Ashley’s Stage 4 EGFR+ Non-Small Cell Lung Cancer Story

Ashley was leading a career in her local community college, enjoying being around students, when she was diagnosed with stage 4 non-small cell EGFR+ lung cancer.
In this video series, she shares how getting her kind of lung cancer was like hitting the jackpot in the lung cancer lottery, taking a daily pill instead of infusion chemo, and diving into how her journey changed her perspective and outlook.
Explore her incredible 3-part story series below. Thank you so much for sharing, Ashley!
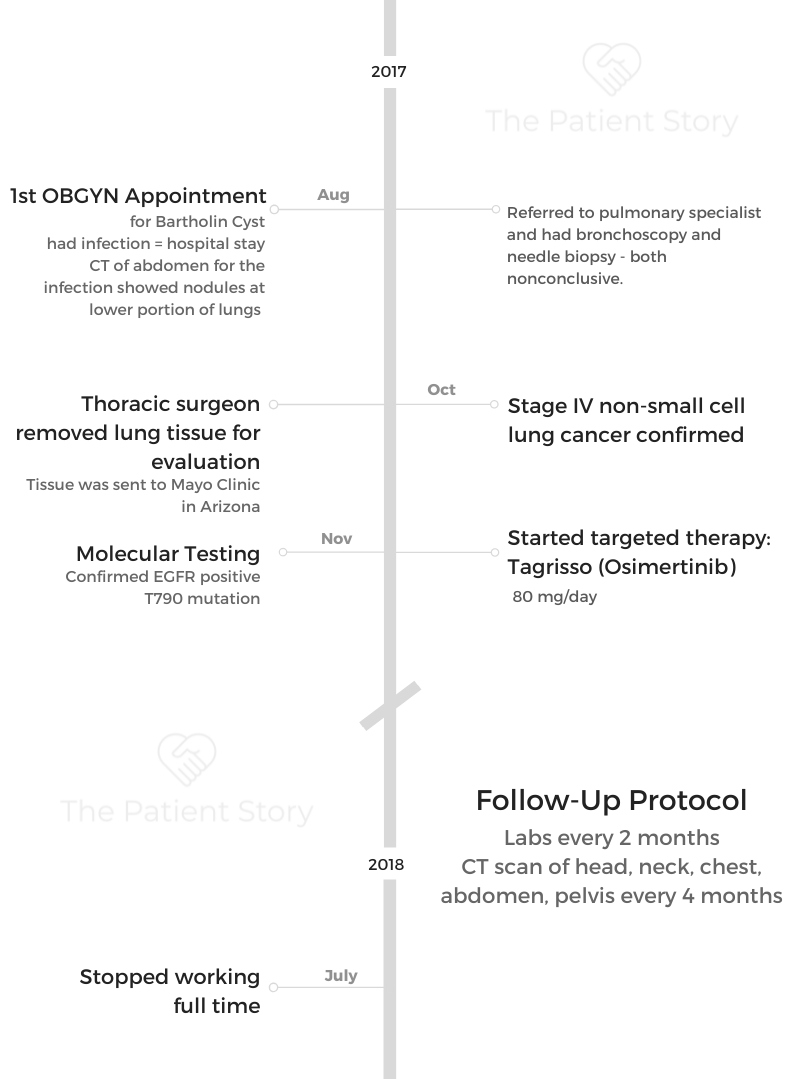
- Name: Ashley R.
- Diagnosis (DX)
- Non-small cell lung cancer
- EGFR+
- T790M
- Stage 4
- Age at DX: 36 years old
- Symptoms:
- Tiny nodules on both lungs
- Tests for DX:
- CT scan
- Tissue removal sent to Mayo Clinic for genomic testing
- Treatment
- Tagrisso (osimertinib), 80 mg/day
Ashley describes how seeing her OB-GYN for a cyst turned into news that would change her life: She was diagnosed with stage 4 non-small cell EGFR+ lung cancer.
Ashley takes us through the endless tests, treatment decisions, and how she is actually navigating her new take-a-daily-pill life. Ashley shares her treatment regimen, side effects, and some of the things she’s doing to feel better.
I thought, “There’s hope, and I can keep going. I’m not going to be taken out of here tomorrow. This is not a death sentence. I know what is possible. I know what the end result could be.”
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Ashley’s Lung Cancer Diagnosis
Ashley’s life outside cancer
I’m from Mississippi. I am an Air Force wife.
I am a mom to a spoiled little dachshund. I was in higher education in my career for many years. I was a registrar at my local community college and also worked in the registrar’s office at the University of Alabama. I enjoy students and all of that. I miss them sometimes. I love musical theater. I’ve spent a little bit of time on the stage putting up my heels, though, because I can’t remember lines anymore.
First encounter with the doctor
A doctor admitted me right away due to the severity of the infection. He said, “First, I want you to go to the imaging center so that we can know exactly where the infection is.”
It’s just typical of an abdominal CT to go up to the lower portion of your lungs, and that’s where nodules were noted. They thought, “Well, it’s not uncommon to have nodules show up in the lungs when there’s an infection in the body.” He said, “We’re not going to worry about that, but we are going to be solution-minded and figure out exactly why.”

Then 2 weeks later, we looked again, and they were still there when I went back for a follow-up. Nothing in the hospital mentioned the lung situation at that time. We only dealt with the issue that I was dealing with right then and there, but the doctor didn’t forget it.
He could have said, “It’s from the infection, and we’re not going to worry about it,” and sent me away. Then I’m a ticking time bomb. But he was solution-minded, kept a watch on it, and then forwarded me to a pulmonary specialist to look into this. It was very rare, so he felt it needed attention.
Initial diagnostic procedures
The pulmonologist initially did a breathing test. If you know anything about how it’s rated, I was at 94%. I was breathing fine. If you’ve never had one, it’s so hard to do all of that in and out.
I made it to the bronchoscope. I was under anesthesia, kind of in a Twilight Zone kind of thing. They did put me to sleep, but it wasn’t full-blown. I didn’t know what was going on, but I woke up pretty quick, too.
He did his own scans, of course, but it didn’t tell them anything. It was not conclusive, so we went to a needle biopsy. He obviously went in through my back to the biggest nodule that I had. I had over 100 spread across both lungs, 1 millimeter or less. There was one that was like 3 mm.
He went in to grab some tissue from that nodule that was a little larger than the rest. That, too, was inconclusive. By this time, I thought, “What is wrong with me?”
He asked me, “Did you do you work in the soil? Do you garden? Do you plant flowers? Do you work in a plant of any kind?” Those answers were no.
He showed me the scan. It looked like the most starry night you’ve ever seen in my lungs.
Those are all little tiny tumors. He said normally doctors would watch this for 4 months and see if anything has grown. If everything’s the same, then these are benign, and we’re just going to watch them. But he said this is very rare.

Observing my symptoms
I was 36 at the time. I’m 40 today. This is way rare for somebody that doesn’t work in the soil, doesn’t work in any sort of plant, doesn’t work around chemicals, and never smoked. He too was very solution-minded in trying to figure out what in the world it was.
I thought I have some sort of fungus in my lungs because he mentioned that. I thought I’m going to get an inhaler, we’re going to blow this junk out, and I’m going to roll out.
I wasn’t coughing. I was tired, but who isn’t tired? I work 40-50 hours a week. I wasn’t losing weight. I had occasional allergies, but I’m in Mississippi, and we have all sorts of stuff. I get a sinus infection every year but nothing abnormal at all.
Nothing had changed. This didn’t tell us anything. That’s when I was sent to a thoracic surgeon.
Even though sometimes you don’t want to know, but at this point, I wanted to know. My patience was on edge. I need to know now.
More diagnostic procedures
The thoracic surgeon wasn’t there to be my friend at all. He was all about business, cut and dry. That made me a little uncomfortable, but he was so knowledgeable. He was the very best I could have gotten in the entire state.
He comes in. He plopped down and said, “Here’s what we’re going to do. We’re going to collapse your lungs, put a tube down, go in, take out 2 or 3 sections of your lungs, and we’re going to send it off to Mayo to evaluate it.”
They didn’t know what it was, so they ended up going to Mayo. I was just staring at them.
I said, “Hold on, back up. You’re going to do what? Do we really have to do this?” He said, “No, it’s up to you. We don’t have to do anything. But if you want answers, this is what we need to do.”
We did it the following week. I went into the operating room, and that was the first time I had ever had anything major done surgery-wise. That was the first time I had experienced real anesthesia. I had a lot to take in. I had to sign papers saying that if they put the tube in and it did something else to something else in my body, they weren’t responsible.
It was possible that there could be an issue with my lung, and they would have to go back in if air got in there. I’m like, “Okay, I can do this. They’re the experts, not me. I won’t know it, whatever it is.”
Upon waking up, I was in a lot of pain. I felt like there were knives stabbing me in the chest. After a few hours with a morphine pump, I was okay. He removed the line and removed the tube, and I was okay.
They gave me a little bit more anesthesia than normal. I don’t know if I was being difficult or what, but it took me a little longer to wake up than most. The whole process was maybe around an hour from prep to recovery. I don’t recall exactly, but it wasn’t very long. That seems like a daunting process. They’re the expert, yet that was their first time.

Waiting for the results
By the time I left the hospital that next day, he did not know yet. He said he’d never seen anything like it. It was like ground-glass-looking nodules. That’s when the pathology went to the Mayo Clinic in Arizona to make the final conclusion.
Even then, I still didn’t have answers. It wasn’t until about a week later when that pathology was returned to him from the Mayo Clinic.
They tricked me at the doctor’s office, because he said the nurse called and said he was going on vacation. He wanted to check those incisions on the side.
My incision was fine. I knew it was fine but okay, so I went in. The doctor came in with that pathology report.

I was by myself. My husband didn’t go with me because I thought they’re just checking the incision. It’s not a big deal. I’m going to zoom over, go in, let him check everything, and come back and go to work. But that did not go down like that.
He was looking behind the door, looking around this little tiny room. He’s like, “Are you by yourself?”
I knew right then what was about to come. I knew. I just had this dark cloud of emptiness that just left. I can’t even explain it. I’m by myself. At that point, I thought, ‘I’m not going to fall apart. I’m going to do this.’
There was a gut punch, the sucker punch of my life, especially when you’re thinking it’s just benign. “Nobody has lung cancer in my family. I don’t smoke, so this can’t possibly be lung cancer.”
They concluded that this was an unfortunate case of stage 4 non-small cell lung cancer.
Both lungs were involved. It wasn’t anywhere else in my body, but both lungs had innumerable nodules. No surgery would benefit. I wouldn’t have any lungs left if they took out all those little bits.
Digesting the news of cancer
It was as if it was almost like an out-of-the-body experience. A dream I’m going to wake up from.
He was very not compassionate. He was like, “I’m sorry, darling, this is lung cancer. Do you want this report? She’ll help you with the rest. Good luck.” Pat, pat on the shoulder. Out he went, unbothered.
I know it’s not his job to feel sorry for me or to coddle me or whatever, but it could have been a little bit more. This is life-changing here. Anyway, he did a good job. The nurse was very kind to me and said she was going to be praying for me, which I welcomed.
I kept it together until I was in the room alone. When she went to make the phone calls, I opened up my phone and texted my friend that was a hospitalist for that hospital. I said, “I have to see an oncologist. Who do I see?”
I was fine. I could hardly see the letters or the numbers on the phone because I was fighting tears. The nurse came back in, and I told her who I wanted to see for my oncologist based on the recommendation of my friend.
Thankfully, I had somebody on that side of things that was in the know, because I didn’t know any of them.
I remember walking out of that doctor’s office, and the ladies at the front desk were like, “Hey, how are you?” They had no clue what I just heard. They were just doing their job and being nice, but I remember just not looking up at them.
I just looked down and handed them my paper, gave them my debit card to pay my copay or whatever it is I had to pay. I just kept my head down walking out that door.
That day, I was dressed for work. I had on dress pants and heels, and I felt like I had cinder blocks for shoes on my feet. I was putting one step in front of the other just to get the heck out of there. Just get me out of here.
When I heard the click of my car door, I lost it. I lost my mind. I was weeping and wailing. If somebody was nearby, they likely would have called a crisis intervention officer to come to help me, because I lost it. I cranked up my car and just sat there.
Breaking the news to loved ones
I had to call my husband and say, “This is what’s happening.”
I called my mother. She asked, “Do you need me to come and get you?” I said, “No, I can drive.” But I don’t remember the drive to her home. Then I called my dad.
The next day, I did a PET scan just to make sure there wasn’t cancer anywhere else in my body. It was a big 2 days.
I was on the phone the rest of the day telling people. They were calling me and sending messages because word traveled like wildfire. I was just mentally exhausted from the whole thing. To have to think about that and relive that in my mind…
People say it’s not a death sentence. But of course, I went straight to Google. I read about 2% or only teens, at the time, survive beyond 5 years. I thought, “I’m out. This is the end.”
That was heavy thinking about my own mortality. I still am forced to think about it, but I’m almost 4 years in. I have gained a lot of strength in that amount of time.

Lung Cancer Targeted Therapy (EGFR+)

Treatment and testing
My doctor initially, the gynecologist that found the nodules in the very beginning, was in our capital city in Jackson, Mississippi. When he asked about sending me to a pulmonary specialist, he said this is his friend. He knew him. I said, “Would you consider someone local to me?” He said he would prefer me to go see this person.
That’s how it unfolded. My doctor initially was already about 90 miles away from me. My mom lives there. It just made sense that since all the other doctors were there that I stay, too.
Plus, my whole reasoning for choosing doctors in that area is because the equipment is more advanced. They have incredible care within their hospitals. It’s just a personal preference for me.
Locally, we have a cancer center. We have 2 major hospitals. For me personally, I just chose to be there because I felt like there was better care there, more cutting-edge equipment
I think it’s very important that I have a facility that I trust, a facility that I know will fight for me because they’ve proven that they can do that in my diagnosis. It was just a personal preference. Like I said, it’s about 90 miles away. It’s doable to go and come in a day by car.
Completing the diagnosis
My tissue was already at Mayo Clinic from the thoracic surgeon that sent it over. I’m not sure who connected with who, but my oncologist was able to ask them to complete the biomarker testing.
I waited a long time for that. It felt like it was like a couple of weeks of calling. I actually went there for blood work shortly after, and he was like, “I’m sorry. We don’t have it.” I was almost harassing him.
Finally, he did get it back, and he called me himself. He didn’t send his nurse practitioner or a secretary. He called me himself and said, “Okay, here’s what you need. Here’s what we’re doing. This is the plan. I’m going to send the prescription over to where you want it.” I picked CVS Specialty.
My question was, “Can I have wine?” He’s like, “Oh, so you want to get sloshed now?” I’m like, “I have permission to do so, right?”
We laughed about that. His approach was, “Live your life how you would normally live your life. You just have to take a pill every single day. Don’t worry about restrictions. Do what you feel like doing.”
I’m going to be okay, but obviously with that comes side effects and a whole lot of things that I wasn’t ready for.
Treatment decision-making
At my initial appointment with the oncologist, there is a mountain of paperwork you had to fill out. He was with me for 2 hours because this was a new world. He told me that he was going to send off the tissue and request for further testing from Mayo Clinic.
He went down the list with all the possible courses of treatment: “If you have PD-L1, this is immunotherapy, this is what it does, and this is how you do it. Your hair will be fine. If you have ALK, it’ll be this. If you have this EGFR, there’s a brand-new drug called Tagrisso. It’s a targeted therapy. Take it by mouth. If you don’t have any, then you’ll be on traditional chemo infusion.”
The impact of a pill
I heard ‘a pill taken by mouth,’ and I’m like, ‘I want that.’ But it doesn’t work that way. You don’t get to choose exactly like that. He was rattling off all these letters and numbers, but the thing that resonated with me was the pill.
I was wishing I can do it, even though I had no idea about a mutation or a biomarker or whatever. Thankfully, he did.
Targeted therapy
I was EGFR T790M, and the oral treatment that I got to start targeted that exact mutation. It’s like I have the lung cancer lottery. If anybody can find something positive out of this, I felt like I had overcome the world. I thought, “Okay, I’m going to live. I’m going to be all right. More runway for me. Where are my pills? Give them to me.”
The FDA just approved Tagrisso (osimertinib) specifically for EGFR+ non-small cell lung cancer also with the T790 mutation.
I had seen people sick on infusion therapy, and I don’t want to be like that. There are people that are so terribly sick right now that are fighting just to get up out of the bed, feed themselves, and to go to the restroom.
I don’t take any of it for granted. I certainly do not brag and say, ‘Look at me. I don’t have to do all of that,’ because I know things will change. Eventually, there will be resistance. There will be a next treatment. I’m not going to get to sit here and be here forever.
I don’t take for granted that I was able to take something by walking to my medicine cabinet and swallowing a pill that has kept those cells at bay and has kept my cancer under control.
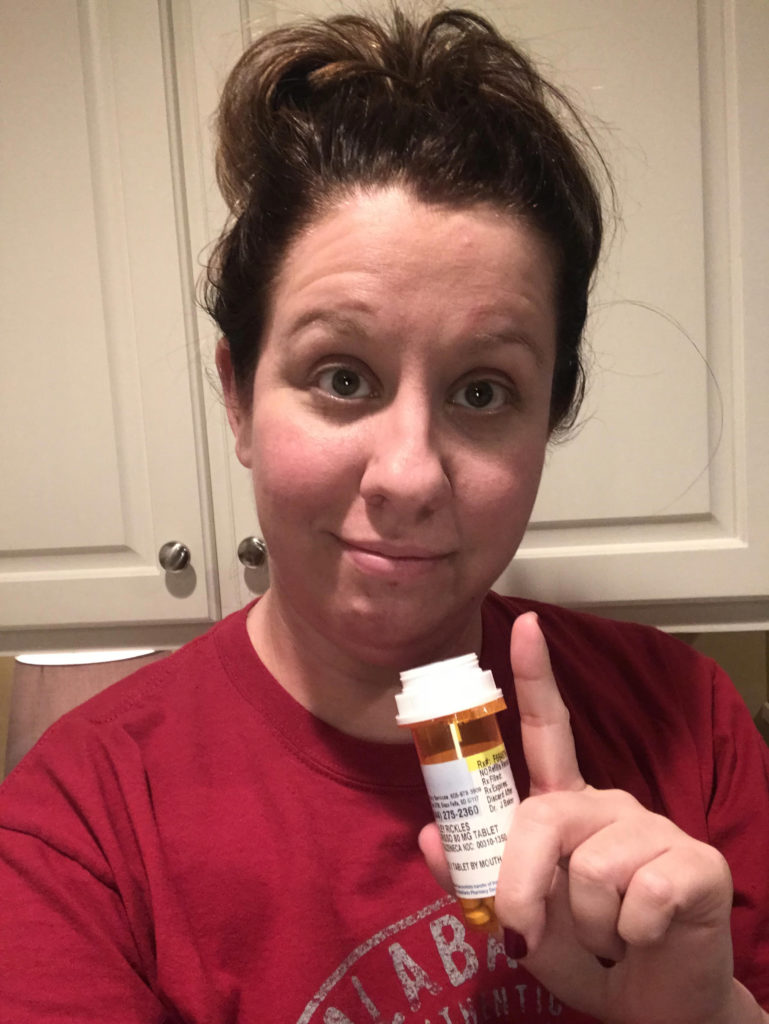
Treatment routine
For the very first time, I took my first dose at 9 p.m. In my head, I thought, “If I’m going to be sick from this, at least I will be in bed. I will be able to hopefully sleep it off.” That was my whole thinking around it, but it wasn’t like taking an antibiotic.
You feel funny within an hour. The side effects stay and come and go. 43 months in on the same drug, I still have no side effects. It’s just very weird and strange, but I’m thankful that I can still take it.
Side effects
At first, I felt very worn down. I felt heavy. It wasn’t that I wanted to sleep all the time, but I had very little motivation.
If somebody said you can stay in bed all day, I would say okay. That kind of leveled out. I thought this must be really working hard in my body, like a pregnant lady that’s tired. You’re growing a human; you’re going to be tired.

My body’s trying to get used to it and accept it.
There was a skin rash. I had these little things that looked like little acne bumps all over. But you couldn’t treat it like acne. If you tried to do that, it made it worse.
I was able to take an antibiotic to combat that. It only lasted for about 6 months or so. I don’t have any skin rash anymore.
Then I had a new symptom of GI flares. Sometimes, there’s nausea and a lot of upset stomach.
There was no rhyme or reason to it.
What helped with side effects?
Imodium became a staple in my purse, car, and my office — everywhere. I even made a joke at work. If I’m running, don’t stop me. I’m sorry, this is a fact of life. This is how it is. I still have the GI flares from time to time.
Exercise and diet
Some days, I get to move my body. Sometimes, I feel absolutely exhausted. I don’t know if that’s a combination of medication, being in the middle of the crisis our world is in right now, and staying at home.
Maybe it’s an emotional thing. Getting dressed is a major ordeal.
I tried to move. I had an exercise bike. I try to get on it. I go outside and tried to walk. But the biggest side effect with Tagrisso to date is fatigue.
Some days, if I want to just sit or stay in bed, turn on Netflix, turn on some music, and sit in the recliner or lay down, I will.
When I don’t eat junk, I do feel better. Diet does absolutely play a part. I can feel when I’m dehydrated. I love coffee, so I would much rather drink coffee all day than water all day. But I can feel the difference between when I do drink water and when I don’t.
I have to listen to my body.
I don’t have a port, so they actually stick me. It’s a lot harder for them to get a vein when I’m dehydrated, and it hurts. I get back to realizing I have to drink water whenever I’m going to the doctor. I noticed a huge difference when I don’t drink enough water. That often helps to boost energy.
I’m not a big supplement person. I know a lot of people rely on supplements, but I don’t. Every once in a while, I have vitamins and whatnot. Matcha and green tea, they say, are helpful. I might drink it today and then not for a month or 2 and then drink it again. I’m not consistent with it.
There is a holistic clinic near where my doctor is that does natural infusion. I badly want to go, but it takes $150 to do it. Insurance doesn’t cover it, but it’s all good things.
It’s supposedly all natural, and it would give you vitamins and minerals that your body needs to help. It’s specifically for cancer patients.

It’s okay to draw boundaries
I wrote an article, and it was on not feeling guilty when dealing with a physical battle, whatever it is, especially cancer.
I don’t have any children, so I don’t understand what that looks like for some. I feel like as a wife, I have the responsibility of keeping the house clean and having a meal on the table when he gets home from work. Some days, I just don’t feel like cooking. That’s the last thing I want to do, and he understands it.
Don’t feel guilty for the things you don’t feel like doing. Your body has changed. You are the same person, but you’re different. There’s a new thing in you that’s changing, and it affects people differently. Some folks still work full-time.
It’s okay to say no to family if you don’t want to do a family gathering. It’s okay to just say, “I’m going to sit at home, and I’m not going to go to that.” It’s important that we understand that we’re dealing with a lot.
Some might not understand us because they look at us on the outside and think, “They look fine; they must be fine.” That’s always a good education topic. We all don’t look like the cancer patient on TV, but we are still sick.
Sometimes we just have to educate others about how we’re feeling and not feeling guilty about it.
Getting the targeted therapy pills
My doctor called and said, “You have EGFR, T790. You need to be on Tagrisso. I’m going to call this then or send it up to the CVS Specialty pharmacy.” But they declined it.
I had no clue of any of this or how it all works. I’m on the phone with the secretary, and literally, she and I talked so much. I was writing letters. They were writing letters. too.
Thankfully, I had a very close friend that also works in oncology, and the doctor that she worked for prescribed Tagrisso. She said it has just been released as first line, so insurance companies don’t have the update because it is that new.
I got on the computer and Googled it. I found an article. I printed the article out. I put it in with my letter, and my husband thought to call the manufacturer, AstraZeneca, to see if they can help us.
He did. They wanted to speak with me. I talked to them, and they confirmed that it has been approved in September.
The lady at AstraZeneca said the insurance companies don’t even have the addendum yet because it’s that new apparently, and they’re later in their updating.

I did phone calls to AstraZeneca, to the insurance companies, and to the pharmacy like it was my full-time job for about 48 hours.
I wrote the letter. I printed out the article and sent it back to the insurance company. My doctor wrote a letter. AstraZeneca said they would be happy to write a letter, but it didn’t come to that. They did their own research and approved it.
In the meantime, AstraZeneca understood where I was and that I was a brand-new cancer patient. I needed to start my treatment. They put a starter of 15 pills, and I started that very next day free of charge. Everything worked out within about a week.
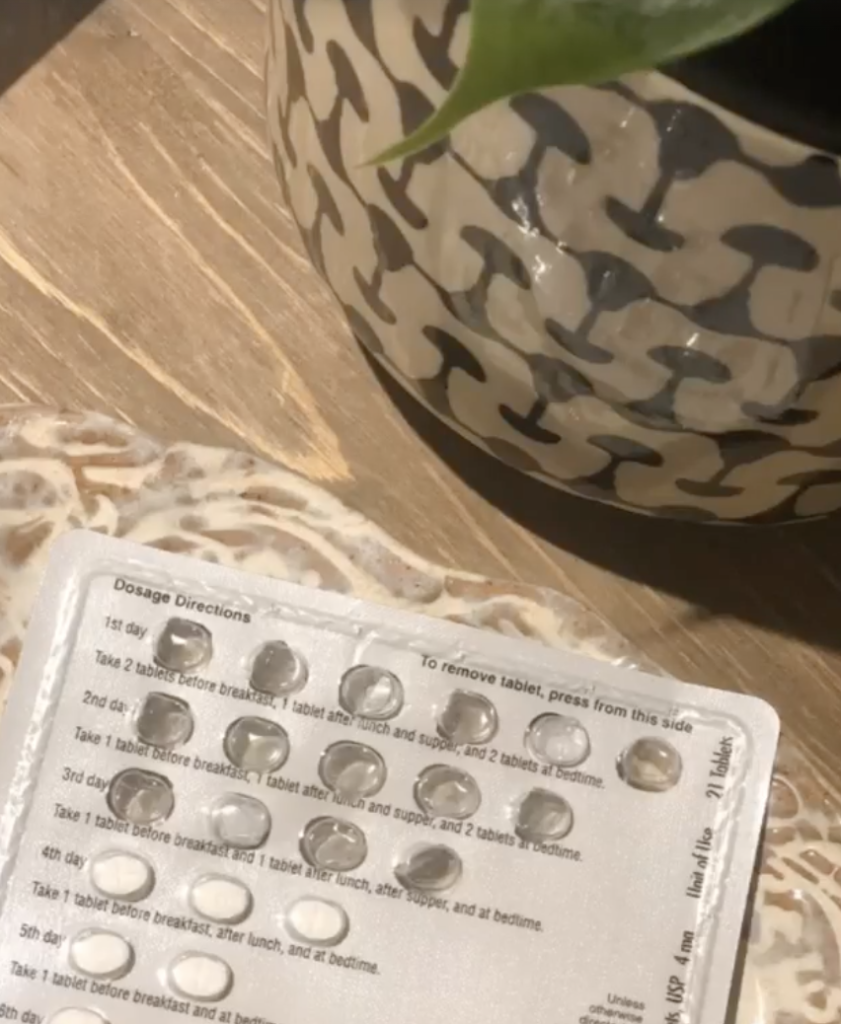
That was both an amazing experience and frustrating, to say the least, because I’m blind. I only ever had antibiotics for a sinus infection or upper respiratory sickness.
When the doctor sends in the prescription, there was really a lot of red tape you have to go through just to get in some sort of survival mode.
Here’s this cancer growing in my body. It’s been almost a month now. I need to fight this stuff, and I’m just walking around fighting to get the meds I need.
I was thankful. I was nervous to be able to start the drug because I thought of the possible side effects. Am I going to start throwing up within 30 minutes? Am I going to be able to hold it down? Because a lot of people can’t.
Thankfully, my body accepted it, because there are many out there whose bodies won’t. It’s a really awesome, incredible, life-preserving drug. We can’t thank enough for the cutting-edge research done on that.
Hopefully, there’ll be something next when I need something that’s similar to what I’m currently on for EGFR resistance.
Progress monitoring
I go every 2 months for blood work, and my blood work is fine every single time. It’s another thing to be thankful for because so many have to come off of their chemo because of different blood counts.
Then I have scans every 4 months. I was doing every 3, but we got pushed out to 4 months just to not risk getting any sort of radiation poisoning. Everything has been stable since.
I do CT scans. I don’t do PET scans. I just do head, neck, and basically full-body CT with and without contrast.
I’ve developed relationships with the techs and the nurses because I’m a frequent flyer! Sometimes they change out and I won’t know who’s there, but normally it’s the same people.
They’ve become my family. I could say, ‘Wink at me if it’s okay,’ and luckily I get same-day results.

Dealing with scanxiety
So many of my friends that I connected with and the lung cancer community have to wait days for their results. If that happens to me, I would lose my mind.
If I go get a scan at 7:30 in the morning, by 9 a.m., I’m sitting in the doctor’s office getting the results. We all have scanxiety. I’m thankful that I’m in a smaller community.
Living with Lung Cancer
Finally, Ashley shares how lung cancer changed her perspective, outlook, and her life.
To Ashley, she was lucky enough to be taking a daily pill instead of going to IV infusions, feeling like she still had some sense of normalcy. Despite her odds, she shares the gift of reflection and hope with her cancer community.
Here’s her story of living life with lung cancer. Thank you for sharing your story, Ashley!
Living with lung cancer
I made the mistake of going to Google. Then I started finding groups on social media and saw people that were living with this.
I thought, “There’s hope, and I can keep going. I’m not going to be taken out of here tomorrow. This is not a death sentence. I know what is possible. I know what the end result could be.”
I started looking at it as a chronic disease and then one day at a time. Because one day at a time is all we get anyway. I’m able now to think about things from a different perspective. I can get low. I can get sad, but I try not to camp out there.

Initially, when I was first diagnosed, I said, “This is what intentional living is supposed to look like.”
I always hear, “Cherish every day. Life is a gift.” Those are just pretty words. I didn’t truly understand it. It didn’t necessarily click.
When you’re faced with your own mortality and it is concrete that this might end sooner than later, then there’s a mind shift. There’s a perspective shift. There’s a new mindset that comes in.
Do I have it all together? No. Am I always positive? No. But I try to be positive, and I try to always share the good things in that Tagrisso group.
Inspiration in the community
I am proud to tell people I’ve been here for 43 months. To the person that just started last month or today or last week, I want to give hope. There were people in front of me through a screen that offered me hope when they were sharing their story.
None of it is obviously to brag or anything like that, but just to say I’m on this journey. I was 36 years old. It felt like the rug was ripped out from under me.
Ultimately, it’s the club that nobody signed up for. It’s the social club, the army — whatever you want to say —that nobody signed up for.
We were drafted, but there’s an entire international group of incredible people within this community that simply want the same thing, and that’s more runway.
It helps to have people that understand you.
My husband lives here in this house with me. We sleep in the same bed every night. But he has no clue what it feels like to have lung cancer. I can talk to him and tell him how I’m feeling until I’m blue in the face, and he still doesn’t have a clue.
When you connect with someone that also has just cancer in general, whether it be breast or any of it, we understand each other in a way that others can’t understand us. We understand a different outlook on life that others can’t understand.

Changing outlooks
I often say that I wish people could get just a glimpse of how we look at life now than before. I appreciate things that maybe I took for granted before — all the griping and complaining because somebody pulled out in front of you. Well, it’s not really important. Move along.
My doctor said you would revert right back, but I don’t want to do that.
A lot of people say cancer was the best thing that happened to them. It took me a while to understand that, but I understand it now because I’m loved by so many. Nobody necessarily feels sorry for me, but they show love. They check in on me, send me a message, and are praying for me today.

Prayer is the big thing in my life. It means a lot that somebody is thinking about me. Before, maybe I wouldn’t get those. It’s just been an incredible experience to be loved by so many people and also to be able to share like I’m doing today.
When I see or hear of somebody that’s newly diagnosed with cancer, regardless of what kind, I feel compelled to reach out to them to say, “Hey, you’ve got this. You’re going to fight. It’s going to get rough. You’re going to experience this, this, and this, but you’re going to be able to keep going. You’re going to get up every morning. Push through even when you feel like giving up, because giving up isn’t an option.”
We were handed this for whatever reason; we don’t know the reason. At first, I thought I was being punished for something, but that’s not how it works. That’s not how the universe serves us. That’s not what whatever higher power that you look up to wants.
This is merely something that has happened to us and not who we are. I only was able to grasp that through time, because it felt like I did something wrong to deserve this diagnosis, when in fact, it just happened. Like a car wreck. We didn’t know what tomorrow held before lung cancer, and we certainly don’t know what tomorrow holds with it. I try to keep that perspective as well.
Being able to take a daily pill
I think at the time, and even now, the pill road was more of a freedom. It’s hard going to the doctor when I’ve had other things come up. If it like was going to the doctor every single day, it’d be like a full-time job.
Taking the daily pill gave me a sense of feeling more normal, even though normal is basically sitting on our clothes dryer.
I try not to use the word ‘normal,’ because I don’t think there is really a normal. But for my own life, I felt like it would give me more of a sense of normalcy.
I wouldn’t be running to the doctor. I wouldn’t be going to the infusion room. I wouldn’t be constantly checking labs.
I had taken a pill before for something, and so that just felt like the normal thing to do. It was something I knew, whereas going to a chemo room with other sick people that were in all kinds of different stages and sitting for however long just felt heavy.
And it is. It has to be. I’m not there, but I have friends that have gone there. They make friends, which I like that part — developing relationships with those around you. I just wanted to be able to swallow a pill at my own home and not feel like I had to be interrupted.
I know one day that’s coming for me. I will have to go and do that. I feel like a targeted therapy is a little bit lighter on your whole body, the whole makeup of all the cells in your body, because it only attacks the bad cells and not the good, unlike what an infusion would. I guess it’s that piece.
There’s also that selfish piece of I want to be able to continue living as normally as possible without the interruption. That’s the selfish side of the treatment.


Inspired by Ashley's story?
Share your story, too!

7 replies on “Ashley’s Stage 4 EGFR+ Non-Small Cell Lung Cancer Story”
Ashley, your story has been very inspiring. After seeing the video, I wanted to see more of your story, so here I am! Even though I don’t currently have cancer, I had a “Wonky” mammogram in Oct ‘23, two ultrasounds and am now scheduled for a Diagnostic Mammogram & Ultrasound (same day) this coming April ‘24. Hoping my results are in my favor! I have watched some Breast Cancer videos over the last few months on what to expect. YouTube recommended your video and I decided to watch & listen. As I said earlier, you & your story are very inspiring. When I saw the pic with doc and you wearing your red sweater and houndstooth scarf, I thought, that girl’s an Alabama “ROLL TIDE” fan! And now, I’ll be darned, I was right! You got this! As a fellow fan, I offer you the best “ROLL TIDE” I can muster! Like I said, “You Got This”.
Are you sure Kay today, now, what medication are you on?
Hi Ashley,
Thank you so much for sharing your story! I am day 16 of Tagrisso after recently being diagnosed here in Ireland. You have inspired me and given me hope. It feels so strange and scary right now, but people like you sharing their story is such a help. I already feel a difference in the pressure in the side of my body from the one in my lung and the headaches have stopped from the one in my brain. I resonated so much with everything you said! Even though it was only two months ago I didn’t know about this, I now look back at the me before and think of how innocent and carefree I was!
Sending lots of love xx
Hi, Ashley,
Just wanted to say that you have imparted so much wisdom in your interview segments, filtered through your utterly charming personality and sense of humor. I am also a member of “the club”, a never-smoker who was diagnosed with stage one non-small cell lung cancer in 2015. Your observations are spot on regarding how cancer changes a person. Even with my early stage cancer, the whole experience was life-changing and sometimes people don’t understand that.
You are so eloquent and just a delight to watch. Thanks for sharing! And, all the best to you, your husband and your adorable pup.
Thank you Ashley for sharing your story. I can relate to all of this cause I was told I have lung cancer with the EFGR mutation this Sept 2022 and on the pill Tagrisso that was started immediately. I share all those feelings you mentioned and just do one day at a time. My family has been very supportive but our lives have changed going forward. A lot of Dt. Appointments and scans To read that you have years since you were given the news of cancer gives me hope going forward. I lost my husband 17 years ago to cancer and know what the road ahead is on going for me.
Ashley. Thank you so much for reaching out to others who have lung cancer like you. This is so compassionate of you. I was diagnosed with lung cancer September 2nd 2022. (It hit me like a bomb shell). Finally after my full diagnosis and biopsy I was prescribed Tagrisso Oct 7th. Yes I must appreciate a daily pill but recognize this can be for a short time.
thank you so much ..I have had a recent diagnosis of self with a brain metastasis..im also on tagrisso . im on day 18 early days
I’m trying to get positive
a lot of what you said about not having chemo .. resonates with me .. trying to remain ‘normal ‘ cook for my husband .. be at home although I’m exhausted .. I laughed when you said living on thd clothes dryer
sending you love
from the UK
rose x