Cherylinn’s Stage 4 Mantle Cell Lymphoma (MCL) Story

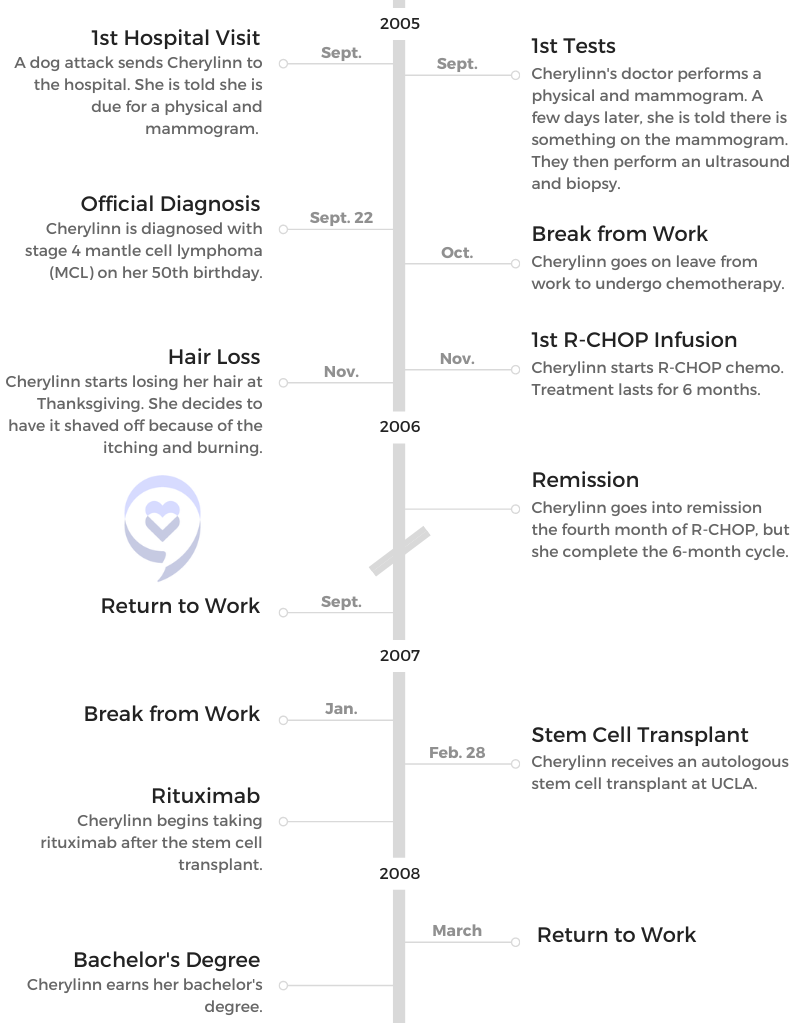
When Cherylinn was diagnosed with stage 4 mantle cell lymphoma (MCL) in 2005, she was told it was terminal. She decided to fight anyway.
Read her incredible story of undergoing chemotherapy, 2 relapses, and thyroid cancer while also earning 3 degrees and being a single parent.
Thank you for sharing your story with us, Cherylinn!
- Name: Cherylinn N.
- 1st Symptoms:
- No initial symptoms
- Diagnosis:
- Non-Hodgkin’s lymphoma
- Subtype: Mantle cell lymphoma (MCL)
- Stage: 4
- Treatment:
- R-CHOP chemotherapy
- Stem cell transplant
- Ibrutinib
- Rituximab
- Clinical trial
- 1st Symptoms and MCL Diagnosis
- MCL Relapse and Treatment
- Clinical Trial and Stem Cell Transplant
- More Mantle Cell Lymphoma (MCL) Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
1st Symptoms and MCL Diagnosis
Introduction
Tell me about yourself
I’m retired from City of Hope. Now I’m just at home. I have a Great Dane who’s my partner, and she and I do a lot of things. We go walking and try to get healthy, and I love to read. I used to have a lot of books, and then I found that I had tons of Rubbermaid containers with books. I got into the Kindle, and so now I have hundreds of books in my Kindle, but that’s what I like to enjoy.
There are some mountains in Los Angeles, where I live. It’s nice sometimes to sit on the deck when it’s really nice and just have my Kindle or maybe a glass of wine, some music and just enjoy reading.
I volunteer for the Leukemia & Lymphoma Society (LLS), and I enjoy doing that. I talk to people who call in that are newly diagnosed with cancer and just give them some insight. My philosophy is that if I can make one person not fear cancer as a death sentence — that it’s something that you can get past — then I’ve done my job. I try to help people to withstand cancer. I tell them all the educational and financial programs. There’s a lot to LLS, and that’s why I’ve been volunteering with them since 2007.
After a freak accident sent you to the hospital, what happened and what tests were run?
The paramedics and the hospital said, “Go see your primary doctor afterward.” It was when I saw my primary doctor that she said, “You haven’t had a physical or a mammogram.” I had a sister who had passed away from breast cancer, so she said, “You are due for a mammogram.”
Now that I’ve gone through this, what am I going to do to cure it?
“Okay, fine,” I thought. I didn’t think anything of it. I felt healthy. I’m overweight, but that’s pretty much the only symptom that I had. They did the physical when they did the mammogram. A couple of days later, she said there was something on the mammogram.
They did an ultrasound. I assumed it was breast cancer. They were doing the ultrasound but under my armpit. I was kind of worried about that. Then within that same week, they said, “No, we’re going to do a biopsy.” It was during that biopsy that they discovered that it was mantle cell lymphoma.
At what point did you realize something serious was happening?
It was so fast. One day I’m having the ultrasound. Two days later I’m having a biopsy. Then all of a sudden, it’s like, “By the way, you have cancer.” But again, I was assuming that I had breast cancer, and my sister was such a strong person that she always made me feel like you can get through this. That’s why she was my role model.
I was like, “Okay, I have cancer. I will see the doctor, and I’ll deal with it. I’ll do whatever I need to do and then go from there.” I had the “Why me?” and the crying and the anger, but it was more of, “Okay, now that I’ve gone through this, what am I going to do to cure it?”
MCL Diagnosis
Testing and waiting for results
They put me under because they did the biopsy on both sides and took out lymph nodes. They just said it was a biopsy. That’s why all along I thought it was breast cancer.

I received the results probably within a week. I was close to my 50th birthday. Ironically, the day that they did the biopsy, my kids were giving me a surprise birthday party with family and friends. I’m the kind of person that when I have to go to chemo and stuff, I just go by myself. I don’t bother anybody.
I thought the biopsy was just go in, get the biopsy and go home, and so my kids had planned that party for that night. I was in the hospital, and they were like, “You can’t have this.”
I was like, “Well, it’s okay. I’ll be fine.” It worked out okay. Then the following week is when they actually told me that it was cancer. When I saw the oncologist, that’s when he told me that it was mantle cell.
Then he said it was stage 4 and I was terminal. For me, terminal was my sister, who was maybe 80 pounds. You look like a living skeleton. That was terminal. I was looking at myself and saying, “How could I be terminal?”
He just said, “You’re terminal. We’re just going to make you comfortable.” I had been newly divorced after 26 years of marriage, and I had 2 children at home. My daughter was 14, and my son was 17.
How did you break the news to your children?
I made dinner. I have 3 children, 2 boys and a girl. My eldest son was married. He’s actually a paramedic. I had them all come to the house, and I just told them. I said they found cancer and that I’m going to try to go through treatment.
My daughter was 9 years old when my sister died, and she and I were very, very close. I didn’t realize that she had a memory of seeing my sister like that. When I said it was cancer, the first thing my daughter asked was if I going to look like my sister, like Auntie Pat. Like I said, my sister and I had talked a lot. I decided I was going to be very truthful, and I just said I didn’t know but that we would get through it.
»MORE: Breaking the news of a diagnosis to loved ones
Being honest with children
There was an incident where the paramedics took my uncle to the hospital. My daughter had asked a paramedic, “Are you going to bring him back?” The paramedic said, “He’ll come back.” He died in the hospital.
When the paramedics came for my aunt, it turned out it was the same paramedic, and it was like 2 years later. My daughter said, “Are you going to make her come back?” He said, “Oh, yeah, she’ll come back.” S he told him, “You’re a liar because you took my uncle, and he didn’t come back.”
I told him, and then he realized it was the same house. I said, “You have to be very careful what you tell children, because they remember.” I didn’t want to tell my daughter, “Yes, I’m going to be fine,” and then what if I passed away?
When did you find out it was mantle cell lymphoma?
He was an older doctor. When I went back in after they had done all the PET scans, the bone marrow and all the tests, they told me that he had left. He had to leave on emergency medical leave.
He said, ‘Do you want to fight?’
I said, ‘Yes, I’m going to fight.’
They had this young doctor from UCLA who was going to see me. I saw him, and I asked him, “How long do I have? 3 months? 6 months? What do I have?”
He looked at me and said, “Lift up your left leg.”
“What?”
“Lift up your left leg.” So I lifted my leg. Of course, if your doctor tells you to do something, you do it. He said, “I don’t see an expiration date.”
“What?”
He said, “I don’t see an expiration.”
I said, “Really, doc?”
He said, “I don’t believe in it. When it’s your time, it’s your time.”
»MORE: Patients share how they processed a cancer diagnosis
Chemotherapy and Side Effects
Treating with 2 forms of chemo
Then the doctor said, “Now, I will tell you, the person in this chart is as bad as it gets. You’re stage 4. It’s in your entire body, and it’s also in your bones. But I’m looking at you, and I can’t see it.” With that, he said, “Do you want to fight?”
I said, “Yes, I’m going to fight.”
He said, “I want to treat both cancers at the same time. Normally we would take care of the mantle cell first and then the bone cancer, but if the bone cancer goes to your brain, all bets are off.”

Like I said, I had no symptoms. The only symptom I had is I was always tired. I decided that I wanted to fight. When I started the aggressive chemo, the second day, they would go to radiology.
They would take the spinal fluid out of my spine and then inject the chemo directly into my spine. I did both chemos at the same time. It was really painful because I had to stand up and hold on while they drew the fluid and then put the chemo in.
What were the side effects from R-CHOP?
It was the typical side effects: you lose your hair, you can’t eat, you throw up. I had some butterscotch hard candy. For some reason, my body accepted the butterscotch candies. My son was at the market, and he found some butterscotch pudding.
He bought it just to see, and it turned out that my body could accept it and wouldn’t throw it back up. When I was in the hospital, I would always have my butterscotch pudding. If you can find that one thing that your body can tolerate, maybe that’s just what you need to help you.
Hair loss
At Thanksgiving, I was cooking, and all of a sudden a whole chunk of my hair came out. It was like my realization. My head used to itch a lot and burn. When that happened, I actually put a shower cap on because I didn’t want it to go in the food. Then I went to a barber.
It was kind of strange because this was 2005. Women being bald was not usual. I said, “I need you to shave me.”
He said, “Oh, you want your hair really short?”
“No, I need you to shave it,” I said. He questioned it, and then I just pulled my hair. Then he saw, so he shaved my head. It itched really bad, so it was easier just to shave my head at that point.
I was okay with being bald. My daughter was going into high school. I had a wig, but I would only wear it in front of people or her friends and stuff like that when I had to go out. Most of the time, I would just stay bald.
»MORE: Cancer patients share their treatment side effects
The emotional toll of being bald
I’ve been bald 3 times. This last time that I got the cancer, I asked the doctor about the chemo. I asked her, “Will I be bald again?”
She said, “Cherylinn, it’s just hair.”
What you don’t understand is for a woman, hair is important. For me, even though I’m okay with being bald, being part of a woman is having hair. She said she didn’t know, and luckily I didn’t lose my hair.
If there’s dishes in the sink, just let there be dishes in the sink. As women, we want to just do supermom things. When you’re going through treatment, you can’t.
I’ve been bald 3 times, so I understand. That’s why sometimes when I see ladies that are bald, I wonder if they are going through treatment or if it is now because women are bald. You see it all the time, so it’s not that big of a thing.
Sometimes when you know somebody is going through treatment, it’s like a sisterhood. Sometimes I wish I could just put my arm around them and say, “I understand.” I don’t want to go into their space, but I understand what they’re going through.
»MORE: Patients describe dealing with hair loss during cancer treatment
Going into remission
I went into remission about the fourth month of R-CHOP. It was like, “Okay, good, we can stop this.”
My doctor said, “No, you have to do the whole 6 months.” So I did, and I was okay. It was just standard. I was sick.
Being a single parent, when I would come home from the hospital, I’d see dishes and laundry. The first 1 or 2 times, I started going back to mom mode where I was cleaning the kitchen, wanting to go to the market, do washing and all that.
I ended up in the hospital because my counts went really low. I had to learn that I have to accept that I can’t be supermom. If there’s dishes in the sink, just let there be dishes in the sink. As women, we want to just do supermom things. When you’re going through treatment, you can’t.
»MORE: Parents describe how they handled cancer with their kids
MCL Relapse and Treatment
Testing
Thyroid cancer in 2010
I had an endocrinologist as well because I had Hashimoto. When they did the CT scan, they found that I had thyroid cancer. That was in 2010. They just took out my thyroid and 3 of my nodules, and that was it.

Relapse in 2014
An MRI scan showed that I had nerve damage on my right arm. It turned out my neck was degenerating, and I wondered if it was related to the bone cancer. The doctor said he didn’t know. He didn’t think it was. It was just my neck degenerating.
They ended up putting a titanium rod in my neck. Unfortunately, there were some complications during the surgery because it was a 2-part surgery, and they weren’t able to do the second part. I just had the titanium rods put in my neck, and that helped.
I was able to get all the feeling back in my right hand, with the exception of my thumb. My thumb still feels like it’s numb, like it’s asleep, but it’s there.
They did a mammogram. At first, when the radiologist had said there was a spot on my right breast, she didn’t want them to do a biopsy because she said, “Mantle cell doesn’t go in the breast.” But he was really adamant about wanting to do the biopsy.
We did the biopsy, and then it turned out to be the mantle cell. It was a surprise for me. I’ve been told that it was an aggressive cancer. I always knew in the back of my mind that it was going to come back sometime.
Of course, I went to see what my options were. At that time is when she told me that FDA approved a pill chemo, which was the ibrutinib. She wanted to put me on that, and so I did that.
»MORE: Read more about ibrutinib and other patient experiences
Treatment and Side Effects
Choosing a treatment option you can still work while taking
We were looking at all the different options. Rituxan had always had a really positive effect on me in regards to my treatment. She recommended this new drug that was available.
With my history, she was confident that would be the route to go, and it would also allow me to continue to work. That was one of the things, too. I wanted something that I might be able to still work on. She said that was a good one and that I would be able to. It was a pill. I could take it in the morning, and then I would be able to go to work.
Because I’m a single parent, it’s very important for me to continue to work to provide for my children. My daughter was still going to private school, and my son was still living at home because he was helping to take care of me. He was going to junior college, and I wanted him to be able to go to college. Being able to provide and work was very important for me.
I knew with the Rituxan, I would be able to maybe continue working, but it would mean that 1 day a week I would have to go get treatment. Normally, the next day you’re usually tired, so it’d be like 2 days a week I would be out. When she said that ibrutinib was an option where I could take pills and that I would be able to continue to work, that was a factor.
»MORE: Patients talk about working during cancer treatment
Starting ibrutinib and switching to Rituxan
I worked for City of Hope, and I’m a patient with City of Hope. Because I worked for chairmen, I knew a lot of the doctors. One of the doctors, the provost, is Dr. Rosen. He’s also on the board of directors for the Leukemia & Lymphoma Society.
One of the things is making sure that if people don’t feel comfortable, get a second opinion and don’t feel bad getting a second opinion.
I asked the secretary if I could talk to him as a second opinion. I went to go talk to him, and I explained to him about my side effects. I was concerned about working and having the side effects, and he was the one that recommended maybe I should change drugs. He’s the one that said he would talk to my oncologist. He asked me what I had taken before, and I told him that Rituxan had worked.
Getting a second opinion
When he went to talk to my oncologist, that scared me, too. One of the things is making sure that if people don’t feel comfortable, get a second opinion and don’t feel bad getting a second opinion. When I asked him and he went to go talk to my oncologist, I felt like she was going to be really offended that I got a second opinion.
She told me something that was very interesting. She said, “If they’re a good doctor, if they’re conscious of their patient, they shouldn’t be offended that you want a second opinion.”
I said, “I’m so sorry. I didn’t mean to go over.”
She said, “No, no, no, it’s okay, Cherylinn, because if you’re not doing well and this works, let’s go ahead and put you back on it.”
That’s one of the things that I liked about City of Hope and my doctors. We talked. They listened to you. We ended up changing treatment, taking me off that and putting me back on Rituxan. By the third treatment, I was back on Rituxan.
Discussing potential side effects of ibrutinib
I don’t remember too much. I know we discussed potential side effects, but I think at the time, it was more of, “Let’s just give it a month or 2 and see if it’s maybe just initially in your body, and that’s why your body is reacting to it.” By the second month, I was having the same symptoms, and that’s when I was concerned.
Low immunoglobulin (IgG) counts
I always call Rituxan my go-to chemo medicine, because for some reason I was able to tolerate it, and it seemed to work for me. I just have a low IgG.
It seemed like every 3 months, I would know my counts. I knew my counts were low when I would get a cold sore either on my top lip or inside my mouth, or I’d find bruising where I knew I hadn’t hit myself. I would know my counts were low, and I would just call my doctor and say, “Hey, I think my counts are low. I need to have a blood test.” Sure enough, they were low, and then she would schedule me.
My counts were low every 3 months, it seemed. It got to be where we just knew to set me up for an infusion. It just seemed like for as long as I can remember, like maybe 2010, every 3 months I would have to go to get the immune globulin intravenous (IGIV).
I called it my tune-up. It’s just like your car. You have to go in and have your tune-up. You make the car run well. It’s like I go in, and they plug me in.
Like I said, I was lucky enough that I worked for City of Hope. I would work in the morning, and then I’d go that afternoon to have the treatment, and then I’d be back to work the next day. I was fortunate enough that I worked for City of Hope, so I was able to do that.
Remaining Positive Through Relapse
The importance of positive thinking
Honestly, from the get go, I always thought it’s your attitude. I’ve read that with cancer or any illness, you accept it. Your attitude toward it is, “Okay, I have this, I’m going to fight it,” or “I’m going to deal with it or my treatment.”
Sometimes I think maybe it was like a guardian angel.
I think when you talk to people that are diabetics, it becomes part of their lives. Then it’s just your attitude. If you think, “Oh my God, I have to do this again,” then you’ve already put yourself in that position where you’re dreading it.
I don’t. It’s like, “Okay, I got to do this.” It’s like getting up to go to work every day. I got to get up. Okay, 3 hours I’m going to have to be plugged into this machine. I can look at the TV. I can read my Kindle. There are options. I can relax.
Relapse in 2022
It was in my right leg and my left groin. That was ironic because when they did the PET scan, that was only supposed to be from my neck to my torso. For some reason, it went past into my legs. Sometimes I think maybe it was like a guardian angel where they were like, “Let’s just go a little bit further,” and they found it.
At the time, she was like, “I’ve never really seen it there.” The doctor was like, “We don’t know if it’s mantle or not.” I just had to assume that I had something in my body that shouldn’t be there, and we were going to have to deal with it.
They did a biopsy in the right, but they had found that there was a spot on the left. Because originally I had it in my right breast, they concentrated on that. They also did a biopsy on the lymph nodes as well. It was in the lymph nodes.
Then I had a different oncologist because it turned out my original oncologist wasn’t a specialist in mantle cell. She was a myeloma doctor, so she had referred me to a mantle cell or non-Hodgkin’s specialist.
Meeting with the oncologist
When I saw her, we luckily Zoomed, because my son, the paramedic, lives in Lancaster. His fiancée is also a nurse, and she’s actually an oncologist nurse. They were on the phone with me and the doctor. I wanted them there because I figured if there’s any questions that I might not think of, they would know. Of course, my future daughter-in-law was able to ask questions about my options, which was really good.
What I liked is that my oncologist was very open and took the time to talk to the 3 of us and answer questions. I’m a layman. Even though I worked for City of Hope, I was a secretary. Then she wrote on a piece of paper and was able to show them because they could relate, and they knew more of the medical terms. I was just thinking chemo, and she was talking about immunotherapies and CAR T-cells and all this stuff. That’s why she gave me options.
When my oncologist was explaining, she said that there was the standard Rituxan. She said that those drugs had advanced so much since the time before. There are so many different improvements. Rituxan has improved a lot, and even the ibrutinib had improved.
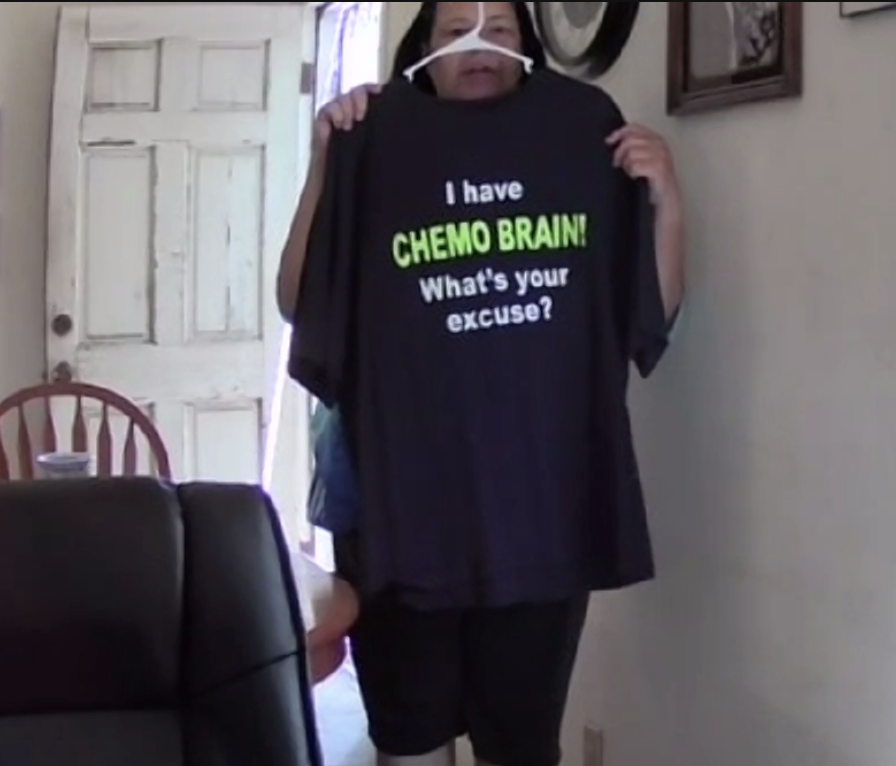
I was leery about that one because of the side effects, but she said they had worked out some of those side effects. The chemo brain was one of those that was like one in 1,000, and of course I happen to be one of those in the 1,000 that had that one. I had it really bad.
Chemo brain
Chemo brain is something for some reason some cancer patients have, and I unfortunately was one of those that had it. I’m talking to you, and then it feels like somebody just put up like a black sheet of paper in front of me, and I have no memory.
You can say, “Cherylinn, we were talking about X, Y and Z,” and I won’t remember. I won’t remember at all, and you’ll have to just talk. Sometimes it can be really scary. Working, especially working for a chairman, that was not a function that I could do. I couldn’t be talking to a patient or somebody on the phone and then all of a sudden be clueless. That was one of my concerns now.
Clinical Trial and Stem Cell Transplant
Clinical Trial Options and Requirements
Treatment options
She mentioned the Rituxan, and then she also mentioned CAR T-cell. I knew a little bit about it. The CAR T-cell, even though it’s a really good therapy, is kind of like the one that you use as your last resort because it’s so potent. You want to really keep that until when you’ve exhausted everything else.
CAR T-cell therapy
My son or future daughter-in-law had asked, “What about the CAR T-cell?”
“That one is a good one,” she said, but she wanted to try other options first and save that one. Like I said, mantle cell is a cancer that’s going to come back. That’s reality. I’d rather keep that one in the back burner. At that point, when the Rituxan doesn’t work anymore or this doesn’t work anymore or there’s nothing out there, then we have that as an option.
»MORE: Read more patient stories and info about CAR T-cell therapy
Clinical trials
There were 2 clinical trials that she had talked about. She said there was one clinical trial where it was an immunotherapy plus a chemo drug combination. Then there was another clinical trial that was just an immunotherapy that was specifically made for mantle cell. When my son and Melissa and I were talking about it, I seemed to gear toward trying the clinical trial.
With anything, we have a chemo drug like Rituxan. It kills everything. It kills the good cells and the bad cells. I’m older, so I want to make sure that if I have good cells, I want to keep those good cells. The clinical trial was made specifically for mantle cell. For me, it seemed like a logical choice to try the clinical trial.
With clinical trials, a lot of people think that some people get placebos and some people get the drug. No. What people have to understand with clinical trials is that everybody is going to get the drug.
It’s just to see how well it works and how it affects people. That’s why it’s always good for people to understand that clinical trials are not where some people get placebos. Everybody gets the drug to see how it’s going to affect you.
»MORE: Read more on FDA approvals of clinical trials
Deciding on the clinical trial
She was really good at explaining the clinical trial, the one that had the drug and the chemo. If I had done the Rituxan, it was going to be the same thing. It was just a general non-Hodgkin’s chemo. It was the immunotherapy plus the chemo.
I have a daughter, and I have a granddaughter. Will this affect them down the road?
It had really good results, but then when she said they had the clinical trial that was specifically made for mantle cell, it just seemed like a no-brainer that I would want something that was specifically for MCL. I asked, “Okay, if you had to choose between the 2?”
She mentioned the one that was specifically for mantle cell. She said, “That one is more toward just for your type of cancer, but they all work. Any one that you want will work, but if you want the one that’s going to be specifically for the mantle cell, this is the clinical trial. That would be the best bet if you’re going that route.”
Requirements to get into the clinical trial
They did a barrage of tests. The EKG, the stress test, tons of blood work, tons of paperwork. Be prepared that you’re going to do a lot of paperwork. What’s good is that wherever you go, if you’re in a clinical trial, you have a clinical trial staff specifically outside of your oncologist who will walk you through it. They will literally sit there and walk you through all the paperwork.
One of the things that they had mentioned to me when I was sitting with them was genetic testing. I thought, “Well, wait a second. At my age, what good is genetic testing going to do?” They explained to me genetic testing would help future generations, especially within my family. I have a daughter, and I have a granddaughter. Will this affect them down the road?
With breast cancer, my sister had told me it may not affect her children — she had 2 daughters — but it might affect her grandchildren. I thought, “You know what? Yeah, maybe a genetic test, which I am going to have done, might help.”
»MORE: Learn more about the process of clinical trials from one program director

Clinical trial experience
Reactions to Treatment
Then you do the clinical trial. For that, your first round of chemo or the drug, you’re in the hospital environment. Like anything, the first time you take it, your body reacts.
That’s reality. I did have a reaction, but they were aware of it. They were able to help me. You had the typical throwing up and the fatigue. In my case, my liver enlarged, but they knew. That’s one of the reasons why you’re in the hospital. They’re aware of these, but it’s good for them in the clinical trial to note those things. The next phase they go into, they’ll know this might be something that happens. They may be aware of it all the time.
Reading through the informed consent document
They did sit with me and go through the pages, but it was like scanning. It’s like anything where you just scan it. They show you the important parts of the paperwork. I actually did sit and read, and there were a couple of places I highlighted. Luckily, I was through the portal of City of Hope. I emailed my doctor and said, “I saw this and this and this. Should I be concerned about this?” Then she responded to me with an answer that made me feel better. I thought it was good.
Financial obligations
Because it’s a clinical trial, I haven’t had any costs for myself. It might also be the type of insurance. Because of my age, I’m on Medicare. Also, because I want to continue to go to the City of Hope, I have a Blue Cross supplement. I haven’t had to pay for anything, but I think it’s part of the clinical trial that the lab work and everything is covered.
Reporting symptoms
For any symptoms that you have, anything that is out of the norm, they ask you to call them and let them know. This way they can say, “Okay, yeah, maybe this might be related,” or “No.”
For some reason, I had really bad headaches. I could take Tylenol, so once I took the Tylenol, the headache went away. I made sure that they knew that I was having headaches.
For some reason, I was always hungry. I was on a weight management program. I had lost 40 pounds, and I was so excited about losing the 40 pounds. I’m on this chemo, and I’m thinking, “I’m not going to be eating.” Then all of a sudden I’m eating, and I’m hungry. I put on like 6 pounds.
They told me to be concerned about my weight, but not to dwell on the fact that I was gaining weight with it. That was one of my side effects, so I don’t know if being hungry is a positive or a negative thing.
Reporting and treating side effects
I would journal my symptoms, and I would email my oncologist. I would say, “This is what’s going on.” I woke up one day, and I couldn’t stand on my left leg. It wasn’t related. I have neuropathy. It was one of those things where I talked to her about it, and then I talked to my pain management doctor. We were able to get me a medication that relaxed the muscle.
I had the chills and the high fevers the day after treatment, and I ended up in the the triage and emergency.
I sat at home thinking, “Is this related to the chemo, or is this just my body?” I let them know that that was what was happening, that I was having pain in my left leg. It was resolved within a few days by just taking medication.
That’s one of the things with the clinical trials. You have to let them know, because what if it was a symptom, and you didn’t tell them? Don’t feel like you’re bugging them. If you say, “Hey, you know what, I have tingling in my right arm,” let them know it because then they can note it.
Then they can work with you to find out what the tingling is. Is it related to your treatment, or is it just something happens to people, especially when you’re older?
Cytokine release syndrome (CRS)
I had the chills and the high fevers the day after treatment, and I ended up in the the triage and emergency. I ended up in the emergency room, but it turned out that my PICC line was infected. They had to take that out, but I think it was a combination of both.
Then again, I had the chills. I thought, “Oh, I could just deal with it at home,” but then I called. I live alone, so I had to call my son, and he lives like 10 minutes away. He took me in because I was running a fever, like 101, and I had the chills really bad. They just kept me, they hydrated me, and then I was able to go home later on that day with antibiotics.
»MORE: Read patient PICC line experiences
Looking Toward the Future
Helping future patients
That’s the whole point of a clinical trial. If I call them and I’m telling them all these different symptoms, it might help the next phase and the next group of people, and they might be able to find out what is causing the chills and what’s causing the headaches. That’s what they do. They tweak it so that they know that for the next phase. They already are aware that these people have had those symptoms.
No question is a stupid question.
Usually within a day or 2, I’m back to normal. I walk my dog. I live in the mountains. I’m back to walking her again. Now I’m on the next phase, where I now get the chemo every third week. For 2 weeks, I’m pretty much back to normal, where I can exercise. I can maintain my weight program and just do the normal things that I’d normally do. Next week I’ll have my treatment. I know the reality is for a couple of days I’m going to be tired, and then I’ll be back to normal.
What guidance do you have for others about clinical trials?
Trust your group. Trust that they will keep you informed. I’m always a person that believes in gut. You’ve had those doctors that you go in, they don’t even look at you, and then they walk out, and you’re sitting there thinking, “What happened?”
I like the clinical trial group that I’m in. She will answer my questions, and if she can’t answer it, my oncologist and her physician’s assistant always will respond to me with whatever questions or concerns that I have and let me know, “This is what we’re going to do.”
Now I want to have a port put in my chest because I don’t have a PICC line. I said, “What are my options of having a port put in?” If you have those kind of questions, no question is a stupid question. Ask the question, and they’re going to give you an answer, one way or the other. It may not be the answer that you want, but they’ll answer.
I can prove to somebody else that it’s not a death sentence. If you have goals in your life, keep your goals.
For instance, they said, “You can’t drink alcohol while you’re in the clinical trial.” I’m not a drinker, but it’s funny. It’s like telling a kid they can’t have a cookie. When they tell you you can’t have alcohol, all of a sudden you’re like, “Today’s really hot. I would love to have a beer.”
You just understand that during the clinical trials there are certain things that they ask of you, and there’s a reason for it. I understand that they’re not asking you not to drink alcohol because they don’t want you to drink it. It’s because there has to be a reason. That’s why for me, it’s okay.
Going back to school and reaching goals
I was going to school, and I could have just said, “What’s the point?” I didn’t. It was a goal that I had put for myself, and I didn’t want the cancer to stop me from doing what I wanted to do. I got my bachelor’s, and then I wanted to pursue it. I wanted to get a master’s in a field that I knew at the time there would still be positions open.
I got my master’s in HR. Because of my work with cancer patients, I thought about getting a master’s in psychology. Maybe it would give me some little bit of insight into what’s going on with people, and maybe it might help me with talking to people.
It was hard because there were times when I had to take a leave of absence from school. By then, it was online. My bachelor’s was going to a classroom, but both master’s degrees were online, so that was easier. I still had to take medical leave.
One time one of the doctors at City of Hope asked me, “What’s the point?”
I said, “I didn’t want to give up just because I had a disease.”
I wanted to prove to myself that I could do it. I can prove to somebody else that it’s not a death sentence. If you have goals in your life, keep your goals. Do them, because you feel so much better to succeed. I also wanted to show my kids that you could go to college. You could go on with your life. You don’t have to let that hold you back. That’s one of the reasons why I got my degrees.

Stem Cell Transplant
Autologous stem cell transplant
I got a stem cell transplant back in 2007. Ironically, I got that through UCLA. I used my own cells, so that’s autologous.
The doctor that I was working for at City of Hope, Dr. John Zaia, is a virologist. One day we just sat and talked about my disease. He’s the one who told me, “Your cancer is really aggressive. Why don’t you get a stem cell transplant?” I didn’t even know it was.
I called up my oncologist, and I said, “I have a bone to pick with you. Why didn’t you do this?” He said I did so well he didn’t think about it. Then he thought maybe this should be an option. Because of my insurance, he sent me to UCLA, and they did the test.
It was already 6 months after I had finished R-CHOP, and they were like, “Well, maybe we shouldn’t do this.” Dr. Pinter-Brown is just awesome. She said, “Let’s just do the test and see if you’re a good candidate.” It turned out I was, and that’s when they decided to go ahead and do the stem cell transplant.
»MORE: Read patient experiences of stem cell transplants
Testing for candidacy
[Testing] was blood work and an MRI to show that the cancer wasn’t back. They wanted to make sure that I was still in remission to do it, because normally a stem cell transplant is done within a month of when you finish chemo. This was like 6 months later, so that’s why it was like, “Let’s see if you’re still a good candidate.”
Stem cell transplant experience
It’s changed so much since 2007. In 2007, I was in the hospital in isolation for like 6 weeks. It was horrendous, because you get like 3 or 4 times the dose of chemo, so you have no immune system. I had told nobody to visit me because I didn’t want to take a chance. They said even if somebody sneezed and I was to get an infection, it’s life and death.
For me, it was really hard because I did have a lot of the symptoms. I had the cold sores in my mouth and a rash. At one point, it was so bad that I actually was put into a coma because the pain was just too bad.
It’s changed now because now people are doing outpatient. It’s changed so much since when I was in, because you had to be in isolation for like 6 weeks.
»MORE: Read in-depth patient stories and background on mantle cell lymphoma

Inspired by Cherylinn's story?
Share your story, too!
More Mantle Cell Lymphoma (MCL) Stories
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: None
Treatments: R-CHOP chemotherapy, rituximab
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: Elevated white blood cell count
Treatments: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Hives, inflamed arms
Treatments: Calabrutinib, Lenalidomide, Rituxan
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Fatigue, enlarged lymph nodes
Treatments: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD




One reply on “Cherylinn’s Stage 4 Mantle Cell Lymphoma (MCL) Story”
Cherylinn your journey is heartfelt & so inspiring! You’re a true warrior with strength that goes beyond human understanding! I do believe God has His hands on you and I love how you’re paying it forward, by being there for others in need! You are making all that you go through really count for your loved ones & those who are walking their own challenging journey, no matter how painful & difficult it becomes. Cherylinn you are truly making a difference in this world! You are fighting the good fight. Never give up hope & keep looking up to the one who loves & created you! Thank you for sharing your soul with us. I had no idea of all that you’ve gone through…you’ve enlightened me! I love you my Dear cousin & I’m sooo proud of you & Blessed to have you in my life! Love & Blessings forever, Barbara