Rich B. shares his melanoma story of his first symptoms, how he got diagnosed, the importance of self advocacy, deciding whether to join a clinical trial, and his actual treatment of immunotherapy and side effects.
Explore below to learn more about each topic. Thank you for sharing your story, Rich!
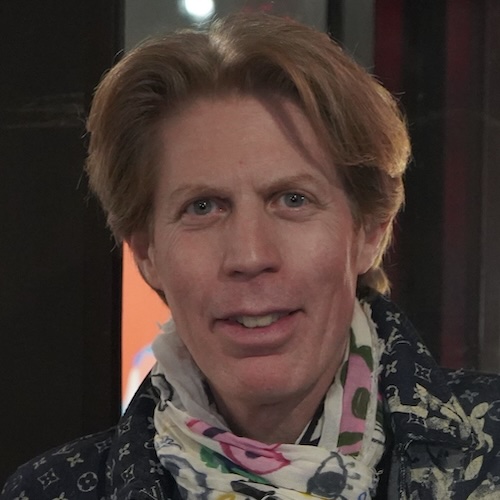
- Name: Rich B.
- Diagnosis (DX): Melanoma
- Stage: 3B
- Age at DX: 34 years old
- Symptom:
- Suspicious, dark spots
- Tests for DX:
- X-ray finds tumor in sacrum measuring 9×6 centimeters
- MRI results show what looks like a giant cell tumor
- PET scan reveals 1-cm lytic lesion, prompting start of treatment
- Treatment:
- Immunotherapy: Nivolumab (Opdivo)
- Pre-Diagnosis
- Diagnosis
- Tests and Scans
- Treatment Decisions
- Surgery
- Melanoma Staging
- Transition from the Surgeon to the Oncologist
- The Importance of Self-Advocacy
- Treatment Decisions
- Could Identifying the Cause of Melanoma Impact Treatment in the Future?
- How did the specialist bring up the possibility of a Clinical Trial?
- How Did the Specialist Lay Out Your Treatment Options?
- Was it a PET scan that you underwent or a CT scan?
- How did you rationalize having to wait for your scans?
- How did the scans go?
- Making the Decision to Join a Clinical Trial
- Clinical Trial Onboarding Process
- What was onboarding onto a clinical trial like?
- What were your thoughts when receiving the clinical trial information packet?
- Any guidance for those considering joining a clinical trial?
- Did you have to consider anything with payment?
- Is it unnerving to agree to pay for uncovered costs not really knowing what is or isn’t covered?
- The Randomization Process
- Treatment Timeline
- Treatment & Side-Effects
- Key Takeaways
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
First Symptoms
Rich describes how he noticed suspicious dark spots on his skin as his first symptoms of melanoma and how he got his diagnosis.
Pre-Diagnosis
Who is Rich outside of cancer?
I’m the fourth of four children. I grew up in a little town called Grand Island in New York, which sits in between Buffalo and Niagara Falls, so I grew up with a lot of snowy winters. I started life out in service as a US naval officer. After I graduated college, I’ve done a lot of different things professionally, but on a personal side of things, I entitle myself as a runner.
My dad was the high school cross-country coach and I started running when I was three years old. I’ve more or less been running throughout my life. And in the last 10 years I’ve been starting to get into marathons and stuff like that. That’s one of those things that keeps me centered. So that’s me on the personal side. Professionally, I’m a designer in Silicon Valley, I’ve been doing that for the last 12 years.
Running is an outdoor sport and my cancer is melanoma, so there’s a correlation between running and where I am in my cancer journey. I grew up in the 70s and 80s and we didn’t have a lot of sun protection back then. I don’t know if any of my current situation is related to that, but I’ve spent a lot of my adult life outside doing long runs and tried my best with sun protection, but nobody’s perfect.

It seemed like within a matter of a few weeks, this thing just really grew and was dark and misshapen on my left calf.
Rich B.

Diagnosis
What were the first symptoms?
I had a dark spot on my upper chest that was there for a long time, and I never did anything about it but it had been there for a couple of years. But then in 2021, around July, I noticed a similar kind of dark spot that just appeared out of nowhere. It seemed like within a matter of a few weeks, this thing just really grew and was dark and misshapen on my left calf. I was paying attention to that part of my leg every day, and within four to six weeks, this thing was protruding out of the skin.
I thought, that really doesn’t look right, I should probably go get these two things checked out. I figured time was of the essence because I was concerned at how quickly this thing had shown up and was growing. I didn’t know a ton about cancer or melanoma, I just knew something was not right.
Tests and Scans
What was the wait for test results like?
The dermatologist set the expectation that these things take about five business days. I was expecting to hear about a week later, not knowing exactly when I would hear back and in what form I would hear back. I probably should have asked at the time, but I didn’t.
Honestly, looking back, I wish I would have asked more. But I had that kind of preconception that it was likely to come back not so bad. And even if it did, I didn’t really know what the path would be. I was definitely ignorant going in, compared to what I know now. I probably would have probed a little bit more as to what to expect and what the decision tree would look like, if things are positive or negative and that kind of thing.
What was it like to get the results?
I’ll never forget this, because in my profession, I’m a design leader and I was having a scheduled offsite with my team. There’s no good time to get a call like this, but it was in the middle of a working session. I knew it was a doctor’s call because I recognized the phone number, but I couldn’t pick up at the time. I called back and then the doctor was busy and there was a little bit of phone tag, but ended up getting my dermatologist on the phone later that afternoon.
I knew I wanted to be by myself and just be prepared for whatever it was that she was going to share. She told me she got the biopsy results back and it tested positive for melanoma. I actually have a pit in my stomach reliving that moment. I was writing on a piece of paper, jotting down everything and trying to ask questions in the moment. But I honestly wasn’t necessarily prepared for that conversation. I didn’t have a script or anything.
Reliving it, there’s just the seriousness and the weight of somebody telling you you have cancer. That’s something you never forget but also probably never stop feeling when you relive that moment.
What did the dermatologist tell you about the biopsy?
The dermatologist said there were certain parts of the biopsy that were concerning in terms of the depth of the melanoma, meaning how deep it’s gone in the skin. They could see the cellular growth in the biopsy. And there were a couple of things that were really good about it. It wasn’t ulcerated, meaning it wasn’t exposed, which would have been a bad factor. So it was some good news, some bad news about it.
She said, this is concerning enough that I’m recommending that you go talk to a surgeon to go to the next stage, which is going to involve some surgery around that site as well as another test of your lymph system.
Did you feel prepared for the call about the results?
I appreciated the fact that they don’t just put the results on their online platform and let you read them by yourself with no professional there to help provide the context behind it. If it’s a phone call, if it’s in the office, you have a human being there that’s a professional to help address your immediate rational concerns. I don’t know if physicians are there to be emotional counselors. I don’t know if I necessarily expect that.
But I would say there’s probably a missing step in between the taking of the biopsy and the actual result delivery, which is what are the possibilities that can come back for you, that would be nice to have before entering a conversation like that. It would have been nice to know what are the three or four things that could happen in this conversation so I know the spectrum of good news and bad news that I could potentially get in this call.
How did you react to getting the results?
I jotted down what she said and took a pause. I didn’t really have time to deal with it in the moment because I needed to be social with my team. And so I had 24 hours to just put it aside for a second before I could deal with it.
Everybody there would have been totally understanding if I had said, I’ve got to go, I’ve got some news I have to deal with, but that’s not who I am. I think it’s just one of those things where I try to put everybody around me before me. I don’t know if it was the right thing, but that’s just what I did in the moment.
Who did you tell after you got the news?
Fast forward 24 hours later, I was done with the offsite and had probably an hour and a half drive back home. I started making some phone calls and my first phone call was to my sister, who happens to be a doctor. She was my primary source of helping me unpack what this means. And even then I was unprepared because my sister was asking me a lot of questions that I just didn’t know the answers to. I didn’t have a document in front of me, I was in the car.
I was looking for more of an immediate conversation, just to get a sense of how serious does she think this is before getting into the nuts and bolts of it all. But she said she needed to see that biopsy report and just really dig in so she could help me a little bit further. And so it was somewhat settling and somewhat unsettling. During that drive back I started to really understand what surgery was going to be, what that was all about and what could potentially happen afterwards.

Treatment Decisions
How did you find your surgeon?
It was a referral within a system that assigned me to someone in close proximity to where I live. And probably a factor was that the dermatologist said because of the rate of growth, time is of the essence and we need to take care of Rich sooner than later.
What was the appointment with the surgeon like?
He walked me through what the surgery was all about. There were two parts to it. First was the shave biopsy. He was going to take a larger portion of the area around that site out to make sure that all the cancer was removed from that area. He set the expectation that it was going to be pretty big and told me what that was going to be like afterwards and the healing process and all that.
Part two was what they call a central sentinel node biopsy, which is basically the lymph node cluster that’s closest to the melanoma site. What they do is test that area, and they’re going to be a little bit smart about it. They use some radioactive material that they inject in the original melanoma site the day before, and then on the surgery day they also apply a dye into that area so they have a visual and radioactive identification of which particular lymph node would be the most likely place where cancer would have traveled to and metastasized.
He explained all of that and what to expect. I asked, is this general anesthesia? I thought it was, but that was maybe something that would have been a headline that I just reaffirmed.
And then he told me that the other part of recovery was talking to a plastic surgeon afterwards about how they were going to repair my wound site, because on the leg it’s different skin and therefore they can’t hold it together like they needed to do a skin graft. So the plastic surgeon needed to explain what my options were in terms of skin graft as part of recovery.
Did you consider getting a second opinion?
This is where I’m lucky to have my sister because she was doing a lot of research on her side. She told me that if there’s cancer on the skin, if it has these types of indicators, a wide excision surgery is definitely recommended. The lymph node biopsy is standard procedure, everything the surgeon said is all pretty standard action. I was able to get her opinion and using her network, I probably had five opinions coming into this, so I was pretty confident. Plus, she could look up the surgeon and see if he was a good surgeon or not. So I was pretty lucky from that perspective.
Did you know what stage your cancer was before the surgery?
It was loosely explained to me that your lymph node biopsy will determine if you’re more advanced. If it does, if your lymph node comes back, you’re some form of stage three, potentially stage four, because stage three means it’s traveled outside of the local site to somewhere else. Stage four would be if it’s traveled beyond the lymph nodes to other organs. And this is where I realized that melanoma was much more serious than I first thought when I started down this journey and how really serious this cancer is.
Did you look up anything about melanoma online?
This brings up the second pit in my stomach as I’m reliving this journey. This is where Google is maybe not so good because you start Googling survival rates.
– Rich B.
I did not realize that if I’m at stage 1, it’s a 99% survival rate, you’re all good. But then if you’re stage 3, it’s about a 65% survival rate. That biopsy was really important now that I might have a third less chance of being alive in five years.
And then, heaven forbid, if it’s stage 3 and I have to go get scans for stage 4 and if it’s stage 4, it’s a 1% survival rate. At least that’s what I was reading online. The curve is just ridiculous.
That puts you in a panic mode. I thought, wow, two months ago, this was not even a thing, and now I’m in this world of I don’t know, my future is so uncertain at this moment. You’re in this place where you can’t know until you get some more procedures and tests and you have to follow this path and be patient, even though it’s really hard to be patient.
Do you have any guidance for people seeing those kinds of numbers?
My advice is, the numbers online are much lower than what is probably going to be true for your particular situation. There are other factors, like what access you have to health care. The treatments in place are totally changing the game in terms of survivability and your ability to overcome this diagnosis. So it’s hard to rationally program your brain to interpret numbers, but my one piece of advice is to be a little bit more optimistic than what you’re reading online.
Staging
Rich describes how it felt to go through surgery and his reaction to learning about his melanoma staging.
Surgery
What did you have to do to prepare for the surgery?
This was my first surgery ever in my life. I was freaking out about the actual surgery itself. I think it’s probably pretty natural for human beings to be afraid of being put under. You just get all these notions about will I wake up, all these things. Even though it was a relatively straightforward surgery as surgeries go, you still have that in the back of your head.

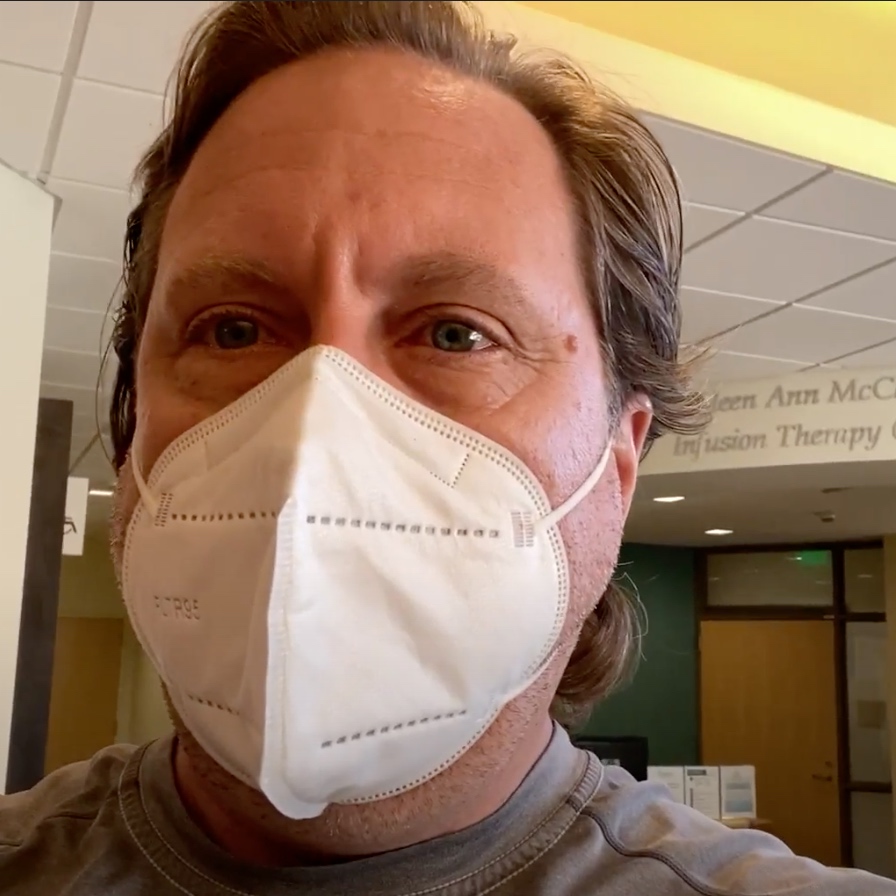
One thing I had to deal with was having cancer during a pandemic. There are extra procedures to even be in the hospital and all these things, and I had to be extra cautious beforehand to make sure I wasn’t doing anything risky whatsoever to get COVID prior to my surgery because time was of the essence, every day mattered. I was already really cautious, but I wasn’t going out anywhere the couple of weeks prior to surgery.
Then there were just the normal procedures to get ready for surgery. I had a COVID test a few days prior and then they give you a special soap to disinfect your body that you use during the two showers before you go into surgery. Then there’s the fasting the day of surgery, for about 12 hours or so. I was fortunate enough that my surgery was in the morning, so I had an early check in and that’s always easier than fasting for 12 hours when you have a surgery later in the evening.
What was the surgery like?
I was pretty anxious about it, to be honest. The people that do surgeries have had a great bedside manner and were keeping me at ease.
The worst part of the day was getting the IV set up for the anesthesiologist to do the anesthesia. The rest of it was a cakewalk in terms of any pain. There was no pain or anything along those lines.
– Rich B.
The actual surgery lasted around two and a half to three hours. You’re on the table and you’re talking and then you wake up and that’s pretty much what it was. The anesthesiologist was asking me about this and that. I remember waking up and my girlfriend was there, just walking into surgery, it was really great.
Waking up I was a little, not groggy, but I was just a laid back version of Rich is how my girlfriend described it. I’m always polite, but she said I had a very, very warm, polite tone asking for a sandwich. I was really hungry. Then I was there for about an hour under observation, my girlfriend was there hanging out with me. And then I didn’t have any complications, so then they were ready to move me.
How did you feel right after surgery?
There really wasn’t much in terms of any side effects from the anesthesia. For the next 24 hours after the surgery they prescribed me painkillers, but I’m afraid of painkillers, so I was actually able to successfully avoid all painkillers after surgery. Even though there’s a good portion of my leg that was taken out and I had a skin graft and a surgery site to access my lymph nodes, I was pain free post surgery. For the next week I was quite immobile because I had one leg that was in a boot.
What was the recovery like?
One part that was a little inconvenient was I had a skin graft close to my hip. I think it’s a little unique to this particular scenario where they take the top portion of your skin and it’s exposed. It’s a perfectly square open wound. They have to wrap it in plastic. It’s almost like Saran Wrap and it has to sit there for like a few days before they can take it off so it can disinfect itself and heal without anything that will infect the area. You can shower with it since it’s sealed up, so that’s not a problem.
My original melanoma site was a pretty sizable deep surgery site that they had to basically stuff with antibiotics. It almost looked like a garlic clove that they just put in there and they needed to leave it there for a number of days. I couldn’t shower with that. So I had to half shower my body with that leg out of the shower just so I could at least clean my upper body once or twice before I went back in four days later to get the bandages taken off.

How have the surgery sites healed?
It is still pain free where they took the skin graft. If you’ve ever had a road rash, that’s what it feels like. It would scab over like that. The self heal didn’t look great for a few weeks, but it was healed enough where the body wouldn’t get an infection. My surgery site is still healing months later. I’ll always have that scar. But it was a couple of weeks before I could take off all the bandages and expose that area to the air.
When did you get the answers from the lymph node biopsy?
This was probably the most tumultuous part of my journey, because I had researched and been talking with my sister for counsel, knowing the importance of this biopsy report. If it was negative, my cancer journey was done, I would have been at stage 1, which has that 99% survival rate. Then there’s no treatment required, it was just localized. All would be well, I’m done and would just need to recover from my wounds.
If it was positive, then that puts me in at minimum stage 3, which going back to those survivability numbers is a big freakout. You’re building up to this very important moment in your life that could go in very opposite directions. There’s a lot of anxiety I felt during that time.
– Rich B.
The surgeon did say that the labs were backed up. I don’t know if it was COVID related, I don’t know if it was lack of staff or just a lot of other tests that were backlogged. It was going to take a little longer than normal. They couldn’t give me an exact time of when this was going to get back, which made me more anxious, of course.
It was probably a week and a half later when I was called back into the surgeon’s office, and that was the moment where he had a piece of paper. I could just tell it wasn’t good news. Even though everybody was wearing masks, I could read their body language, and I could tell he would have a skip in his step if this was a different report. That was the moment where he told me I had a small tumor on the lymph node and that was going to set me on my next path in the journey.
Eventually that would result in a stage 3B diagnosis. But at that moment, I only knew it was at least stage 3. I didn’t know if I was in a stage 4 situation because if it had traveled to lymph nodes, it could potentially have traveled to almost anywhere else in the body. I know the brain is an obvious spot for melanoma to travel to, but any number of organs plus the skin plus other lymph nodes, it can go anywhere once it’s metastasized.
Melanoma Staging
How did you feel after receiving the test results?
I had with the surgeon who delivered this biopsy piece of paper that said my lymph node tested positive and I had a tumor. That moment is like, I have a tumor, right? Melanoma was like, it’s on the skin. I think this is also, at least from a language perspective, ups the ante even more.
I feel like my blood pressure even going up now, hearing tumor, because it wasn’t tumor yet, in my mind anyways. It was a thing on my skin. And I think this is maybe something specific for melanoma, where it’s on the surface, it’s visible, it’s slightly different than maybe most cancers that are internal. And I think this is a threshold. It’s like, wow, this is now an internal tumor versus something I could see on my skin. I can’t see this thing, which made it even that much more scary.
And so I was kind of left as a quick conversation. I don’t know if surgeons are the best humans necessarily to deliver that message. It’s nothing against surgeons. I don’t know. They’re not cancer experts. Anyways, I was just kind of left like in a cold room with another setback in my life.
And I just kind of wanted to cry. I had hopes that my cancer journey would be done at this point, but it was tough.
– Rich B.
Did you have to see a new specialist?
The surgeon left me was like, okay, we’re going to refer you to oncology. Never had to deal with oncology before. So it’s another first, and that’s another threshold you never imagine yourself personally having to go down that path. Cancer is around all of us. But I don’t know. I guess I never… We all probably do deal with it the same way. It just becomes so real when it’s you, even though you’ve had family members that have battled. There’s something different about that news directed at you. And so, I don’t know. I was freaking out, but I was like, okay, here’s the next thing.
How fast can I get an appointment? Because days matter for me, right? This thing could have traveled within a matter of weeks. If it’s in my lymph nodes, the sooner I can get a scan, the sooner I can understand if I have bigger problems or not.

Treatment Decisions & Self-advocacy
Rich shares how he processed the emotions of the diagnosis, having to advocate for himself to get treatment options and information more quickly, the shared document with important information and questions he and his caregivers shared (called “Rich’s Fight”), and the importance of speaking up for yourself for better care.
Transition from the Surgeon to the Oncologist
How did it feel being referred to an oncologist?
Yeah, I just remember sitting in that room. It felt cold. It just felt really cold.
Like here’s a third of a death sentence. At least that’s how I felt. This is such an important piece of information, and it seemed so transactional.
– Rich B.
And again, I’m not faulting the surgeon. It’s not his fault necessarily. I think it’s more the system of how to think about somebody’s emotional journey through this process, but kind of seeing a seam in the system in regards to okay, now, you’re on to the next phase and I did my part for you. Again, no fault to the surgeon, but it’s like now I’m kind of in a chasm.
I don’t know who’s this next person I’m going to talk to. I need to wait for them to call me in the next two days. And it’s so ambiguous, the timeline, the who, the what, how…how it’s all going to unfold. I felt a little aimless and lonely, I guess would it be, at the end of the day. I remember sitting in that room.
What were the steps for finding an expert?
So it was just feeling a little unknown because it’s a don’t call us, we’ll call you situation. In a couple of days, oncology will reach out and to schedule an appointment with an oncologist that we need to kind of talk through what the next steps are for you.
So again, that was just part of the system, but it’s also you don’t have any control. You’re just waiting, waiting for the system to get back to you. And again, I can’t express this adamantly enough, at least for me in my situation.
I knew I was still catching this what I thought was like super early and that literally days matter, and it felt like a ticking time bomb was potentially still going off inside my body.
– Rich B.
I didn’t have any control over how fast I could get more action to determine if that bomb still exists or not. And if it does, how can we get to solving this problem as quickly as possible? Because we all know early detection, early treatment is the biggest success factor no matter what type of cancer you have.
Did they follow-up within two days?
Yes, they were on it. I think it was less. Honestly, they were all over it. And I had an appointment with oncologist within days.
The Importance of Self-Advocacy
How did you prepare for your appointment with the specialist?
A lot of prep went into that one. This is where, again, I have had the importance of having my sister, and what we had been doing up until that point is we created a Google doc. We called it Rich’s Fight, and I started just layering in all the questions I potentially had for my oncologist.
My sister was doing a great job of the timeline of everything that we’ve discussed and this conversation is documented with actual pictures of what it was before I got diagnosed, after the shave biopsy, after the surgery. She’s got a great documented timeline and this is a thing that I would recommend everybody does and just kind of share with your inner circle and your support group because you’re not thinking of everything. Your head’s not in the right space, and it’s a place where everybody can pile in all the information that you need to know or need to ask. And so there was a lot of that. There was a lot of research being done on the outside in terms of what to expect next, and what the decision tree looked like, and what kind of questions I needed to ask my oncologist. So I felt really well prepared.

The other thing that I learned from my sister, which is really important, is… This sounds bad, but everybody needs to know it:
If you are an informed patient, you will get better treatment.
– Rich B.
If you ask really good questions and you come in as if you know a lot about your situation, your treatment success will increase. And so I always kind of had that mindset of going in and trying to be super articulate and thorough about everything and every interaction from that moment forward.
What did you learn from the Melanoma experts?
So I met with my oncologist, and we went through all of those questions. In the meantime, my sister was able to, through her network, set up an appointment with one of the best melanoma experts here on the West Coast, who happened to be up in San Francisco, which is about an hour, hour and a half drive for me.
So my sister flew out and we met with this doctor, and he spent 90 minutes with me. My sister did a full-body exam again, had all of my data, my biopsies, all of that as fingertips. He did a thorough job of walking through my staging, because he broke down based on no ulceration of your melanoma but the depth and rate of growth, and brought up, hey, there’s this mutation that we should test for.
I didn’t know anything about that. It’s called BRAF. Really important to understand that. And I still don’t know everything. I’m not the expert, but for melanoma, it can be caused by sun damage or it can be caused by mindless cell mutation, not sun damage.
I think the current treatments don’t really factor into… You’ll get the same treatment for that regardless of the origination. It’s still important to know that, and you should ask for that test. Make sure let’s be thorough about our testing so that we have a full understanding of your situation so we can make the right recommendation for your treatment.
Treatment Decisions
Could Identifying the Cause of Melanoma Impact Treatment in the Future?
It could, yeah. I definitely think so. As they continue to advance the medicines, I’m sure it will be a factor.
How did the specialist bring up the possibility of a Clinical Trial?
So kind of towards the end of that conversation, he’s like, look, based on your case, I think you would be a great candidate for a current clinical trial. There’s always clinical trials going on. They come and go. I think he was kind of more attuned to the academic world of melanoma research.
I was so thankful to be able to talk to him and have access to him because I don’t know if the clinical trial would have been put on my plate or not otherwise.
– Rich B.
It probably would not have. It’s nothing like my current oncology treatment support. They just aren’t part of that faction. I realized there’s community oncologists that are there to deliver treatments, and then you have more of the academic side of things where they’re on the cutting edge and have an understanding of the latest and greatest things that are going on. And he just happened to be that.
So within an hour, and this is highly unusual, he took my case to the tumor board at that hospital and presented my case. That started me on the path of wanting to opt in to that clinical trial.

How Did the Specialist Lay Out Your Treatment Options?
So there’s one step in here before getting to that is needing to go get scans to understand if there’s any further spread or detectable spread. And so any path would take you down this road of getting a full-body CT scan. And for me, it was important also to get a brain MRI again, because melanoma tends to want to travel to the brain. So both of those things were recommended.
I got both of those things relatively quickly, even though that’s a little harder, I think. Scans are in such high demand. I had to shop around at local places to get earlier appointments versus something local. I was almost going to drive 3 hours out of town to get something faster if I couldn’t get something within a week. Again, there’s this ticking time bomb situation, and I wanted to get these things knocked out as fast as I possibly could.
Was it a PET scan that you underwent or a CT scan?
It was a PET.
How did you rationalize having to wait for your scans?
I think it’s one of these things where I just had the perspective of there’s a system, I need to advocate for myself, and I’m just going to push and get alternative answers if I don’t like the answer here. Hey, if you can’t get me in in two weeks, is there other places close by that might have some availability, and they’re super happy to help. But you have to ask. It’s not a thing that is top of mind for them to serve up.
If I can drop one piece of advice, it would be don’t just accept the first answer. If it’s not good enough, continue to advocate for yourself. And if you can find something faster, you might be able to do that.
– Rich B.
How did the scans go?
Again, this is like now the third moment of truth, right? You’ve gone like stage zero to stage one, stage one to stage three. Now is this a three or a four situation? And thankfully for my particular situation, all of my scans came back negative. And so that was like, oh, wow. Finally, finally a win. Finally a relief for me and my situation.
I remember just being so, so happy. And those things come back so fast. It’s a little unnerving like that. They do a good jobs, reading all this stuff. I’m sure they did. But as a human being, there’s a lot to look at, and I’m not an expert. Did you double check that? Because it’s like, within hours, okay, it’s negative. It shows up in the portal like before even a physician is going to give you the outcome there.
Deciding Whether to Join Clinical Trial
Rich shares how he learned of clinical trials for his advanced melanoma and walks us through what got him to his final decision of whether to join a clinical trial as his first line treatment.
Making the Decision to Join a Clinical Trial

Did determining your melanoma was stage 3B allow you to look for treatment options outside of the clinical trial?
Exactly. I’ll just kind of combine both conversations with the specialist and the community oncologist, because there’s a lot of commonality. I think this is something that everybody going down this path with melanoma, where the treatments are today are pretty standard and super effective.
We’ll talk about that in a little bit, I’m sure, but everything is kind of guiding us towards immunotherapy these days, which I had never heard of a year ago before starting down this path. And that’s going to be the recommended approach, what they call a baseline treatment arm of a clinical trial. Most clinical trials are going to have that as a treatment arm, plus something extra that they’re trying to test out efficacy.
What was your initial response to joining a clinical trial?
I think even before going into this and clinical trials even became a possibility,
I had this misconception that clinical trials were either you get randomized into like a placebo, which is like no treatment, or you get the miracle medicine and it’s that’s what it is.
– Rich B.
I feel embarrassed to say it, but I think I’m not alone. And I think it’s really important just to put my personal embarrassment out there for others and it’s okay, but that’s not how these things work. You’re going to get treated. And it really is, especially in the melanoma world as it is today. In 2022, you have that immunotherapy as a baseline treatment, and that will be your minimum. If you get randomized into that 50%, you’ll know it going in, and you’ll just be receiving basically the same treatment you would at any other place with your oncologist.
My particular clinical trial was testing out immunotherapy with interleukins, which is basically a little bit more targeted, and it’s all around trying to reduce future recurrence for me. But the treatment arms would be the same most likely if I was even stage four.
What other considerations were there?
A lot of things floating in my head, right? I’m still kind of in somewhat of a relief mode that I’m a stage three B, but I’m trying to figure out what the next year is going to be like.
In my own personal journey for this clinical trial, I would have to be traveling a good three plus hours of commute to be a part of the study. That’s a year’s worth of going to an infusion center with that level of travel commitment, plus probably a ton of extra scans and blood tests and just like beyond what you would normally get, just because there’s a lot more rigor to clinical trials and you’re going to get poked and prodded and scanned a little bit more based on whatever the rigor is for that particular study.

So was figuring out more or less the burden on me to enter this phase, not knowing where I was going to get randomized and whether or not that would be worth the extra potential protection I would get if I got randomized into the arm that had the interleukin portion.
Plus the other factor is I wanted to take my situation and turn it into a positive. And if I could be a part of continued research and giving back, I wanted to try and do that as well. Those were all the things in my head as I was trying to decide what to do.
Clinical Trial Onboarding Process
What was onboarding onto a clinical trial like?
So once I said yes, I had to go up to the facility. That’s a little bit of a commute for me. Sign a ton of paperwork. It probably took a good hour to sign all the documents that were required to sign in terms of just giving them all access to everything, including HIV status.
Basically everything about my medical history would be part of the study, of course. And then I would have to more or less redo all of my scans and blood work because, again, there’s a particular way that each study wants its scans to be done, wants its blood work to be done.
I went and did a full a full day of MRIs, PETs, everything, blood work, just to try to get it all done at once and minimize my trips up there.
– Rich B.
Then it was a wait and see if I got randomized once I kind of did all the pre-work, then you kind of wait and see what the coin flip is going to be, if you’re going to go to baseline treatment or the study treatment.
What were your thoughts when receiving the clinical trial information packet?
It’s a lot as a non-medical professional. A lot of this stuff is just going to go over your head. It can be pretty intimidating. I had my sister here to read through all 50 plus pages multiple times and distilled it down for me and added a little bit to my takeaways.
But more or less, the way it was explained to me by the researchers that were conducting the study, they had a pretty good summary of what it was. So I think they were able to distill. They did a great job of distilling all that 52 pages down to human speak.
Any guidance for those considering joining a clinical trial?
Yeah, I think just if you take a step back, it’s going to be an extra burden on you as a patient in terms of time. Needle pokes, scans, these types of things.
But there’s also a potential benefit, I think, making sure that all of your scans are scrutinized. You’re getting extra blood work. All these things can give you a lot more confidence that if they do find something along the way, they’ll probably catch it sooner than if you’re not on a clinical trial. So there’s a benefit there.
So everything comes with a cost benefit, and you kind of have to factor that into your own journey as well as I think the part about contributing back to future cancer patients and how much that weighs into your decision making.
– Rich B.
There’s no wrong in any of it. I think this is how I was thinking about it.
Did you have to consider anything with payment?
I am so glad you asked this question. I’d actually forgotten about this because there is some language within the clinical trial paperwork that mentioned patient responsibility for things not covered. And I remember asking that specifically to the doctors that were running the clinical trial. And kind of glazed over it, like I wouldn’t worry about that, but it is there in black and white and is a little unnerving and it’s really non-patient-friendly language.
Like you’re putting yourself out there for extra exposure to expensive tests and for having language there that says if your insurance doesn’t cover this, then you have the responsibility because you opted into trying to be helpful. Something to always ask for and read about. But I don’t know if you’re going to get great answers. At the end of the day, I think that’s just where these things are.
Is it unnerving to agree to pay for uncovered costs not really knowing what is or isn’t covered?
Yeah. And it can vary. It varies by every situation, every insurance coverage, doctor, all that stuff. And I remember my sister caught this and said I know it’s in my question doc that we have and I know the language in there. I don’t have to read it. She said this is very un-patient-friendly language. Ask the investigator about this is like one of my top three questions.
The Randomization Process
What was your reaction to being placed in the control arm?
I had already prescribed my decision making that had I got randomized to the non-baseline arm, so like the extra medicine arm, I was going to do it. It was going to be worth the burden for me, and I was doing everything I could possibly do for myself to just improve my survivability. I believed in everything I was reading with the drug combinations and was willing to add the extra inconvenience for myself, but also putting myself out there for probably a greater risk of side effects, which we can get into.
Because that’s the other thing we haven’t talked about with clinical trials is if you’re going into a place, it’s a little bit more unknown as to what to expect and how your body is going to react, because less patients have gone through that.

How did you approach considerations of side effects vs quality of life?
I think this is where everybody’s journeys individual and I can’t tell you how many times I’ve been told how young I am, that I’m 47 and I’m less likely or I’m probably going to be more capable of handling side effects. And I think that’s why I was such a great candidate for a clinical trial. They wanted to run somebody through that was young, as it were, and healthy. Run marathons and all that. That I would probably be able to tolerate side effects.
But you’re exactly right. I was really willing to take on any side effects just because of where I am in my journey. And I was going to do anything I could at any cost to improve survivability was my number one thing.
How did you weigh staying in the study vs what was best for you?
So unfortunately for me, I got randomized into the baseline treatment and at that point I was debating. So I’m going to take the burden of inconvenience and not knowing how I was going to react to even that baseline treatment. Was that going to be worth it for me personally versus… Basically I’m doing this for others? And I think that was at that moment where I was like, I think I need to be selfish here.
I think this extra burden is going to be a little bit too much for me to take on while I am going into the unknown. Like I’ve got a year of treatment in front of me, and I don’t know what that’s going to be like. I can just take all of that extra complication in my life, go back to a baseline treatment that’s closer to home and will fit more into my life, and whatever comes my way, I’ll probably be better able to handle it. So that was the decision-making process for me. I still feel a little guilty for choosing myself, but at the end of the day, I think it was the right choice for me.
Immunotherapy (Opdivo)
Rich shares his experience with his immunotherapy treatment (nivolumab or commercial name Opdivo) for his stage 3B melanoma, as well as side effects.
Treatment Timeline
How did the treatment timeline impact your treatment decision?
There’s another thing that we haven’t discussed here is there’s actually, aside from the internal ticking time that I felt I had that more or less went away with my scans and it kind of put me at stage three B, but there’s also a time window that we’re dealing with post surgery. So there’s a 90-day time window after you’ve gotten surgery that you’re supposed to get on a treatment, whatever that treatment is going to be.
This extra complication with entering a clinical trial, with just managing all of that, really kind of was pushing the limits on me getting my first dose of immunotherapy within the 90-day window. So I was feeling a little anxious about that.
– Rich B.
I was like, Look, I need to make a quick decision. Whatever I get randomized into, I need to make that decision very quickly to get started. Because I got randomized and opted out of the clinical trial, I was kind of back at square one and I needed to kind of reenter the world of the oncology community that was close to where I live to get on schedule and start treatment with my original oncologist, where I started right after surgery.
So it’s a little bit of a panic outreach to like, Hey, Dr. So-and-so, I opted out of a clinical trial. We’re getting close to this 90-day window. Can we meet and start to talk about commencing my treatment plan, which they were very responsive on. They had a level of urgency, thank goodness. And technically, I was just a little outside of the 90-day window when I started, but it was close enough.
Can you tell us more about the 90-day window?
It felt like I was maybe the one managing that the most, because I think once I opted to go into the clinical trials, not a part of that world, but I think they saw, oh, wow, you’re getting close to that. So they hopped all over it.
Treatment & Side-Effects
Can you describe your treatment and its side-effects?
I think there’s two primary different immunotherapies. I won’t go into the other name because I forget it. But they more or less have the same efficacy. And so I think I’ve talked to a number of doctors that are in the world of melanoma, and they say the difference between those two is very negligible. So they’re basically almost the same medicine.
I won’t get hung up on this decision too much. One is delivered every four weeks, and one is delivered every six weeks. But it sounds like there’s really no difference in terms of how effective it is to treat. And so I have chosen the the drug called Opdivo, and I started in late December, got my first infusion.
Basically I go into the infusion center where patients that are on chemotherapy or immunotherapy go into. I walk in, I get an IV set up, and once it’s set up, the drug only takes 30 minutes to get infused. So it’s actually a relatively quick session.
And like I said, it’s every four weeks. So I have 13 total doses that I will get over this year. I have five down, eight to go. I’ll actually finish up the Tuesday before Thanksgiving. So I think Thanksgiving will be a nice, nice holiday. We’ll have finished treatment. That’s the schedule.
Then in and around all those infusions, I get blood drawn the week prior, and then a day or two later I’ll meet with my oncologist to just monitor the blood results. They’re checking to make sure all of my blood cell counts are okay. And specifically for these drugs, they can potentially interfere with the thyroid. And so I’ve got specific blood tests for thyroid that they’re just making sure my thyroid is operating. It doesn’t sound like it’s a big deal. If it’s not, they’ll just put you on medicine. It doesn’t sound like a very serious, serious side effect. It’s something they see pretty commonly. And that’s it. I’m in the middle of that. It’s not just part of the regular routine.
Do you also need a PET Scan every six months and a skin exam every three months?
Correct. Since I haven’t actually done a scan since the clinical trials, I have one scheduled here in the coming weeks with my first six-month date, which I’m not super concerned about, because I know at least with how effective these drugs are, there’s a pretty low probability of recurrence for me in this first year.
I think I’ll be a little bit more nervous about next year when I’m off the treatment, and hopefully my body is in a good place. But I think those scans will be a little bit more tenuous.
– Rich B.
And then, yeah, I’m seeing a dermatologist for a full-body skin exam every three months this first year, and it’ll probably go to every six months in perpetuity. I’ll be seeing a dermatologist for the rest of my life every six months.
What are the side-effect of nivolumab (Opdivo)?
So for me personally, I’m experiencing zero side effects so far, which I’m so thankful for. But I don’t feel like I am an odd case. I feel like most patients, I think at least two thirds, probably go through without any side effects.
If there are side effects, they generally will be like some itchy skin, diarrhea because the immune system might be attacking some of your gut bacteria. But that’s all stuff that can be treated. Those are kind of the most common side effects. There are more severe, but they’re pretty rare.

I make this really bad analogy probably, but you know, I kind of equate immunotherapy to a sniper, it really like programs your body to target very specific cancer cells. And it is so smart versus what I see with chemotherapy, which is more like a shotgun. It’s an onslaught on every part of a patient’s body. And I think that’s the big thing for for the melanoma, folks, that this drug… You can’t equate it to chemotherapy. It’s an entirely different, different treatment.
Key Takeaways
What are your takeaways going through this experience yourself on this shifting landscape?
The word that comes to mind is just grateful. I’m grateful to the science.
– Rich B.
I’ve been told so many times melanoma in 2022 is so much different than even 2012. These therapies and these treatments did not exist back then.
That’s where all those Google searches like survivability curves are based on the 2012. That’s why I said before, don’t look at those. It’s all much, much improved, and I’m just thankful at how advanced the science has become for my specific cancer.
And I want to try to be a part of helping this goodness spread to other cancer treatments. So patients aren’t in a death sentence and can have treatments that are more humane. We should just be grateful that we have treatments, but I think now, seeing where immunotherapies are, hopefully we can get this goodness translated to other types of cancer. Because honestly, aside from going through my routine, most days I forget that I have cancer, that I’m even getting treatment. That is an insane realization I had one day.
I was like, Man, I went through a whole day and I didn’t even realize that I’m a cancer patient. What a blessing that is.
– Rich B.

Is there anything else that you want to share?
Yeah, I think there’s just one moment. We didn’t cover that I want to emphasize, and it was a big moment in my journey. I had gone past my surgery. And it wasn’t until a couple of discussions after having my scans where I confirmed I was in stage four and I had been told I was a stage three B, but not told I was a stage three B in remission. And it wasn’t until I came back to my community oncologist, where he said the words, You’re in remission, that I didn’t know I was in remission.
How big of a deal is that? Anybody that has gone down this road hopes for that day to hear those words. And even though I was like early on and my journey has been short. I caught it early. I was in that kind of unknown state. And I just wish those words had been uttered a bit earlier.
Why is it so critical to let a patient know that they are in remission?
I don’t know the exact technical term of remission, but I’ll translate it for how I would define it. You’re at a point where there’s no detectable cancer in or around your body. And if you’ve had cancer in your

Inspired by Rich’s Story?
Share your story too!
Skin Cancer Stories
Tara S., Melanoma, Stage 1B
Symptom: Mole on back that became thicker and changed color
Treatments: Surgeries (wide local excision, sentinel lymph node biopsy)
...
Brittanny G., Skin Cancer (Melanoma), Stage 3A
Symptoms: Mole that enlarged, changed shape, and became dry, patchy, and flaky, fatigue
Treatments: Surgeries (wide local excision, lymphadenectomy), immunotherapy
...
Teresa B., Recurrent Breast Cancer (Hormone-Positive), Oral Cancer (Lip Cancer), and Skin Cancer (Melanoma)
Symptoms: Lip cancer: chapped lips & a pimple-like growth on lip, breast cancer: enlarged left breast with lump, melanoma: none
Treatments: Surgeries (bilateral mastectomy with reconstruction, lumpectomy, craniotomy, Mohs, surgery, wide local excision), hormone therapy, radiation therapy
...
Jennifer M., Melanoma, Stage 4 (Metastatic)
Symptom: Persistent cough, body and chest aches and pains, night sweats, fatigue
Treatments: Immunotherapy, surgeries (lung resection, pericardiectomy)
...
Cheyenne E., Melanoma, Stage 3B
Symptom: Itchy mole on her back that changed in appearance
Treatments: Surgeries (wide local excision, sentinel lymph node biopsy, lymph node removal), immunotherapy
...
Robin A., Melanoma, Stage 4
Symptom: Appearance of a small bump on the chest
Treatments: Chemotherapy and immunotherapy (under a clinical trial)
...