Arielle’s PMBCL Non-Hodgkin’s Lymphoma Story
Arielle was diagnosed with primary mediastinal B-cell lymphoma (PMBCL), a subtype of non-Hodgkin’s lymphoma.
In her story below, she explains in detail how she got through intense chemo, how she approached fertility preservation and how she advocated for herself as a patient. Thanks for sharing your story, Arielle!

- Name: Arielle R.
- Diagnosis (DX):
- Non-Hodgkin’s lymphoma
- Subtype: Primary mediastinal B-cell lymphoma
- 1st Symptoms:
- Swollen lymph nodes (neck)
- Fever
- Appetite loss
- Weight loss
- Fatigue
- Night sweats
- Coughing
- Itchy skin
- Hard to breathe
- Age at DX: 40
- Misdiagnoses:
- Mono
- Costochondritis
- Treatment:
- Chemotherapy:
- R-EPOCH (Dose-Adjusted)
- 6 cycles, each cycle = 3 weeks
- Inpatient, receiving services in the hospital (instead of outpatient, which means driving into appointments)
- Chemotherapy:
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I dug deep. I did more than I thought I could. I endured more than I thought I could. We’re resilient humans, and I believe in you. I believe you can do it. You’ll get to the other side, too.
Arielle R.
Arielle’s Story on Video
Diagnosis
How did you get diagnosed?
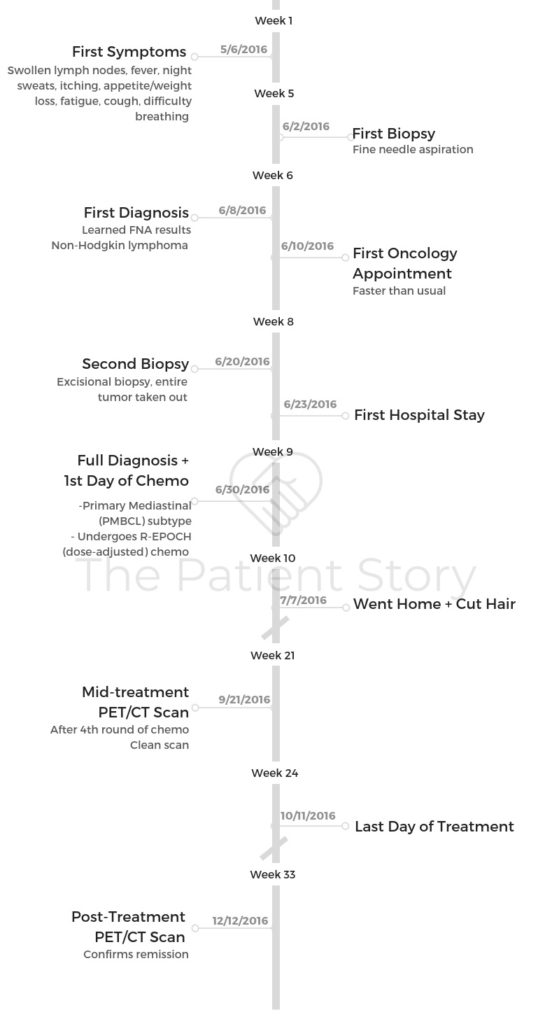
Summary: I felt the first symptoms and was misdiagnosed a few times before getting a fine needle aspiration. Results took one week.
My first symptoms were pain in my neck, shoulder and chest. They were misdiagnosed for a couple of months as “costochondritis.” I went to urgent care while out of town and followed up with my primary doctor. Both did chest X-rays and came to the same incorrect diagnosis.
My appetite waned, and I started to lose weight but didn’t take any action. Then the lymph nodes along my neck, throat and clavicle area swelled up suddenly. I called my primary doctor’s office, but they couldn’t get me in that day, so I went to urgent care again.

The doctor there suggested it was probably mono, did blood tests and told me to come back in 2 weeks if there was no decrease. I returned 2 weeks almost to the day and then went for a fine needle aspiration (FNA), an initial biopsy, the following week.
I remember that last week before I did the test, the FNA, to find out, I decided I was going to not work at all and just stay home. I rested and rested, and that was the week when I did the Google searching. I was just so low. I was so exhausted. I had zero energy.
I’d never had an FNA. It’s really an intense experience. I remember my head had to be turned a certain way, and it wasn’t just one needle poke. It was 5, 6, 7 — I don’t even remember. It’s so scary thinking about a needle going into your neck. Luckily, my sister was there with me.
The results took a week, and that was unbearable. That wait was awful. I know why it takes that long, but that was pretty painful to wait. I got the call from my primary doctor, who I don’t know really well, and she said, “We got the results of your FNA. It’s lymphoma.” And I just burst into tears.
How did you choose hospitals?
Luckily, my primary doctor is with UCSF Women’s Health, so I’m already within that system. When the urgent care doctor sent me for the fine needle aspiration, it was all linked through UCSF. I was then referred to my hematology oncologist.
Did you choose treatment?
Summary: No, I just followed my doctor’s recommendation, despite my history of using more alternative medicine.
I don’t know if this is true for other people, but a part of me felt like, “Is [R-EPOCH chemo] the right choice? Is this going to save me? Should I be questioning this?”
There was so much to question about the process, but I never questioned the chemo, even though I’m pretty strongly alternative in terms of alternative medicine. I don’t typically go down the traditional western medicine path and yet cancer… Chemo? Let’s do this.
Whatever they tell me, whatever’s the right chemo — okay, you just tell me what to do. I questioned everything else, but that I did not. That was just take whatever they tell you. This is the poison of choice? Okay, got it.
I was getting so sick, not oxygenating and all these things, so they needed to give me a round of chemo to start. Before we even had the full diagnosis, they gave me two baby doses of Cytoxan, which is kind of an evil chemotherapy.
It’s very harsh, very old, makes your hair fall out immediately. Then we found out what my diagnosis was. I did a full round of what my treatment would be, which was 6 cycles of dose-adjusted R-EPOCH.
Chemotherapy
Describe each cycle of chemotherapy
- Week 1: Continuous infusion through PICC line (arm) or port (chest) for 24 hours, lasting 5-6 days
- Week 2: Side effects tend to kick in, ranging from nausea to mouth sores
- Week 3: Typically the healing week when blood cell counts recover
- NOTE: If your white blood cell count (WBC) doesn’t rebound back into the standard range, your next chemo cycle may be delayed.
What was Week 1 of chemo like?
Summary: It was the week when I got the drugs infused.
I did it as an inpatient, so I would check into the hospital and do approximately 6 days of the continuous infusions around the clock.
The R-EPOCH chemotherapy is a 21-day cycle, so approximately 6 days I’d be in the hospital. Sometimes it was longer if I had a complication, but approximately 6 days.
During those 6 days, I’d get hooked up and be hooked up continuously except for when they would switch the chemo bag. For that time, I was totally connected to the IV line.
They would encourage me to get up and walk. The more you move, the better the chemo moves through you, the faster it moves out of you, so that was key, right?
The “R,” then four bags of “EPOCH.” That’s 4 24-hour bags. Then the final day would be Cytoxan, which we would clear out as quickly as possible, because it can affect your bladder and tons of fluids throughout.
How about weeks 2 and 3?
Summary: Week 2 was symptoms. Week 3 was trying to recover in time for the next cycle.
I would get home [from the hospital], and honestly a lot of what happened was checking in with my oncologist. I went in 2 times a week in the 2 weeks I was home. In the hospital for 1 week, home for 2 weeks, but go in at least twice a week to check in. There was always something to do or monitor.

Then by the end of the cycle, maybe 3 to 4 days before the next cycle, I’d start feeling better. I’d start to get more energy and want to do something.
I’d want to go out. I’d want to go for a walk, which was amazing. I wasn’t driving, so I would start walking. I didn’t feel safe driving, so I would just walk here at my house, out on my deck, and get a little sunshine.
I could just do more, a little laundry, little things. Maybe I’d wash a dish or something. Then I’d remember that I would have to go back in for my next round, which was really hard.
How did you deal with chemo?
Summary: I welcomed each bag of chemo into my body, told it to do its job, then told it to leave.
After that first round, I realized I was very angry at the chemo, so I did a little bit of work on that. I realized that I was both angry and grateful, so I created this mantra. I would look at the chemo bag each time and call it “liquid gold” because it was gold-colored for EPOCH, and etoposide is the orange-y color.
I would look at it and say, ‘Thank you so much. Please come in my body, welcome it, welcome to come into my body. Do your job, then get the f-ck out. No lingering!’
I would spend those 6x days welcoming each bag and telling it to get out. Honestly, those days were all about a regimen of drinking enough, eating enough, using the bathroom enough, because that was tracked in the hospital. How much fluid you peed out, if you had a bowel movement. If I didn’t, I couldn’t get the next bag of chemo, so it was really serious.
We all cheered on, ‘Please poop!’ Never talked about poop that much in my life! Then also getting in that walk, so it was super, super regimented in the hospital, and I had to focus on the basics.
What was the first cycle of chemotherapy like?
Summary: I was scared and shut down emotionally, went through the motions of getting my chemo and did not process anything.
Honestly, I shut down in the first cycle. I think I was so scared of chemotherapy and so scared of — I don’t know I if was scared of dying, but I was so scared of the experience that I really checked out. I think for the emotional safety of that moment, I shut down and [my wife] was really, really was scared that I was going to shut down for the whole process.
What I realized is that after my first cycle, I came to that moment of, “Okay I can now take a breath and can grieve this.”
I just cried.
I just cried about it, and my lovely therapist did Skype therapy with me. I got to just be present with all the feelings that were coming that I had shut down during that first round, and I think that’s when it felt less scary.
I’m grateful, though. I wouldn’t change it. If I could go back, it’s not like I would say to myself, “You need to feel during this first round.” I think that was exactly what I needed to do to get through such a scary moment, the acute scary moment, to then have enough energy, enough emotional energy especially, to move through all that was going to come. Not only the chemo, but all the side effects and all the other problems that I ended up having.
How was the port and PICC line?
I had 3 PICC lines and 1 port — a port that went wrong, unfortunately.
I knew the port was a good choice. Under the skin, less chance of infection. It was either infected, or something was not happy underneath the port. We took it out, and I was fine.
I managed the PICC line. It’s just a lot more work but no infections, no problems. You just have to keep it clean. It’s weird. You have a tube sticking out of your arm, which is totally different than a thing in your body that you can’t see.
For me, every so often I’d get a little nauseous when I looked at my PICC line and think that tube’s going into my body right now. There’s some disassociation that has to happen to be able to go through some of these things.
(Editor’s Note: The port infection is considered very rare.)
»MORE: Read patient PICC line experiences
What was the PICC line like?
You were connected completely except those moments when they changed the chemo bag. 6 days of just being connected. I remember having to figure out how to shower, how to put on and off my clothes so they wouldn’t get stuck on the tube when I would take it off.
I did that once. The way we put the lines on, the way the nurse did it, we got it on backwards. When I went to shower, my shirt was stuck! I pulled it off and got it through the arm, and it was stuck on the line. I rested it on my IV machine, and we waited 20 hours later till we could disconnect it from the channel.
Side Effects
What were the side effects?
Editor’s Note: A lot of the type and degree of side effects vary person to person.
- nausea
- fatigue
- constipation
- mouth sores
- loss of appetite
- stomach/digestive pain
Describe the side effect cycle
[Starting Week 2] I would have a few days where I would feel kind of loopy from all the chemo. I’d feel really nauseous, kind of lightheaded, and I would become neutropenic. That’s when my white blood cell count (WBC) would drop, and I would just be exhausted.
Usually every round I would get some quantity of mouth sores. Sometimes it would just be a few and I was sort of okay, but mostly once I got to Round 4 it was awful. I do not know how many mouth sores I had because I couldn’t open my mouth even a tiny bit.
The doctor wanted to look at it, and that’s the only time I would open my mouth. If I wasn’t in the hospital, then I was lying on the couch. I was miserable for a few days. I had no energy. All I could do was make myself eat and drink.
I think constipation was the biggest one. Oh man, something we don’t want to talk about, but we have to talk about it because figuring out how to manage my digestive system was probably the hardest part about chemo. Once I figured that out, I was good.

I figured it out, but I went through some pretty terrible experiences to get there. That was a thing that my doctor didn’t really know how to guide me on. I found that the suggestions from the nurses and doctors did not work for me, and I needed something gentler. Finally, my oncologist suggested a different option, but it took awhile to get there.
Nausea was different round to round. It increased with each round, so I know by the end I was taking round-the-clock Zofran. I would set a timer. I actually ended up not doing the normal every 8 hours, but we split it into 4-hours doses, which was very rare. I took the Zofran all through treatment and probably for 3 months afterwards because that nausea just lingered on.
I think I was also terrified to go off of it because I was so nauseous, and nausea’s bad. It’s one of the worst symptoms. It makes you feel terrible. It made me feel like I couldn’t function. You don’t want to eat. I tried some other drugs when the Zofran wasn’t enough — and it was never enough — but some drugs worked, and some drugs definitely didn’t work.
We ended up giving me more and more and more of the anti-nausea drugs in the last 2 cycles. It didn’t work. I was just nauseous. I just kind of had to accept it. I did a lot of laying around in those moments, and I also did a lot of distracting.
I’m not a big TV watcher, but man, I needed TV. I needed something to fixate on so that I could stop thinking about my body, and TV really helped. I could do a show, something small, take a break because my brain couldn’t really follow for that long, and then go back to it.
That was really key for me with nausea, to try and distract or pace around the house. Just something to change the moment.
Please rate the side effects you got from chemo
Everyone tracks differently. Arielle rates her side effects with chemo an 8 out of 10. This indicates that she happened to have a more difficult experience.
Were you prepared for the side effects of treatment?
Summary: No, my medical team did not warn me about the side effects nor how to deal with them.
Absolutely not. My doctor was far more focused on the big picture, to the point where she didn’t believe me when I was having side effects. I had to self-advocate to the point of frustration just to be believed and supported. It shouldn’t have to be the patient’s responsibility, and I wish that the doctors spent a bit more time learning about the side effects to help patients along from the beginning.
One example: I had pretty awful stomach/digestive pain from the chemo, got a prescription for an anti-acid, but no one told me that it works best in the morning on an empty stomach. I spent several weeks in pain until my doctor randomly shared this information.
»MORE: How to be a self-advocate as a patient
Hair Loss
Describe the hair loss
Summary: It can hurt when the hair falls, so I buzzed it off short first, then shorter as more hair fell. Hardest part was when the eyelashes and eyebrows also fell. Oddly, it was less weird because at least my appearance matched how I felt. Wore a lot of cute hats!
Oh, hair. I had to let go of hair right away because I had not only my R-EPOCH Round 1 but that double dose of Cytoxan, so the hair just needed to come off. It hurt.
Because I was so sure about that, I sat in my living room, and I asked my sister to be here. Jess pulled out the buzzer. I decided I didn’t want to shave my head. I didn’t want to have a bald head. There’s something about that smoothness that was more scary to me.
I know some people really want that. For me, I just wanted it really, really, really short, so I buzzed it down to an inch or half an inch, and we would get shorter as it was falling out more. We would maybe buzz it down a little bit more.
But it was so tender on my head. Everything was so tender. It was really hard. Hair is just one piece of the puzzle. As I’m talking about hair, I’m thinking I didn’t feel beautiful at all. Because I attempted to harvest my eggs, I was bloated. From my chemo I would get small, then bloat from the steroids and all the fluids.
I was constantly in this state of flux, and I was nauseous. Who feels sexy when they’re nauseous? You don’t feel beautiful. You feel awful. In some ways, the lack of hair went with everything. It was part of the package, like, “Oh yeah, that makes sense. That’s what I look like.” It got harder the more pale I looked.
I kept some hair, and it slowly went away through the cycles. Then my eyelashes and my eyebrows went, and that was so hard. That changed everything. I didn’t look like myself anymore.
I remember I would get up in the middle of the night and go to the bathroom because of all the fluids. I would go to the bathroom and catch myself every time, and I was startled every time.
»MORE: Dealing with hair loss during cancer treatment
I still would look at myself and feel this overwhelm of, ‘That’s not you. That is not Arielle. That is someone else.’ I think for me, the hair was just a piece of the puzzle so I could acclimate to my whole body not feeling like me.
My skin didn’t feel like me. Everything, every part of me, felt foreign. I think if my hair had been the same, that might have been an even more bizarre experience. I would joke that I looked “cancer-y.” I used that term. “Oh, I look so cancer-y. Can’t you tell when I’m out in public?” Or someone would come see me, and I’d say, “Don’t I look cancer-y?” I would try to lighten the mood. I don’t know.
I looked like I felt, so for me I just had to let go of the vanity, because there was nothing about me that felt good. I covered my head up. I definitely wore hats. I was in treatment from July through October but in San Francisco, where it’s not warm in the summer, so I was cold. I was thin.
I had just really simple cute hats that I found. Almost ski hats that were comfortable, hold my head because my head would get tender, too, not only when the hair was falling out but as it kept falling out.

Your scalp hurt when you lost your hair
Your scalp hurts. At least for me it did. It was so painful. I had very, very white-gray hair naturally. Now it’s a bit darker grown back in, but you could see the red of my scalp, and I just wanted it off. It was painful. No one tells you that. In the medical system, no one tells you that because it’s not “important” right?
What’s important is curing you of cancer, but what’s important to us as cancer patients, as the person who is dealing with it, is to know how to navigate all those pieces of the puzzle. And to be able to anticipate some of it. This may not happen to you, but I wanted to give you a head’s up.
Hair grew back 2 to 4 weeks after the last chemo. How was that?
Summary: I was happy the hair started to grow. Then the awkward phase hits.
It was so amazing when my hair started growing back. I never had super, super short hair, never buzzed my hair or anything, but I thought I looked pretty cute when I had really short hair. I all of a sudden felt this new confidence, maybe like, “Oh, I actually look okay!” It was not a look I had ever intended, but it was fun. There was some joy in it, joy in the hair coming back in general, but joy in the styles.
Then of course the awkward of, “How is this going to grow out, and what am I going to do with it?” And there’s the growing pains. I’ve had my first hair cut! This is grown-out first hair cut. I let it grow. I got the amazing curly, weird look that just did not have a style and finally chopped it. I’m so happy.
I think that was actually the biggest shift for me away from feeling like I looked still like I had had cancer, even though I’m sure people couldn’t tell. But to me, getting a hair cut, getting a style, meant I was just Arielle. I wasn’t Cancer Arielle.

Quality of Life
What was the worst part of treatment?
- Summary:
- Waiting
- Sorting prescriptions
- Figuring out medical-speak (doctor talk, test results, etc.)
UCSF has wonderful care, but the hematology clinic is completely overloaded with patients. I found the following to be hard:
- Doctors have too many patients and practice nurses are overwhelmed, so they have a hard time responding to questions or giving you test results. It was the worst for my post-treatment scan.
It took me calling several times, emailing and speaking with a supervisor to get my results. Even though this is their day-to-day work reality, I don’t think my doctor (or her colleagues) really appreciates how personal and scary this journey is. - I had to do my R-EPOCH treatment as inpatient for several reasons. I found the hospital admittance system and their lack of needed beds to be awful. One cycle, I was delayed by 9 days because they simply didn’t have a bed for me, and then I was put into a room with another patient.
Going through chemo is a ghastly experience, one that should afford some privacy. This is not always true and, to be frank, it was humiliating, scary and frustrating to share a room with a stranger while going through this overwhelming experience.
What was the biggest surprise?
My port bruised up and didn’t “work.” My oncologist didn’t believe me, and it was really a terrible experience to get it checked and then removed. That could’ve been handled so differently and in a supportive way.
What helped when you lost all your energy?
Summary: Getting blood transfusions and IV fluids, available in hospitals and clinics (if you’re outpatient).
Blood transfusions. I think I had 3 or 4. I can’t quite remember. They were amazing.
I was terrified, totally terrified of course. Blood, someone else’s blood going into your body — it looks crazy going in your IV, but it’s the best thing ever. I would feel like a million dollars 24 hours later; I had energy. Same thing with getting fluids, so if you’re worried about that, it’s not as scary as it seems. It’s actually such a blessing, so sometimes I’d get a little extra something to get me through [the cycles].
How did you manage your thoughts and emotions?
Summary: I took it one step at a time.
I decided very early on that the only way for me to manage it was to stay right in the moment. Anytime I started thinking about the next day or next round or how many more hours I had left on the bag or anything future-thinking, I would flip out. I would panic. I would get super emotional. I’d get fearful.
It’s manageable, but the only way for me it was manageable was to slow down to the moment like, ‘What do I need to do right now? I need to go to the bathroom. I’m going to go pee. I need to eat something. I need to have a snack. I’m going to take myself to the kitchen or call the nurse for a snack. Or just the next thing right in front of me.’
I could not think much beyond that. “Jess is going to visit me this evening. Okay, what do I need to do between now and then? I need to eat 3 meals. I need to drink 6 cups of water.” Whatever it was, I would just quantitatively help myself get through the day. I couldn’t think beyond that. Then it wasn’t manageable to have cancer and be in treatment.
It’s interesting. I think in some ways I set [the cancer part] aside a lot, and I was so in the treatment part of it. Maybe there was just this background belief that I was going to be okay.
I think I felt I was going to die in the very beginning when I was having trouble breathing. I think there were probably moments there, but they were fleeting.
It’s not that I was overconfident or ‘I’m going to beat this.’ I was not a cheerleader for myself, but I just had this fundamental belief system that I just had to move through these steps, and I would get to this other place. I didn’t know if I would need more treatment.

I wasn’t thinking beyond. It was just all about the steps along the path, and that’s what made it manageable for me.
What do you wish you had known before you began chemo?
Summary: I wish I found someone with the same cancer for emotional support from the start.
It’s really hard to answer that, because I think that everyone needs something different. For me, I cope with people. That’s just who I am. I’m a dependent coper. I do better when I’m in communication with someone, so finding other people’s stories was the best gift for me.
I could take what I want and leave the rest of it, like I didn’t have to take it all, so that was really important.
I wish that even sooner in my cycles I had met in person people who had this specific cancer. To me, that connection, that face-to-face contact, was just huge. I met a woman here who didn’t have a lot of side effects.
»MORE: What kind of support cancer patients say helped the most
It’s not like she could really empathize with some of those things, but there was enough that she could empathize with. She could empathize with the anxiety. I had anxiety through the roof! I didn’t know I was an anxious person.
I’ve now learned I’m an anxious person, but it really came out. I’m not anxious in my day-to-day, but there’s anxiety underneath so full force. Having someone else reflect back at me, like, “Oh my god, I was so anxious, too!” It was critical.
Be your own advocate
Summary: The doctor is focused on saving your life, not quality of life like side effect issues, so self advocate by asking any and all questions important to you.
The thing I did not get from my oncologist was any helpful information on side effects. This I what I’ve learned: Oncologists are amazing, they are brilliant, and what they know is chemotherapy.
They know treatment. That is what they studied. It’s what they see day in and day out. It’s what they have to care about because it’s the treatment, whether it’s chemotherapy or immunotherapy, it’s the treatment that’s curative.
I started to get neuropathy, and I told my oncologist. She lowered one of the dosages, one of the chemo’s within the cocktail, and my neuropathy went away basically. I was like, ‘People don’t know to do this. If you just say something, and the oncologist can help you, maybe, sometimes you have to really push.’

It was painful. No one tells you that. In the medical system, no one tells you that because it’s “not important” right? What’s important is curing you of cancer, but what’s important to us as cancer patients, as the person who is dealing with it, is to know how to navigate all those pieces of the puzzle and to be able to anticipate some of it. “This may not happen to you, but I wanted to give you a head’s up.”
When you have those gut instincts, you have to go with them. You at least have to explore them is what I learned. When I have something in my gut saying, “Whoa, whoa, whoa, hang on a second,” voice it.
Doctors did not like how many questions I had, but I asked them anyway because they were critical. I’m a human being, and I get to ask all my questions and take up space.
That’s the best advice I can give: Take up space. It’s your life. It’s not their life. They’re not the ones going through the chemotherapy. They know a lot of things, but they’re not the one. You know your body.
»MORE: How to be a self-advocate as a patient
Can you work during treatment?
There are people who didn’t have any side effects, who worked full-time through treatment. I was a wreck! It was impossible. It’s laughable. There’s no way I could work at all.

How important is it to have caregivers?
Summary: It’s important to have constant support so you don’t have to overthink or overdo. TV and iPads can be very helpful when you’re alone, especially in the hospital.
Everybody around you copes differently. I have to remind myself of that, and I had to remind myself of that during treatment. I needed a lot of people in my life to be available to me. Sometimes that happened, and sometimes it didn’t.
I needed people to handle those logistics. I needed someone to remind me to breathe. I needed a therapist. I was so reliant on having remote Skype therapy. I couldn’t go in because I wasn’t driving, as I said, but I needed the emotional connection. I don’t think that you can ask to get everything, all your needs met, from one person. I don’t think that’s true in life in general.
So I could get certain emotional needs met by Jess, and I could get certain emotional needs met by what ended up being some of my oldest friends and some of my newest friends.
It was who could be there for X and who could be there for Y, and maybe some people get that from 1 person or 2 people.
I had to kind of piece it together. As I said, I didn’t get everything that I had hoped for or that I felt I needed, so there was still loneliness in that, but I definitely asked for things as best as I could. And I had to accept when I couldn’t get them.
I found other ways, too. This is going to maybe sound funny, but I decided I was going to watch a TV show I watched long ago from start to finish. It was an intellectual show, so I was intentionally going to stimulate my brain, as my brain was becoming more mushy.
I think there were 7 seasons of the show, so I basically did a season per round. It was almost like they were my friends during that time. It’s so cheesy, right?
We sometimes feel close to TV, but I needed that in the hospital. I’d have my iPad. I would just watch a show before bed, and it would help me feel, I guess, not as alone. Connected. It was this line I could pull through treatment. I had to pace myself to not watch it too quickly, because I wanted that. I wanted to be able to savor it all the way through.
I use that example because it’s not always that obvious [that] it’s your partner that meets all your needs, or it’s your sister or parents. It’s not. It doesn’t have to be, at least. It can be so many different things, but for me the point is that I had needs that needed to be met.
I had emotional needs. I had physical needs, logistical needs. I needed people to drive me places to go to the doctor, and I had to get those met by others, by television and by myself.
I did a lot of work on meeting my own needs through treatment. Really crying and being sad and holding myself in space and acknowledging that it’s really an unpleasant experience. One of the most unpleasant experiences — or hopefully the most unpleasant experience I will ever go through.

I don’t wish it on anyone, even people that I struggle with. I would never want that for them, because it was awful. Getting as much support as I could was the only answer, and some of that support had to come from me.

Inspired by Arielle's story?
Share your story, too!
Primary Mediastinal B-Cell Lymphoma Stories
Lauren D., Primary Mediastinal (PMBCL)
Symptoms: Dry cough, extreme fatigue, trouble breathing, swollen and discolored left arm, lump under the arm
Treatment: Chemotherapy
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough; low-grade fever; night sweats
Treatments: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatments: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.




