Lauren’s Stage 1 Lung Cancer Story

Lauren’s story is a powerful reminder that lung cancer doesn’t discriminate. In her own words, “Cancer is cancer, and it will attack anyone.” Lauren, a vibrant 25-year-old with a love for hiking, running, and enjoying time with her dog and family, was unexpectedly diagnosed with lung cancer despite being a nonsmoker and living a healthy lifestyle.
From a young age, Lauren struggled with breathing, bronchitis, and pneumonia. Over the years, her asthma was treated with different medications, but her condition kept deteriorating. She vividly remembers the chronic wheezing that made even simple activities like running and hiking challenging.
Lauren’s medical odyssey took twists and turns. She endured multiple bouts of illness, testing, and incorrect diagnoses. At one point, she was even told she might have leukemia, but her diagnosis remained elusive. Finally, after persistent symptoms and a collapsed lung, Lauren’s intuition led her to push for a CT scan, which revealed a tumor. Despite facing skepticism, she advocated for herself and secured the necessary medical attention.
Her journey didn’t end there. Lauren underwent surgery to remove a tumor that had been growing for around 12 years, significantly impacting her lung health. With resilience and determination, she defied doctors’ expectations by returning to her active lifestyle within just a few months of surgery. She faced fears of illness, coped with post-surgery challenges, and navigated the anxiety of scan days.
Lauren emphasizes the importance of self-advocacy in the face of medical uncertainty. She learned that lung cancer isn’t solely linked to smoking and wants to spread awareness that anyone can be affected. By sharing her story, Lauren is dedicated to educating people about non-smoking lung cancer.
In addition to Lauren’s narrative, The Patient Story offers a diverse collection of lung cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Lauren C.
- Diagnosis:
- Lung Cancer
- Staging:
- Stage 1
- Initial Symptoms:
- Chronic wheezing
- Difficulty breathing
- Recurrent pneumonia and bronchitis
- Treatment:
- Surgery: VAT surgery (video-assisted thoracoscopic surgery)


Introduction
I’m Lauren. I’m 25 years old. I love hiking, running, biking, doing some arts, music, and hanging out with my dog and my family.
Pre-diagnosis
Initial symptoms
When I was younger, all of my friends, including my twin sister, had grown out of their asthma. I never had any asthma issues. But then when I was around 9 or 10, I started struggling to breathe all the time. I would have bronchitis and pneumonia multiple times each year to the point that I would have to be on an air mask for a nebulizer and missed a lot of school.
As I grew into a teenager and went to college, my asthma only got worse. They kept giving me different inhalers, different medication. I got more and more bouts of bronchitis and pneumonia and I would spike these random fevers out of nowhere.
I had this chronic wheeze that would never go away to the point that everyone kept calling me wheezy. Every breath, it would just be constantly wheezing, which is hard when you love hiking and running and doing all the sports.
When I was in sixth grade, I went to a primary doctor appointment and my blood work came back with low red blood cell counts and abnormal white blood cell counts. I don’t remember if they were low or high or what was going on. They sent me to the hospital, which then sent me to a different hospital because they were telling me that I had leukemia, but then they sent me home that night and nobody ever followed up with me on it.
Twelve years later, I ended up in the hospital again because I couldn’t breathe. I had these high fevers going on for months and months, and that’s when they found a collapsed lung.


Realizing the symptoms weren’t asthma
I trusted my doctors, but I would tell my parents, “These inhalers aren’t working for me. This medication that they’re giving me isn’t working.” I got bronchitis, they give me antibiotics, and then a week later, they’re giving me more antibiotics.
In 2021, I started to realize it wasn’t asthma. I remember telling my family, “I think I have lung cancer,” because I had nine out of the ten symptoms. Everybody said, “No, the doctors will tell you,” so that’s when we really pushed for a CAT scan.
Symptoms intensified
I had some leg pain going on for a couple of years and I thought it was just varicose veins or whatnot, but my legs hurt so much. Breathing-wise, it wasn’t as much pain as it was a constant tightness. I’d always felt like something was squeezing me.
I have always been a great swimmer. In 2021, I went to a lake with my boyfriend and his friends. I hit the water and immediately started drowning. I couldn’t breathe. I was blacking out so they dragged me back to shore. Since that day, I kept getting sicker. I figured it was because I worked with kids so I was getting sick.
They treated me for bronchitis, then a sinus infection, then pneumonia, then an upper respiratory infection. I had four rounds of antibiotics. I kept spiking these fevers and they kept telling me it could be COVID, but I never tested positive for COVID.
In November 2021, I was at work and they sent me home early because I had on a long-sleeved shirt, a sweatshirt, a jacket, my 30-below sleeping bag, and I was shaking. I drove myself to the emergency room. I had a 104°F fever.

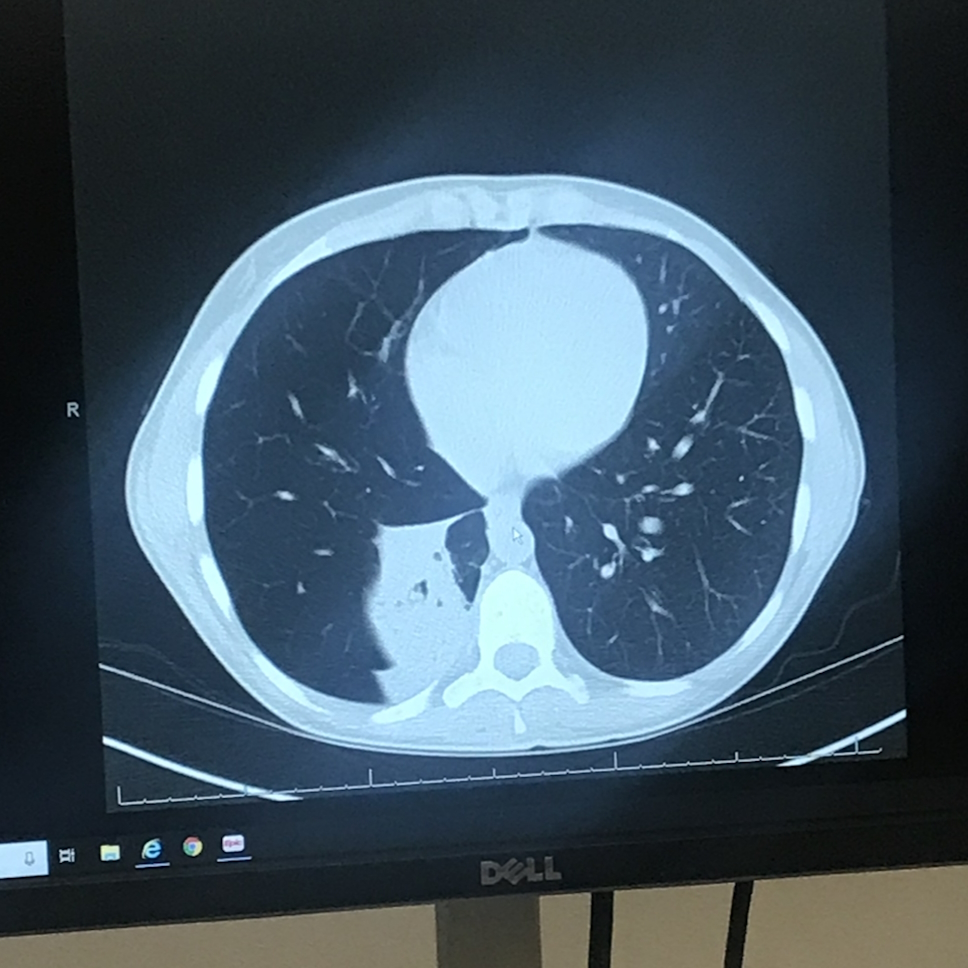
They tested me for every blood disease. They took a chest X-ray and found out I had a collapsed lung, which explained the reoccurring infections because the infection was trapped in my lung.
They told me it was a mucus plug or scar tissue that was causing the collapsed lung and that it will go away. But at that point, after three months of being extremely sick, I knew I had lung cancer. I kept telling everyone, “I think I have lung cancer.”
My mom and I said, “We are not leaving until we get a CAT scan booked.”
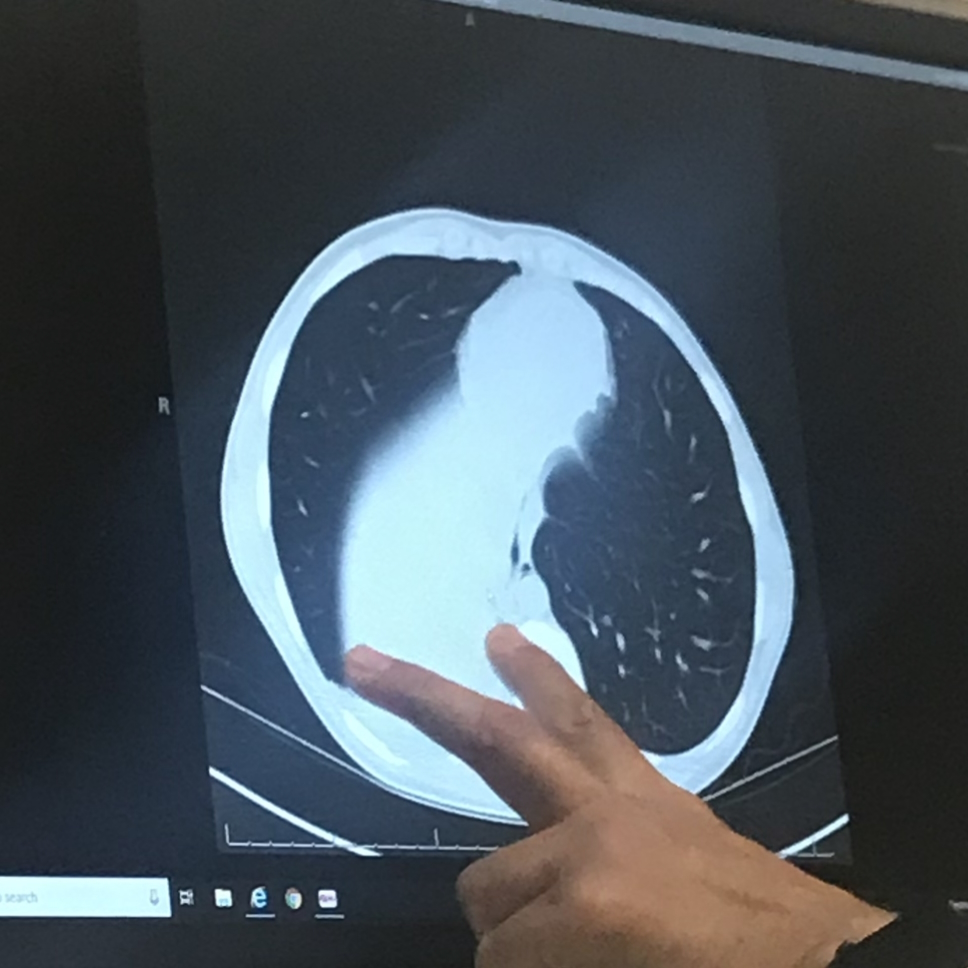
Diagnosis
Getting the diagnosis via phone call
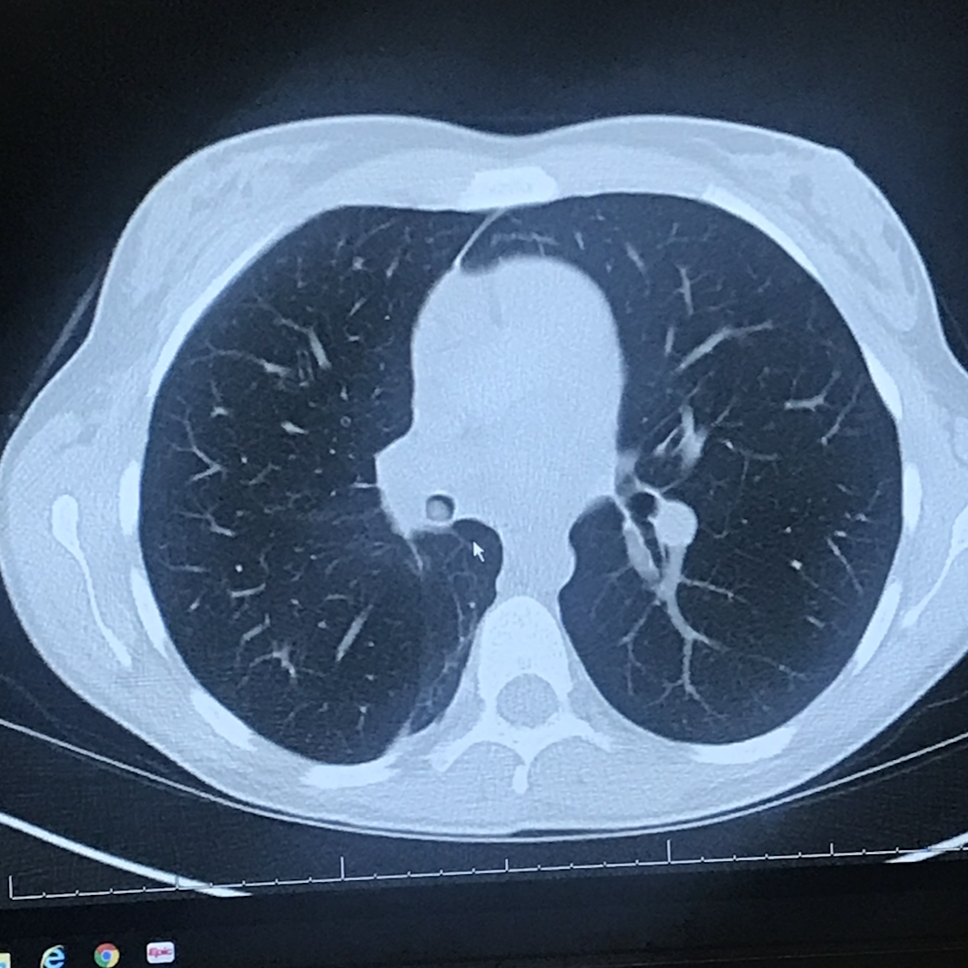
A month later, I got my CAT scan. It was a Friday night and they told me to wait until Monday, Tuesday for my results. But before I even arrived home, they called and told me that I had a tumor and they wanted me to go see a specialist right away.
The specialist they wanted me to see was booked all the way until April so they set up an appointment five months after telling me that I had a tumor.
Looking for an oncologist
The next Monday when I was able to go to work, I called my insurance company and begged them to send me a list of every single specialist in the area. They sent me a four-page list. That day, my mom and I called every single number on the list. Only one place took our call and they had me into the hospital within two days.
I was not comfortable with the fact of knowing that they had missed it for how many months. At that point, I had a collapsed lung since probably September. Now it was December and they wanted me to wait another five months.


Being dismissed by your doctor
I had seen my primary care doctor so many times. I mentioned to him that I thought it was lung cancer. He said, “It’s not cancer. You’re too young. You don’t smoke. You don’t live with anyone who smokes.” But, of course, then he had to say, “It could be, but I’m just telling you it’s not.”
I’ve seen him a couple of times since and it’s definitely been a very different type of relationship. He’s apologized, obviously, so much for it.
There’s no explanation for why I have lung cancer. In my case, it’s not genetic. I don’t have any of the gene mutations. I don’t live with smokers. I’ve never lived with smokers.
We’ve tested my house for radon levels. If it’s four or higher, then you’re likely to have lung cancer, but mine’s at one and sometimes below one so it makes no sense. It’s just where my cancer decided to grow.
Bronchoscopy & tumor biopsy
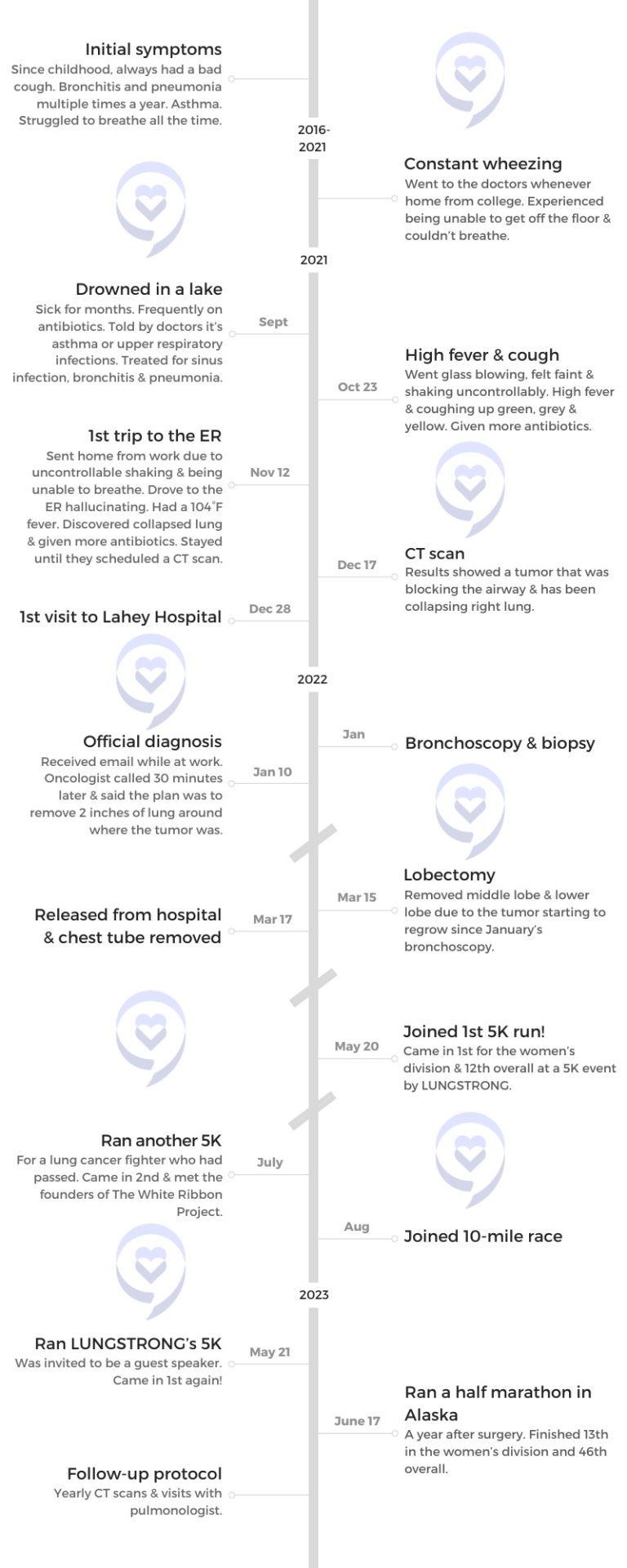
I had my first CAT scan when they found the tumor on December 17, 2021. I went to Lahey Hospital to see my specialist on December 28th. Before the doctor even said hello to me, he came and asked if I ate breakfast that morning. He said, “If you didn’t, I’d be putting you into an emergency bronchoscopy right now to get that tumor out because that needs to leave right now.”
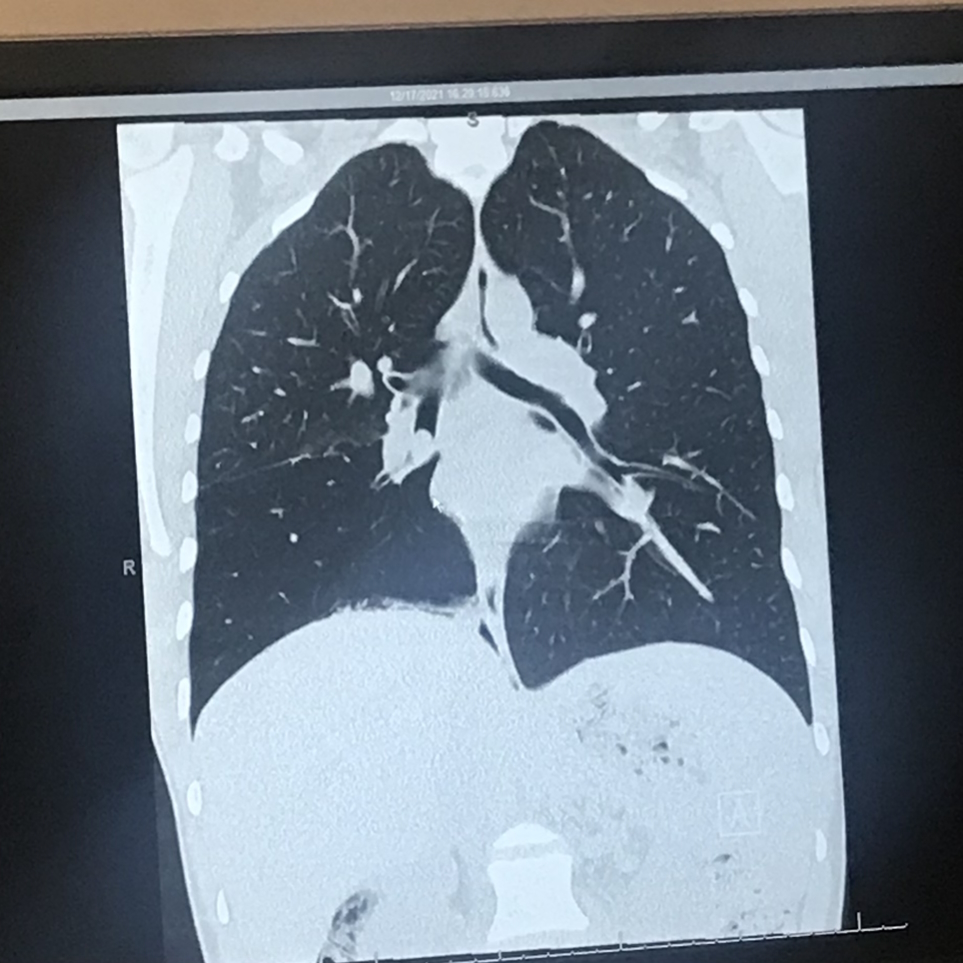
A week later, on January 6th, 2022, they did a bronchoscopy to remove most of my tumor. They biopsied it but left some of it in there because it was too dangerous to take it all out during a bronchoscopy. They took enough out that my lung could open back up because it was completely blocking off the airway in my right lung.
It’s just a quick procedure. They put you under and they go down through your throat. They were able to go into my airway and my lung and cut out the tumor. They were able to remove it and biopsy it that way. It was very quick. I think I was only under for maybe 45 minutes.


Getting the official diagnosis & staging
On January 10th, while I was at work, I got an email from the hospital. I figured it was just a bill, but the email said, “Your tumor had tested positive for bronchial and lung cancer.” It was CD56-positive, which is a neuroendocrine tumor.
I’m still not quite sure about the stage, but some doctors have said stage one; some said that they don’t really know.
They had told me that it looked like it was probably growing for about 12 years so that’s what kept making my asthma get worse and worse. It was actually just a tumor slowly blocking off the air. It grew inwards into the big hole of the bronchial instead of the lung.
They said it’s a very slow-growing tumor. A lot of doctors kept telling me, “It’s the good type of tumor.” Is there a good type of cancer? People kept saying, “Cancer was kind to you. It grew slow and took your time.” We could have caught it earlier.
Reaction to the diagnosis
I left work when I got the diagnosis. I remember just crying in the car with my mom for five minutes. I turned to her and said, “Crying isn’t going to do anything. What can we do to be proactive about this?”
My oncologist called me later that night and knew that the email went out. She was very mad that somebody had sent the email to me and that’s how I found out that I had cancer.
She was telling me that the next steps were going to be to remove the rest of that tumor. At that point, they thought that it was only going to be removing two inches of my lung so we were getting ready for that.


Treatment
Meeting with the surgeon
They sent me to the surgeon. He was looking through my case and said that they would have to most likely remove the whole lower right lung lobe just because of where the tumor was growing. It was growing so much into that area that they would have to remove it in case it was spread.
For months, I was only prepared for the lower lobe to be removed. They kept telling me all the things that I wouldn’t be able to do after surgery, things I could do after surgery. My lifestyle was going to change forever at the age of 24.
Video-assisted thoracoscopic surgery (VATS)
I went into surgery on March 15th. I woke up with my lower lobe missing and my middle right lobe missing because the tumor just started to regrow into my middle lobe as well as the lower lobe.
After my surgery, they did talk about maybe doing some radiation. But as of right now, it looks like everything is stable so they don’t want to have to put me into treatment as long as I don’t need it.
Video-assisted thoracoscopic surgery is robotic. They used to have to pry open the ribs. They cut in between the rib cages to cut the lung out, pulled it out, put a chest tube in, and stitched it back up.
They wanted me to stay for a week, but I only ended up staying for two days. All these different medications and sleeping.
I kept forcing myself to get up and walk to the nurses’ station and to the end of the hall. I couldn’t stand just laying there and knowing that things were going to change. I wanted to go back to normalcy as soon as possible.


Recovering from surgery
I still don’t always feel very recovered. I still get pain in my scar tissues and even down towards my stomach area. They said that’s normal because of my age. My nerve cells are still young and most people who get the surgery are older and their nerve cells are dying so it’s not as painful for them.
They wanted me to stay for a week, but because I was doing so well and forcing myself to get up and move, they sent me home two days after my surgery.
At that point, I forced myself to get up and walk at least five times each day: to the end of the driveway, to the end of the street. Less than two months after my surgery, I did a 5K and ended up winning. I was back doing that within two months.
It was honestly just pure determination. When I was running, I kept thinking my lung was going to explode and I was going to have a heart attack. It was a lung cancer event so there were a bunch of doctors. There’s a bunch of doctors here. If I pass out, I’m going to be totally fine.
It didn’t take as long as I thought or what the doctors thought it was going to take.
Post-surgery results & monitoring
I don’t have any signs of more cancer, which is awesome.
I did CAT scans once every three months and then it was once every six months and now it’s once a year. A lot of going back to the pulmonologist to do follow-up appointments with different medications.
I’m still trying out different inhalers because I still do get very wheezy and very tight, which is normal they said.


Life after cancer
Dealing with anxiety from feeling respiratory symptoms
Cold and flu season was coming back around for the first time since I only had one lung and I was so scared. I still wore my mask all the time. Even if I’m going to really public places, I’m still the only person in a mask. I’m still petrified of getting sick.
I had bronchitis maybe three months after my surgery and my doctors said, “Do you need to come to the hospital?” And I said, “I’ll be okay. I’m going to just lay low.”
I had a really bad flu in January 2023; that was really scary. Sometimes when I get very anxious or anything, I can’t breathe and I can’t even speak.
Continuing to process the cancer diagnosis
I’m still processing it. Sometimes I’ll brush up against my scars with my fingers and freak out. What is this on my body? Every day it takes up the majority of my thoughts like, I can’t believe I have one lung and I’m doing this, or, I just did a half marathon in Alaska, and the doctors had told me that I would never run again or that I would never hike again.
Every time I hike a mountain, I feel so proud of myself and so accomplished. Even with just day-to-day things, I’m petrified of what’s going to happen, but then I’m proud of myself that I made it through another day each day. It’s a very strange thing to have.


Being able to run & hike again
I had two months of medical leave after my surgery so I had a lot of free time. On my walks, I kept trying to extend them further and further.
The first day after I got home from the hospital, I’d do a quarter mile and then go back, and keep building and building and building.
Somebody in the cancer community reached out to me that there was going to be a 5K for lung cancer called LUNGSTRONG and she wanted to meet up with me. We could walk the 5K. I wanted to run it because the doctors had told me that I would never be able to run. I was 24 and can’t listen to what the doctors say.
On my walks, I would start running the downhills. Then I would start doing the downhills and the flat surfaces. Then I would start adding the hills. By the time of the 5K, I hadn’t built myself up to three miles yet, but I did it.
During the two months I had off, I would go on short hikes with my dog and my boyfriend. Eventually, we built it up to do Mount Washington. I take my time if I need to, but I’m keeping up with everyone who we’re hiking with.
Honestly, I think a lot of it was that I am so young that my body could recover and that I did have a very active and healthy lifestyle before my surgery. What’s left of my right lung is slowly starting to expand back into that space that my two other lobes were removed from so I think that’s helped a lot.
I honestly think it was just a lot of determination and not giving up because cancer can take so much from you. It took my lung, it took part of my breath away, but it can’t take anything else away from me.


Managing the risk of respiratory infection
The mask is definitely one thing that I do. I get very mad when I go places with my family and they’re not wearing a mask. Other people in my life will wear a mask just for me so that’s been very awesome and supportive to see other people wearing a mask around me.
When I hear of a certain person I know is sick or something, I stay away. I avoid certain areas a lot.
I’m starting to go back out to things like concerts and on airplanes again. But for a long time, I was absolutely petrified of going anywhere. I would make people go to the grocery store for me. I was afraid to go back to work. I was afraid to do anything. But I work outside, luckily, so I’m okay.
When I had the flu, they gave me certain medications to help shorten the flu symptoms, but I ended up having symptoms for a month straight. When I got bronchitis, I’ll have it for maybe a month or two.
I haven’t had COVID yet, knock on wood, but I’m definitely petrified if I ever get COVID because it’s a disease that attacks your lungs. When I was super sick, it was 2020 and 2021. I was diagnosed in 2022 so I was just so scared to know that I had lung cancer and there’s this disease going around that attacks your lungs.
I had to go to all my doctor’s appointments alone. Luckily, after my surgery, they allowed my parents to come and see me in the hospital. But it was definitely very scary and it still is very scary.


The stigma of lung cancer as a smoker’s disease
What I’ve learned from the lung cancer community is that lung cancer can happen to anyone. Even just cancer itself. It’s not biased. It’s not prejudiced. It doesn’t care what you look like. It doesn’t care what race you are, what religion you are, anything. Cancer is cancer and it will attack anyone.
It doesn’t matter if you’ve smoked. It doesn’t matter if you live the healthiest life. You have lungs and anyone with lungs can get lung cancer just like anyone with skin can get skin cancer and anyone with breasts can get breast cancer. It’s just something that happens.
It’s a shame that when I tell people I had lung cancer, a lot of them ask me, “Who in your family smoked?” Or, “How much did you use to smoke?” I never have and no one in my family has so I just really would love to just keep spreading the word that anyone with lungs can get lung cancer. Most of the people that I know with lung cancer have never been a smoker. I think I know one person out of the 50 people I’ve met with lung cancer who has been a smoker.
Lung cancer is on the rise for a lot of young people and females especially. It’s the number one cancer killer in the world. It claims more lives annually than breast cancer, prostate cancer, and colon cancer combined. Nobody seems to really care about it because they just have this assumption.
Being a lung cancer advocate
We learned in high school that you can only get it from smoking and that’s why I went back to my high school and spoke at one of their events to let the kids know it’s so much more than a smoker’s disease. I was only told it was from smoking and I avoided cigarettes my whole entire life. And here I am, you know?
You know your body more than anybody else does. The doctors can see the test results. They can see you physically, but, ultimately, you know your body.
When I was telling everybody that I thought I had lung cancer, even my parents said, “No you don’t.” And I said, “Mom and Dad, you see me coughing up different colors. I’m very sick.” Again, you know your body and you have to push for it.
The doctors want you to get better and they want you to feel better so sometimes, it’s easy to miss something, especially because of your age and your lifestyle.


My mom is a nurse and, luckily, she was with me that day that I found out I had a collapsed lung. She kept saying, “Hey, I know this routine. We want a CAT scan and we want it now,” and they kept trying to send us home. “We’ll call you later for the CAT scan,” and my mom said, “We are waiting to put it on the books. We need it now.” If you have to force it, force it. It’s that simple.
They want you to go in and get out as fast as possible so they can take more and more and more patients. A lot of people go to the hospital for help, but you are also there for help. If you need to be pushy and kind of annoying, so be it. You need the help to get it. It’s not simple, but if you need it, you need it.
Follow-up protocol
Then it was just a lot of doctor’s appointments, more PET scans, CAT scans, and X-rays.
Managing scanxiety
When I have my scan days, I take the full day off of work, even if I don’t need it, even if I’m feeling confident, fine, and don’t need the whole day off. I try to make the appointment as early as possible so I can get it over with quickly and spend a day doing things that I want to do.
I’ll get my scan then go and treat myself to fancy coffees only on scan days so it’s something that I look forward to. If I go to a store that I pass by, I allow myself to buy one or two things that I normally wouldn’t buy for myself on a typical day. I allow myself to do that.
I take myself on a trip somewhere; not a big trip, but to the national park nearby or to the mountains or a weekend away somewhere and make it into a celebration as well as something to look forward to. I do have my scan that day, but once I’m done with the scan, I get to go and do this. I have this to look forward to.


Words of advice
You are all really so strong. Everyone’s story is different. I know sometimes people, at least the lung cancer community, see me going out, running, hiking, and everything while they’re not.
Everyone’s story is different. This is my story. I’m still suffering all the time with this, but it’s all ultimately up to you what you do with your story and your message so you can make your mess and make it into a message, honestly.
I run and I hike for people that can’t do it. I do it for my friend who passed away two years ago from lung cancer. She kept telling me, “One day, I want to go up and meet you. Let’s go for a walk. Let’s go for a run. I saw that you did something today and it motivated me to get up and off the couch for the first time in a long time.”
I want to prove to people that doctors can tell you all the things that you can’t do. They have a list of the can’t, can’t, can’t, can’t, can’t. Again, you know your body so if you feel like you can go and do one of those things, do it. Push yourself a little bit harder each and every day.
It’s okay to fail. It’s okay to cry. It’s okay to be upset with this. We have cancer. It sucks. It’s terrible. There’s nothing we can do about the fact that we have cancer, but there’s so much that we can do with the fact that we have cancer and that could be making a positive difference.


Inspired by Lauren's story?
Share your story, too!
More Lung Cancer Stories
Luna O., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptom: None involving the lungs; severe abdominal pain
Treatments: Chemotherapy, targeted therapy
Calvin M., Lung Cancer, Stage 1
Symptoms: Frequent illness (monthly cycles of sickness), breathing difficulties
Treatment: Surgery (pneumonectomy)
Jill F., Non-Small Cell Lung Cancer with EGFR Exon 19 Deletion, Stage 1A
Symptom: Nodule found during periodic scan
Treatments: Surgery, targeted therapy, radiation




One reply on “Lauren’s Stage 1 Lung Cancer Story”
I had the same cancer – diagnosed and had a RLL lobectomy in Feb 2023 at age 43.