Gregory’s IgA kappa Multiple Myeloma Story

Gregory was diagnosed with high-risk multiple myeloma a few months after experiencing lower back pain. What started as a nagging pain that felt like he had pulled a muscle continued to persist until the pain got so severe that his movement was limited.
After initially seeing his primary care physician, he reached out to his spine management doctor. He was in excruciating pain by then, prompting the doctor to order an MRI, which revealed a mass.
Within a matter of days, he had to find an oncologist. After running a series of tests, his doctor told him that he had multiple myeloma and that he had to get his affairs in order.
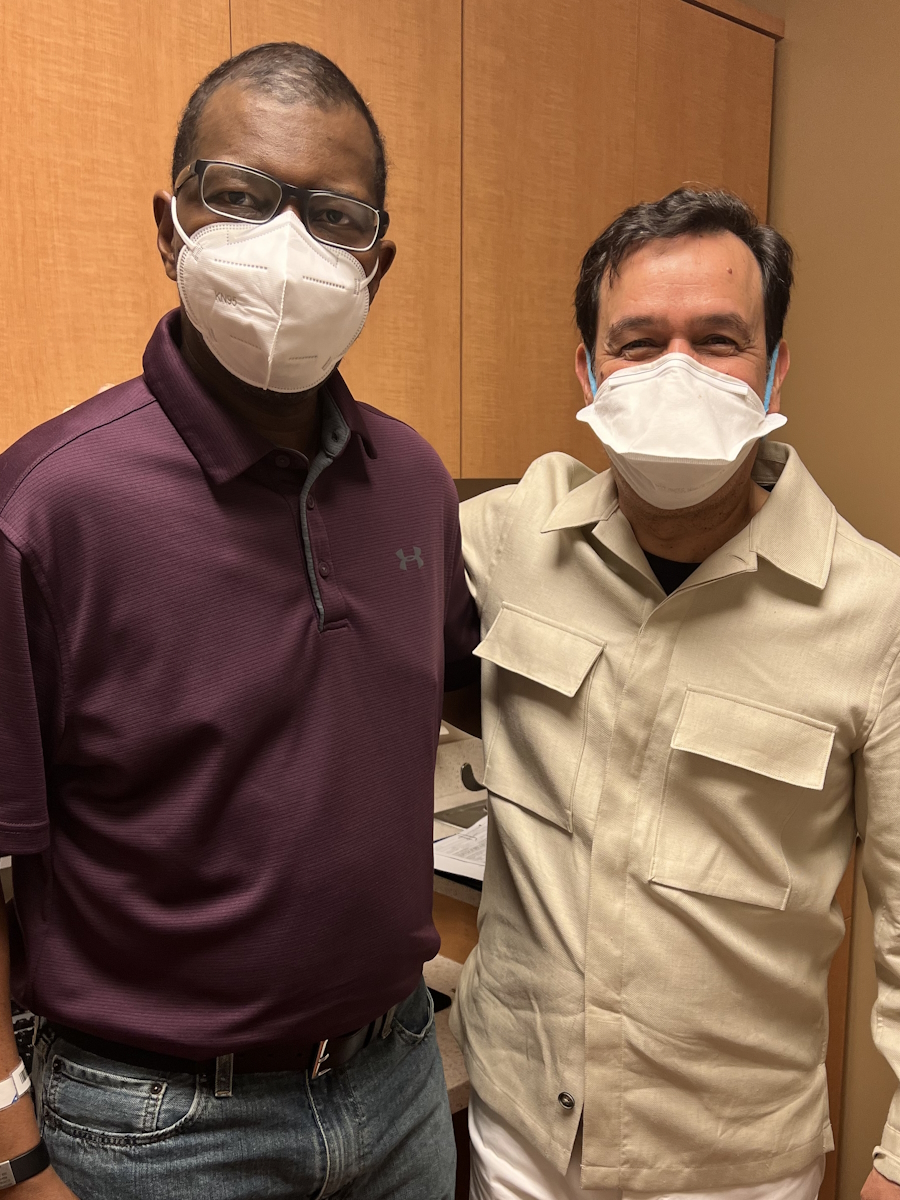
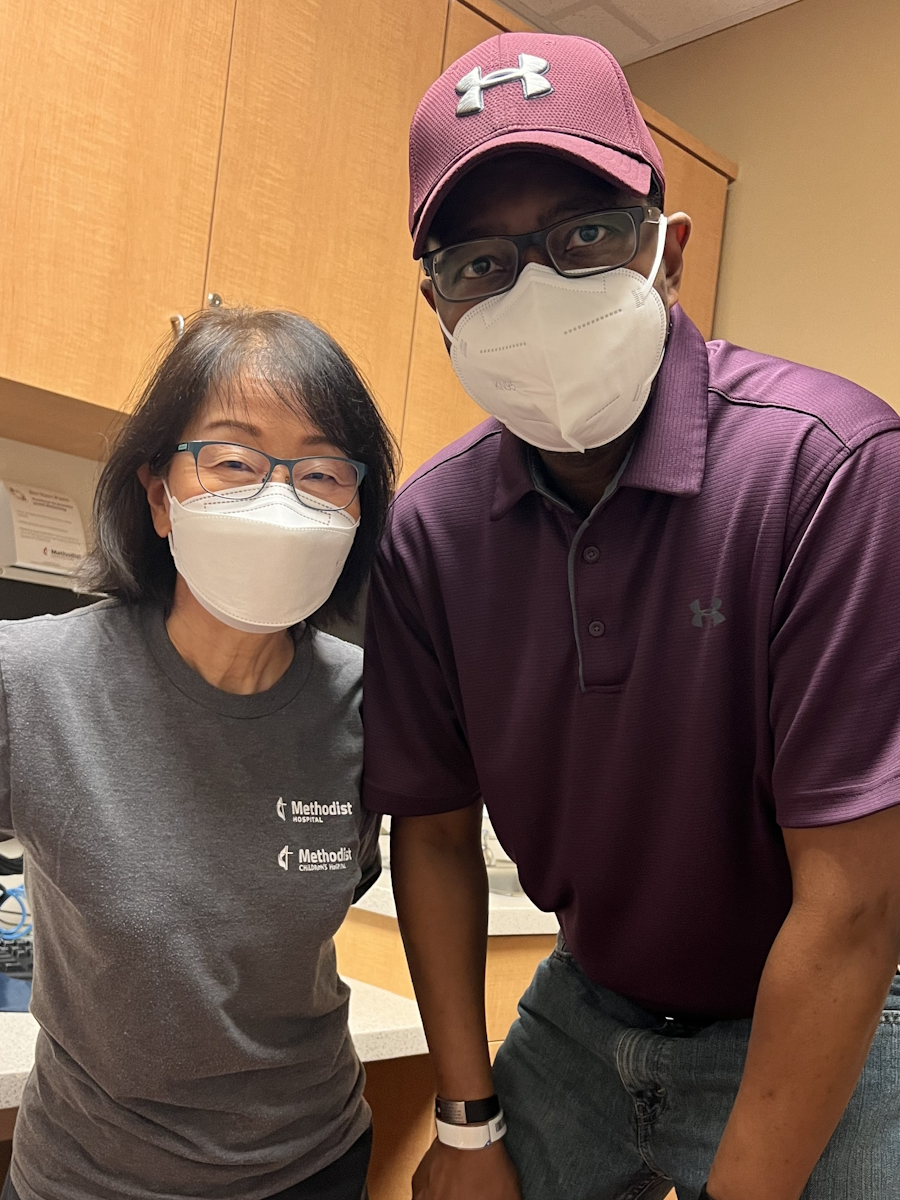
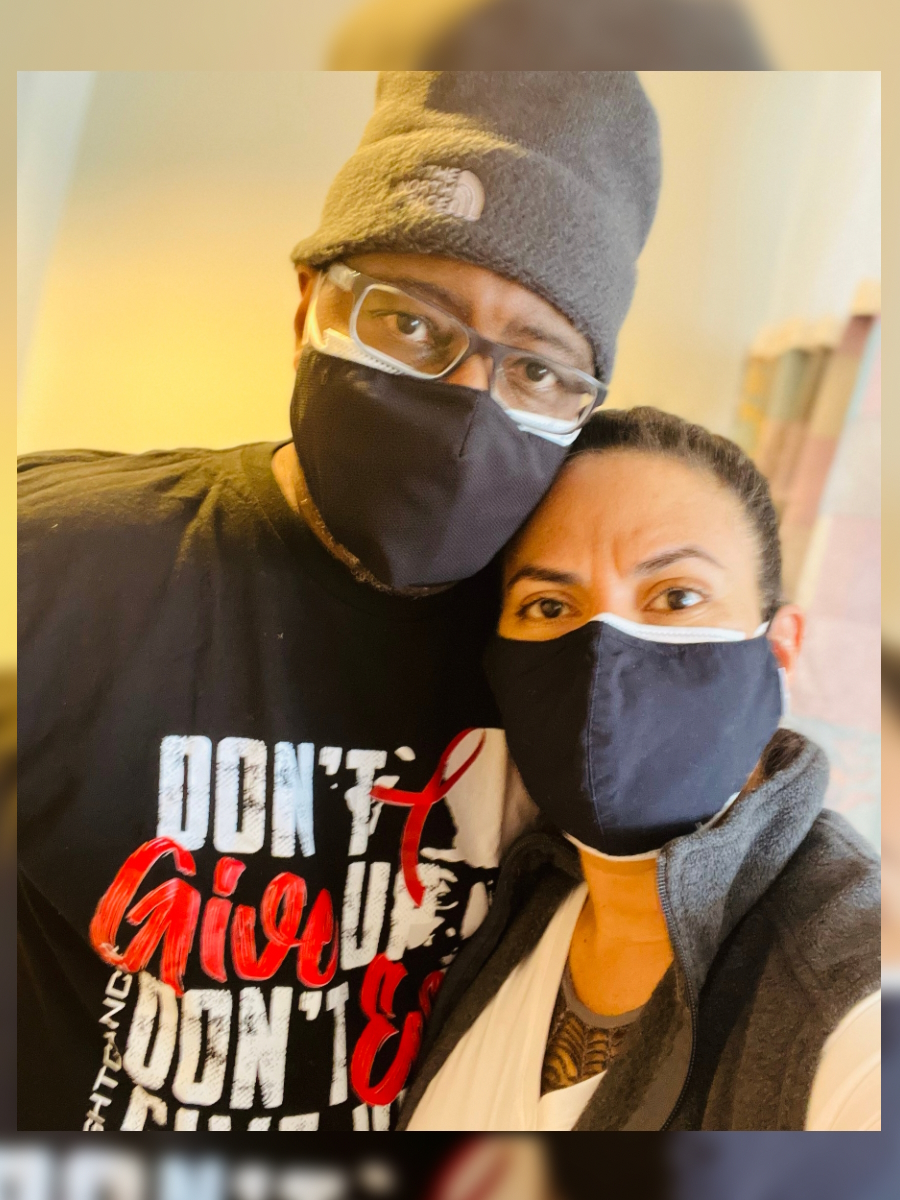
He shares how he and his wife teamed together, how the cost of cancer treatment led to financial toxicity, and how he almost had to stop treatment.
He describes the frustrating ordeal of having to follow up with insurance while going through cancer treatment, experiencing engraftment syndrome after his stem cell transplant, and how he relied on his faith. To chronicle his powerful journey, Gregory wrote a book titled, “Faith, Strength, and Courage: A Memoir of Overcoming Adversity and Embracing Life’s Journey.“
In addition to Gregory’s narrative, The Patient Story offers a diverse collection of multiple myeloma stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Gregory P.
- Diagnosis:
- Multiple myeloma, IgA kappa, 17p deletion, with two sub-mutated genes
- Initial Symptoms:
- Lower back pain
- Treatment:
- DVd: daratumumab, bortezomib, dexamethasone
- Stem cell transplant


Introduction
I’m very passionate, motivated, and inspired by being able to help others, uplift others, and offer my value and my voice.
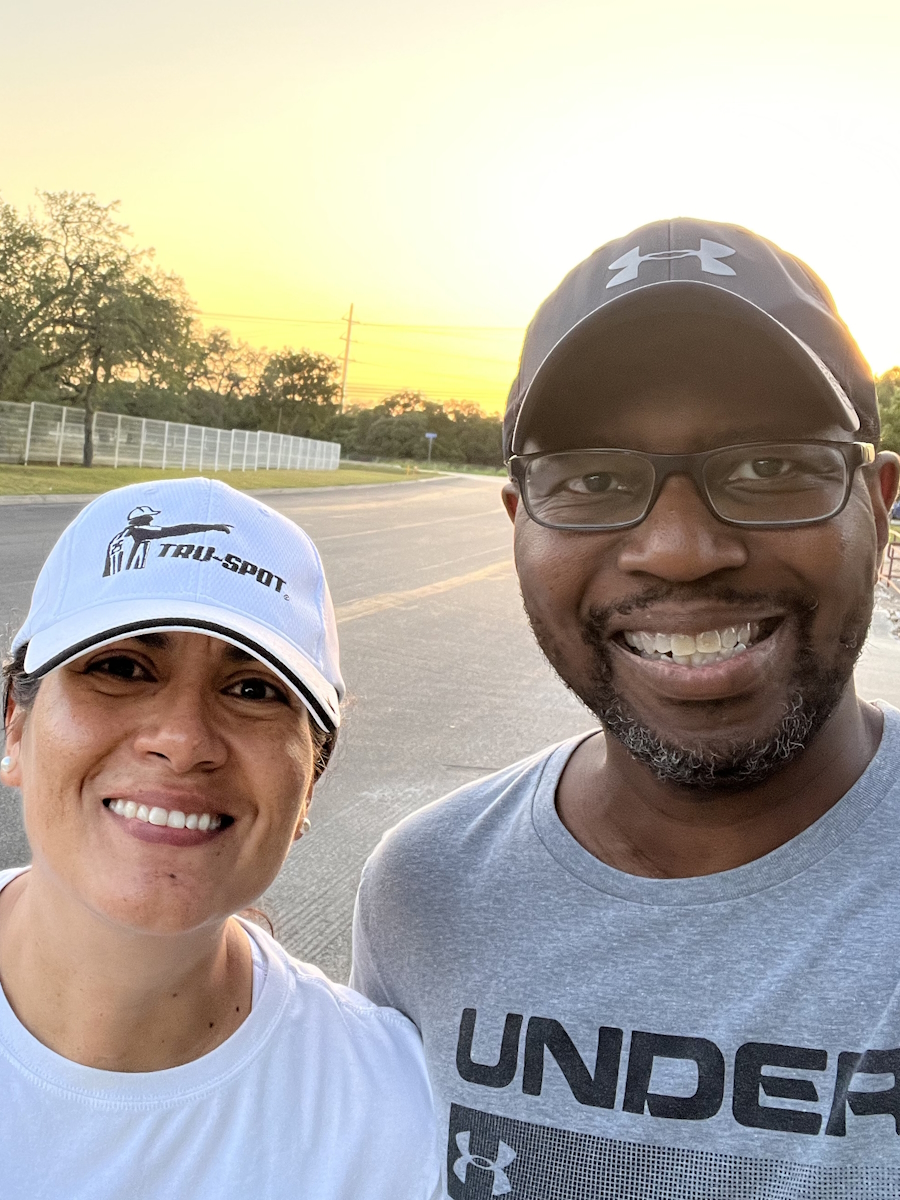
One of my hobbies is being out in nature and walking.
Most people know me from my podcast, Kut2ThaChase, [where] friends, family, [and] professional colleagues talk about things that impact their ability to thrive. We’ve been known worldwide [for] bringing forth inspirational stories of hope, motivation, and triumph over challenges and adversity.
Other people know me [from] my project management consultancy firm where we’ve supported a lot of Fortune 500 companies all over the world.
My application company called Tru-Spot is an augmented reality program developed for fans to view concerts, movies, or television programs worldwide without having to travel.





Pre-diagnosis
Initial symptoms
I started having lower back pain around April or May 2021. It started as a nagging pain, as if I had over-exercised or pulled a muscle. The pain continued to persist day after day, week after week before I finally threw my hands up and said, “I need to go and get something done about this.”
At the time, I was home alone recording podcasts, going through a capital raise with my business partner regarding Tru-Spot, and spending a lot of time not moving around or exercising as much as I would.
I saw my primary care physician and he said, “We may be dealing with a pulled muscle, a slipped disc, or something along those lines. Let me give you a steroid shot and some pain medication. Let’s do X-rays and take blood work.”
I came home that weekend and realized that this pain was way more severe than anything I could ever imagine. The steroid shot [and] the medication they gave me [were] not reducing the intensity of the pain. I realized that I needed to take this to the next level and see a specialist.
I reached out to my spine management doctor. He realized that the case was pretty severe. He poked and prodded and a couple of times, I said, “Please don’t touch me there again,” because I was in such excruciating pain. He said, “I need to get you over for an MRI.”
They ran the MRI [with] no contrast. They identified a mass. They didn’t know if it was cancerous or not so they wanted to schedule me for a second MRI, which would be done with contrast.
At that point, I started hearing terms like multiple myeloma and lymphoma, not wrapping my head around that this could be cancer. I just figured, I can have surgery, have whatever removed, and go on with my life.
As we went through the next series of tests, we quickly realized that this was beyond the control [of the] two doctors I had previously seen.
My back pain started in [the] lower right back where my back connects to my hip area. The tumor, that was about the size of a grape and as long as an egg, already protruded through my bone. It was cutting across my sciatic nerve, [which] inhibited me from being able to walk. On top of that, having such a huge amount of pain radiating throughout my entire body made it difficult for any type of mobility.
I saw my primary care physician [and] my spine management specialist within 48 hours. I had the first MRI done within 96 hours. The second MRI took me about two and a half to three weeks.
Once we had the second MRI, it was a matter of trying to find an oncologist that would be able to see me right away, which took a little bit of time as well.




Finding an oncologist
The first MRI was inconclusive, but the spine management doctor concluded that this was going to be very severe, as if he had seen cases like this before.
Once we ran the MRI with contrast, he pulled us back into the office and said, “Mr. Proctor, I can’t go into a lot of detail, but you guys need to find an oncologist right away.”
We’re trying to find an oncologist [when] we still don’t know what’s going on. We’re in the dark because we’re not getting a lot of information from my spine management doctor or my PCP. We were fish out of [the] water, trying to navigate this uncertainty, hoping and praying that it’s not what the conclusions are based on the various reports that we were able to dissect and somewhat understand.
You hear certain things. It puts you in shock. What do I do next? You’re almost hopeless to a certain extent. Every patient is outside of their comfort zone. For me, it was no different.
One of the things that my wife and I processed during that time was the fact that whatever it was, we wanted to deal with it head-on. We thought we could overcome it.
My spine management doctor had a friend that he went to college with that was an oncologist. We said, “Okay, this is great. Let’s see if you can help us get an appointment with your friend.”
Having to find a new oncologist
As we went down that path, his friend decided that they were not going to accept my insurance, which was a national healthcare plan. For lack of a better term, it was a bunch of bollocks that we had to go through.
We were very frustrated. We’re back trying to call around, see who can expeditiously see us, and get over the hurdle of our insurance.
We found an oncologist in San Antonio on the third or fourth try. It took about 72 hours.
Once we had that first consultation, everything that they needed to run again was run within the next 48 hours — bone marrow biopsy, extensive blood work, PET scans, you name it.
I was always a healthy individual — never really had a lot of health issues, maintain very good physical fitness, never had a broken bone. I’m put into the throes of the medical industry, not really truly knowing how to navigate besides paying [my] insurance premium and things that we normally do just as a sense of comfort. Now I’m faced with this head-on. It was very, very scary at the time.


Diagnosis
Getting the official diagnosis
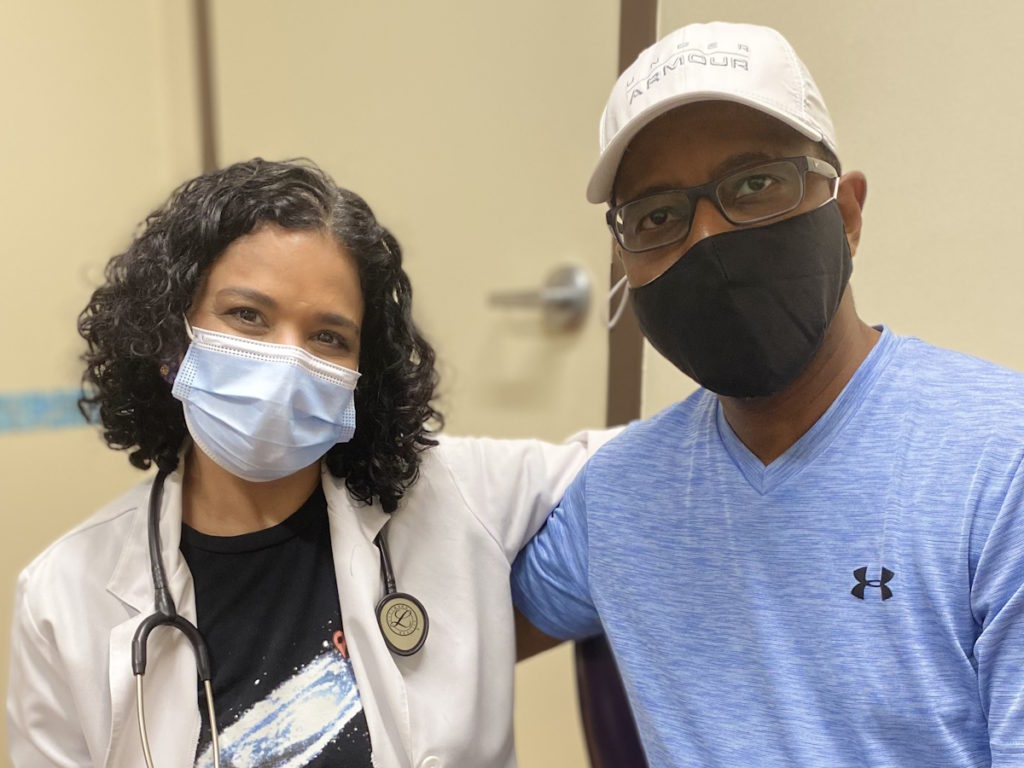
After we secured a local oncologist, she brought us in and based on the scans and blood work, she listed off different cancer types on the report. She said, “I hope we’re not dealing with one of these. I’m uncertain until we have more blood work, more scans, and a bone marrow biopsy.”
We had the consultation [on] a Wednesday. [On] Thursday, I [had] a lot of scans and blood work. On Friday morning, I end up having a bone marrow biopsy, the worst procedure that anyone can go through unless you’re completely sedated.
I went through it on local anesthesia and realized that I needed to be put to sleep because the pain was something that I’d never experienced in my life. It was completely off the threshold scale for me and I could not tolerate it.
My bones were very dense so they didn’t [know] if they had enough bone marrow material. They thought I was going to have to come back for a second procedure. They ended up having enough material. After they ran it through, I was diagnosed with multiple myeloma.
Knowing about myeloma
At the time, my knowledge [of] the disease was very, very low. I was not familiar. I’ve heard lymphoma and things like that but not really paid attention to the severity and what people go through.
Things were being thrown at us at an accelerated pace, like being on a roller coaster and feeling like you’re free-falling indefinitely. We knew that the first thing we need to do is get ourselves educated and get ourselves up to speed.
Reaction to the cancer diagnosis
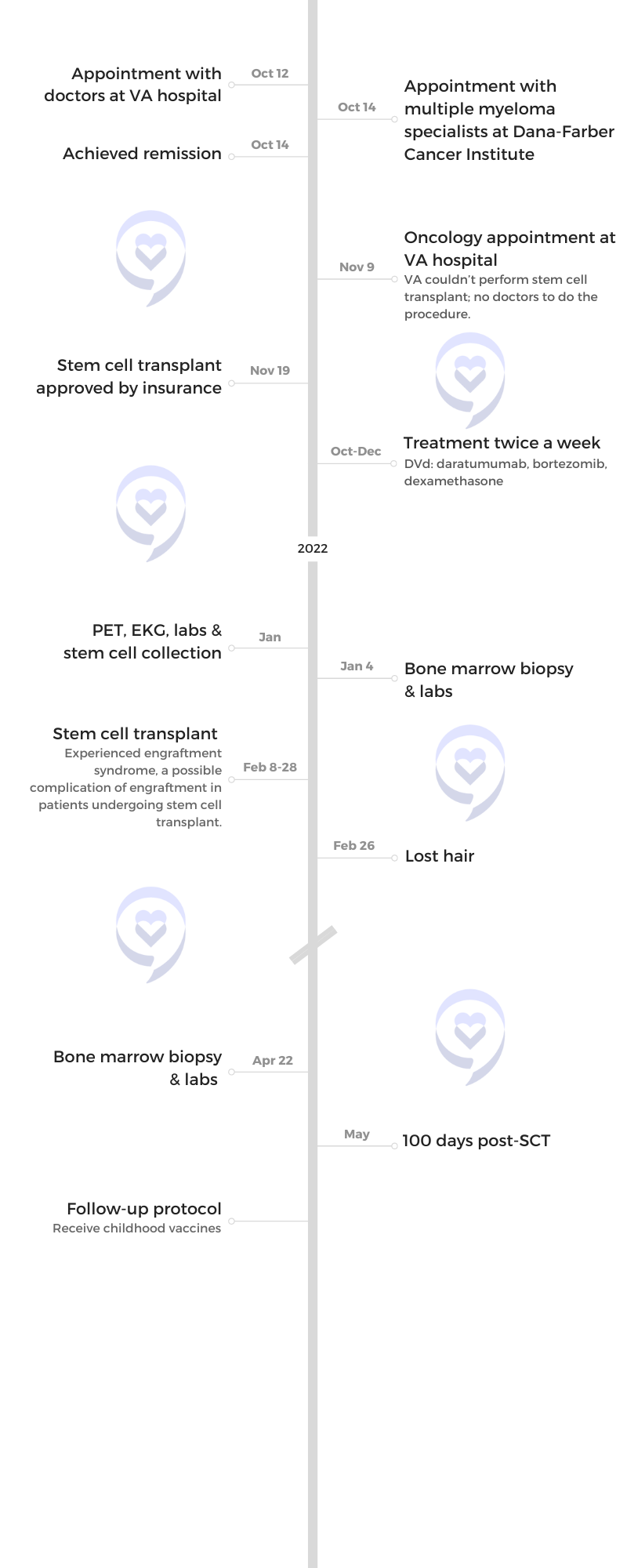
Initially, [when it came] from my spine management doctor, we took it with a grain of salt. July is when I was officially diagnosed [with] multiple myeloma, IgA kappa, 17p deletion, [and] two sub-mutated genes, which put me at high risk.
My oncologist said, “Mr. and Mrs. Proctor, you need to get your affairs in order.” That broke the camel’s back for us because no one had ever said that.
We had limited time to process everything because, in the second breath, she said, “We need to start you on chemo treatment right away.” This was on a Friday. We were told the diagnosis right after my bone marrow biopsy and I started chemo the following week.




Not having time for a second opinion
My wife and I were very naive to the situation. We knew that I was extremely ill. It was very hard for me to walk and my mobility was limited. I needed assistance back then more than I had ever needed assistance before.
Everyone else we called was unable to provide us with any type of service nor did they even want to see us. We were pretty much going with this oncologist based on faith.
She consoled us, hugged us, and said, “I need you guys to trust me. We’re going to get you through this. It’s going to be an arduous process. Mr. Proctor, as long as you can handle this and as long as your organs continue to function the way that they’re supposed to, we believe that we can get you into remission within probably 3 to 4 months.”
We stepped out on blind faith because it was so overwhelming. We were feeling hopeless at that point that we had nothing else we could fall upon.
We didn’t have an opportunity to get a second opinion. I wasn’t going to get on a plane or drive from San Antonio to MD Anderson in Houston, which is three hours, or even another cancer institute. The pain was so severe that I could not take it much longer. I needed for something to happen and I needed for something to happen right away.
Breaking the news to the family
My wife and I were trying to maintain a strong persona, trying to maintain the support and love that we have for each other. But it was hard. It was really, really hard.
We started trying to think about what do we do next. Do we have enough financial means to get us through this? Do we have the family support? We hadn’t even really told our family at that point. We were still in shock and trying to digest and understand how we would move forward with everything that was going on.
I don’t think it was until the day before I had treatment [when] we reached out to all of our family and decided to let them know what was going on.





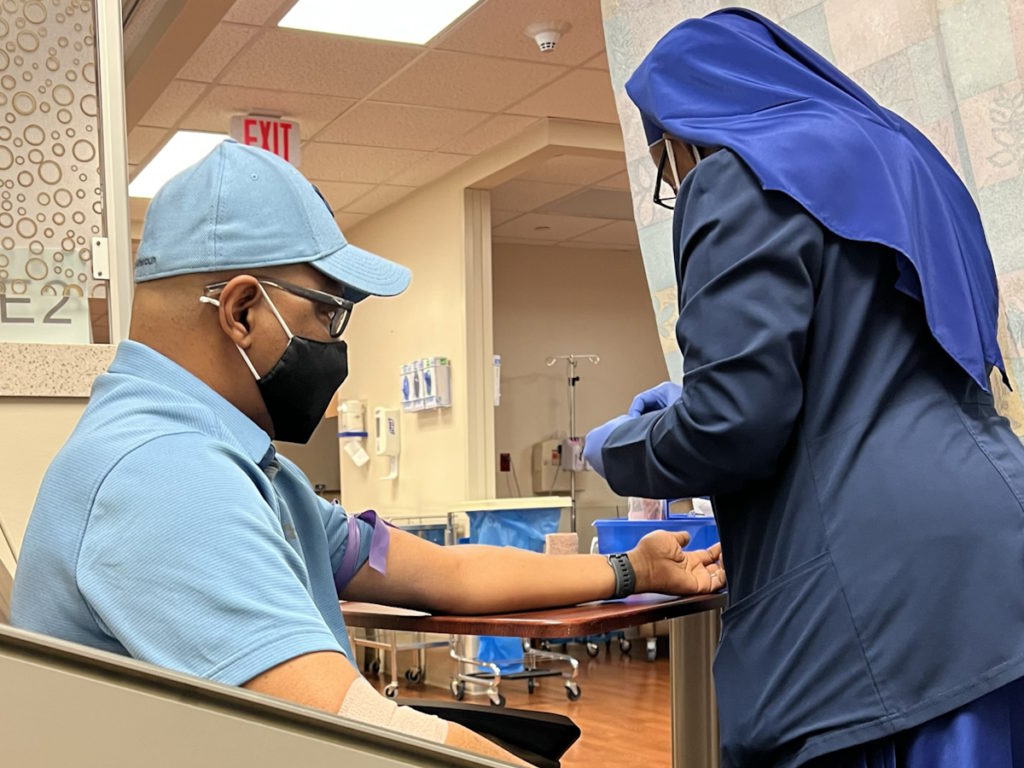
Treatment
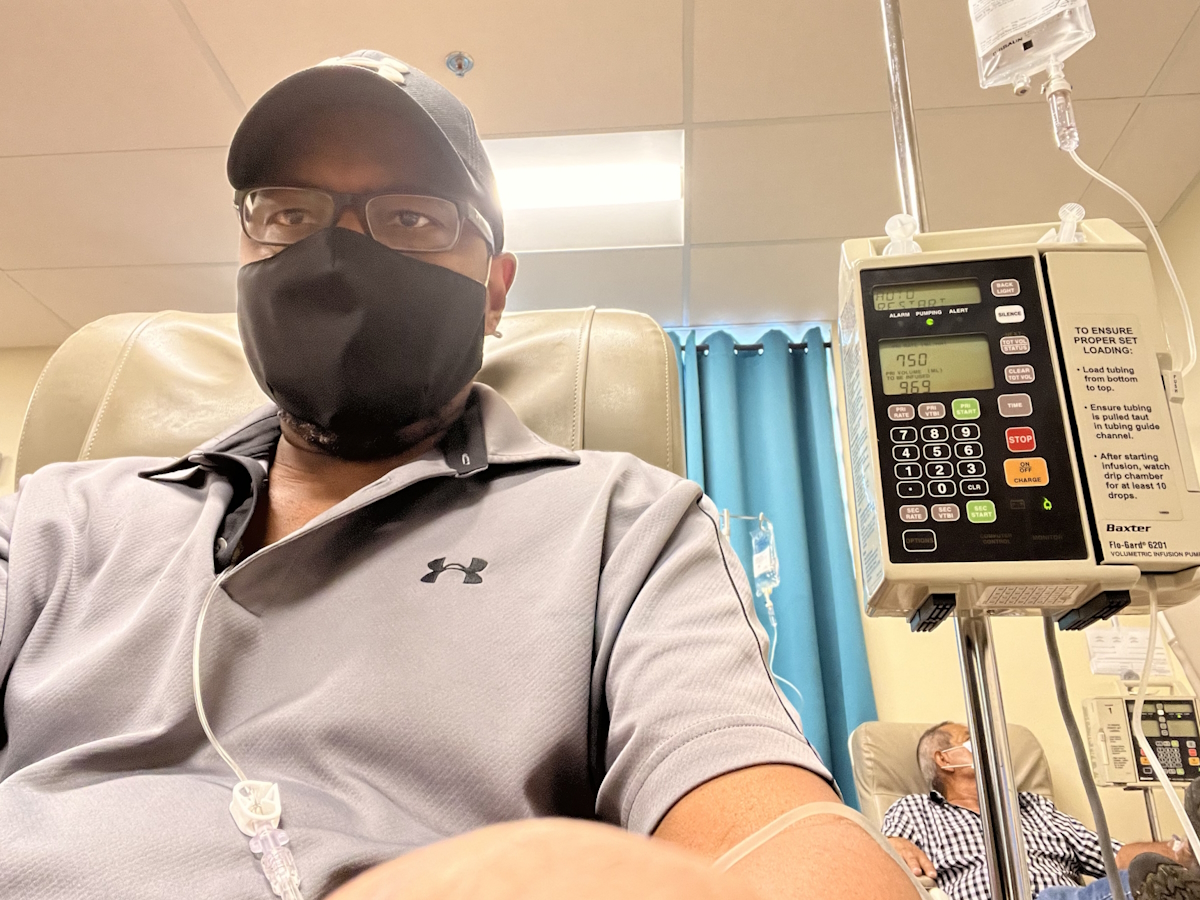
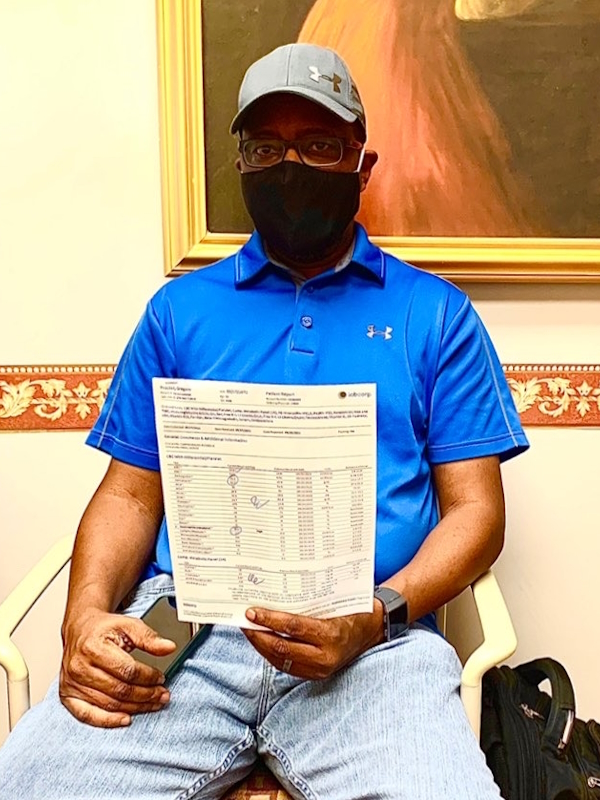
The beginning of my treatment started within 48 hours. After the diagnosis on a Friday, on Monday, I was sitting in the chemo chair for the very first time. That was very surreal.
Walking into the treatment center and seeing multiple people in different chairs, under blankets, and [having] these units hooked up to them, I was scared out of my mind. Are we being killed? Are we setting ourselves up for me to go to the morgue here? It’s the first thought I had when I first walked in there.
The nurses came over, sat me down, and said, “Greg, we will be administering Darzalex and dexamethasone. We’re going to start with these two drugs. Sometimes people have an allergic reaction, sometimes they don’t so we want to see [how] your body’s going to react.”
The very first time that they administered Darzalex, I did have a reaction. I felt like my ears were beginning to tingle. My nose felt like there was some major reaction going on. They said, “Okay, we’re going to stop your treatment. We’re going to upload you with a lot of Benadryl. Then we would restart your treatment.”
My first treatment was five days a week for two and a half months. The only time I came out of a brain fog from dealing with all the chemo was late Saturday night, maybe early Sunday morning, and having to start this treatment all over again.
We ran that regimen for about two and a half months before we started to see the numbers begin to come down. My M spike was greater than 6,000 and there were a lot of other variables out of range, which were very, very concerning. The 17p deletion and the two sub-mutated genes didn’t add a lot to my overall diagnosis as well.
The mental anguish of cancer
You get caught up in this turbulent cycle, trying to figure out what’s next. For us, getting the cancer abated was the very first step.
I was going to be hooked up to an IV for two and a half months, trying to get my numbers down, and ensuring that everything was back within range before we could move on to the next step.
We were spending a lot of time researching, reaching out to Facebook groups, and having different types of discussions with folks. At the very beginning, we were not thinking about the stem cell transplant or any of those things downstream because it was just too hard without getting through this first cycle.
How quickly can we get the cancer abated? How quickly can we get the pain diminished? How quickly could I get back on my feet and be able to function again? How quickly could I get a good night’s rest and be able to sleep horizontally and not vertically because of the way the pain radiated through my body? How do we survive financially?
There was a plethora of things that we were trying to process within the first three months, well before we got to the second phase of the stem cell transplant.



Financial toxicity of cancer treatment
What a lot of people don’t realize is that you still have to live even though you’re tied up in a medical facility every single day. You still have bills that you have to pay.
We were trying to think about what we could relinquish and get rid of. How could we streamline our lifestyle a little bit?
Even though we had gone through all the different processes, making sure our deductibles were paid, and tapping into various grants that I should qualify for, my insurance company was very slow to pay.
I had racked up a quarter of a million dollars because I was burning $22,500 per week on my treatment, which consisted of Darzalex, dexamethasone, and Velcade. My insurance company said, “We’re still waiting to go through our audit process. We’re still waiting for this paperwork. We’re still waiting for this. We’re still waiting for that.”
Roughly early September, my doctor said, “Mr. Proctor, we’re going to have to stop your treatment because I haven’t received any money from your insurance company.”
Think about how hard that is to hear. I’m trying to fight for my life. Of all the things we’ve already heard, now I’ve got to put forth the energy to be on the phone with the insurance company to say, “Why haven’t you guys paid my oncologist? This is unacceptable.”
These are the harsh realities that are not talked about enough.
You think, I’m paying my insurance so I should be covered. You think that everything’s going to be handled based on the fact of you doing what you’re supposed to do as a customer, which is making sure your premiums are paid.
What you don’t realize is that they’re going to take their sweet time. You’ve never been this ill before. They see your bills coming in so they’re going to do an excruciating, deep-dive audit. Eventually, you hit your ceiling.
My insurance was based on a 70/30 split. Even though I met my deductible of $15,000, I was still responsible for 30% of my medical bills. When you start adding up 30% of $22,500 a week, it becomes a financially toxic situation.
I had a mid-average coverage with my provider and certainly thought that was going to be enough. But three and a half months in, they said, “You’re very close to hitting your ceiling.” It was very discouraging.
You start throwing your hands up. What do I do now? If I’m going to go through a stem cell transplant, what do I do? On top of all of the medical costs that I’m already dealing with, that’s going to be extremely expensive. My insurance company covered their portion, but there were a lot of out-of-pocket expenses.

Educating other people about multiple myeloma
Since we didn’t know a lot about this disease, we wanted to coach, educate, and help mentor others and make them aware. Our family was reaching out to us, saying, “Greg’s going to be resilient. He’s going to get through this. They can just go in and cut it out.”
I kept telling my family, “You can’t cut out blood cancer. If I don’t have blood going through my body, it’s going to be very difficult for me to live.” It became an educational process. So many people were reaching out, calling, and contacting me. I told my wife, “We just can’t deal with all of the phone calls and text messages.”
At the time, we disagreed about putting my story out online and being very transparent, but that was the only way for me to communicate with people that knew me. They were all concerned and want to wrap their arms around us and figure out what could they do to help.
Dealing with insurance while undergoing cancer treatment
Don’t give up. Don’t ever give up. For me, it was about getting locked in. It was about transforming my mind beyond the pain. It was about utilizing all of the professional skills that I have and bring those into the fold as a patient.
My background has been in project management. I had to take those skills and apply those to my wife. There was only a limited capacity that I had for brain power and energy that I could stay focused on. I helped her become the project manager and I was the project.
We divided up roles and responsibilities. It was up to her to talk with the doctors, look at the labs, run the trend analysis, and chart out symptoms, discomforts, ailments, and pains that I was telling her about so these would be discussions that we could have with our doctors.
For me, it was all about trying to survive six hours per day every single day of the two and a half months, and just getting through the harsh treatment. Then making those arduous follow-up phone calls to the insurance companies.
In the beginning, that was very instrumental in helping us not have so much burden on each other. We knew our roles and responsibilities.
It was just as hard on her being the caregiver, seeing her husband suffer and have this disease, and watching that on a day-by-day basis.
A few friends said, “You’re in a dark place right now. You guys need to sit down, come up with your strategy, and you guys are going to come out better. It’s going to take you guys getting over this dark place because it’s all overwhelming.” It was like a tsunami had taken over and we were still swimming, trying to figure out if we were going to be able to make it to the surface for air.



Working on a plan to keep treatment going
There was no way I could stop. We hadn’t even gotten to the point where the numbers were starting to trend downward.
I call my doctor up along with her billing department and said, “What will it take for me to be in a position to continue my treatment?” She said, “We need some type of good faith payment. We need something that, in earnest, is going to allow us to continue your treatment. If not, we’re going to have to stop.”
I said, “What number are we talking about?” Her office manager said, “Is there a way for you to come up with $10,000?” I can’t just pull that out of a safe or out of my bank account and make that happen to prevent my treatment from stopping.
With the multiple businesses that I own, I took one of my business credit cards and said, “You know what? This is not a business expense, but I need this to continue.”
I broke down the payments into $5,000 increments. We managed to keep the ship afloat for a couple more weeks so I could continue to be on the phone, try to get money out of our insurance company so they would pay the claims that were already submitted.
It did happen eventually. We went from July to almost October before my doctor saw a large portion of the claims paid. Very scary time.
Side effects of treatment
Early on, because of the dexamethasone, I was dealing with a lot of insomnia [and] not able to rest very comfortably. I was only on 8 mg per day but that was probably way more than I ever wanted to take in a single shot.
I was dealing with all types of ailments [from] the bone lesions that I had throughout my body. My rib cage, my chest, and down the right side of my leg felt excruciating bone pain from where the disease had just really attacked my body. Those were extremely discomforting.
Besides those, just dealing with chemo going through your body. Nausea, vomiting, [and] various things that your body cycles through. Psychologically, you’re freaking out because you just don’t know if this is normal.
My doctor said, “These things are going to occur, but they shouldn’t persist. They should clear up. Things should start to get back to normal once they flush through your body.”
I didn’t deal with a lot of neuropathy. My wife and I spent a lot of time researching the disease and looking at natural things that my body needed to have to recover from the chemo as quickly as possible. We started instituting a lot of those regimens and those things were able to help.
I was in pretty bad shape until I achieved remission. My body was going through a lot of physical transformation that I had never experienced ever before, primarily getting rid of the disease and eradicating it from my body.

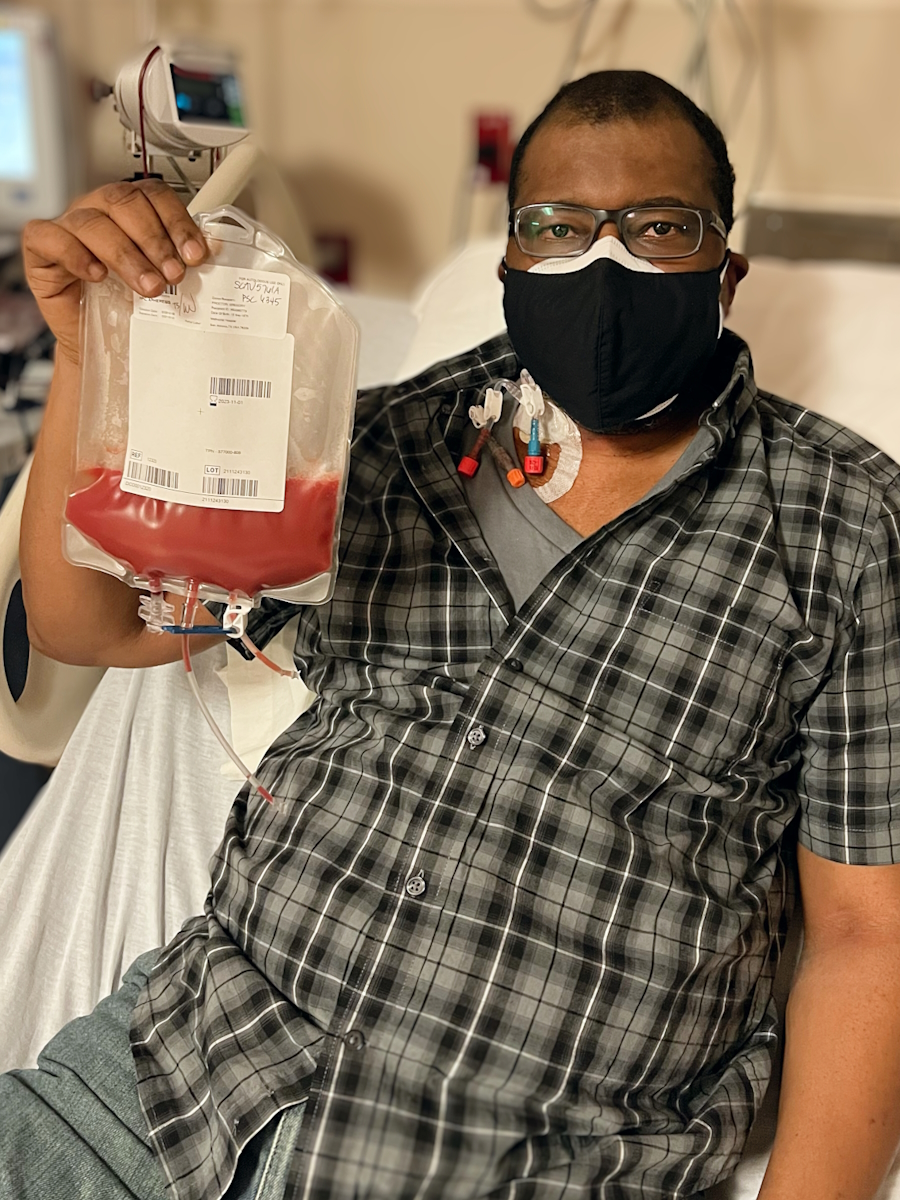

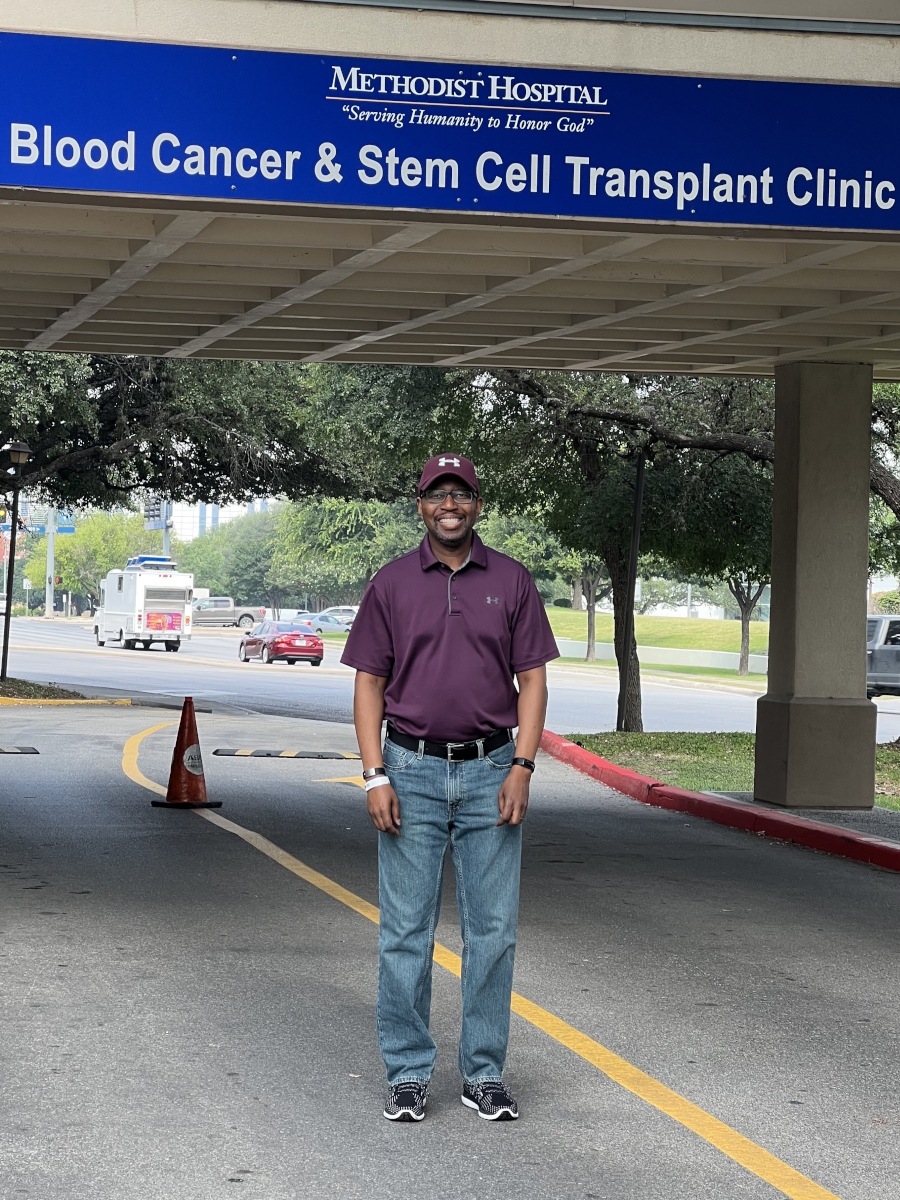
Stem cell transplant
Once we got to remission, the first thing that came to mind was having to prepare for a stem cell transplant.
We did blood work. They look at your M spike along with other characteristics, like LDH, creatinine, and protein levels in urine.
Those numbers were drastically low compared to what they were from the onset of my diagnosis. At that point, everybody was with a sigh of relief but, of course, I had to go through another bone marrow biopsy.
The bone marrow biopsy was conclusive. The disease had pretty much been eradicated from my body. But considering I was high risk, there was no getting around the stem cell transplant if I wanted to have long-term survivorship. It was all a matter of timing.
Getting the stem cell transplant covered
We were still in the throes of dealing with the financial components. If we reached our ceiling, what was our insurance company going to cover with regard to our stem cell transplant?
We received that letter that said they will cover the transplant, but if there are any complications after discharge, then I’m on my own. It’s going to be out of pocket. I was appalled when I got that letter.
Because I’m a veteran, we were trying to get the VA hospital to step in. We were trying to get approval. We had two parallel paths going simultaneously.
The VA stepped in and said they will cover all transplant costs and post-maintenance costs for up to two years. That was probably one of the best days, knowing that we were not going to have that financial burden.





Preparing for the stem cell transplant
I spent the first two and a half months in this fog. We said to ourselves, “We’ve got to get a multiple myeloma specialist.” Our insurance company said, “You can utilize within the network and it wouldn’t cost us very much.”
We ended up at the Dana-Farber Cancer Institute. We were in Boston the time that I received news that I was in remission. We were inquiring about the stem cell transplant. We knew that I needed to be in remission for the transplant to be successful.
Dana-Farber started getting us into the system and running through all of their processes. We were still very apprehensive. I wasn’t feeling back to my old self, but the pain had subsided. I still was dealing with a lot of ailments because of how much damage the disease had already done to my skeletal structure.
Do I have the strength, mentally and physically, to get through this process? We all knew this was very arduous. We didn’t know much about it at the time, but we knew it was very harsh on the body.
We did the same thing that we did with trying to understand the disease. We poured our energy and time into finding out everything that we possibly could with the stem cell transplant and where the best location would be for us to get this done.
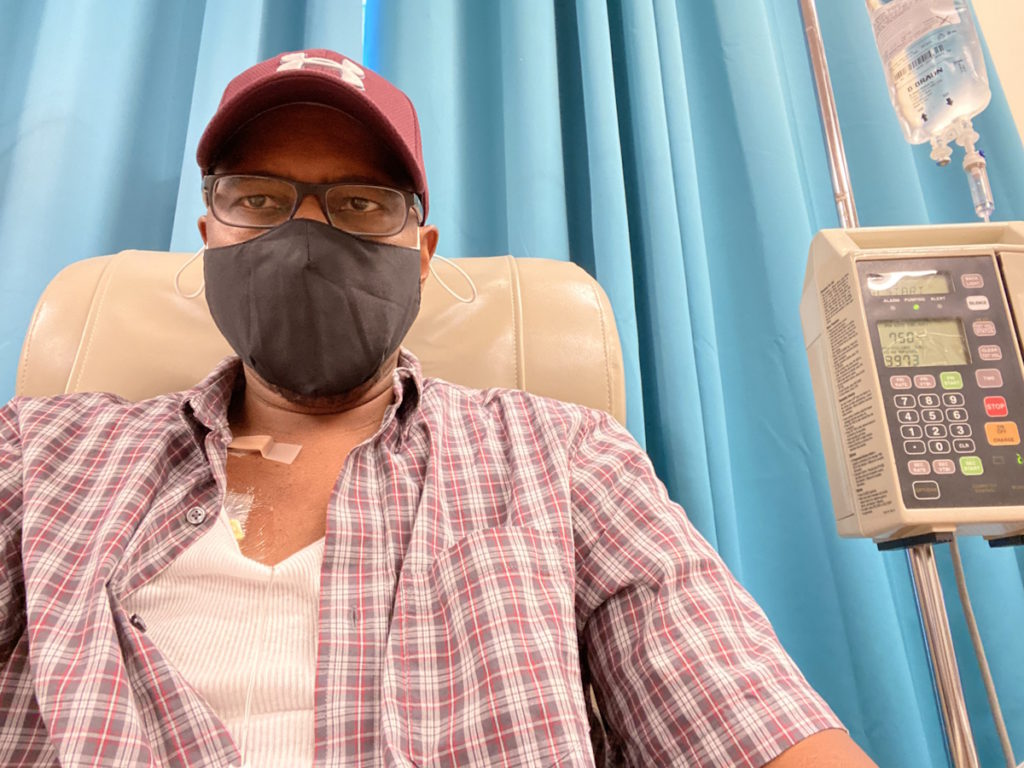
Stem cell transplant process
The transplant got delayed until February 2022, which pushed me into another calendar year, which also pushed me into another deductible. Luckily, with the VA being there, it was a blessing for us to move forward.
I checked into the hospital on February 8th where I was administered the melphalan. February 9th is when my transplant occurred. I stayed in the hospital for approximately 11 days.
We talked with the doctor, “You collected 8 million stem cells. How many stem cells are we going to put back into me?” My doctors said, “We think we’re going to go with two, two and a half, no more than 3 million stem cells.”
We started trying to wrap our heads around it, not understanding all of the science but knowing that if I had a re-occurrence, I would have X number of stem cells in the bank.
They came in with my stem cells. The nurse practitioner said, “Mr. Proctor, we’re going to put 4 million stem cells back into you.” My wife and I looked at each other and said, “Is that too much? We were told no more than three and you’re putting in another million. What is that going to do to me?”
After going through it, it helped me recover, but the roller coaster ride that I had to deal with was just horrible.




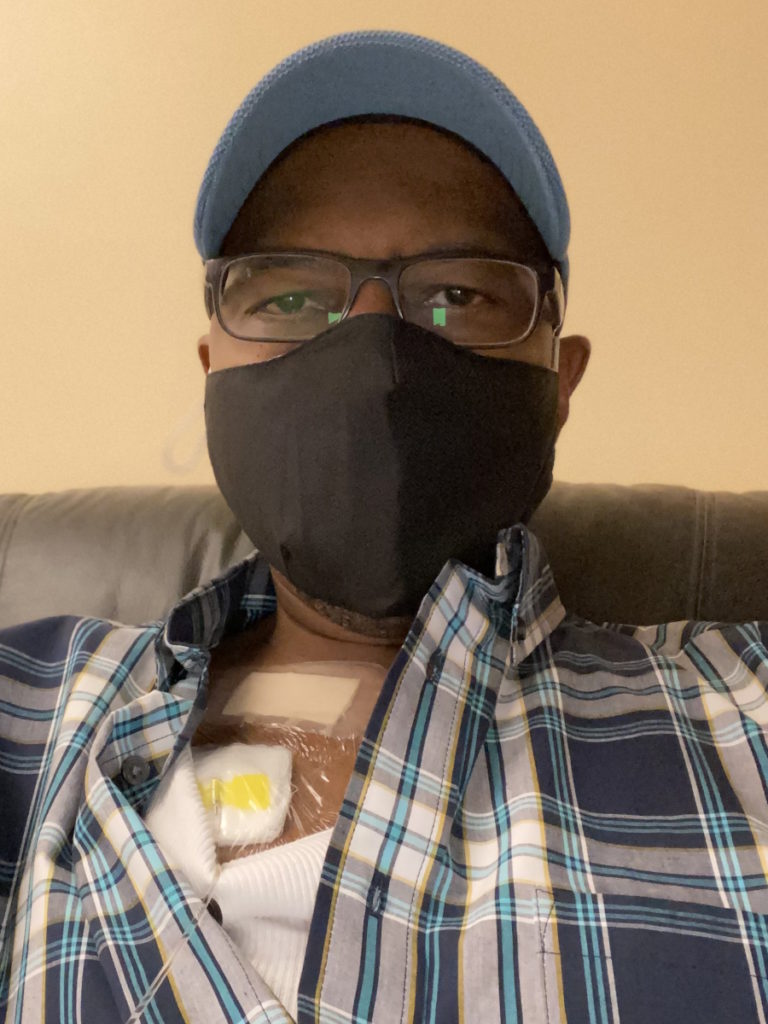
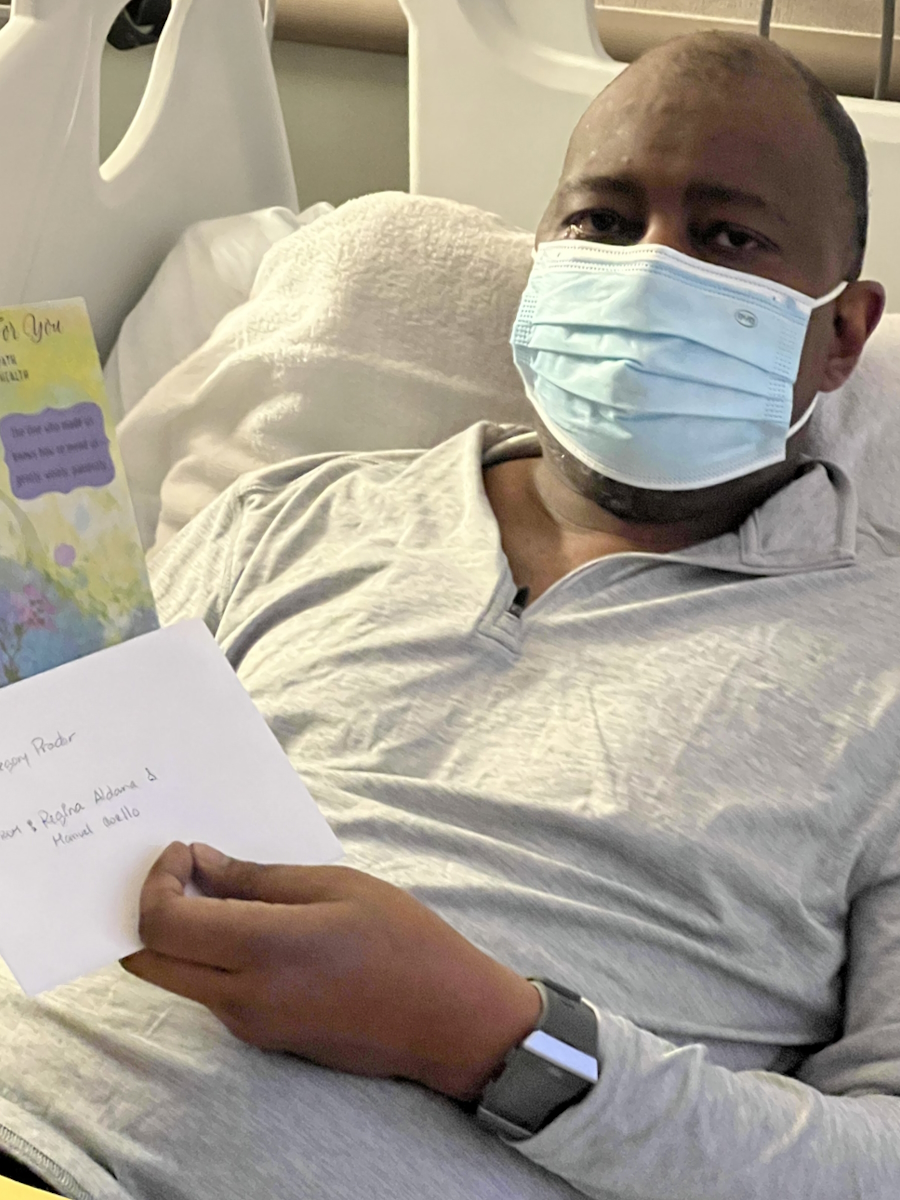
Side effects of the stem cell transplant
I came home for 14 hours, spiked a tremendously high fever, which my wife could not even read on a thermometer, rushed back to the hospital, and ran through an excruciating series of tests to look at all different types of infections.
On the 8th day, the conclusion was engraftment syndrome. That in itself was very scary.
Initially, you hear a lot of bad things with regard to stem cell transplants. Your doctors are prepping you and ensuring that not only do you have the mental fortitude but also the physicality to get through it.
I had gone from 185 lbs to 225 lbs, which was very concerning because I’d never been that heavy before. Once I was admitted into the hospital and started the melphalan then the stem cells, I didn’t want to eat. I had no appetite. No strength.
I was very, very weak. I felt like my mind was still intact, but my body was doing something of its own. That was very scary. You feel as if you’re in control but you’re not.
I went through the first 3 or 4 days very lethargic, tired, sleepy, and just somewhat coherent. Then I hit the point where your body is at its lowest point of immunity and you start to rebuild. I went through a cycle of vomiting and nausea. They had me on a lot of medications so I didn’t have much fever.
It was an experience that I can only describe as riding a roller coaster at full speed, coming off the steepest fall that you could imagine, and then having your head thrown back as if you’re catching a tremendous amount of g-force and trying to hold on for dear life.
You’re praying to the good Lord above every single day saying, “Please don’t let me die,” because no one’s bringing you any answers.
When no one’s bringing you any answers that you can wrap your mind around, all logical premises or notions go out the door. What do I have to rely upon if I can’t trust modern medicine? You only can rely on faith.
Every time, they came into my room and said, “We’re going to take you down. We’re going to run this test. We’re doing this. We’re doing that. We’re taking your blood. We’re checking for this. We’re checking for that. Sorry, Mr. Proctor, we don’t have an answer for you.”
If I wasn’t with fever, I think I would have said, “You know what? Let me out of here.” It was so frustrating dealing with inconclusive information.
I had so many doctors checking on me all the time because everybody was puzzled as to what was happening.
My private transplant doctor and the hospital doctor were at odds with each other. You could see the friction and intensity building up between them. One’s saying, “We may have to give him a blood transfusion if we can’t get his fever down,” and all these other things.
My wife and I said, “We don’t want a blood transfusion if my counts are where they need to be.” At the time, we didn’t know anything that can resolve this. They kept me on a slow drip to keep my fever under control.
Finally, around the seventh day, they came in and said, “We believe this is engraftment syndrome and we’re hoping that this will run its course,” considering that we were now approaching day 21 in the whole process. If my fever was kept under control without the drugs they were giving me, then they would release me.




Managing the side effects of the stem cell transplant
They give you something that’s going to harm you in one aspect and then they give you something to offset that. For me, it was a constant battle of dealing with this back and forth.
Psychologically, it wreaked havoc on me because I’ve never had to deal with an excruciating amount of medication so I was having a hard time trying to cope with it.
Very early on, my doctor said, “You won’t get a medal for how much pain you can tolerate. Take the tramadol if you’re in pain.”
The least amount of this stuff going through my body, the better because I didn’t want to get addicted. I was trying to put myself in a situation where I could think to some extent and not be completely in a brain fog all the time.
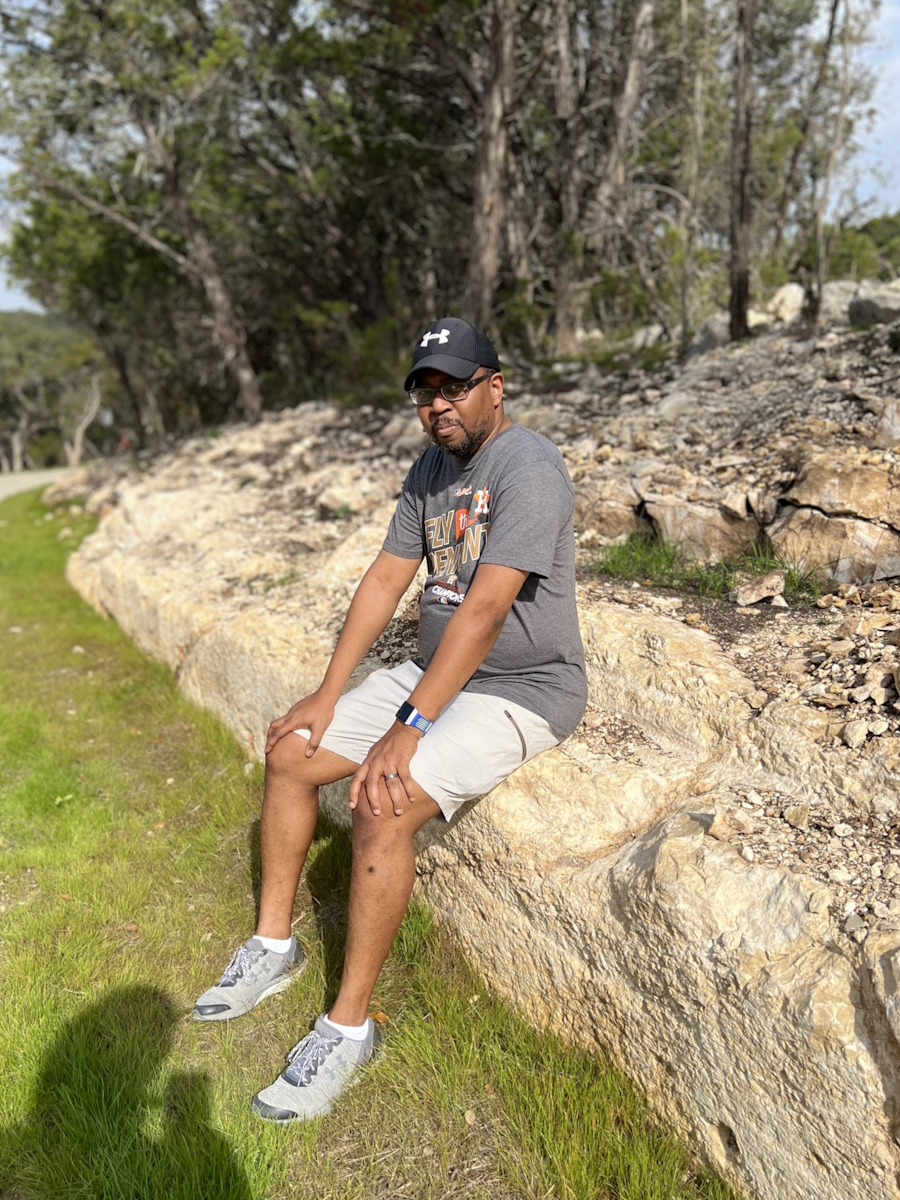
Post-stem cell transplant
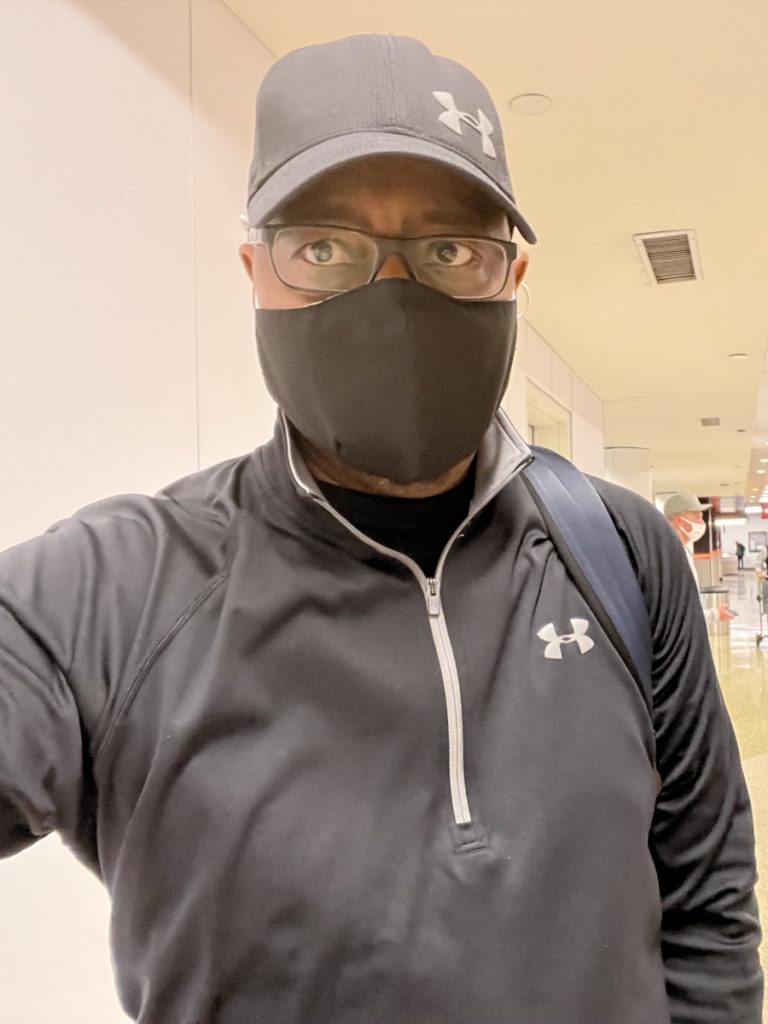
I get home and the only thing I want to do is sleep. I’m forcing myself to eat, drink, and rest. I only walked 15 miles throughout March. That’s how much energy I had.
As April began to roll around, my wife said, “Let’s see if we can get you out of the house. Let’s walk around the neighborhood and see how far you can walk.”
My doctors were calling and checking in on me. “Mr. Proctor, the more you can exercise, [the more] that’s going to help your stem cells rebuild and help the process move forward.”
We went from walking 15 miles in one month to averaging 10 to 12 miles per week in April. By May, we were up to about 25 to 30 miles a week.
I can only thank my wife and all of my family for helping us. The fruits, vegetables, and everything that was going on helped me rebuild as fast as I did and regain strength not only through medicine but through nourishment. Those were instrumental aspects of my expedient recovery.


Follow-up protocol
At the 100-day mark, they wanted to do another bone marrow biopsy. From the time I was diagnosed, it was going to be bone marrow biopsy number four.
We did the biopsy, the MRD test, PET scans, bone density scans, blood work, and everything across the board so we can have solid affirmation.
I’m MRD negative.
I thank not only my team of doctors but the good Lord above that these things have continued the way that they have. There’s been a lot of my work as well — eating healthy, exercising, and the regimen that I stay tried and true to from the time that I was diagnosed.
Words of advice
Do bone marrow biopsy under sedation, even if you have a very high threshold for pain. I did two with local anesthesia only and I would not recommend that to anyone. The last two were under sedation in a hospital. The recovery was so much better.
Once you’re diagnosed with blood cancer, understand that you’re not alone. There are thousands of other patients. Their experience can help you prepare for what is yet to come.
Appreciate every moment. Life is extremely precious. Even though you’ve been diagnosed with cancer, it’s not the end of your journey. We’re known for being warriors. In dealing with cancer, you have to have the fortitude and the mental capacity to see the other side.
Prioritize your health. Before the diagnosis, I was a person that had a sweet tooth. Those are no good for individuals diagnosed with cancer so you have to take it to heart.
Follow the rules. A lot of times, people say, “I don’t want to follow rules. Maybe I want to have a beer, I want to have this, or I want to have that.” The more you follow the rules, the better the outcome will be.



I used to drink. I used to enjoy having a candy bar. I don’t do any of that anymore. Everything I do now is based on what I know.
Whatever I consume, whether I made it myself or my wife made it herself or it’s from the restaurant we frequently go to, we know that things are made from a natural standpoint. I can’t emphasize that enough. Your body needs those nutritional elements.
Spend time with loved ones. You’re dealing with a circumstance, which is overwhelming psychologically, mentally, and physically. Have that affirmation of positivity around you all the time.
You’re dealing with so many things that are coming at you at once, whether financial toxicity, insurance, treatment routines, medications, or scans. You don’t control your life very much so when you have that time, embrace that to the fullest.
Don’t take anything for granted. Ensure that you live life to the fullest. They call me G 2.0. Put your attention to what makes you happy. Don’t let anybody steal your joy.
I was in the Navy and stationed overseas when I found out that my cousin had passed away from leukemia. He was a few years older than me — in his late 20s, maybe early 30s. He was on the list waiting for a donor for him to get a stem cell transplant. His body was unable to hang on.
I never knew about anyone in my family having any type of illness. As I grew up, even in the generations preceding me, we don’t talk enough about what’s going on in people’s lives. What we don’t realize is the impact and the implications of being able to share that information go a long way.
It’s really important to open up when you’re dealing with adverse situations, particularly with health or illness. There’s so much information out there. When you’re trying to find out genetics, you want to know if it’s in your family or the likelihood of it striking someone in your family.
Very early on, I wanted to share my journey, bring forth awareness, help people understand what I’ve gone through, and what they should look for. If I could do that and help one person, it would be of significant value to me.
I have thousands of people reaching out to me from all over the world. I do realize the aspect of being able to be vulnerable, to be transparent, to enrich others, and to provide that sense of empathy and compassion. Those go a long way.



Inspired by Gregory's story?
Share your story, too!
More Multiple Myeloma Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...





2 replies on “Gregory’s IgA kappa Multiple Myeloma Story”
Powerful stories so remarkable how each story has family, love, and faith!
I’m meeting my oncologist team on January 11th! I’m ready to tackle this disease head-on.
Reading these stories are very powerful and informative. I actually couldn’t put my phone down. Its a terrible disease. I’ve been smoldering for 9 years and recently my labs starting to go up. Right now I am at a month to month blood work and watch. Just about when I thought, my treatment is just about to happen, my labs dropped. I have been one lucky person. I am a RN and maybe getting some blessings back for all I have given.