Kay’s Waldenstrom Macroglobulinemia Story
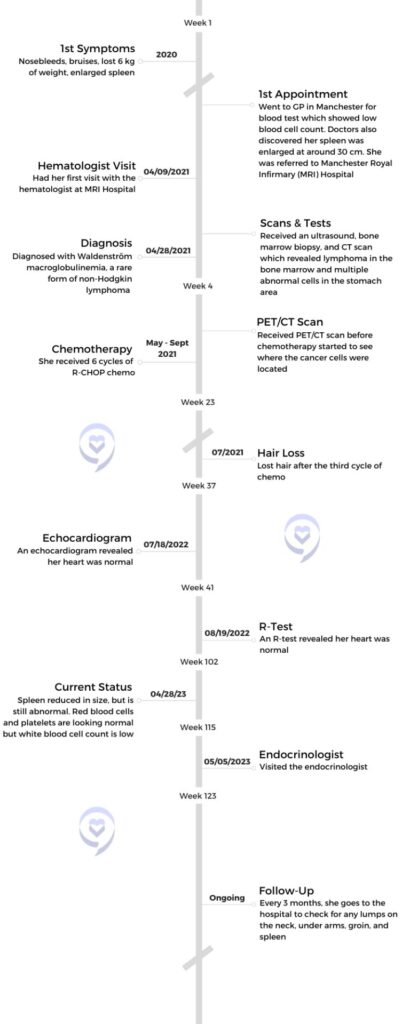
Kay* (alias for privacy) often visited the doctor as strange symptoms arose, including nosebleeds, weight loss, fainting episodes, and hair loss. Her doctor told her she likely had anemia and was not vigilant to check her for other issues. This led her to switch doctors, who discovered she had a rare type of lymphoma called Waldenström macroglobulinemia (WM) and an enlarged spleen. Doctors told her she was one of the youngest people in the UK to have this disease.
Kay began R-CHOP chemotherapy to combat her cancer, but she did not complete her first cycle due to various side effects which she was not warned about by her medical care team. Further lack of information from the hospital Kay was at ensued, which led her to switch hospitals, only for her to receive similar care. Rather than accepting this, she sought a second opinion who helped her better understand her treatment options, including stem cell transplant.
Today, her cancer is stable, in partial remission, and is being actively monitored while her care team considers giving her a stem cell transplant. She shares her cancer journey with us, including the importance of standing up for yourself, her quality of life with lymphoma, her side effects from chemotherapy, expelling misconceptions about cancer, and her advice to those on their cancer journeys.
- Name: Kay* (Alias)
- Diagnosis (DX):
- Non-Hodgkin Lymphoma
- Waldenström macroglobulinemia (WM)
- Non-Hodgkin Lymphoma
- Staging
- 4B
- Symptoms
- Nosebleeds
- Extreme fatigue
- Fainting
- Bruises
- Hair loss
- Breathlessness
- Bone pain
- Treatment:
- Chemotherapy
- R-CHOP
- 6-cycles
- R-CHOP
- Rituximab
- Chemotherapy
I think it’s truly beautiful to share your story, but also reminds people that they’re not alone.
Kay
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms & Diagnosis
Tell us about your diagnosis
I never knew in a million years I would be diagnosed with cancer.
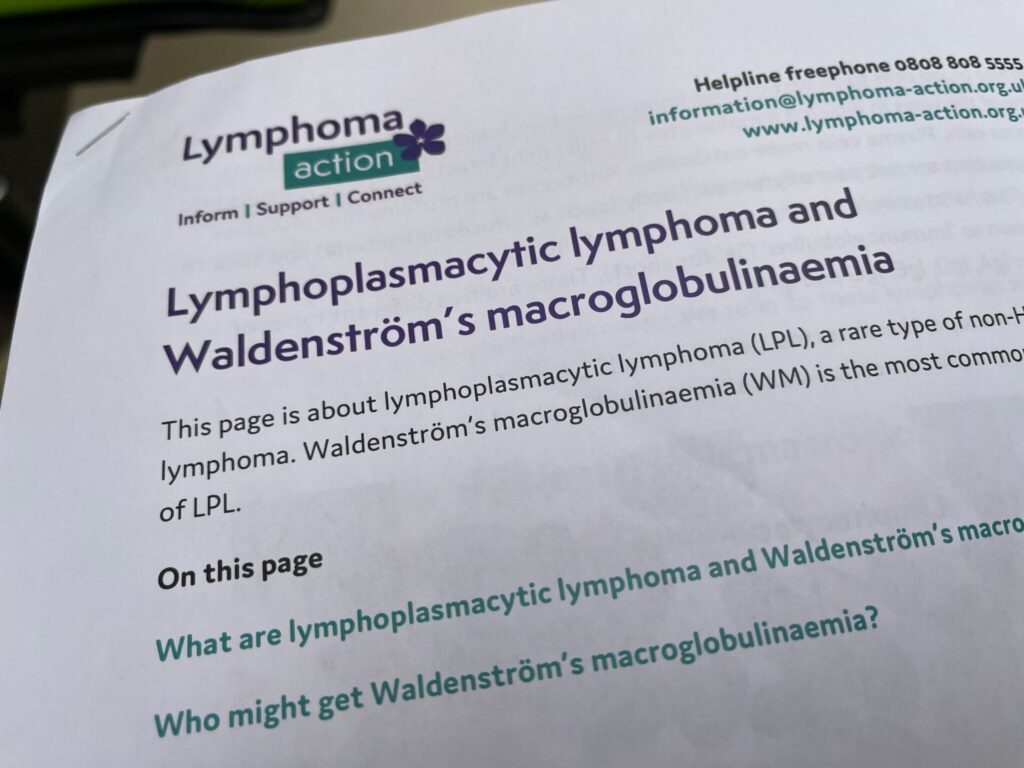
My name is Kay and I have a rare cancer called Waldenström macroglobulinemia – it’s a long name. It’s WM lymphoma, you can say. It comes under blood cancer, non-Hodgkin lymphoma, rare cancer, B-cell lymphoma.
I was diagnosed in 2021, and I had high-grade aggressive cells and I had an enlarged spleen 3 times larger than normal size. And of course, something was growing inside me. Initially in 2020 I already recognized this.
What were your initial symptoms?
The GP that I used to go to in Manchester, England said, “It’s going to come and go.” They were not clear with me, but they kept on taking blood tests to see if I am anemic. I started with anemia and they kept asking me to come back and forth, but I said, “I need some medication or something. I can’t keep on going [like this].” So I didn’t want to go again.
I felt like I needed a new doctor to check on me. That’s when I moved to another [doctor] and I felt much better because I was looked upon quickly and after my blood test they said something is abnormal. [I received the] results in March 2021. I was like, “Oh, what is wrong?” They said, “We’re going to refer you to a hematologist.”
I used to have nosebleeds. I had unexplained bruises – I’m thinking, what’s going on – and weight loss. I lost 6 kilos, so things were unexplained. I was not feeling well either.
»MORE: What Does Cancer Feel Like?
In 2020, I had a bald patch. I was like, “Oh my God, what’s going on? That’s abnormal.” My eyelashes were falling out. I thought, “Maybe it’s a castor oil allergy.” Then I started bleeding in December. My nose was bleeding and I was losing so much hair. I thought it was normal for an anemia patient. My doctor said, “That’s not normal.” I was losing hair, losing weight, not eating well, and my body was collapsing. I [fell] on the floor. My dad picked me up and said, “Have a banana, have this.” They thought my blood pressure was low.
What was happening in your life around the time you had these symptoms?
My sister was like, “Are you sure you want to move?” I was also moving to another home. I used to live very close to City Centre in Manchester, so I was like, “Yeah, I’m 100% sure. I want to be independent.” I think that was a bad idea for me to move.
Did you suspect you had cancer at that time?
Things went a bit downhill in my life, and I think it hit me when the doctors were saying, “We need to talk to you face to face.” I’m like, “What do you mean?” They said, “Your blood cells are abnormal.” It’s like, what is supposed to be abnormal?
I spoke to my sister. She was a doctor and she said, “It means it’s abnormal.” But they didn’t tell me anything. I think my sister is the one who saved my life by saying, “Something is off with you. You should go to your doctors for a check up.”
She was saying before diagnosis, maybe it could be lymphoma, because [she was] looking at the ultrasound diagnosis as well. I was like, “No, honey, I don’t have blood cancer. It can’t be.” I was very determined that it must be a blood disorder, but I [didn’t believe] I had cancer. That never came into my mind.
How did you react to receiving your cancer diagnosis?
I never knew in a million years I would be diagnosed with cancer in April 2021. I was like, “What? No.” I didn’t take it really well. I threw my stuff on the ground because I was so frustrated. I was like, “No, this is not it. This is unfair. Why is life so unfair to me?” My family kept saying, “Calm down, calm down.” My sister was like, “Don’t worry.” I think the more months went, the more I accepted that I had cancer.
My sister and I had a little bit of an argument because at Manchester Hospital, the hematologist was writing to my sister rather than to me, the patient. Communication is key if you really want the patient to be in the know. She was writing to my sister and my sister was writing to me. The thing is, I should get the appointments [directly]. I should know when things are [happening], so that was not professional. They did ask me initially, “Do you want your sister to know?” But I didn’t know they would write to each other and that I would never get to know about when my appointments are. Only my sister knew. Because she works in a hospital, she wouldn’t be able to constantly give me emails. I think they should email me only.
»MORE: Reacting to a Cancer Diagnosis
Did you take anyone with you on diagnosis day?
The more you understand your disease, the more you accept it.
They told me they wanted my sister to come on the diagnosis day and that I wouldn’t want to take my mom because she would start crying. I did take my mom initially for the diagnosis day, because I said to my mom, “I do not want to keep on repeating myself and what I have.” My sister knows medical terms so she was easier to go with.
On the diagnosis day, she asked the doctors and the hematologist what’s my survival rate and am I curable? I know the word lymphoma is coming. I know I have cancer coming. I have also done research beforehand and I have accepted in a way that I have this. Looking at the diagnosis with the ultrasound, I was connecting the jigsaw puzzle of what I have. I said, “Maybe, sister, I have Waldenström macroglobulinemia.” She said, “No, no, that can’t be.”
I mentioned the name even though I didn’t even know what it was. I know it affects white cells, it lowers your white cells and it gives you plasma cells. There’s an abnormal plasma cell that gives you IGM protein, so I have studied my disease. I think that’s very important to study your disease. The more you understand your disease, the more you accept it. Acceptance is very important with cancer. Once you accept it, then you can start living your life.
Chemotherapy
What cancer treatment were you on?
There were a lot of things going on. I was signed up with Manchester Infirmary Hospital because I didn’t have any preference. I didn’t know how the team members or the team people would be. I was just referred by my GP to them, and I had my R-CHOP chemotherapy for about 5 to 6 months to treat high-grade [cancer]. They said, “We suspect that you have transformed to high-grade,” but later on they confirmed that I had high-grade aggressive cells, which were treated with R-CHOP.
What is the status of your cancer today?
Now I have a low-grade. They said my PET/CT scan that I had this year in 2023 is much better than what it was 2 years ago. Now it’s reduced completely to its former size. My lymph nodes are nearly reduced to small size.
I just have active cancer cells in the chest area. As long as it’s not doing anything, my sister said it’s fine and to take it easy and keep eating healthy food. So it’s much better now, but the past 2 years it was a mixed response. This year it’s like, wow, magic. I had a nearly clear scan. Last year they were telling me the spleen size was still enlarged. I’m happy that this year it’s normal size.
Did you have any side effects on chemo?
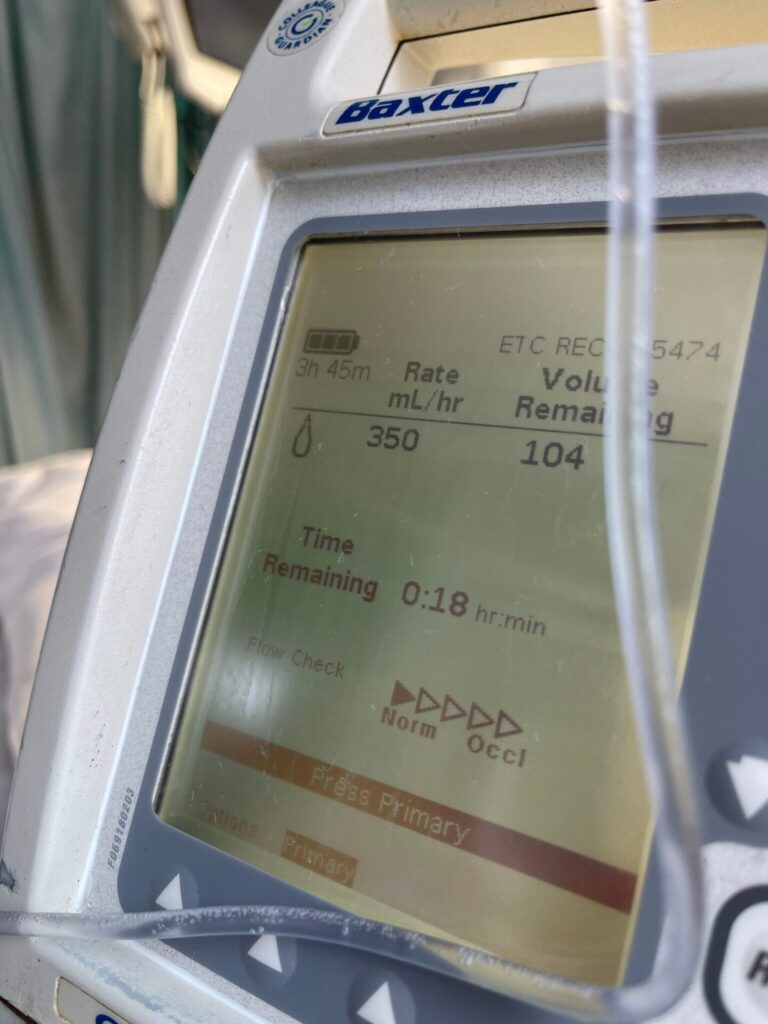
When I had my chemo in 2021, I wanted to give up. I initially didn’t complete my first cycle because I reacted to rituximab. My heart [was beating] so fast. I still have that issue at the moment. I feel that impact when I travel with speed.
My heart feels really weird, like it’s tightening. I have had heart scans last year to rule out if I have any heart disease, considering my dad has heart problems. My heart is normal. They said they might do [a scan] with a dye contrast. I keep [telling them] that when I travel, even when the train goes fast, I feel weird in my heart. I’ve asked, “Can you please check this again?” That’s why they’re going to do it with dye contrast, which is still on wait. It’s a long waiting time.
I still have bone pains I’ve been dealing with since before diagnosis until now. I’m dealing with numbness in my feet, so I’m trying to walk. I feel like I’m flying a bit high. I fell down this Thursday badly on the road where there was a car. I was in the middle of the road. Nobody picked me up, or said, “Are you ok?” I picked myself up gracefully and I was happy that I was not fractured or bleeding because I can easily fracture – that’s also a problem I have.
I have a dental issue as well, so I’m going to the dentist to get my treatment. I have cavities and they did fill them. They said because I have non-Hodgkin lymphoma, I’m still able to get dental. One thing I didn’t [learn from] Manchester Royal Infirmary hospital (MRI), was that you could get dental help.
Every 3 weeks I had chemotherapy, which is not bad, but I felt like it was drugs, drugs, drugs, and then more side effects. I think the first cycle and the third cycle were much worse because I had more side effects. You also feel weird in your mouth, like an ulcer or something. I thought I could take these side effects.
Did doctors prepare you for chemo side effects?
They kept saying to me,”Please don’t read about side effects.” They gave me a leaflet, but said, “Don’t read it now,” because I was a very anxious person. They were not [understanding] of me being an anxious person. Some hematologists ask, “Why are you anxious?” It made me think, “Are they [understanding] me as a patient or are they not?” That’s why I moved to Christie Hospital because I wanted a better team.
It’s not like everyone was [bad], just one particular hematologist and a few of the nurse specialists. I moved to Christie Hospital. I judged the building by its cover and not the inside. Unfortunately, I am in a situation where I expressed my feelings to them and I don’t think they’ve taken it really well. They know that I’m going to move to another hospital again. It will be my third time.
Did anything help with the side effects?
The first cycle, as I said, I didn’t complete because I was having a reaction with rituximab. I told them my heart was beating really fast and they said, “Nothing’s wrong.” I asked, “Can you just stop the treatment?” I was so worried. After that I went home and I was feeling sick. Even the anti-sickness medicine was not working for me. Whenever my mum fed me, it came out.
I felt like I was going to collapse. You feel like you’re going to collapse when you have this chemotherapy, especially R-CHOP because it’s high-intensive. They also gave me an injection for thinning blood clots because you’re on the bed all the time. You can’t move. I remember it exploded on my clothes. The blood exploded everywhere. I didn’t make a scene, but I told the nurse. They were a bit rude, one of the nurses. She said, “Oh, you’re such a baby.” I meet different people with different mindsets and I’m just like, “God bless you.” That’s all I’m going to say.
I feel like the side effects that I had from chemo were the worst. The first cycle was the worst, because everything was entering my body. When a drug enters, your body is trying to figure out what it’s doing. It’s attacking the cancer cells, but it also attacks the healthy cells. It doesn’t just attack your cancer cells. That’s what happened.
It doesn’t let you eat properly. You lose weight. Again, I had a low weight at that time and a low BMI. They were like, “Eat, eat.” I was like, “I feel like I can’t eat. It’s killing me inside.”
Being A Patient Advocate
You need to remind yourself of your value and you need to step up and stand up for yourself. That’s what is happening now – I’m standing up for myself.
Do you feel like your first doctor listened to you?
No. They were saying I had anemia. I did take iron tablets. I had hair loss, and I felt fatigued and breathless. I vlogged. Three years ago I joined YouTube. I remember when watching my old vlogs, I did sound breathless, like I couldn’t breathe. That’s proof that I wasn’t feeling well. And I was so fatigued. I was extremely tired. Even walking 11 minutes to my GP was a lot for me. I can’t walk for 11 minutes, I’m too tired. I’m thinking, I can do this, I can do this.
They did blood tests that time. The GP that I use, I still have them but I have moved to my local now because I think I’m done with them. You know when you feel like they’re helping you, but they’re not helping you? You need to remind yourself of your value and you need to step up and stand up for yourself. That’s what is happening now – I’m standing up for myself. There’s a lot of things happening around the world and I’m not forgetting that. But I think you need to focus on yourself too. You can’t keep forgetting yourself as a cancer patient. I do believe in spreading love and not hate because there’s a lot happening around the world. I just feel like I keep forgetting myself. I need to take care of myself as well, because who else will?
Switching doctors
The first GP said [the problem was] anemia. I said to my sister, “I really think I should keep on looking for another GP.” I got my appointment in March. I used to faint a lot in 2020 as well. [My cancer] was not visible and everyone was doubting what was going on. “Why are you fainting if you’re unwell?” I was like, “No, I’m fine. I’m sure it’s just anemia,” but I seriously did not understand what was going on.
I had hair loss, bald patches, and white hair. I’m like, “What is going on?” Things were not making sense for me at that time. I used to have heavy bleeding. I do have a second opinion as well, so there are a lot of doctors involved in my case now. But I’m more than happy to have a second opinion from London. She’s more knowledgeable than I feel the Christie Hospital was. Maybe they just follow the principles, but I’m going to be honest, I love her.
I met her recently at a conference that I went to, WMUK. They are international, based in Florida, USA. They [held it] in Birmingham and Amsterdam, so I went to Birmingham last month. It was really good and I got to meet my second opinion and other people around the world. It’s really nice to be able to talk about Waldenström macroglobulinemia, how you can manage your symptoms, and actively monitor it. That was very useful.
Is it common for young people to get WM?
I’ve been told many times that I’m the youngest patient in the UK to have this disease.
I got to meet different patients. I didn’t get to meet young patients like me. There are young patients in London, but I’ve been told many times that I’m the youngest patient in the UK to have this disease. It usually occurs in older people above 65 who are caucasian. I am from Denmark originally, so I could have it from them. When they did a mutation test at MRI in Manchester, it was negative. They usually look for MDY88 DNA, but it was negative.
Did you get a bone marrow biopsy?
My second opinion wanted me to do a bone marrow biopsy this year to see if it turned positive. I was not keen to do a bone marrow biopsy again because it’s painful. I don’t know how I [got them to] agree to do it under general anesthesia (GA). My sister said, “No, don’t do it because it’s under the tube.” I said, “Don’t show me the videos and pictures. I’m not interested. I’d rather just do it on GA.”
I was dealing with an enlarged spleen 3 times larger [than normal]. It was 30 centimeters in the ultrasound and 31 centimeters in the PET/CT scan, which is why they were saying we have to do a bone marrow biopsy. They didn’t want to delay my treatment because they could immediately see it was growing.
Reacting to a life expectancy
If they didn’t give me treatment, I would’ve possibly been hospitalized or worse because I felt I was enduring a dire situation. I felt that. Of course, they can’t tell you, you’re going to die. They will be diplomatic. They won’t be straightforward, especially at MRI. But the Christie Hospital was very direct with me and told me I don’t have much time. They told me I have a short life [expectancy] in October 2021. That hit me so hard. I was thinking, “Why? Why did they tell me about this?” I’m like, “That’s up to God.”
I believe in Allah, so I would do my best to leave it up to God. But there were 4 people telling me, “You don’t have much of a life with this disease and because of this, what we’re doing is giving you a treatment whenever you need it. If you are relapsing or high-grade, we’ll give you a treatment, then slowly we’re going to give your body time to recover.” They said, “This chemotherapy doesn’t really improve the quality of life.”
Were you given alternative treatment options?
My second opinion talked about a stem cell transplant and said, “If that is needed we might give you.” But the Christie Hospital – there’s a debate going between these two people – said, “We might not do it because it could be a risk of 20% death and 80% survival.” But why are they looking at death only? Why are they not looking at the good, positive impact?
They were telling me, “Okay, you have reduced lymph nodes and they’re still in the chest area, but it’s looking as if it’s clear and it’s still partial remission you are in,” thank God.
Do you feel your doctors have been straightforward with you?
The second opinion has a way of telling me the truth and says that there’s active cancer cells. I’m like, “Why couldn’t the Christie Hospital say that?” I’d rather you give me honesty and truth. Truthfully, nowadays, people do not have the ability or the courage to say [these things]. I’m seeing it in today’s world and today’s generation. But I like to speak the truth rather than [spread] lies, manipulation, and gaslighting.
I feel like I wasn’t treated well enough at Manchester Hospital, to be honest. That’s why I moved to Christie Hospital. I thought Christie Hospital would be better, but I think I judged them by their cover rather than the inside. With the second opinion, I can’t move to London. I live in Manchester, I live alone, I pay the bills and everything is [expensive], so it’s not easy to come back and forth. Especially when I have heart problems. It’s difficult now.
I think doctors should be very honest and truthful. Just say it. I’ve heard the worst. People have said, “You’re going to die, you’re going to have a short life, you don’t have much time,” and this and that. For me, it’s a normal conversation because I’m a cancer patient. You hear these things, but to normal people, they’re like, “What? No way. That’s not normal.” That’s because you’re not in that position, but actually, you just have to be a human.
These days humanity lacks everywhere, to be honest. I think people need to be human, be careful, and grateful in life, whatever they’re dealing with. If you haven’t had cancer or have had cancer, just be grateful in life. Be happy, don’t worry about it, and spend as much time as you can on this earth.
Quality of Life
Describe your quality of life with WM
I’ve been living with cancer. Obviously it’s a bit of a limitation for me. I can’t go in crowded places, I can’t go to certain things. I do go to events, but I go early in the morning so that I know not many people will come. Once there’s so many people, I’m out of there because I don’t want to trip on people. I don’t want to faint or pass out. I don’t want to make a fool out of myself. Yesterday I went to this event in Preston and my mum was like, “Are you sure you’re going to go?” Because they’re worried about me.
Since I got the diagnosis, my family has been very cautious about me and very worried about me. They keep on calling me to ask, “Are you ok?” Every single day, my mom calls me. She asked, “How are you going to live alone? How are you going to do this and that?” My sister suggested I live alone because she said, “I don’t want you to get infections because of us.”
Last time she got COVID, thank God I was living alone. Cancer support had some advice and they said, “You should go and isolate yourself. If you don’t have COVID, then save yourself because it will be a risk factor for you.” I think I only had the flu. I didn’t have COVID that time in 2021.
Have you had any complications with cancer?
This year I had sepsis, I had COVID, and I was hospitalized for 3 days. This year has been a nightmare for me. I’ve been very traumatized, to be honest. Being told to your face that you’re going to die if you go against our rules. It’s like, I want to go home. Can I just go home? Because I can’t sit here for 6 hours or more. They said, “No, there’s not enough beds.”
I asked, “What do I even have? What have you diagnosed me with? Oh, sepsis. Sepsis? No way.” I’ve heard about sepsis, but it didn’t click for me. I said, “If I go home, what’s going to happen?” They said that the complication is death. I said, “You know what, keep me. Admit me to the hospital.” I didn’t have any choice. If I go home, what if I get worse? If I didn’t get any fluids in my body – because I was not eating well and my body was breaking down.
My mum saw me at my worst. I was coughing a lot. They [thought I had] COVID and said, “Keep your mask on.” I said, “Mum, keep your mask on.” I think it was too late for them to send my mum because all night, she was not able to sleep like me. She was worried and crying. She didn’t want to leave me. I was like, “Don’t worry, mother, I’ll be fine. I’ll be here for 2 days and I’m out.” At least that’s what they told me.
But sepsis is life-threatening and it’s not fun. You’re on fluids, you keep feeling full and you can’t taste anything. Then they said, “Oh, it was a misdiagnosis.” Then I found out it was a misdiagnosis. I said, “Why did you fool me?”
How has cancer changed your outlook on life?
I take this cancer as a blessing. Because I believe in Allah, I take this as a blessing. I know a lot of people take it as bad or think life is unfair. In 2021, I thought, “Oh my God, how bad.” Then I took it as a blessing, thinking, “Okay, I got this. I’m learning something.”
Before, I used to care about what other people say about me. I used to take care of other people rather than myself. This cancer journey has led me to focus on myself and what I want. I think this is a lesson learned, but also a blessing for myself to focus on myself. Like, honey, you need to focus on yourself. You have cancer now. Sit down and focus on yourself instead of other people around you.
[People] can say whatever they want. It doesn’t mean if it’s true because that’s just a narrative they put on you. Some narratives could be very false about you. People make up rumors. Some people assume a lot of things like I’m living a normal life. I wish I was living a normal life. I don’t think this is a normal life. I’m wearing a face mask and I can’t be in a crowd. If you want to go to an event, you can’t go [because you might] fall down.
I feel numbness in my feet now. I’ve been telling the Christie Hospital this and I’m actually going to see them on the 20th of November. Hopefully I can tell them what exactly happened and how it happened, but I twisted my ankle as well and I’m wondering if it’s swollen. I can see my knee is swollen and I’m just bearing it.
Overcoming people’s perceptions of what cancer looks like
I don’t [like to] show people that I go on walks. People say, “Oh, she’s not sick.” My appearance doesn’t look like I’m sick, but inside, whatever the cancer is doing, you won’t ever see with a magnifying glass. You can’t see it unless you make a diagnosis.
I think a lot of people’s mindset needs to change, especially people with canes and pregnant women. I know there are priority seats for them, but I’m seeing so many people in England being diagnosed with cancer and it’s crazy, but you can’t see whether they’re well or not. They might look beautiful with makeup. They can cover their scars and they heal, but so many people are saying, “Oh, you don’t look sick.”
I’ve been told by a social worker in the UK, “Oh, you don’t look sick.” It was day one after my chemo. I’m thinking, “How do I not look sick?” It’s crazy to pass these kinds of comments. It’s not nice. Be in our position. You would understand [if you were]. We can’t imagine being in a position [of someone] lower than us who doesn’t even have cancer, but who are not able to live in a house, or don’t have shelters. If we talk about that, we should have to be grateful in life.
Finding the right support system
I remember I completed my first cycle on the 1st of June. I at least completed it. I took my mum. I was like, “I’m going with mum,” but I felt so bad taking her because they were not letting her get in the ward. There was a lockdown in 2021, they were not letting anyone go in for a bone marrow biopsy. My sister couldn’t get in, despite being a doctor. They only allowed her to go on diagnosis day because they were like, “Okay, she’s a doctor.” Otherwise they would never let other people go in, which is a bit of a pain. At least get me someone.
My friends asked, “Do you want us to go?” I said, “No, it’s okay. It’s too overwhelming. I don’t think you can handle it.” You need someone who can handle it because you can’t just go with anyone. Everyone has a different tolerance.
»MORE: Read More About Cancer Support
I don’t think my mum could tolerate it, but she still came despite waiting for so many hours. I said, “Sister, do you want to tell her or should I tell her?” I told my mum I got cancer, so she started crying. I said, “Don’t cry, mother.” I was hiding my tears sitting there and doing nothing.
Having help getting to and from the hospital
I was so happy my sister said, “I will send your mum to your home. You’re not going to live alone.” I’m like, “Why?” She knew for a fact that it’s not good [to be alone] and I’m so happy my sister told me so. My sister has been very supportive. She has been to most of my appointments in April. In May she was working so she couldn’t.
She said, “You can get a hospital transport.” I’m so happy that the hospital transport was actually free of cost. They took me from my home to the hospital and from the hospital to my home, so that was a great help. Even the Christie Hospital still gives me a transport home. I think this is great because transport, when you’re living alone, will cost you a lot of money. That’s great because my sister can’t always take me. She still works so I think that’s nice.
Cancer Treatment
Describe your latter chemo cycles
When I was in the fourth and fifth cycle, I became extremely tired and I couldn’t stand it. After chemotherapy, once you’re sitting in the wheelchair, you can’t stand. Your body is weak. You can’t even get up. My body was breaking. My bones were aching and you have to take steroids to help you with bone pains. It also can give you weight, which came afterward in 2022. I can feel the masses.
In 2021, they did my PET/CT scan and discovered [the chemo] had worked 50%, but 50% it hadn’t worked. I asked, “What does that mean?” They said, “You have partial remission.”

The MRI hospital, before chemotherapy, they were giving me high hopes saying, “You will be in remission in the sixth cycle.” Then they said, “You will never be in remission.” I said, “Well 6 months ago you’re telling me that I’ll be in remission, and 6 months later you’re telling me I won’t be in remission.”
I was about to [ring] the bell. They didn’t even have the bell. I was like, “Let me [ring] it. Let me find the bell on Amazon and I’ll buy it.” I’m glad I didn’t buy it, but I’m just like, they’re not clear. Why couldn’t you tell me this before? They just wanted me to do [chemo]. I asked, “Is there no alternative to R-CHOP?” I learned from other doctors that there is an alternative. I thought, “Why did MRI hospital say I needed this?”
How long were you on R-CHOP?
I think 6 months because I need to have 6 cycles of chemotherapy to complete it.
Wanting to give up on chemo

I kept saying to my sister I want to give up every month. I want to give up. She said, “No, you can do it. You can do it. You just need to think, you did one, you have 5 left. You did 5, you have one left.” She kept telling me to keep going. I asked, “How am I going to do this? It’s too awful to think about.
With the bone marrow biopsy, they did it under GA. The thing is the MRI people didn’t want to do it under GA. They didn’t recommend it. I asked why and they said it was because I have an enlarged spleen. I can’t stand, sit, or sleep. I’m just in pain, and you’re telling me I can’t do it. I wrote to my GP. My GP was very sufficient. I explained to him that MRI hospital doesn’t want me to do any GA. Also my sister, because she’s a doctor, was also insisting for me not to get it done because she knows how things work. Maybe she saw a video or she has seen people with this and there’s a lot of complications. I think she just wants to protect me.
Being uncompromising
I don’t think there should be a compromise from my end all the time. I feel like if you’re going to compromise, then where do you take your stand? Where is your worth? I love to stand up [for myself]. So I went to my GP, I said, “Write a letter to her [that approves] me being under GA.” Less than 24 hours later, I got an appointment with GA. I was like, “Should I cry? What should I do?” I was frozen for a while. Then I said, “Oh, it’s tomorrow. Oh my God, I haven’t prepared myself. I don’t know what to do.” I was so scared. I was crying.
I realized that my tears were not my weakness. I think a lot of people think tears are a weakness. It’s not. It’s my strength. If you have nothing and no one, you have your tears. That builds strength. A lot of people admire me and say, “You’re so inspirational.” I said, “I’m not an inspiration, honey. Not for that.” Someone telling me I’m dying – I’m not inspirational for that.
The importance of sharing your cancer journey
Nobody wants to see people dying, but there are so many people who’ve died from cancer on YouTube who I used to follow. I’m shocked. I’ve talked to them and it’s painful to see them die. They did mention that they were dying, but nobody wants to see them dying. It’s heartbreaking. I don’t know what to say. I’m clueless right now. [This YouTuber] has inspired so many people by talking about things.
What I want to do is share my cancer journey on YouTube to find a cure by giving interviews, but also saving people’s lives. I feel like when you save one person’s life, you save the whole human entity. That’s what it is in Islam, because Islam is a peaceful religion. Saving people’s lives makes me happy. If I can help one person, I can help another person. I think it’s truly beautiful to share your story, but also reminds people that they’re not alone.
Living With Lymphoma
Have you lost friends on your cancer journey?
I have lost some friends during this cancer journey. Some people didn’t speak to me. I recently lost a friend. She was there with me with the diagnosis. During that time, she disappeared. Everyone has depression and anxiety. Fair enough. That doesn’t mean that you can’t ask how I am doing. So I have lost friends, which is not good.
Some people are good at saying, “Do you want us to help?” But when I ask them for help, they disappear. So what’s the point of saying these things? I think they just want to say that they were there for me, but they were not there for me. I think that people should stop doing that. You’re not helping. I felt alone in this cancer journey. Let’s be very honest, I feel I’m still alone.
People don’t understand my cancer, or they think I am cancer-free because there is no more treatment. So many people said to me, “You shouldn’t do chemotherapy.” Like, honey, if I don’t do chemotherapy, I would not be in this world. I would be dead. They said that I didn’t have the option to freeze eggs. This year I learned I’m in permanent postmenopause. My sister said that is infertility. This year is bad news.
Switching hospitals
When they said, “You won’t be in remission,” my heart broke. After that, I decided to move to another hospital.
Had you finished chemotherapy at that point?
I had already done the cycles. The doctor said [my care] would be lost in transition. She said, “You’re a cancer patient.” I said, “Don’t worry, I’m moving to Christie Hospital and they’re doing my PET/CT scan. It’s just a transition.” I told myself I have to stand up for myself because I was getting mixed signals from MRI Hospital.
I was thinking about writing a book very soon [about my experience], but I can’t write the hospital name for some reason. A lot of people said I could be sued and God knows why, but I’m very honest. It has to be transparent, otherwise, I can’t write a book because I don’t like to tell the half truth.
What were your results after finishing chemo?
It happened in October 2021. They said I had 50% of cancer cells and 50% had been reduced. I said, “Okay, and what about my spleen?” They said it had reduced but not by a lot. I asked, “Okay, so enlarged meaning, it can’t be ruptured?” Rupturing is life-threatening. You can die from it. [Because of this], I can’t carry heavy stuff.
I have to be very careful not to rupture it. They said I couldn’t sleep on the right side because it was too heavy. The left side wasn’t heavy, so I had to sleep on the left side. Usually on the right side, I can sleep better because I don’t feel the heart weirdness. My heart felt so weird after chemo. I think because of the drips from the machine and the speed that it goes in [caused it]. Otherwise, I don’t know how I got it. They said one of the chemo drugs can affect your heart. I’m like, that’s not good.
Delaying chemo
I went to another hospital because I got mixed signals from the MRI people. They were not being clear. They should never say, “You won’t be in remission.” They were convincing me to do things that I didn’t want. They were saying that there’s no other option. They said, “We don’t want to delay your treatment.” Then why are you talking about pre-surgery, honey? Why are you talking about pre-surgery if I don’t have the option for that? Because they said pre-surgery would take another 2 weeks and they don’t want to delay.
They gave me my first cycle on Eid day. I said, “Can you at least give me one day off on that day? Because I want to celebrate Eid without any tension. It will ruin not just me. It would ruin my family’s day as well, because they are fasting and they are celebrating Eid. If I do it on Eid day, everyone’s going to go nuts and crazy because they want to know how I am doing. Can you spare one day?” They said, “Okay, we’re going to spare one day, but we’re not going to be able to delay it.”
I got a bit lucky for the Eid day on the 19th of May. I think the 21st of May 2021, I got chemotherapy, the first cycle and then the second cycle. Then [I had it] in June, July, and August. September was my last cycle, but I landed in the hospital because I was bleeding from the bottom. My family was in Denmark while me and my dad were at home. Then I was in the hospital. I said, “Don’t worry, dad. I’m coming back.” I couldn’t leave him alone at home. My mum was like, “What is going on? Why is she in the hospital?”
Ongoing Cancer Care
Are you currently on cancer treatment?
No treatment. That’s the dilemma. These are the discussions happening. Basically after chemotherapy it was just active monitoring. So, a PET/CT scan to see, okay 50% [remission]. They said, “At the moment, you don’t need the treatment.” This carried on until 2022 and 2023.
They still say I do not need it because my cancer is stable. I was like, “What does stable mean?” Everyone thinks ‘cancer is stable’ means it has stopped or that I’m cancer free. This is a myth. People think when you’re done with chemotherapy, you’re free from cancer. But in my case, they said I’m in partial remission. I’m never going to be in remission in my life. I’m like, “Okay, so I’m living with cancer.” Technically, that’s what it means, but how much I’m living? They couldn’t say how much I’m living. That’s why I’m saying they’re not straightforward. They were hesitating to say things. I think they should have sat down and talked about the side effects, which I was being told not to read about. Otherwise I would have known my dental [benefits] and I would have gone to the dentist. I didn’t get the choice to go and talk about it.
I have a bone marrow biopsy and they want to do a lymph node biopsy. I was praying for no more pain. I don’t want more pain. I’m done. The radiologist said we can’t do it because the spleen was on the surface and behind all the tumors and cancer cells. There were multiple in my stomach. That was weird how that happened. There was a significant amount in my bone marrow. It starts in the bone marrow.
Everyone thinks ‘cancer is stable’ means it has stopped or that I’m cancer free. This is a myth.
What stage is your cancer in?
I asked, “Where would you stage me?” They said, “There’s no stage, but we will stage you in stage 4B. Symptoms such as fever, night sweats, itchiness, and weight loss, that comes in B symptoms. X is a bulky disease because the spleen was enlarged. They said, “You’re the youngest patient that I’m treating.” I said, “Well, at least I’m the youngest and not the oldest.”
Are you currently getting scans?
Yes, now I’m having scans. In October 2021, I had my scan initially, then in January 2022, I had another PET/CT scan. They did 2 to be clear what was going on with my neck. They saw some lymph nodes had gathered here in January. They thought that maybe this could be cancer, but they can’t confirm. They want to confirm that with a lymph node biopsy. I said to them, “I don’t want to do that. Do I have to do this?”
I did have a CT scan after my bone marrow biopsy, just 4 days after. That was on my birthday. Unbelievable. I said, “You guys can not give me at least one week?” They said, “We don’t have much time.” I’m like, that’s my birthday.
I had to drink 3 liters of water. I remember the whole total. I don’t know how I did it, but it was a disaster. I remember the [injection site] used to bleed. It was not stopping. They put one, two, three bandages on it and it was not stopping. Your platelets get so low. You get bruises, you get bleeding, but it doesn’t stop within 10 or 15 [minutes]. I remember I had a deep cut, it didn’t stop. It was still bleeding for 2 hours and wouldn’t stop.
So right now it’s monitoring. I have another scan this year and it looks like every year I’ll get a scan because of my second opinion. She wants to see where the cancer is. If she didn’t insist or recommend it, I would never know if my spleen was normal or if things were getting reduced.
Where is your cancer and symptoms today?
There’s no lymph node sitting on my neck area. It’s a bit small. Lymph nodes are sitting in my chest area and they’re active. I don’t know what they’re doing, but I do have night sweats every single day. In the morning when I wake up, I have hair around my neck and itchiness, which is a pain. I’m dealing with it. I have bone pains every single day. I’m feeling numb.
I’ve had UTI infections 2 times this year. One of them led to sepsis because I had a blood infection, chest infection, and COVID. I’ve had so many in one day. I was hospitalized for 3 days. The CT scan also showed reduced lymph nodes and my spleen being normal, 10.5 cm. That’s better than the 31 centimeter that I had initially. I’m happy that my second opinion pushed [for me]. I was rejected twice from my one consultant I met at Christie Hospital.
I asked her, “Do you want me to go all the way to London for the scan? Because that’s not going to happen.” She said, “No, we’ll do it [here].” After 2 times I tried convincing them to do a PET/CT scan. Otherwise I would never know about my spleen being normal size. I would never know what was going on. They said, “We want to have a picture before we do anything.”
Are you still considering a stem cell transplant?
The second opinion spoke about it and said, “Have they not discussed it?” I said, “No, the Christie Hospital hasn’t spoken about the stem cell transplant.” When I mentioned it to them, they said, “Okay, yeah, we might do it if you need it, but we’re just waiting.”
Usually the PET/CT scan only happens when it’s progressing. They won’t do it if it’s stable. Stable doesn’t mean that it’s completely gone, it’s just slowly progressing. So this cancer is slowly progressing. I thought stable meant it stopped, but it doesn’t mean it stopped. So in 3 or 4 months they’re going to see me again for a checkup.
Active monitoring
They check my neck and armpits for lumps. They check my groin and my stomach area to see if there’s enlargement. This is what I get and also blood tests. They check my IGM. My IGM has been low, which is great. It’s lower than 3.0. I think the IGM I had in 2021 was 24 IGM, and that was high.
You have fainting episodes. You will feel your body collapsing. You can’t walk. You will feel anemic because your red blood cells, white blood cells, and your platelets will be low. Also plasma cells are abnormal in IGM because that’s the IGM protein. So now I’m being actively monitored. It [feels] a bit slow because right now they’re just seeing me if I need to, but they are planning [a possible] stem cell transplant.
The second opinion said they want to prolong my quality of life. At my age, we have to consider that. I was like, “Why is the Christie Hospital not considering that?” So I am looking for a good [health care] team. It’s going to take time to find one. I have to see my local [doctors] now because I’ve just moved. I have to tell them how I’m dealing with these things, then maybe I can get into a new hospital. It’s a bit hard. They said not to move because then I have to refer myself to a second opinion, so I am in a bit of a dilemma.
Reflections
Surrounding yourself with positive people
Share your story, your journey with diaries, or however you want – on YouTube, Instagram, or with your friends. My closest friend was surprised when I was diagnosed with cancer. She was like, “Are you sure?” I had to show her my folder. I think she was shocked and she couldn’t take it. She told her family. Some people won’t be able to take it. I have other friends who were crying. I was like, “Don’t worry, I’ll be fine. I’ll keep you updated.”
She sees me nearly every month and comes all the way from London to Manchester to visit. I’m so blessed to have these kinds of friends in my life that come to visit me. You need these kinds of friends. Be with friends who would consider supporting you, even telling you [they’ll be there] if you need any help. Be around positive people. Negative people would make you depressed and sad.
The importance of focusing on yourself
If [doctors] are not telling you the truth and you’re getting answers via other people, you can seek a second opinion. It’s your right.

What I’ve learned about myself is that I also need to focus on myself. I know it’s not easy to focus on yourself, especially with whatever you’re dealing with and what is happening around the world. I understand that some people might have bad things [to say] about you, but you know who you are. You know the truth. Don’t let other people tell you what to do. Think about yourself. Do you accept these things from other people?
If [doctors] are not telling you the truth and you’re getting answers via other people, you can seek a second opinion. It’s your right. They can’t tell you not to. You can seek opinions 2, 3, and 4. Wherever you want to go, you can seek opinions. You just need to do it. If you feel you can not today, you feel bad, then do it the next day. You may surprise yourself.
Do you have any advice for those on their cancer journeys?
You should stand up for yourself if they’re giving you mixed signals like I did. I’ve received mixed signals, and dealt with them not being able to tell the truth. People should be a bit kind as well, because some people might not accept you the way you are. If you’re able to accept yourself and know your value, you would know how to stand up for yourself.
I think people should learn to accept things and educate themselves about their disease. I’ve seen people who don’t educate themselves and they just put out wrong information. Why are they putting out wrong information? I think you should educate yourself, whether you like it or not. I know it gives you anxiety, but I think the more you learn about your disease, the more you would accept it and you can educate other people about it.
More Non-Hodgkin Lymphoma Stories
...
Pete D., Waldenstrom Macroglobulinemia
Symptom: Irregular blood test results during a regular workup for Crohn’s
Treatments: Chemotherapy, surgery, radiation, monthly IVIG
...
Sheree N., Waldenstrom Macroglobulinemia
Symptom: Feeling anemic
Treatment: Chemotherapy (bendamustine & rituximab)
...



