Jude’s Stage 3 Typical Multiple Myeloma Story
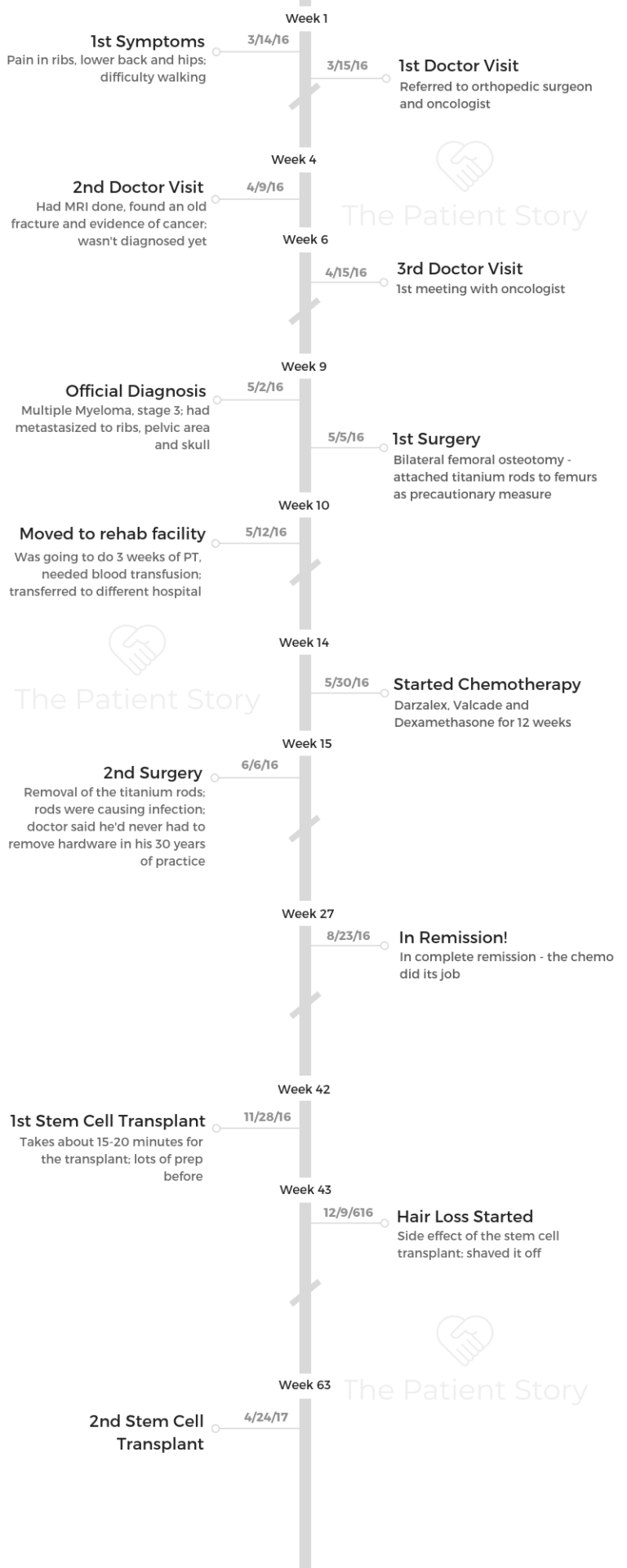
Jude shares her stage 3 multiple myeloma story, which started after she experienced pain in multiple areas of her body. She details undergoing extensive treatment, including surgery, immunotherapy, targeted therapy and two autologous stem cell transplants.
Explore her story below, where Jude also highlights how she navigated life with cancer, including the need for self-advocacy, managing through hair loss, and the support that got her through the entire experience.
- Name: Jude A.
- Diagnosis: Multiple Myeloma
- Staging: 3
- 1st Symptoms:
- Pain in ribs, back, and hips
- Difficulty walking
- Treatments:
- Surgery
- Bilateral femoral osteotomy (insertion of titanium rods to both femurs)Reversal of osteotomy due to infection
- Anti-CD38 Monoclonal Antibody Darzalex or daratumumab
- Targeted Therapy: Velcade or bortezomib
- 12 weeks
- Steroid: dexamethasone
- Once a week
- 2 Autologous Stem Cell Transplants (SCT)
- Surgery
Find a doctor you trust first and foremost. You’ve gotta love your oncologist, trust your oncologist, and believe in your oncologist. Don’t be afraid to get a second opinion. Don’t be afraid to fire your oncologist. Stay positive.
Cancer sucks. It really sucks, but you have the power to squash it by staying positive and doing all the things your body needs.
There are four big things to keep in mind. Nutrition, exercise, hydration, and perhaps most important: sleep. Your body needs to sleep to regenerate itself.
Jude A.
- Diagnosis
- Surgery & Recovery
- Treatment Regimen (Daratumumab + Bortezomib + Dexamethasone)
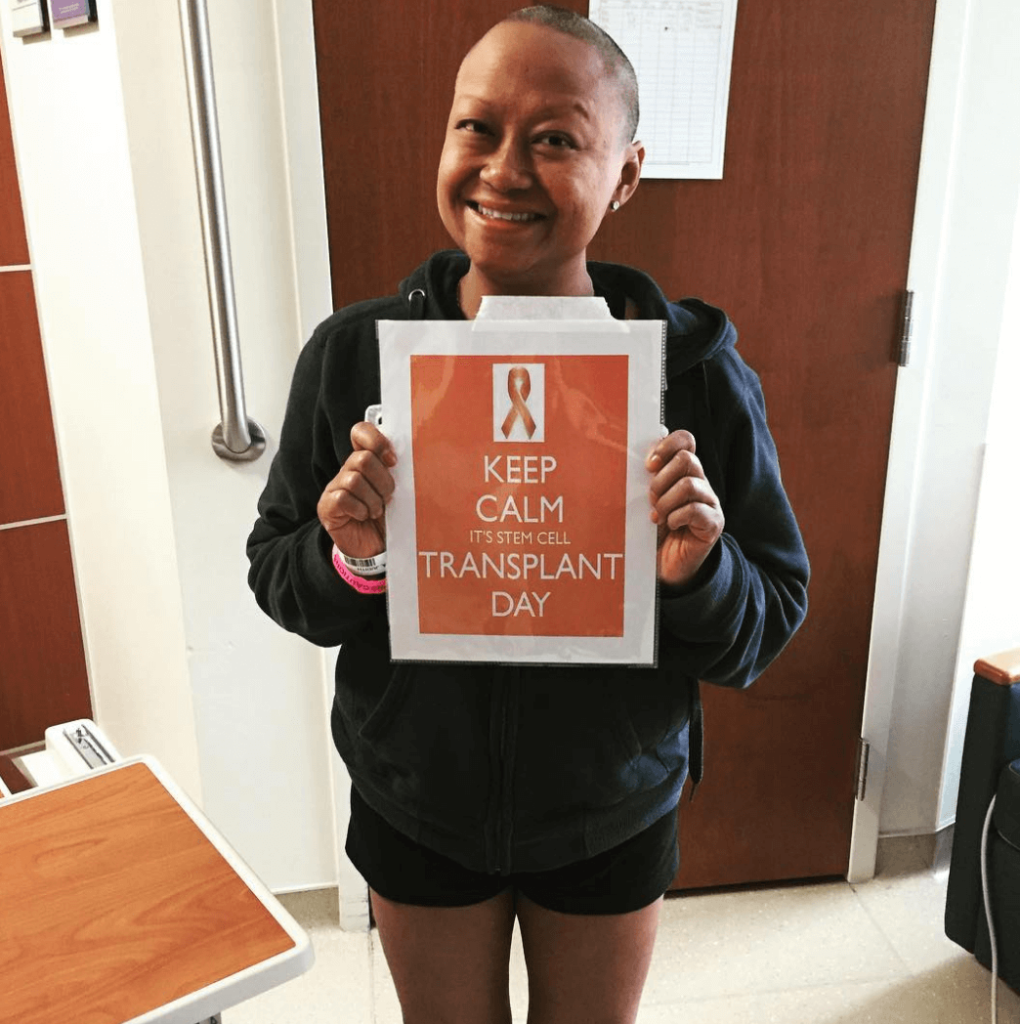
- Autologous Stem Cell Transplant
- Remission
- Reflections on Treatment
- Mental, Emotional and Physical Support
- How important was it to have caregivers during treatment?
- Did you ask for help when you needed it?
- Financial toxicity: paying for cancer treatment
- Did anyone give you a gift or service that made your life better or easier?
- Can you describe your new normal after cancer?
- Advice for someone who has just been diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
It started with some lower back pain, and then everything escalated. My hips, my back and my ribs all hurt. I eventually had extreme difficulty walking or maneuvering at all. It wouldn’t take me an hour to get from a standing to sitting position.
The pain was just so bad, but I muscled through it. I thought it was stress.

Describe the first doctor visit
I was going to school. I had quit my job as an event planner. I had been in the restaurant industry for 25 years.
I decided that I didn’t want to do that anymore. I decided to go to school for massage therapy.
When I was in clinic, I was stretching one of my patients, and I couldn’t get up afterwards. I muscled through it, and I finally got back up.
A couple of days later, I had to cancel clinic. My teacher, who was the owner of the school, said, “I can’t let you back in until you go to a western doctor.”
I had been treating everything holistically up to that point. I chose a doctor and got checked out. I needed a letter stating I couldn’t go back to school.
He finally came in, and I told him about my situation. He said, “I can’t examine your back. I’m going to refer you to a back doctor.”
Then I showed him a lump I had had for years. I had two mammograms before this. and both came back that it was nothing. He said he wanted to investigate that further, and he referred me to an oncologist.
How did your doctor tell you about the cancer?
I made an appointment with the orthopedic surgeon for my back. He did an X-ray and read it that same day. He looked at me and said, “Honey, did you break your back at some point?”
I said, “Not that I know of.” I was really perplexed. He said I had an old fracture, but there was also a dip in between my vertebrae. He ordered an MRI.
I did that on a Saturday, and I started training for my new job that Monday. I was popping Advil like Tic-Tacs at this point. Tuesday, I was in training, and I got a voicemail from my primary care physician.
He said, “Hi, Judith, I hate to be the bearer of bad news, but I just got off the phone with your orthopedic surgeon. You have cancer, and it’s metastasized.”
»MORE: Patients share how they processed a cancer diagnosis
Describe the MRI
You have to get an IV of some fluid, contrast dye. They tell you they’re going to push it and when they do, they tell you it’s going to be warm and feel like you’re peeing yourself. You’re not peeing in your pants.
I went into this tube, and it had a tropical-looking ceiling. There were these loud sounds. I just meditated. I’d heard that you feel claustrophobic. I don’t remember how long the scan itself was, but it wasn’t too bad.
It’s just this series of loud sounds, and there is definitely some claustrophobia. I just focused on my breathing and tried to relax and let the machine do its job.
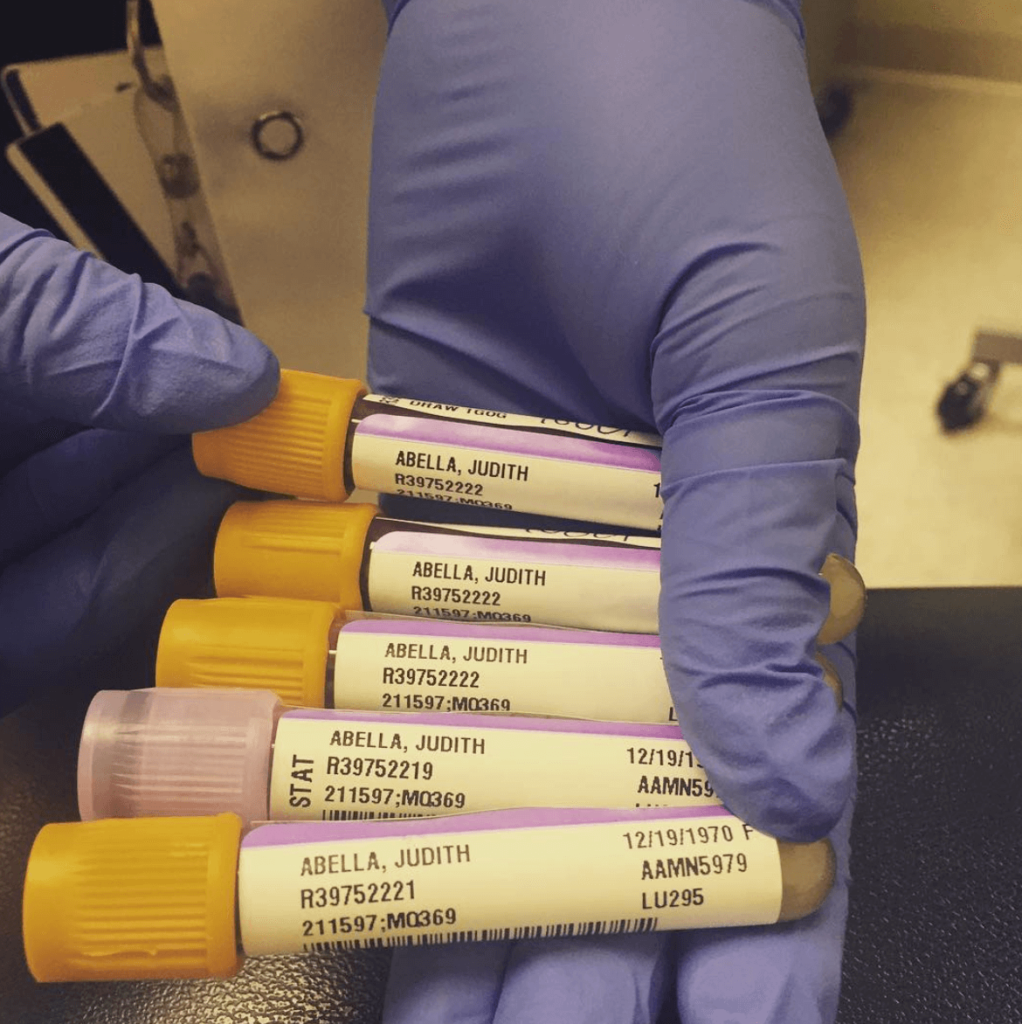
Can you describe the bone marrow biopsy?
It’s hell. It sucked. The first one I had, I was under. The second one, I can remember. They take it from the upper part of your pelvic area. They numb you up, and it’s like a plunger.
They make an incision in your skin, and they go into your bone. They pull the bone out basically, if you can imagine that. It hurts like hell. The pain just kind of radiated down my leg. I screamed bloody murder. They had to pump me up with lidocaine.
The worst part is you can hear it. You can hear them going through the bone. If I have to ever get one ever again, I’m going to ask them to put me under.
How did you react to the diagnosis?
I lost my mind. I’m training with people I don’t know in an unfamiliar area.
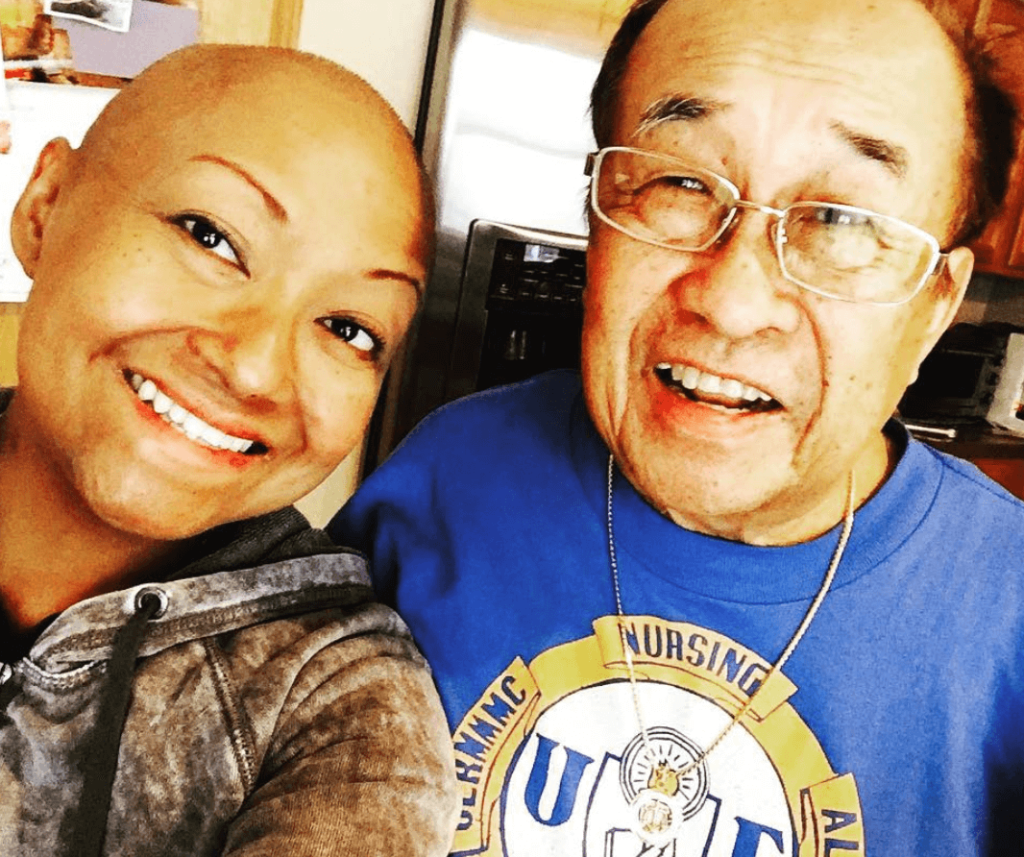
I excused myself, and I listened to the voicemail again. I was in shock. I called my dad, and I told him.
My dad said, “We’re getting a second opinion.” My sister called me and started wailing, and I called my other sisters.
I was in a lot of pain, and I was really concerned. My sister drove from Connecticut to Philly, where I was, on Wednesday night. She said, “I didn’t know your pain was this bad. I wish you would’ve told me.”
That Thursday, I told my boss I had been diagnosed with cancer and couldn’t work. My sister drove me to the airport, and I flew home to my parents.
Everything got very fuzzy at that point in time. I don’t know if my body and my brain were just shutting down because I was so stressed or what. I got to my parents house, and I talked to my primary care physician again.
»MORE: Breaking the news of a diagnosis to loved ones
How was the first meeting with the oncologist?
I had the appointment with the oncologist the following week. I remember being there at the appointment, but everything is very fuzzy. He was checking my glands. He didn’t know what kind of cancer I had at this time, but he knew that it had metastasized.
It was very aggressive, so they wanted to start chemo right away.
He said it wasn’t in my organs. I didn’t know if that was a good thing or a bad thing. The next thing I knew, I was really cold, and I was in the hospital.
They took me to the ER, and that’s when things got crazy. I was in so much pain and in and out of consciousness. The doctors there talked to my oncologist and said they needed to attach titanium rods to my femurs as a precautionary measure. I had done some X-rays, and the surgery happened pretty quickly, maybe a week or two later.
That’s when I found out the type of cancer I had. It was in my pelvic area, in my ribs and my skull, but they didn’t know where the source was.
Then they found out the source was in my ribs, which made sense to me because my ribs had been hurting for a couple of years.

Surgery & Recovery
Can you talk about the bilateral femoral osteotomy?
I was heavily sedated. I wasn’t super conscious, but I do remember being really really scared. I don’t remember signing the release papers. I’m a walker. I walked everywhere.
I questioned whether or not I even needed the rods, but the doctors said if I fell, the rods would protect me. My pelvic area was riddled with lesions.
I prayed a lot before surgery. I don’t believe in the church, but I do believe in God. The situation brought me back to those beliefs. I put my trust in the doctors. I had to trust that they knew what they were doing. I was scared.
What was the recovery from surgery like?
I was definitely in pain when I woke up. I could move a little, but it hurt. Since I felt so out of it, I started refusing my pain meds. All I was taking was Tylenol.
I was in the hospital for a week probably. Then I went to the rehab facility to basically learn how to walk again.
[Editor’s Note: Jude experienced an extremely rare infection and had the rods taken out.]
Describe the rehabilitation process
I was there for 3 weeks. I was doing physical therapy, and I had pulled this chest muscle. They would try to work me, and I was refusing.
I was in this very depressed mode. This was probably the loneliest time of my life.
The facility was super far from my parents’ house, so they could only come late in the day.
I wasn’t sleeping well because the nurse, whom I called my vampire, would come take my blood before the sun came up. It was so painful for me to move, and I didn’t want to do the physical therapy.
Chemo brain
My brain was so messed up when I was in there. I remember once they had a food show on in my room, and I had been in the restaurant industry for years, but I couldn’t even tell what the fire was supposed to be doing on this cooking show. It was like I was in this parallel world in a crazy state.
»MORE: Patients describe chemo brain
Trying to go home
It was a very lonely time. I was seeing things. I wouldn’t sleep in my room. I slept in the common room. Finally, I said, “I have to get out of here. I want to leave.”
My mom said, “You can leave, but you have to do the things they’re wanting you to do first.” I started doing my physical therapy. I was able to actually walk again.
»MORE: Getting mental support when leaving the hospital
Blood transfusion
The rehab facility rushed me to the hospital because I was complaining of heart problems. That’s when they realized that my blood viscosity was way too thick. It was interfering with my thoughts.
They had originally thought I was in the beginning stages of Alzheimer’s because I didn’t even hardly know what food was.
They did a plasmapheresis because my blood was basically like tar. After that, everything became a little clearer for me.
They hook you up to this huge machine with all these bottles, and they circulate your blood. It took 4 hours. I felt very tired after. It was just long. I don’t think it hurt. I was just long and tiring.
I’ve had many blood transfusions because my hemoglobin was very low. Normal hemoglobin for a female is 12 to 15. Mine was at six.
Treatment Regimen (Daratumumab + Bortezomib + Dexamethasone)
Changing hospitals
I went to a different hospital for the blood transfusion. I was all bandaged up when I got there and in excruciating pain. They cut the bandages off, thank God, because they were so tight. They gave me morphine.
At this hospital, they didn’t know what they were going to do with me. They wanted to give me radiation. They wanted to put the rods back in.
Next thing you know, someone comes in late at night to my room and says, “We’re shipping you to another different hospital.” Hospital number 3. I was scheduled to have a second opinion there anyway, but I had canceled the appointment because of the infection.
I had overheard the first doctor at the first hospital talking about it, and she basically told my family, “If she doesn’t do this, she’s going to die.” That doctor was kind of a jerk. Her bedside manner sucked, and I couldn’t connect with her, so I didn’t feel good about it.
When I met the oncologist, he said he wanted to start chemotherapy the next day. He told me about this new drug called Darzalex that had been FDA approved a few months beforehand.
This man cured me.
What was your treatment regimen?
The first week I was on Revlimid and dexamethasone (with Valtrex). That was at the first hospital.
I was scheduled for my second, and that’s when I had the fever. I didn’t have my second round until I got to the third hospital. He put me on a different cocktail. It was Darzalex (daratumumab), Velcade (bortezomib) and dexamethasone.
The Darzalex was once a week for 12 weeks. Since it was a newer drug, he gave the informational pamphlet to my family, and I asked my sister what the drug did. She said it basically blankets the biloma cells, strangles them and kills them.
It wasn’t a true chemo. It was monoclonal antibody therapy. I didn’t lose my hair with this.
»MORE: Learn more about targeted therapy

What side effects did you experience?
I remember that the Revlimid made me feel a little sick and very tired. The Darzalex made me feel really hot about 30 minutes after they started the infusion. I had a bit of a fever, and I kind of lost consciousness for a bit.
They stopped the chemo, treated me, and then started it up again. The first session of that took 8 hours because of that. It made me feel super tired as well.
The second session, a week later, was done in 4 hours. I would say the average infusion took five hours. The Darzalex made me feel extremely wiped out for a day or two after, but other than that and some diarrhea, it was okay. I tolerated it pretty well.
Dexamethasone is a steroid, and I hated it. It had the opposite effect on me that it should have. It made me exhausted instead of wired. It also made me very puffy, and I had some hyperpigmentation. I asked my doctor about that, and he said it was normal and would fade.
I hated the Velcade because it was subcutaneous, so I had a lot of bruising with that.
Did anything help with the side effects?
They gave me Zofran for the nausea, and I was still on morphine at the time. I logged everything. I journaled about how I was feeling and everything I ate.
If there were 4 things that I could tell people to do, that would be eat, hydrate, exercise and sleep.
Your body needs fuel to fight. I always had a big breakfast. I numbered my cups of water to ensure I was drinking enough.
I forced myself to get out of bed and walk. I had to do PT as well for the thigh surgery. They wanted me to exercise and walk. I walked around the nurses’ station.
It was hard to sleep being hooked up to so much stuff, but I tried my best to sleep.
I had a really big fear of going home because I couldn’t do stairs. I tried to manipulate the system and spend more time in the hospital because I felt safe there.
My oncologist told me, “You’re going to be fine. Everything is fine.” I was scared that if I fell, my parents wouldn’t be able to do anything because they were elderly. He really pushed me, though, and he knew my strength better than I did.
Autologous Stem Cell Transplant
Preparing for the stem cell transplant
I didn’t really know what I was in for. It starts with Day -2, Day -1, and Day 0 is when they give you your stem cells.
I used my own stem cells. We had to harvest them, so probably about a month before I had a series of tests and harvesting.
Prior to the transplant, I had to get a PET scan. I also had an enlarged heart the first time. The right side of my heart was enlarged on my echo.
They didn’t know what it was, so that was a scare. I had to see a cardiologist. They put me on a diuretic, and within a week or two it was better. Then I went in for the transplant.
»MORE: Learn more about stem cell transplants
Harvesting stem cells
Prior to harvesting, I had to inject myself with Neupogen. It’s subcutaneous. I had to give it to myself in my thigh.
It basically ramps up your stem cell count. I think I did that for 3 days, and then I went into the center to harvest. That’s an all-day thing.
You sit in a chair hooked up to a machine that looks sort of similar to a dialysis machine. It takes your stem cells and cleans them. My stem cells were so active that they were able to collect enough for three transplants.
I’ve heard there’s a certain amount you have you have to collect.
Some people have to be there for weeks, but I was very fortunate that I only had to be there for one day. Harvesting was fairly easy for me.

Recovering from stem cell harvesting
You feel like crap. I didn’t want to get out of bed for a few days. I was super tired, and all the side effects happened. I got diarrhea. I lost my taste buds for about 2 weeks. Luckily, I didn’t get any mouth sores.
The worst part was the vomit, though. I hate to vomit. That happened after the first week. I had some throat problems, too. I felt like there were lumps, and I couldn’t swallow very well. They were giving me things for that and the nausea. It was pretty horrible, though. I couldn’t eat.
They said that I had to gain 10 pounds before the transplant because they knew I would lose weight, and they were right. I was super thin.
Once I was able to eat, they put me on a low-bacteria diet. It’s basically a processed foods diet: no salad, no fresh fruit without a peel, no cheese. I could eat chips, donuts and cake. That wasn’t a diet I was accustomed to.
Chemo before the transplant
The first 2 days, they give you chemo, a true chemo drug called melphalan. What it does is it wipes out your whole immune system. They want you to eat a lot of popsicles and ice chips because you can get mouth sores from it.
Describe the stem cell transplant process
On Day 3, they give you the stem cells. They say that you smell like garlic, but I don’t know if that’s true.
When they give you the stem cells, it’s really pretty cool because you can see them going down the IV.
That process only took about 15 to 20 minutes, but that’s when all hell breaks loose because all of your numbers start to drop.
Recovering from the transplant
I was in recovery for 2 weeks, and during that time they want you to exercise. People had to get gowned up to see me. They say not to have visitors, but my oncologist okayed it for me.
Second stem cell transplant
About 6 months later, I had a second one. The second was worse than the first one. I think it’s because I knew what I was going to go through. The side effects came earlier.
I was a lot lonelier the second time because my mom was sick, so I was at my sister’s house alone after getting out of the hospital. I didn’t have anyone to converse with, and I was very weak.
Remission
Complete remission after the transplant
I was set to be discharged on August 23rd. Right before that, they did a bone marrow biopsy on me. That Friday, I had my last session of chemo, and then they did the biopsy. That was going to tell just how well the treatment did for me.
I was sitting there after ordering breakfast waiting for the rounds of doctors.
He comes in and says, “You are unequivocally in complete remission.”
Prior to that, he said I was either going to be in complete or partial remission. He came in and did his normal tests and said that, and I just sat there.
I didn’t know how to react. I was eating my breakfast, and I don’t know how to describe it. I don’t know if it was shock, pure joy or denial. I sat in silence for a while. I had to wrap my head around the fact that I was going home and in remission.
My goal was to leave that hospital with zero or little assistance. I had been walking with a cane at least, but I walked out with no help.
Follow-up protocol
I’m not on a maintenance drug, but I should be. I had an allergic reaction, and I had to come off of it. I asked my oncologist about it, and he said there were other options, but I would likely either have a similar response or have to be on a steroid, which I really didn’t want to do.
He suggested that instead of the maintenance drug, he just wants to monitor me closely. With that, so far so good.
As far as my numbers go, they’ve been pretty good. It went from seeing him once a month to once every 3 months, and now I’m just waiting for the once-every-3-months mark.
Reflections on Treatment
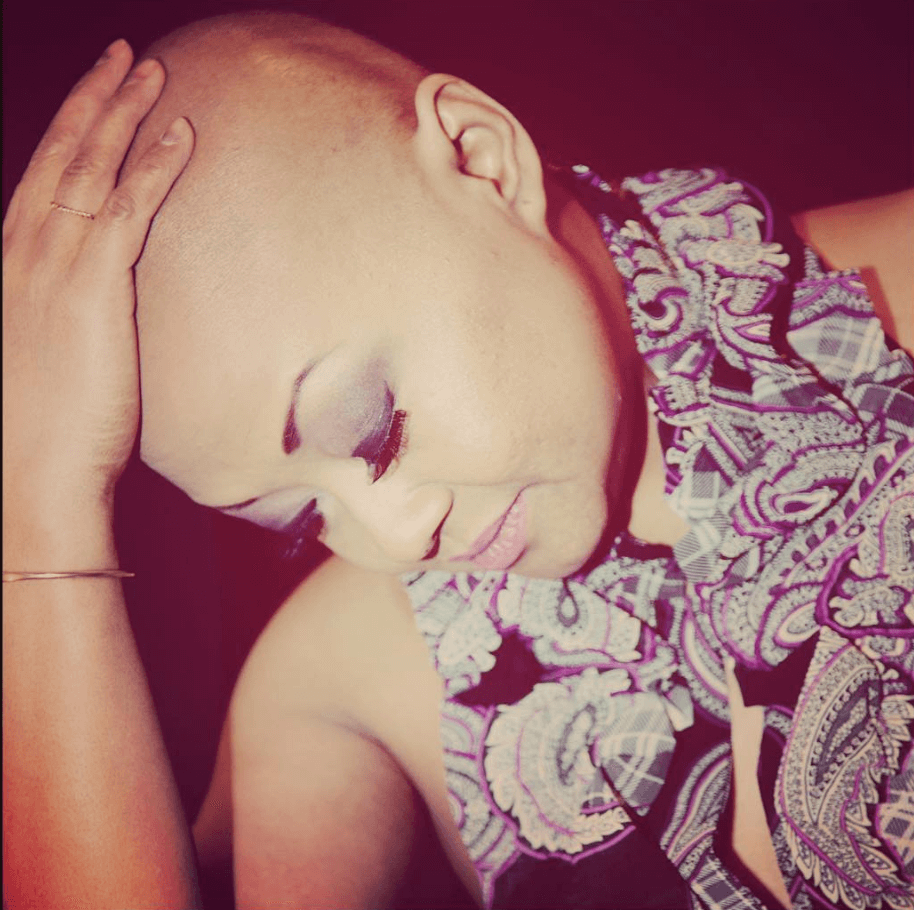
When did you experience hair loss?
The first week after the first stem cell transplant. I had long hair, and it would come out in clumps. I had asked if it was definite that I was going to lose my hair, and they said yes. When it started falling out, I was taking it and wrapping it up. I didn’t get it cut until after the fact.
It was in one huge dread in the back of my head. When I got out, I went to my hairdresser, and I had a little shaving party. I thought I looked hideous bald, so I went to the American Cancer Society and got a bunch of wigs.
»MORE: Dealing with hair loss during cancer treatment

Did you like the wigs?
I didn’t even wear the wigs. They were a hot mess on my head. I started to kind of like my bald head. I got a lot of compliments on my bald head.
It was winter when this was happening, so I’d wear a beanie all the time. When I’d take it off, people would say, “Hey, you have a really nice head!”
So, I embraced it. I embraced my bald head.
I had always had bangs, so not having bangs was a big deal, but honestly? I rocked that bald head. One of my friends got me to send her a picture of me with the bald head, and she sent it back to me with a side-by-side comparison of me and Amber Rose.
I didn’t know who she was. I had to Google her, and I was like, “Wait, she’s a stripper! I look like a stripper?” I was like, “You know what? I’m gonna rock this.” I accepted it and found beauty in it rather than being scared about it.
I had 12 wigs. I wore one probably twice. The baldness was part of my process. I had a professional photographer do a shoot with me. I wanted to document my journey.
The bald head was part of my war wounds. It’s like when my mom would tell me to get cream for my scars on my thighs from surgery.
I’m like, ‘No way. This is me saying I fought and I won.’ It reminds me to tell myself every day that cancer is not going to get me.

Was there anything that took you by surprise during treatment?
I didn’t have any expectations, so I think that may have helped. I did always feel like I was a special case, though. At first, they didn’t know what kind of cancer I had.
The rods had to come out. That was a big surprise. They couldn’t figure out my infection, so I was always hooked up to something.
People couldn’t enter my room without a gown and gloves. I couldn’t be touched. That was a big deal. That was the other thing that sucked. Nobody could touch me. As far as really big surprises, though, not really. Everything seemed to be a surprise.

How did you cope with the loneliness?
I lost a lot of friends in the process of my journey. You find out who your real allies are. I think I like being alone, but I don’t necessarily want to be alone.
In 2018, I finished school. That was a really big goal of mine. When I got diagnosed, I had a month left of school, but then I got diagnosed with cancer.
What kept me going and healing was hustling for myself. I wanted to prove to myself that the vision I had was going to come true.
I’ve finished school now. Sure, there are days even now where I don’t want to get out of bed. I feel bad. I just don’t wallow in it for very long. I wanted to travel again. I wanted to do all these things. That’s what kept me going.
Were there times you felt like you had to advocate for yourself?
Not during treatment. I wasn’t strong enough at the time. I couldn’t. The doctor that left me the voicemail about the diagnosis, though, I gave him a piece of my mind.
Sure, I checked the box that he could leave me a message, but the way he went about it was awful. I let him know how I felt about that.
»MORE: Self-advocating as a patient
Finding the right doctor
I love my current oncologist. I ask a lot of questions, and he’s great. I connect with him. He practices in a way that I think I would. He knows me now and knows I think ignorance is bliss. He tells me what I need to know and not what I don’t need to worry about.
Some of those doctors, though, they were awful. If I didn’t like them, they would know. I would definitely say something. I tell other people all the time, “It’s not wrong to get a second opinion.”
My second opinion doctor is now my doctor. If you have doubts, always ask questions. Educate yourself. Yeah, they are professionals, but they’re humans. Humans make mistakes.
My current oncologist has told me that if I had come to him first, he would’ve never put rods in my thighs. That’s a hard pill to swallow, but I just have to go forward.
With your doctor, you have to love your doctor. You have to believe in your doctor. The mind is a powerful thing. What you feed it, you’re feeding your body.
If you don’t like your doctor and are thinking about how bad they are, you’re probably not going to respond super positively to the treatment they prescribe. Find a doctor that you trust and that is truthful and doesn’t sugarcoat.
Mental, Emotional and Physical Support
How important was it to have caregivers during treatment?
100%. I couldn’t have done it alone. As much as I like being alone, I couldn’t have done it without them. The support of my family was so important.
What sucks about it, though, is I’m the first one in the family to have cancer. As much as they tried to understand, they couldn’t fully.
That’s when and why I found a support group. That was a very integral part of my healing. I always advise people to find a support group.
It’s so important for you to find people who can identify with what you’re going through and listen to them talk about their experiences as well.
Did you ask for help when you needed it?
No. I didn’t because I was stubborn, and also because my parents were older. My dad just passed away in April, so now it’s just my mom and I.
I never asked my parents for physical help. Mentally and emotionally, though, they helped. My mom would visit me every day.
I liked my quiet, and she always had the TV on, but she was there for me. We never had deep conversations or anything, but she was there for me.
She was just physically there for me. That was great for me.
»MORE: What kind of support cancer patients say helped the most
Financial toxicity: paying for cancer treatment
I was pretty much unemployed when I got cancer, so I had Obamacare. Right before I got sick, I had picked a policy. I never planned on using it, but I was very fortunate.
The plan I picked helped me. I also applied for Medicaid. Since I was unemployed, that helped as well. On the insurance front, I was very fortunate.
»MORE: Learn more about benefits available
Did anyone give you a gift or service that made your life better or easier?
I had two fundraisers. That was very generous and kind and mind-blowing. The generosity was overwhelming. That was very touching. My friend that came by and gave me reiki was amazing.
As far as physical gifts, people were very kind. I got coloring books and stuffed animals, but the best thing was the visiting. Feeling like someone cared and loved me enough to physically visit me was amazing. Of course, the calls and texts were great too, but the physical visits were a huge deal.
One friend in particular would come and say, “All I want to do is hold your hand and kiss your head.” I hadn’t seen this guy in 20 years, and now he’s one of my best friends. He would come and just hold my hand through the plastic glove. It was so wonderful.
The generosity of the physical gifts was very kind, but I think that anybody that reached out just meant so much. You never know how you’ve affected someone’s life until you’re in a situation like this.
Can you describe your new normal after cancer?
I’m much more conscious of stuff. I’ve always been a fairly positive person, but I am even more conscious of how powerful positivity is.
As much as my work is physical, it is gratifying. My mother always said I was a healer. Ever since I was in my 20s, my mom said I should go to massage therapy school.
I keep doing me, but I have to limit myself now. That can be a struggle sometimes. I don’t like not being able to do some of the things I used to be able to do.
For example, exercise. I can’t walk long distances like I used to. I can’t just go to the gym and be on a treadmill for an hour without worrying my hips are going to give out on me.
I’m very conscious of my pain levels. I’m in pain every single day. I deal with the pain. Sometimes, I’m in denial about things, too. There are things I have to do now to keep myself healthy, and sometimes I don’t want to do them.
I don’t want to take a handful of supplements every day or always have to make sure I get a certain amount of sleep, but I have to keep myself healthy.
Being a massage therapist, I preach self-care. I have to practice it myself, too. My new normal is also educating other people to be their best.

Advice for someone who has just been diagnosed
Find a doctor you trust first and foremost. You’ve gotta love your oncologist, trust your oncologist and believe in your oncologist. Don’t be afraid to get a second opinion. Don’t be afraid to fire your oncologist.

Stay positive. Cancer sucks. It really sucks, but you have the power to squash it by staying positive and doing all the things your body needs. I had stage 3.
It was really aggressive, but I always felt that I was going to beat it.
I also recommend getting some sort of touch therapy, massage or reiki if your doctor says it’s okay. We’re humans, and we need to be touched — even if it’s just a little hand massage.
There are 4 big things to keep in mind. Nutrition, exercise, hydration, and perhaps most important: sleep. Your body needs to sleep to regenerate itself. You have to keep a silver lining.

Inspired by Jude's story?
Share your story, too!
Multiple Myeloma Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...





2 replies on “Jude’s Stage 3 Typical Multiple Myeloma Story”
Does anyone have Jude A information? I would love to see how she is now. A
Hi and thanks for the story of Jude, very touching. I am a senior, male and for my journey, I was first diagnosed with Prostate cancer. Later it was noticed I had rising blood protein, then the term MGUS was used, That was 5 years ago, now it is MM in the after monitoring stage. Started treatment with the newer drugs, Darzalex, Revlimid, Dexamethasone. Having side affects including what is called Chemo brain/Fog, that is why I looked for answers here on online.