Carlos’ Stage 2 Light Chain Multiple Myeloma Story
Carlos shares his stage 2 light chain multiple myeloma story and undergoing major back surgery, induction therapy, stem cell transplant and maintenance chemo.
In his story, Carlos highlights dealing with losing his hair, the approach with fertility preservation, the impact of the cancer diagnosis on his marriage, and how he turned to natural, holistic approaches to help strengthen his health.
- Name: Carlos C.
- Diagnosis:
- Multiple myeloma
- Light chain
- Staging: 2
- 1st Symptoms:
- Back pain and spasms
- Treatment:
- Major back surgery
- Insertion of 2 titanium rods and 16 screws to fuse T1 and T2
- Chemotherapy
- Revlimid, Velcade and dexamethasone (RVD)
- 4 cycles
- Revlimid, Velcade and dexamethasone (RVD)
- Stem cell transplant
- Maintenance chemo
- Major back surgery
Everything is about today and maybe the upcoming year, but that’s as far as it goes. I’m still very optimistic.
I live as though I don’t have anything wrong with me and never did. Even though I do have certain pains, I just ride it out and enjoy life as much as I can.
Carlos C.

- Multiple Myeloma Diagnosis
- Surgery and Recovery
- Induction Therapy
- Stem Cell Transplant
- Quality of Life
- What’s been the hardest thing for you mentally and emotionally?
- Describe the hair loss
- Did fertility preservation come up?
- How did cancer affect your relationship with your wife?
- Do you have any advice for other married couples going through cancer?
- How important was it for you to have caregivers during recovery?
- Finding your cancer community
- What is your “new normal” after cancer?
- Can you talk about the natural remedies and healthy living you practice?
- What is your advice for someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
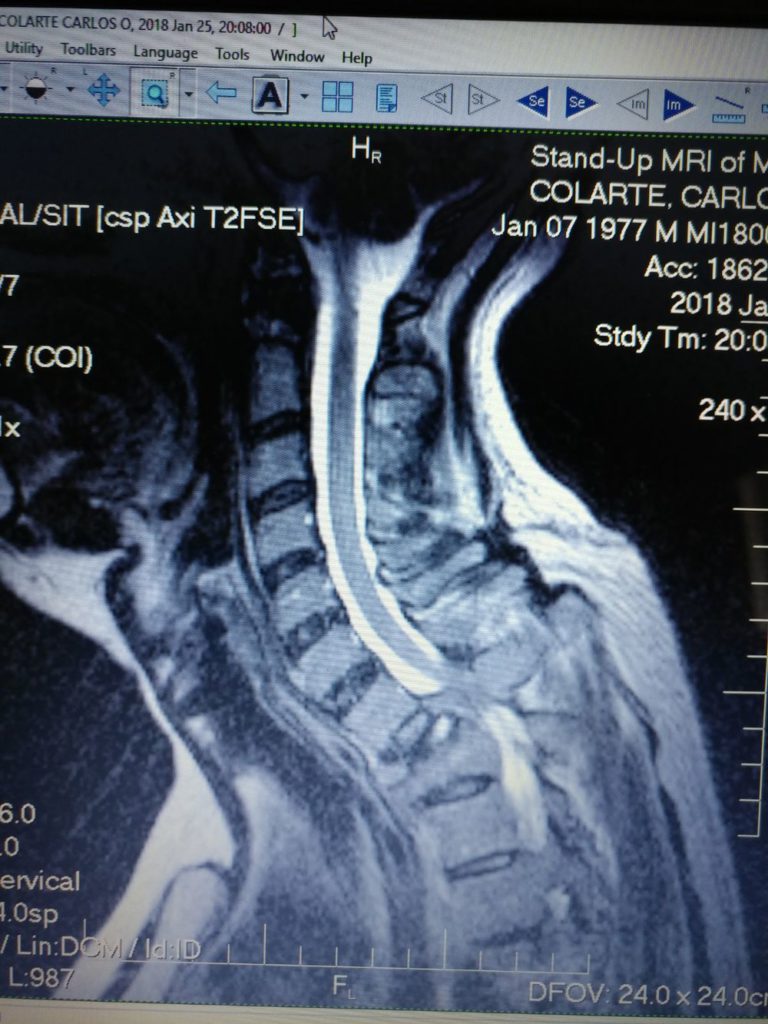
Multiple Myeloma Diagnosis
What were your first symptoms?
It all started with back pain. I had just turned 40, so I thought I was just getting older.
What made you go to the doctor?
One day, I was helping a friend move a TV, and I got a really bad back spasm. That’s the reason I ended up going to the doctor in the spring. I’m the typical guy that doesn’t go to the doctor unless it’s really urgent or necessary.
The doctor did an X-ray first and gave me some muscle relaxers. It helped for about a month. The pain came back, and I went to a specialist.
Getting scans
The orthopedic specialist ordered another set of X-rays and some steroids. In November, we traveled to New York for vacation, and something changed. A lump appeared in my upper back that increased the pain, so as soon as we returned to Miami, I went to the doctor again.
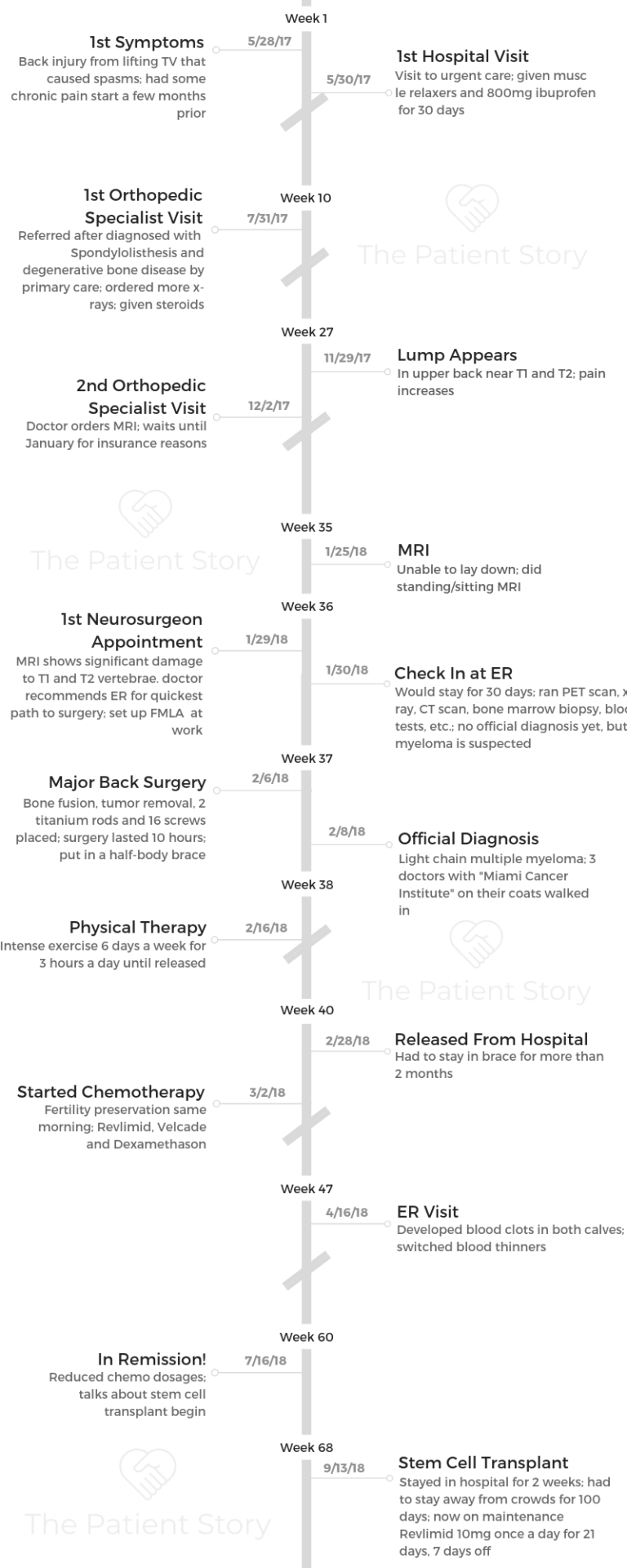
He scheduled an MRI, but by then it was early December. Because of insurance deductibles and the holidays, I decided to wait. In January, I was at the gym one day and lost complete strength in my left arm. I ended up finding a place that did stand-up MRIs because I couldn’t lay down on my back.
This was a Thursday, and the following day, the doctor called me and said he scheduled an appointment with a neurosurgeon for Monday.
Describe the standing MRI
It wasn’t as easy as I thought it would be. You don’t stand during the whole thing. You sit down in a very narrow seat. I actually couldn’t get through it on the first try because of the pain in my back.
The machine started scanning. I couldn’t sit still because of the pain, so I asked them to stop and ran out to my car to spray Biofreeze on the area.
I was able to go ahead with the MRI after this. Usually, people that do MRIs aren’t allowed to say anything to you, but she looked at me and asked multiple times, “Were you in an accident?”
I responded, “No.” I had no idea what was going on until Monday when I went to see the neurosurgeon and got to look at my scans.
Tumor found
She didn’t want to commit to a diagnosis because they have to look at the bone marrow biopsy to confirm it. She did say it was a tumor and that it could be multiple myeloma.
She told me I had a tumor that had devoured 2 of my vertebrae. The myeloma had eaten most of my T1 and T2. That was what was causing the spinal cord pressure that made me lose feeling in my left arm.
I knew whatever it was, it wasn’t good, because it was eating my bones. I was clear that whatever news I got wasn’t going to be good news.
When she told me to go to the ER, I told her I needed to go home and sort things out first. I went home and spoke to my wife, parents and manager.
I told her I would come back the next morning, and she said she would leave notes for the ER team. That’s what I did. I went back the next morning and checked into the ER.
What tests did they run at the ER?
If I would’ve fallen, I could have ended up paraplegic because my head was being held up only by the surrounding tumor. Half of my T1 and T2 were gone, so they put a neck brace on me immediately.
They performed some tests that day, but since I required surgery, they moved me to a room. For a week, they continued with multiple blood tests, X-rays, PET scan, CT scan and 2 bone marrow biopsies.
»MORE: Dealing with scanxiety and waiting for results
Describe the bone marrow biopsy
It’s a simple procedure.
You go into what’s just kind of like an office in the hospital. They apply local anesthesia, and it just feels like a shot in your back. It wasn’t super painful.
For about 24 hours after, it hurt me to walk, but that’s about it. I have a high pain tolerance, so I don’t know if it’s that way for everyone.
It’s obviously not enjoyable, but it’s really not bad. It wasn’t for me anyway. I don’t really mind needles, but for people who have a problem with them, I can see how it could be a nightmare.
How did you get the official diagnosis?
They had done a bone marrow biopsy before the surgery and also took some of the tumor that was removed for a biopsy. The results didn’t come in until about a week and a half after surgery.
They chose the subtle way of telling me by having three doctors with ‘Miami Cancer Institute’ on their coats. I already kind of suspected it, but that’s how they told me.
Surgery and Recovery
What do you remember heading into the back surgery?
I’m normally an anxious person, but the doctor was very comforting. Her presence and the way she handled everything gave me a lot of peace of mind.

I didn’t try to trigger the anxiety by asking questions. I didn’t want to know. I just put myself in her hands and trusted her.
I didn’t ask her what the surgery was going to be like. I just knew that I was going to have titanium inserted, tumor removed and bones fused. I just left it up to her and God.
It was a super long surgery. I was wheeled in around 5:00 a.m., and I woke up around 7:30 p.m. My wife told me that the doctor had walked out around 4:30 p.m. to tell her the surgery went well, but she said that it would take several hours to finish up. It was a very long process.
She basically had to fuse the vertebrae back together and remove as much tumor as she could. They inserted 2 titanium rods with 16 screws into my back. She wanted to make sure I had long-term back support.
Describe the physical therapy
In total, from when I went to the ER to when I left after physical therapy was about 30 days. For the surgery recovery, I was in the ICU for 10 days, and then I spent another 12 or so days in the physical therapy program at the hospital.
Half of my body was cut open basically. I could barely walk. I couldn’t lift my arms. My wife had to feed me. I couldn’t go to the restroom on my own. I had difficulty showering.
It was like being a baby. The physical therapy did help a lot. It was intense.
It was like 3 hours a day. They were teaching me to walk again. They wanted to make sure I could walk up stairs since I lived in a 2-floor home.
The brace they put me in after surgery was on half my body. I had to wear it 24 hours a day except for when I was showering. It was rough. The brace didn’t come off for 3 months.
I couldn’t drive. I had to be very careful. I had to sleep on my back. I didn’t have a lot of pain, but I did have a lot of muscle soreness.
Induction Therapy
Describe the first visit with the oncologist
After physical therapy, they sent me home. The next day, I had my first visit with the oncologist. He tried to explain as much as he could about multiple myeloma and the treatment he planned for me to go through. About 2 weeks later, I started chemotherapy.
Induction therapy regimen
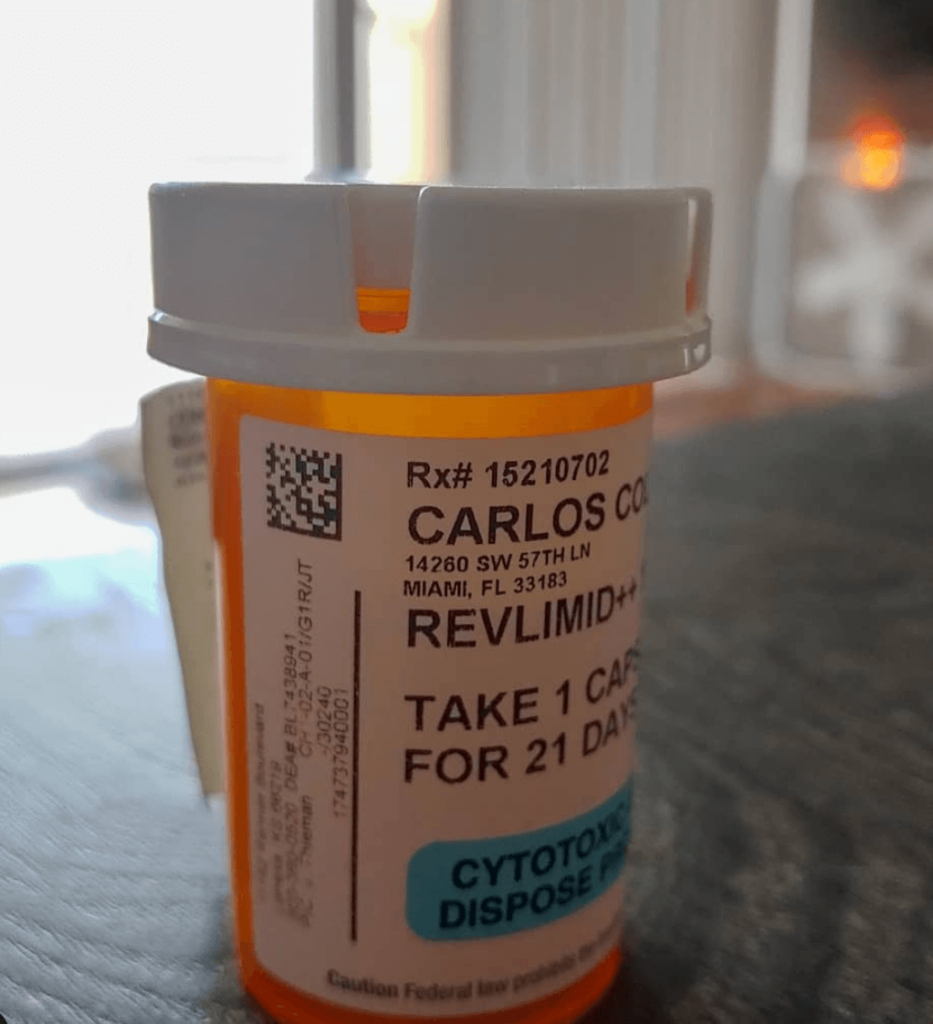
The doctor chose RVD, or Revlimid, Velcade and dexamethasone. That’s immunotherapy, targeted therapy and one steroid.
In total, I went through 8 cycles but reached remission after 4. Thankfully, the medication did what it needed to do pretty quickly. Once I went into remission, they lowered the doses as they prepared me for a stem cell transplant.
The Revlimid is a pill. I was taking it every day for 3 weeks and taking a week off. Velcade was 2 times a week for 2 weeks and 2 weeks off.
It’s an injection they give you at the hospital, and it goes into your stomach. That was definitely not fun. They inject it very slowly. It burns a lot.
Dexamethasone is a steroid that helps reduce inflammation to try and shrink tumors, but it makes it difficult to sleep at night. It was intense, especially in the beginning with the brace. I tried to keep a positive state of mind and do everything the doctor told me to do.
What side effects did you have from chemo?
I had a lot of different side effects. Besides taking the chemo medication, I was also taking muscle relaxers and pain relievers. The side effects we varied.
The steroid obviously caused some trouble sleeping. My pain reliever was giving me blurry vision. At one time, I got really anxious because I was just sitting at the dinner table and lost the vision in my right eye completely. I was having a lot of anxiety. Muscle relaxers, when you use them for a while, can cause that.
I didn’t have much nausea. Supposedly, the benefit of taking the steroid is helping with the nausea. I definitely had some chemo brain.
I experienced a lot of confusion and forgetfulness, and I had this sensation that I was wearing a helmet all the time.
I had some intestinal pain. A side effect that I would get the day after my Velcade was the hiccups. The first time I got them, I tried the usual known remedies like holding my breath and drinking water quickly.
After turning blue and drinking two liters of water with no results, I researched online and found that some hiccups may be caused by stomach indigestion. I took a Tums, and problem solved.
I also developed 2 blood clots, one in each leg at the same time. I started feeling pain in my calves that was similar to what you might experience after a muscle cramp.
I hadn’t really done any rough exercise or anything like that. I tried to use a cream for muscle pain, but it didn’t go away, so I reasoned that it wasn’t muscle related. I sent a quick email to my doctor, and they scheduled a scan that same day.
I went to the hospital, and the nurse came out with a wheelchair and said I needed to go to the ER. They gave me a blood thinner shot called Lovenox and changed my blood thinner.
The clots went away, but then the pain came back and lasted for a couple of months. I had to take medication for that for 6 months.
It caused a lot of anxiety, too, because I didn’t know if it was another clot or just the residual pain.
What helped you with your side effects?
I am a firm believer in eating well, and by that I mean eating for nutrition. Lots of organic vegetables, eggs and green juices, along with some fruits.
In addition, I do intermittent fasting. That’s when I eat 2 times a day, once at 1 p.m. and once at 7 p.m., which I read helps your cells clean out damaged cells, a process called autophagy.
Apple cider vinegar really helped me with any intestinal issues or heartburn. I took all types of different teas. I was already on enough pills, so I gave the alternative medicine thing a try.
In general, it really did help. Eating well and exercising, even if it was just a little bit every single day, was a big deal.
I would go outside and walk to get some vitamin D, which is extremely important for your bones and immune system. I believe all those things really helped to not feel as much from the side effects.
»MORE: Cancer patients share their treatment side effects
Did you work during chemo?
I don’t think I should have, but I did. The whole situation with the insurance and short-term disability is not a smooth process.
Requesting extensions was such a mission, and I was always afraid that I would lose my job.
When I came back after my 3 months of disability, I couldn’t remember anything I used to do because of the chemo brain.
»MORE: Learn more about chemo brain
I didn’t really notice it at the time, but later on when I was absent from work again for 3 months (after the stem cell transplant), I returned and remembered how to do everything. It wasn’t until then that I realized just how much all the medications had affected me.
»MORE: Read more on how others dealt with work after a cancer diagnosis
What happened after you finished your chemo?
After my fourth cycle, they performed the typical blood tests. My cancer indicators were all normal, and they declared me in remission. They also completed another bone marrow biopsy, and the result was 1%. I started with 18%.
I thought they would stop the chemo at this point, but they continued the cycles at a lower dosage for 4 more cycles, they stopped about 1 month before my stem cell transplant.
How did you feel when you got the news about remission?
I was ecstatic with the news, and the very first thing I did was call my wife and let her know. She was so happy to hear that everything we had done worked and that I was going to be okay.
I was also excited because I thought I would be done with chemotherapy, but to my disappointment it had to be continued until transplant.

Stem Cell Transplant
Planning for a stem cell transplant
The next step was determining where I was going to get the stem cell transplant. The hospital I was receiving treatment from had just started doing the transplants, and my insurance said they wouldn’t cover it here, so I had to go somewhere else. That’s when I transferred to the University of Miami.
How did you feel heading into the stem cell transplant?
The lack of information and data available about success and failure was difficult to deal with. I’m the type of person that likes all the information to take appropriate decisions, but unfortunately the best they could do was tell me that statistics show that patients who go through the stem cell transplant on average remain in remission about 13 months longer.
In the end, you go through the stem cell transplant, and they have no idea if it’s going to work, how it’s going to work, or for how long it’s going to work. It’s kind of like magic.
I know cases where people had a relapse within months of the transplant, as there are patients that stayed in remission above 5 years.
They do this big thing to your body and don’t know what to expect. It’s hard to believe in magic when it’s supposed to be science.
Describe the stem cell transplant prep
After reaching remission, they continued the same RVD regimen, just in lower doses. There are many tests they perform pre-transplant. They test your lungs, your heart, and even perform a psychological test.
About 2 weeks before the transplant, they placed a catheter port on me. I found this to be one of the worst experiences. They inject you with local anesthesia, but you still feel a lot of the procedure. It made me really nervous having it so close to my heart.
When I showered, I had to be sure to cover it correctly. I couldn’t get it wet. It was just stressful. You have to really take care of it to make sure you don’t get any kind of infection.
Harvesting stem cells
The next step was to harvest the stem cells. Two days before that, they give you a shot to make the cells come out from your bone marrow into your blood so they can harvest them.
This process went smoothly. They take enough for 2 transplants just in case. It took about 6 or 7 hours of being hooked up to the machine.
How was the actual transplant?
I checked in on a Thursday and left 2 weeks later. The same day I checked in, they gave me the high dosage chemo called melphalan.
During the infusion, you have to chew ice. This is to avoid the development of mouth sores, so I chewed away for about 2 hours.
The following day, they returned my stem cells. This is the day they call your “re-birth” since your immune system is practically starting from zero. They said some people might get a reaction, but I didn’t have anything like that. I was very comfortable.
Something that the doctor didn’t mention before the transplant was that I would have to be connected to an IV pole 24/7, which made moving around and sleeping completely uncomfortable. It dripped potassium and magnesium.
It is important to develop a routine when in the hospital for a long period of time, to shower and do exercise. You have to remember that you are in recovery, not on vacation.
»MORE: Learn more about bone marrow transplants from a specialist

Stem cell transplant side effects
It wasn’t until about 3 or 4 days after that I started experiencing some strong nausea and stomach issues.
They provided me with some anti-nausea medicine, but it didn’t really do much. I had already asked around beforehand, and I brought some CBD with me.
They don’t promote it at the hospital, but after I gave their medications a try, I was like, “Okay, this isn’t working. I need to fix it myself.”
It took the nausea away really quickly and helped me to keep eating. The CBD really helps.
Your immune system gets wiped out, so everything you eat has to be cooked. The options they had were definitely not the most nutritious, so I tried to eat eggs, bananas and other healthier options instead of the pizza, rice, spaghetti, etc.
I had to stay on that diet for the 2 weeks I was in the hospital and another week at home. Afterwards, I had to make sure I washed my food extremely well before eating it. My mother flew in from Chile to help cook for me while I was at home, which we are extremely grateful for.
About a week after leaving the hospital, I began to lose my hair, so I had to shave my head.
The whole stem cell transplant lasts for 2 weeks, but the time that you’re vulnerable to all types of bacteria lasts about 100 days. You’re not supposed to go out in public, be around children or expose yourself to too many germs.
Next steps after stem cell transplant recovery
The final blood check was at about the 99th day, which was right before my parents’ 50th anniversary celebration in December, so it was perfect timing. They checked my white blood cell count to see if I could fight off basic colds and infections, and they gave me the green light to start living a more normal life.
Then in January, we started the maintenance therapy, which I must continue indefinitely for now.
It’s 10 mg of Revlimid every day for 3 weeks with 1 week off. At the beginning, I experienced tiredness and itchy scalp and skin, so I started taking Benadryl too.
Since this is a cancer with no cure, this maintenance helps extend your remission time. I visit my oncologist every 3 months to look at my blood tests. I am hoping the cancer stays away for a long time.
Quality of Life
What’s been the hardest thing for you mentally and emotionally?
The drugs play with your mind. When I was on the steroids, I would get angry or more sensitive to certain situations. I would be watching a movie and start to weep like crazy.
What’s scariest to live with is knowing that the cancer can and might come back.
I’m still fairly new in remission, so I’m hoping the fear will fade away a little bit, but thinking that I might have to go through something like that again is hard.
I have to try and be mindful and take each day at a time.
Describe the hair loss
I didn’t lose my hair until my stem cell transplant. Before I checked in to the hospital, I buzzed down my hair. Later on when my hair started to fall out, I ended up shaving my head. My eyebrows didn’t fall out, but my beard was affected. It didn’t all fall out, but it got patchy.
I don’t think it was as bad for me as it would be for a woman or a child. It’s definitely an additional thing to deal with though.
I didn’t like being hairless because no matter how I felt, I would look at myself in the mirror and think, ‘Yeah, I have cancer.’ I looked like I had cancer. It’s a reminder constantly.
It wasn’t really a confidence thing for me, but it was hard to look sick all the time. I don’t care what people think about how I look.
»MORE: Dealing with hair loss during cancer treatment
Did fertility preservation come up?
During my first talk with the oncologist, he mentioned fertility and the dangers of chemotherapy and trying to have a baby. I’m 42, and my wife is 36. We don’t have children.
He offered to reach out to someone in the hospital to put some sperm into a bank for me. There weren’t any days available until the same day I had to start my chemo regimen.
I had my first chemo scheduled at around 11:00 a.m. in the morning, and the only time the fertility people had available was 8:00 a.m. the same day. That was nerve-wracking, but it was accomplished, and they’re frozen somewhere just in case.
»MORE: Fertility preservation and cancer treatment

How did cancer affect your relationship with your wife?
She has been very strong and supportive when I have needed her the most. On my bad mental days, she helps me push through.
She’s broken down a few times, which is natural. We all do, as there’s a lot of fear around cancer. She maintained her work life, though, and it’s very busy, so I think that helped distract her a little bit. When I was in the hospital, they let her work from home. That was really important.
Physically, I still have a lot of limitations. If I turn a certain way, I can still feel the metal rods like I have a monkey on my back or something. If I want to hold her while we’re watching a movie, it’s difficult for me to put my arm in certain positions.
Do you have any advice for other married couples going through cancer?
We’re brought up as men to be emotionally strong. I tried not to talk about my fears too often, but there were some days I had to.
I would say, “I don’t know if I’m going to be here 5 years from now.” But she would help me come back to a peaceful state of mind with her words of encouragement and hope.
I do suggest that you look for a therapist to work through the whole process together.
That support is so important. There are things that you go through that only someone else who has gone through this or a professional can really understand.

Don’t let cancer and the treatment control your life. Continue to do the things you enjoy. Take small vacations or “staycations.”
This is just as important for the spouse as it is for the patient. We would go to a nearby city to explore and just get away from the routine. Stay at a hotel and relax.
»MORE: 3 Things To Remember If Your Spouse/Partner Is Diagnosed With Cancer
How important was it for you to have caregivers during recovery?
My parents live in Chile about 8 months of the year. They’re usually only here between Thanksgiving and February, and luckily they were on extended stay when I was diagnosed. That took a lot of pressure off of my wife.
My parents were able to take care of our cat while we stayed the 30 days in the hospital, and my father drove me to my chemo appointments afterward. I was immobilized for a while, and I couldn’t drive.
Besides direct family and friends, Instagram users were extremely encouraging. It was amazing how much support I received from people I don’t even know, sometimes more than the ones I do know in real life.
Finding your cancer community
Connecting with other cancer survivors was extremely helpful. After all, only other cancer patients really understand what we go through physically and mentally.
We would bounce ideas off of each other, share what our doctors were saying, and just get support. I met some really amazing warriors.
Music was another important support for me during my journey. When I needed to relax, I would listen to Bob Marley’s “Legend,” and one of my favorite’s songs, “Three Little Birds.” That song would transport me to a beautiful beach in Brazil and bring me peace.
What is your “new normal” after cancer?
Now, everything is a lot more short-term than it was before. There’s no 5-year project or plan. Everything is planned out by 1 year at most. It’s a lot more about doing what we enjoy the most as often as possible, whether it’s a walk, traveling, eating out or just being together watching a movie.
I’m still very optimistic. I live as though I don’t have anything wrong with me and never did. Even though I do have certain pains, I just ride it out and enjoy life as much as I can.

Can you talk about the natural remedies and healthy living you practice?
Some of the best natural remedies are ginger tea, chamomile tea, apple cider vinegar, astragalus, lemon water, and of course eating lots of vegetables and fruits.
»MORE: Chemo Diet: How To Stay Healthy During Treatment
Please check with your doctor before trying any other medications.
Something else that I do is called intermittent fasting. There’s a lot of science behind it. Go ahead and watch a YouTube video on it to find out how this simple way of eating can help your cells recover at the cellular level. I believe this helped me enormously.
Ginger tea and CBD helped a lot with my intestinal issues and the nausea. My uncle was diagnosed with colon cancer last year. He was brought up to believe that marijuana is the most evil thing in the world, so he was against taking CBD.
He had some intense nausea, and after taking medications the hospital gave him, we suggested CBD. He would take a couple of hits, the nausea would go away, and he was able to eat.
Keep an open mind about it, that’s all. There are a lot of people that will talk to you about cancer remedies. Any time someone asks me about this, I say the same thing:
‘I don’t believe there are any natural remedies that will cure your cancer, but I believe there are natural remedies that can cure your side effects.’

What is your advice for someone who has just been diagnosed?
First, stay optimistic. Keep your mind thinking that you will overcome this life test. Remain hopeful and faithful that you will reach remission. Take the medications at the times that the doctor orders.
I also recommend finding some sort of mental therapy even if your doctor doesn’t mention it.
I’m a pretty strong-minded person, but even though I am, it was rough for me. If you feel that’s not your strongest point, then seek help or push your doctor to help you get the care you need mentally.
Again, I insist in the importance of eating as healthy as possible, and by this I mean reduce the amount of junk food, fried food, dairy and sugary products you eat. Substitute them with good amounts of organic vegetables, legumes, and some fruits.
These will not only give you the necessary nutrients your body needs, but they will also help your liver detox the various chemicals from the medications. Eating well helped me deal with the side effects a lot better.
Ask questions, reach out to other people, find groups of myeloma patients to join because there are a lot of questions, and answers don’t always have to come from your doctor only.
Plan a celebration for when you reach remission. Having this on your mind will help you push through difficult times.

Inspired by Carlos's story?
Share your story, too!
Multiple Myeloma Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...






3 replies on “Carlos’ Stage 2 Light Chain Multiple Myeloma Story”
I have had multiple myeloma since December 2018 and have gone through the non treatment approach and have tried turmeric and black seed oil capsules as well as essiac tea and a good diet. I don’t know if I am cancer free but I am still alive today in 2024. I refused treatments in 2019 when I was offered 3 months to survive. I haven’t had any flu shots since 2019 and I refused to get a single COVID vaccine. Sure I have lesions on my brain and spinal cord but staying alive for my family is the most important thing to me.So I endured the pain and despite IGA Kappa multiple myeloma.I also have multiple sclerosis but I refused to have my right foot amputated and I steered away from conventional treatments. I have cancer but don’t care because I am still alive when I was told I would be dead in 2019. I had no conventional treatments for the same reasons that you have had them. I wanted to be there for my family and so far I am. Have a great day but keep an open mind. Chemotherapy works in 3 percent of patients and radiation therapy not much better. I have had friends who have had all their COVID jabs and didn’t survive to tell the tale because they aren’t vaccines but rather GMOS. Do what you like with my comment it doesn’t bother me but I am the other side of the coin and I definitely don’t regret it
My Mom is suffering from antibiotic resistant UTI with multiple myeloma. Is there any natural remedy to treat her UTI?
Hi Nikki, I am so sorry to hear about your mother’s situation. We don’t offer medical advice, so the best path is to consult with her doctor(s). Sending you both all the best. -Stephanie