Nicole’s Stage 3 Undifferentiated Pleomorphic Sarcoma Story
Nicole shares her stage 3 sarcoma story, a soft tissue subtype known as undifferentiated pleomorphic sarcoma (UPS), and undergoing chemotherapy and a Whipple surgery.
In her story, Nicole also dives into navigating life after her cancer diagnosis, from dealing with hair loss, the impact on her marriage, how to ask for help, and transitioning to survivorship. Thanks for sharing your story, Nicole!

- Name: Nicole B.
- Diagnosis:
- Soft tissue sarcoma
- Undifferentiated Pleomorphic Sarcoma (UPS)
- Staging:
- 3
- 1st symptoms:
- Inability to tolerate food
- Treatment
- Gallbladder removal surgery (Cholecystectomy)
- Chemotherapy
- Gemcitabine: 1.5=hour dose, once a week for two weeks in a row, one week off
- Taxotere: 1 hour dose, once every 3 weeks.
- Whipple surgery
You are absolutely beautiful, and you will have everything you need to fight this.
Continue one day at a time. Sometimes it will be one hour at a time, but you are doing an amazing job, and we believe in you. We love you. You have got this.
Nicole B.

- Diagnosis
- What were your first symptoms?
- After years of this, what got you to go to the doctor's?
- Were there symptoms from your tumor itself?
- What happened the first time you went to the doctor?
- How did the doctor diagnose your cancer?
- Describe the HIDA scan
- Learning about the failing gallbladder
- Results of the gallbladder surgery
- Waiting for the pathology results
- Unexpected cancer diagnosis
- Processing the diagnosis
- How did your husband react to the diagnosis?
- How did you approach breaking the news to loved ones?
- Treatment Decisions
- Did you get a second opinion?
- Introducing the Whipple surgery
- What was the subtype of sarcoma?
- What was meeting with your medical team like?
- What was your attitude towards your medical team?
- How do you suggest other patients prepare for initial hospital visits?
- How did you handle treatment options that made you uncomfortable?
- Chemotherapy
- Describe your chemo regimen
- Getting a central venous catheter
- When did you get hit by the worst side effects?
- List of side effects & what helped them
- What do you wish your doctors had told you about chemo beforehand?
- Did you do fertility treatments?
- Any changes to physical ability post-chemo?
- Did you go through radiation?
- Hair Loss
- Whipple Surgery and Recovery
- Survivorship
- How did going into remission affect your outlook and lifestyle?
- What's your advice to someone moving forward as a survivor?
- How did your cancer experience affect your relationship?
- How important is it for people to find their cancer community?
- Guidance on asking others for help
- Do you have anything else you want to say to someone going through this?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
My story is unique in the way that I was alerted. It really goes back a few years. I had just gotten married to my husband. After our wedding, I started having all these issues tolerating food.
We could not figure out what was going on with me. I had colonoscopies; I had my gallbladder and other organs tested. We tried every diet on planet Earth to try to figure out what we could do to help with these symptoms I was having. Nothing I was changing about my diet was helping.
I honestly had given up on it and was like, “It does not matter. I am going to be sick anyway.” I ate whatever I wanted. I was falling into a depression. We still had amazing memories and great times, but it was still depressing going through that because I was sick with every single meal.
After years of this, what got you to go to the doctor’s?
In June 2017, we had a barbecue at our house and with Wes’ family because my family had just moved down to Houston, Texas. I was bumming about that, so we had a big barbecue. It was an amazing time, but as usual, I was expecting I was not going to tolerate food.
That was not anything out of the normal for the last few years, but it was bad. When I went to go to sleep, I immediately sat back up because I felt like I was going to throw up. Usually whenever you sit up, you get relief from something like that, but unfortunately, I did not.
I hovered over the toilet for 20 minutes until it finally settled down. When I went to go back to sleep, the entire thing happened again. Something was wrong. I was crying. I could not lie down at all.
The next day, I could not eat anything. I could not eat; I could not sleep. I was just exhausted. I felt so sick. I had to be seen immediately.
Were there symptoms from your tumor itself?
Sarcoma is not like a thyroid cancer or testicular cancer, where you know the origination points. Sarcoma starts anywhere.
It can manifest in the bones, in the soft tissue, or with the fatty tissue outside of the pancreas in my case. It shows up anywhere.
Some people will find a lump on their arm. I met a person who had it wrapped around the cartilage right by his eye. It was so deep within me, and it had reached the maximum point before it was going to metastasize. It had stayed in that one spot at that stage 3.
What happened the first time you went to the doctor?
My doctor was out, and they had another guy who was half-retired – only working 1.5 days a week. He took me under his wing, and he started ordering some more of the same tests I had already had.
Through having those tests, he did an ultrasound, and he said, “We did not see anything wrong with your gallbladder, but there was something nearby. It is round. I do not know what it is. It is probably nothing, but I do want to order further testing.”

How did the doctor diagnose your cancer?
We moved from an ultrasound to a CT scan, and I received a phone call after the CT scan. He said, “Nicole, I am never going to forget getting the results for your CT scan. I was at home on my couch, obviously only working 1.5 days a week, and it said negative.”
Meaning they found nothing at all. Not even this round thing they saw on the ultrasound. He said he felt God move him to call the radiologist personally.
I am not even his patient. I have only been seeing him for a couple of weeks. He calls the radiologist and says, “I m so sorry. Would you please just look at Nicole’s scans again?”
She went and got back to the phone. She says, “Oh my gosh, I cannot believe I missed it. I think that she might have cancer.” He calls me and tells me that they think that there is a possibility that I have cancer.
The radiologist, the doctor — no one has seen this before. They do not know what it is, but the way that it is reflecting on the CT scan looks suspicious, so we needed to see a surgeon the next day.
Describe the HIDA scan
The doctor ordered a series of tests. He did one test I had never had before, called the HIDA scan. It is a nuclear medicine test that tests the excretion rate of your gallbladder, something that I had never done before.
They put a tracer in your arm, let it drop in your gallbladder, and then they inject an enzyme that causes your gallbladder to squeeze for a half an hour.
Learning about the failing gallbladder
After that test, we found out that my gallbladder had been failing. It was only operating at 25% of what it should have been. It was nothing that would have showed up on a CT scan or on an ultrasound. It had been three years of suffering to find out that it was my gallbladder the whole time.
He said, “We cannot access this lesion because of its location. What I am going to do is for the less-than-1% chance that it’s even cancer. I am going to remove your gallbladder, and then I will remove this tumor-type thing we are seeing there.”
Results of the gallbladder surgery
July 6th is when I went into have my gallbladder removed. When I wake up, he says, “We successfully removed your gallbladder. However, the tumor is resting against your pancreas, so we could not remove all of it. I removed part of it. We are sending it to pathology. I am not worried about it.”
Waiting for the pathology results
It was difficult. It tested me in a way that I had never been tested before. I am a planner and an organizer. I have a paper planner that I write everything down in. I have stuff planned out through October of this year already with things going on.
I love to plan; I get excited about that. It is something that is a passion of mine. Realizing I could not control it? We called three times a day, every day, during that time period to see if anything had come back. But nothing. “Nope, not yet. Sorry.”
It was a huge testing of my faith. Learning, “Hey, there are some things you cannot control in life.” Where do you find peace? Where do you go to for peace in that?
That is another part where my faith came in so strong because there was a lot of time of prayer and talking with family and friends and trusting that God had a plan for my life. A big part of learning to trust and learning to find peace in an area that has not been peaceful.
I am also in excruciating pain from my first surgery, trying to recover and trying to heal. I am asking, “What are these results going to say?”
It was a whirlwind of emotions. It was interesting because even though they had said there was this very low chance that it was cancer, you just cannot help but go there sometimes.
“And what does that mean for my life if it is?” I had to sit back and say, “Okay, I cannot live in this world of what if because I am trying to live my life now and recover and still find joy and laugh.”
»MORE: Patients describe dealing with scanxiety and waiting for results

You hope in those moments that you worried for nothing. If it turns out to be one of the potentially worst-case scenario options, what are you going to do with that? It was all these different scenarios coming my way.
I knew that no matter what happened, I did not want to waste this. I wanted to find a way to live with abounding faith. I wanted to find purpose. I wanted to love other people, and I wanted to grow.
It made me realize that life is so short. Even before I was diagnosed with cancer, I realized at 27 years old that life is so short. It really got my wheels turning for a number of days.
What was I going to do with that? It was horrifying but freeing, and it woke me up. It was this balance of redirection of purpose and making the most of things. There was so much amidst the thoughts that I was having of what would happen next.

Unexpected cancer diagnosis
I go home to recover. 12 days later, on July 18th, I go to have my drain removed out of my side, and as he is pulling the drain out, he tells me, “I am so sorry to share this with you, but you have been diagnosed with stage 3 sarcoma cancer the size of a racquetball, and it is angry, aggressive, and high grade.”
Processing the diagnosis
It was the most awestruck that I have ever been. I couldn’t believe that I had been diagnosed with cancer. How do you tell everyone that you love that you’re diagnosed?
I immediately turned to prayer and got my game face on that I was going to fight for my life and do everything I could to beat it.
I remember I said, “Can you repeat the word ‘sarcoma?’” I had never heard it before. I couldn’t even pronounce the name of the cancer I had just been diagnosed with. I went down the hall, and I walked back and forth.
I was like, “We got this. We can do this. We are going to fight as hard as we can. I am a Christian, and I believe that God has a plan for my life. Whatever that looks like, we are going to fight this.”
There is something that happens when you hear the words “you have cancer” that you cannot describe. The word “cancer” had always been defined as something that someone else had until that point. It was like taking a word that I knew and redefining it as it now pertained to me.
That was huge. Trying to wrap my head around the fact that there was something inside of me trying to kill me. That was so bizarre.
You never think it is going to happen to you. Not in an arrogant way. It has always been something that someone else had until this point.
»MORE: Patients share how they processed a cancer diagnosis
How did your husband react to the diagnosis?
My husband is the most amazing human being I’ve ever met in my entire life. He said, “I do not care what we have to do. I am coming with you.”
He left his job, sold his truck, left our house, left his entire family here, and we packed up the car and moved down to Texas temporarily. We lived with my parents so I could receive treatment at MD Anderson.

How did you approach breaking the news to loved ones?
It was so hard because we had taken everybody on a roller coaster already with us with. It was this up and down leading to this final diagnosis.
I was saying, “I really hate to tell you this news, but it is cancer, and it is called sarcoma. It is at stage 3, and I am going to need this major procedure.” I know that as I was saying that, they are on their phones Googling sarcoma, and you do not see good results from that.
People were looking to see how I was going to react to this diagnosis. I told them, ‘I do not know what is next. It is scary, but I promise you I am going to fight every single day as hard as I can. I am going to do whatever it takes to be here and try to stay upbeat.’
People bounced off that. Everybody reacted differently, and that was a huge lesson, too. It was amazing that I felt like I had people I could call. I felt so grateful for the people that surrounded me, that wanted to know, that cared about me enough.
You really get to see in the mundane of the day to day going by and see people dive into a really difficult situation saying, “I am here. What do you need? I love you. I am with you. I am praying for you.”
I got to see friends and family and strangers in a whole new light of love and what life is all about. It was so hard making those phone calls. Especially when everyone’s on the up and up saying, “Oh, it is probably not cancer,” down to, “It is an aggressive type of cancer I need immediate surgery on.”
But we were ready. We were ready to fight, and I felt like everyone was. It made me feel thankful to be surrounded by such amazing people to take this on with.
It was a big piece of my journey — finding reasons to smile and seeing little things here and there. This half-retired doctor who does not even know me feels a stirring in his heart to call.
That was amazing in and of itself. Then to have the radiologist look again. Then my parents moving at the time that they did. There were so many things leading up to this. I felt very cared for, and in a weird way, it was poetic.
I do not ever want anybody to think cancer is a good thing. I do not think cancer is a good thing. I think it is terrible. I think that God can do incredible things through cancer.
I think we can grow in incredible ways during struggle in general, and that was something that happened to me. It changed my life.
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
Did you get a second opinion?
They had sent my tumor to MD Anderson to confirm with them that it was sarcoma because it is so rare. The MD Anderson Cancer Center has been rated the number-one cancer hospital in the world, and they have an entire sarcoma department dedicated for my type of cancer.
I felt very confident with the placement of everything with my parents moving there. I felt so confident that that was where we needed to be. There were only 44 sarcoma oncologists in the country at that time, and a big chunk of them were in Houston.
In terms of the diagnosis and symptoms, after my first week of appointments at MD Anderson, I spoke to them about my cancer. It was about the size of a racquetball on my pancreas, and they said the way that sarcoma is, it would not have caused any of these symptoms. The only thing that warned me it was there was discovering that my gallbladder was failing at just the right time.
They said by the time I would have seen it, it would have metastasized throughout my whole body. At least up into my lungs. I did not have any symptoms from my tumor at that point.
That was a miracle — suffering for three years of anguish every day to find the cancer at just the right time to give me a fighting chance to live.
Introducing the Whipple surgery
The diagnosis happened, and then he said the procedure that you are going to need is called the Whipple procedure. It is a four- to six-hour surgery. Open surgery of the abdomen, about a nine-inch incision down the abdomen.
They remove your gallbladder, a portion of the small intestine, the head of the pancreas. For me, they were going to remove part of my stomach and part of my colon along with the cancer.
It would be a major surgery, full reroute of the intestines. There is a percentage of people who do not make it out of the operating room. If you do, it is certain to be life changing.
My surgeon sat down and said, “With the rarity of your cancer and the complexity of the surgery, there are very few places that I know, that I can count on one hand, that would treat sarcoma and be specialized in the Whipple procedure.
“The place I would recommend that you go is MD Anderson Cancer Center, located in Houston,” where my parents had just moved in the weeks prior to all this happening.
What was the subtype of sarcoma?
Undifferentiated pleomorphic sarcoma, also called UPS. Within the 70 different subtypes of sarcoma, there are different categories that they test for when they do pathology. In a UPS patient, none of them are dominating. It shows properties of all of them. It is in its own category. Mine did not show enough properties of any type of the subtypes to be classified.
It is altogether very rare, so we were very thankful to be at a high-volume clinic that knew how to treat that.

What was meeting with your medical team like?
Between all the testing, the scans, and everything, the first week was probably the most overwhelming week of my life. There were just so many things that happened, blood work, fertility tests — it was crazy.
We were having to go into my wrist because everything that was happening was blowing out my veins. I had multiple tests to gauge where my baseline was going to be. When I met with my team, they were the most kind, uplifting, and incredible people.
They stayed in the room and answered every question I had without making me feel rushed. I had a list of questions out to ask them because I did not know anything. I did not know what to expect at all, and they were very, very kind. They were amazing at what they were doing. It was incredible to have such an amazing care team.
What was your attitude towards your medical team?
They are here to help you and to try to get you better, and you are important; you’re an urgent case for them. I think that brought me peace. They are trained to do what they’re doing.
Being able to put that into their hands was an amazing thing. There is a reason for all the tests, and you are going to talk about them.
How do you suggest other patients prepare for initial hospital visits?
If it is at all possible, go with someone. There are so many emotions that come with it because you are a patient. Go with somebody and have a journal.
Have somebody take notes; have questions written out beforehand to ask your doctors and your oncologist. Take notes on things because you are going to hear things differently. You will miss things; you will hear things that the other person does not hear.
Maybe even ask them if you can record what’s going on. There are so many things that go on, especially in that first week. You just want to have an idea of what’s going on. I would say that is probably the first thing.
And remember that this is what these doctors and medical teams do every single day. I think that that kind of brought me peace. You feel like the world has stopped moving, but it has not. There so many other people there that are being looked at and treated and diagnosed. This is what these people do all day, every day.
How did you handle treatment options that made you uncomfortable?
If something does not feel right, ask questions. If there is something that you are uncomfortable with, see if there is another option. For example, I had developed a blood clot, and they wanted me to do the injections in my stomach.
I am horrible with needles, so my husband went up and advocated for me. We were able to get moved to a blood pressure pill or a blood clot pill to take instead.
You do not have to take the first thing as the only way. Even if that is their routine way, they might be able to find another way. No question is off limits. You can ask any question. The worst they can say is no. They are not going to laugh at you. They understand that this has not been our world up until this point.
Chemotherapy
Describe your chemo regimen
I started chemotherapy. I had two medications, gemcitabine and a combination of gemcitabine and Taxotere. I would have gemcitabine on week one. It was a 1.5-hour dose.
A week later, I would have another dose of gemcitabine and an hour of Taxotere. Taxotere was my aggressive chemo, and it caused the majority of the side effects — the hair loss, nausea, all these different things.
Getting a central venous catheter
I had a CVC, a central venous catheter, put in my chest. That developed a blood clot in my right jugular vein during the first cycle of chemo. It was the beginning of launching into chemotherapy before the Whipple procedure happened.
It is different from the port. CVC, the line goes in, but it’s on the outside. It looks like this little bat wing that’s on the outside, and there are two dangly lines hanging down.
They have to be covered and have dressings over them. Every time you take a shower, you have to cover it.
I was awake when I had that put in. If anybody is getting this, I highly recommend asking to be put down on the anesthesia, even if it’s an extra cost. Being awake was probably one of the most difficult things during the process. That was very painful and very scary to have that put in my chest while I was awake.
The port, on the other hand, is surgically done. It’s underneath your skin. They inject a needle in every time to access it.
CVC is on the outside so they can hook it up for blood work. They are able to hook it up for chemo. We named mine Carl. You have to make it fun because it is what it is. So, it was Carl. Carl was my CVC line.
They also do PICC lines, and some people have them in their arms. I wanted mine in my chest just because I don’t like needles at all. It was better for me in my chest since I could put on a shirt and cover it up.
There are multiple different ways for chemo administration. I appreciate that because you do not want to blow out your veins by having so much medication pumping through them so often.

When did you get hit by the worst side effects?
For my cycle, in week two, I had the double infusion. Week two was always my hardest week. The side effects always amplified when I was getting both medications. I experienced mouth sores, nausea, and loss of taste.
Week three was a rest week. I had no administration of medication then, but I did have blood work done. In week three, they wanted to make sure it was okay to start the next cycle.
List of side effects & what helped them
Summary: joint pain, loss of taste, chemo brain, blood clot, nausea, thrush, folliculitis, mouth sores (mucositis), fatigue
Nausea
I took anti-nausea medication. I cannot remember the name of that. I also took what are called “queasy drops.” We got those on Amazon after my boss had sent them to me. I used those all the time. They had some pretty good flavors, and it kind of helped with the nausea, so those are probably the best things. Week two was the worst with nausea, but I was pretty much nauseated around the clock.
Thrush
Thrush usually happens in babies, but it can happen with chemo administration. My entire mouth was gray, and my tongue looked like it was wrinkled. It was a thick mucus throughout, and there was a throbbing pressure with it. I had a liquid medication for that, but I don’t remember the name of it.
Folliculitis
Folliculitis is an intense acne breakout, and I broke out all over my neck and my face. I have scarring from it. Every second week, I would completely break out in acne. I did not really do anything for it. I was in so much pain in other areas that it was almost a nonissue.
Mouth Sores
They had mouth rinse that helped. It was called Magic Mouth Rinse. But then I would get really nauseated with that, so I would only take it if I was in a lot of pain, but the sores would come and go as the weeks went on.
The mouth sores weren’t bad enough on their own. It was a combination of those and the thrush. The thrush was tough because it affected my tongue, too, so my whole mouth was gray. It was thick, and I wasn’t hungry, and it was so uncomfortable. I would try to eat softer foods. Smoothies were really nice.

Fatigue & Weakness
After every chemo, it felt like I had a cinder block like sitting on my chest. It was exhausting. It did not matter what I did. It is different than being tired. Tired is quenched by sleep.
Sometimes I would sleep for 16 hours. When I would wake up, it still felt like I had been up for three days. My eyes were so tender to the touch. It felt like somebody had punched me in the face.
It was hard to think. I was tired and exhausted, especially on my week two double dose. I was very exhausted. We would play card games, and in the middle of a game, I would have to say, “I’m going to bed right now,” because I could not keep my body up anymore. Even though sleep did not quench it, I was not having to use as much energy by lying down.
Lying down was something that I did a lot that helped. I had an online journal on my phone, and I journaled every day during treatment. I was able to type lying in bed if I could not sleep. I would type on my phone, sharing a little bit about what had happened that day, side effects that I went through, experiences that I had, and emotions that I was feeling.
Joint Pain
Joint pain was really bad after I had Neulasta injections done. I had that after every second cycle. That pulled white blood cells from the long bones to try to keep your white blood cell count up. It caused full-body joint pain. It was so bad one time that I went to the ER for it.
The joint pain was excruciating. The one time that I went to the ER, they put me on morphine, which was an instant relief, but morphine makes me sick. I threw up, but getting rid of the pain for a little while helped a lot.
Loss of Taste
I completely lost my taste almost through the entire cycle. I would get it back one or two days at the end of the third week, but I would lose it again. I would eat bread with mustard because I wasn’t very hungry. It was nice because the bread was soft, and I could taste mustard. I could taste olives for whatever reason.
It was helpful to be reminded there are still taste buds in there. It took me about three or four weeks after chemo was done for my taste to come completely back. I could not taste very much, but mustard and olives I could.
I would repeat myself or be unable to recollect things — not only short term but long term, too. I remember my mom bringing up memories we had, and I just could not get there.
In the game UNO, there was a green 8 that was laid down. I would see it, look at my hand, and by the time I looked back I forgot what was down. I was struggling trying to process information in front of me. It was hard to even think straight trying to get through a game.
I encourage trying to play games, though. Do not get frustrated with yourself but try to engage your mind when you can or when you feel well enough. Try to keep yourself on your toes a little bit. We played a lot of board games and cards during treatment.
Blood Clot
I took Xarelto every day for that, and the blood clot dissolved quickly. Within two months of getting the clot, it had dissolved. My doctors still wanted me to take it for at least six months. I would bleed out of my CVC, so I had to get that dressed often. My husband trained to do it, so we could do it at home. Other times I would go in.
What do you wish your doctors had told you about chemo beforehand?
They gave us a giant book of stuff to go through. We had a chemo class, which I was thankful for. They gave us so much information. One thing, though, is you have to keep going. You are going to be amazed at how far you go. I cannot believe that I made it to the next day every day.
Did you do fertility treatments?
There was no time. They said, “We have to get you on chemo now. The size and location of the tumor demand we get started.”
We did not have time to freeze any eggs or anything. We did find out that I lost 75% of my follicles. It did not look good for us to have kids biologically. I am not supposed to get pregnant in the first two years anyway.
We have already watched a miracle happen, so whatever is meant to be, we will find a way. My mom was adopted, so if we are led down the path of adoption, that would be such a blessing.

Any changes to physical ability post-chemo?
I am not able to do some things I could before, especially with restrictions on my spine. Like a flightless bird, I am going to be the most boss ostrich on Earth. I might not be able to fly, but I am going to do what I can on the ground.
Finding ways to redirect your purpose and live your life to the fullest is so important. If that involves children, we are going to go for it. If not, okay. I am taking it all as it comes.
Did you go through radiation?
At the end of my fourth cycle, they found that I was no longer responding to chemo. My tumor was no longer shrinking. It had shrunk after the first two rounds, but after the second two rounds, it was staying the same.
Initially, they thought about trying to up the chemo dose, but my liver levels had spiked up so high. My AST and ALT were five or six times higher than what they are supposed to be. I almost had permanent liver damage from the chemo.
They wanted to move on into radiation therapy, but they opted out of that because of the location. It was two weeks from then that they had scheduled the Whipple surgery for me.
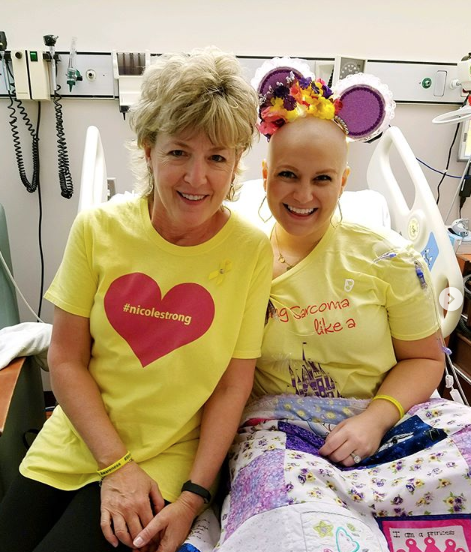
Hair Loss
How did you deal emotionally with your hair falling out?
I talked with other people in the hospital during my first week or two after I knew I was going to need chemo. I decided that I was going to shave it.
Everyone is going to choose what works for them, but I had talked to too many people who had traumatizing experiences. They would sit up and find a clump of hair on their pillow. I had long blonde hair. I did not want to have to watch that.
Having something that I held onto so tightly and letting go of it was so rewarding. I realized I had been hiding behind my hair because I gained so much weight in those first three years from a gallbladder issue.
Then I saw beauty in myself, not for how I looked or my hair, but who I was in God and how I was created.

It is kind of fun now. I never thought I would say, ‘Hey, honey, pass the hair gel.’ There we are, though, another bonding moment. I try to make the most of it because my hair was always going to go. I could either sit and sulk about it, or I could find things to be joyful about.
The circumstance was the same. If I was going to sit and pout, it was not going to change the fact that I was going to lose my hair or that I had cancer.
»MORE: Patients describe dealing with hair loss during cancer treatment
Did you wear wigs after you shaved your head?
I bought wigs, and I only wore each once once because it was so hot. I wore caps out in the sun to protect my head. I would wear caps a lot around my dad. My dad had a really hard time seeing me bald because I am such a daddy’s girl.
That was something that he wanted me to do, and I wanted to respect that. I wore caps a lot of times around him, just a little tie cap that they provided at MD Anderson for us.
I love being bald. It is so funny because now we use all the wigs we bought. We volunteer at children’s hospital once a month. We dress up as characters and go visit the kids. I have a long wig, and I dress up as Belle. It all came full circle because of the cancer.
Whipple Surgery and Recovery
What were the preparations for the Whipple procedure?
We planned on being in Houston for two months, long enough to have the procedure and recover. Then they said, “Actually, in order to give you a better chance to survive, you will need to have chemo first.” We thought we were going to be down for two months. We are in the middle of summer in Houston, Texas, where it is very hot and humid.
All we brought were sweatpants and button up stuff because we were just preparing for me to recover from surgery. But they wanted me to do chemotherapy first. I was scheduled for six rounds of chemotherapy at three weeks apiece, so it was going to be a total of 18 weeks, radiation afterward, and then the procedure.
No need for Whipple procedure
I went in on December 13th to have the four- to six-hour procedure done. When I woke up, my husband said that I was cancer-free and had only been back there for two hours.
He said they went in to remove the cancer and start the procedure, but they could not find cancer anywhere. They looked at the scan from two weeks prior. They were talking amongst one another. They moved everything around to try to see if the cancer had moved.
We talked to the radiologist, my oncologist, everyone. They could not find the cancer. Then they said there was no need to do the Whipple procedure.
They took a sample of the area of where it was supposed to be, where it just showed up on the scan, and they closed me back up. Then there I was. That pathology came back as benign. I have gone back every three months since then, and I have been cancer-free.
What was the surgery recovery like?
I got out of the hospital four days after my surgery. It was very painful. It is an open surgery, so it went all the way through my abdomen, nine inches down my stomach, and it broke open later. I have a very thick scar down my stomach.
I did physical therapy. I went to counseling with what’s called a psycho-oncologist. She specializes in counseling people who have gone through cancer, are going through cancer, or survivorship. I cannot recommend that enough.
Physical therapy
After surgery, I could not sit up or lie down on my own, so I went to physical therapy for that. I slept on a recliner for months. I’m still on long-term disability, even having been 16 months out of surgery, because of back problems.
The chemotherapy caused deterioration in my spine, so I have degenerative changes in my spine and bulging disks. I am still in physical therapy, continuing to work on strengthening my core. I am trying to manage the pain that way. I try to go on walks. I try to do Pilates one or two times a week.
Mental recovery
It is difficult in survivorship. It is a different type of challenge — between survivor’s guilt and trying to submerge yourself back into the world you were in before.
There are a lot of things like that, but I recommend physical therapy. I recommend a psycho-oncologist as a counselor to talk you through those things or to just even voice your thoughts.

No explanation for no evidence of disease (NED)
It was a complete miracle. They could not explain it. They still say they laugh every time I come in the room because they do not know what to do with me. That has never happened before with the Whipple procedure.
I have a nine-inch incision in my abdomen. I think what makes that so cool is that validates that this was definitely a miracle is. You do not cut somebody open like that if there is no cancer in there.
It was an amazing mix of emotions. I had gone through such excitement. I was in awe. I was in pain. I was doubting that this really was a miracle that had happened.
I was also overcome with sadness, too, because here I am, and I just had to see all these people around me who were battling cancer and not cancer-free.
It is the only time in my entire journey I asked, “Why me?” I did not ever think that I was above having cancer. We all struggle with things, and we all face hard times, but I was left asking, “Why do I get to live?” I had to turn that question into, “What am I going to do with it?”
Survivorship
How did going into remission affect your outlook and lifestyle?
It was incredible to be part of an experience like that. I am so thankful for my team and to be here today. It changed everything. I changed my diet, everything that I do.
I have lost 90 pounds and my husband has lost 45 pounds because we want to take care of our bodies.
It made me want to invest in relationships and in life. We went to D.C. to lobby for the One Voice Against Cancer, and we are meeting with members of Congress to talk about cancer research and funding. It has been amazing being able to connect with people. I feel like God has redirected my life.
I am so thankful to be able to share my stories. There is life ahead of you during treatment, after treatment.
I used to sit on the couch when my husband got home from work and only be able to say “Hey, babe.” It was nice enough, but I could not get up off the couch. Now, I hear the garage door open, and I am waiting in the garage ready to give him a hug.
What’s your advice to someone moving forward as a survivor?
Continue to advocate for yourself. If something feels wrong, go see your doctor. It is a balance of not obsessing and not being lackadaisical.
It takes some time. Just have grace.
No one picks up a golf club and magically becomes a professional golfer. It takes some time to learn this new post-cancer lifestyle. You will get there. That is why things like The Patient Story exist. I started a social media page, and I have met and connected with people who had struggled with things like I do now, like infertility after chemo, back issues.
We are all here for each other. Using that for good, reaching out to one another, has been a huge part in the post-surgery, post-cancer life for me.

How did your cancer experience affect your relationship?
You have to love every moment you get together, because even though there are hard times, patience with one another is so important. It is important to keep making memories.
Some of the most romantic and sweet moments that I never knew I could experience in my life happened through this cancer journey. I watched him live out his vows.
For people who are not married, it is something to think about. When somebody says, “For better or for worse, in sickness and in health,” they are making a promise to an unknown future. I have a love and loyalty towards him that I never thought that it could even be possible.
We were in Disneyland on Star Wars Day, and we got buttons that say, “I love you,” and, “I know.” I am going to wear the one that says, “I know,” not because I am arrogant, but because I know he does.
He showed me and still shows me. He is the most amazing man I have ever met. I love him so much. Even if it was just sitting next to me or him sitting behind me and rubbing my back that was covered in acne, he showed me love and loyalty.
Even if you are a patient going through it, you still have so much to offer your spouse, too. I remember he was so tired when I was going through chemo treatment. One time, he crawled up in the hospital bed, and he fell asleep on my chest. Knowing that I was needed and I could be a safe place for him, too, was one of the most beautiful moments I have ever experienced in my life.
Forgive quickly, because there are going to be moments that are just hard. You are exhausted. Love with all of your heart for the days that you have, whether it’s 80 years or eight days. Make the most out of every day, knowing the beautiful relationship that you have ahead. We do not have kids, but love your kids and be there for your kids. Know they are fighting for you, too.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
How important is it for people to find their cancer community?
It is incredibly important. I went to a cancer retreat in California for young adult Christian women last summer. It is amazing to be able to connect on so many different levels with people who can truly relate to you.
We always laughed about press and seal. I can never look at press and seal the same. Somebody who has not gone through treatment looks at that as a kitchen item. For me, it was a covering item for my CVC for months while I would take showers.
Being able to talk about going through side effects, blood clots, treatments, hair loss, and what it feels like to persevere is vital.
It is important to connect with one another and to seek wisdom from people who have gone through it before or be encouraged by people who are going through the same thing and to pray for each other.
»MORE: Join other patients and caregivers on The Patient Story Instagram

Guidance on asking others for help
You will need help. We picked up and moved. I would have never set up anything for myself, but we had friends set up a YouCaring page, which is like a GoFundMe page. It was amazing watching friends step up like that and seeing how many people love you in different ways.
I had pen pals. People wanted to make meals. My mentor bought an air-conditioning [unit] for us because we did not have air conditioning in our old house.
It is often a blessing for someone when you allow them to bless you. In turn, you get to see how much it meant to you. You go through this experience, and you realize how much you want to help other people.
That is why we started volunteering at a children’s hospital. People came and sang Christmas carols to us when we were in post-surgery. I told my husband, “As soon as we get out of this and I’m healthy enough, I want to do this because it meant so much that somebody wanted to come to my door and sing to me.”
There is no shame in asking for help. We need one another. That is why we are in community. That is why we have friendships.
Whether that be on social media, in person or support groups, and retreats, I cannot encourage people enough to get involved with the cancer community.
When you ask for help from friends and family, think of it this way: You have somebody who gets diagnosed. Don’t you want to help them? Well, of course, you do. They want to help you, too, and it is okay to accept help from other people.
»MORE: What kind of support cancer patients say helped the most

Do you have anything else you want to say to someone going through this?
You are absolutely beautiful, and you will have everything you need to fight this. We are here cheering for you. I am praying for our cancer community every single day.
You do not even know it yet, but you are in my prayers, and we just became a family. It is a club that no one signs up to join, but once you join, you are automatically family. I will be here as a resource if I can help with anything.
Continue one day at a time. Sometimes it will be one hour at a time, but you are doing an amazing job, and we believe in you. We love you. You have got this.

Inspired by Nicole's story?
Share your story, too!
Undifferentiated Pleomorphic Sarcoma Stories
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Symptoms: Tightness and lump in left breast
Treatments: Chemotherapy, radiation, surgery
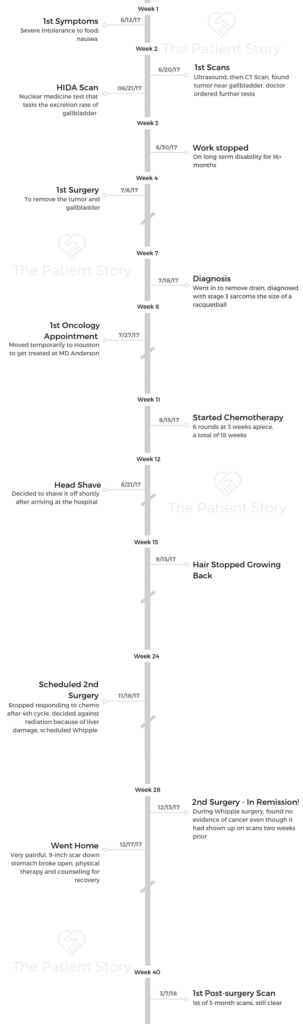
Nicole B., Undifferentiated Pleomorphic Sarcoma, Stage 3
Symptoms: Severe intolerance to food, nausea
Treatments: Surgeries (cholecystectomy, Whipple), chemotherapy (Gemcitabine and Taxotere)


2 replies on “Nicole’s Stage 3 Undifferentiated Pleomorphic Sarcoma Story”
What an awesome story! I couldn’t stop reading it especially since my younger brother is a patient at the same Sarcoma Ctr at MDACC. He had surgery April of 2019 & is CT checked every 3 months. Even though his surgeon disclosed post surgery that he could not say with certainty that the tumor had been removed in its entirety, to date, all of his check-ups have shown no recurrence. He is a man of God and affirms that the Lord is sovereign and knows the plans He has for him. Nicole, you are an inspiration. Indeed, God has been by your side during your difficult journey.
Thank you so much for this wonderful comment for Nicole! So wonderful to hear about your brother and his progress. Wishing him, you, and your family the very best!