Michele’s Acute Myeloid Leukemia Story
Michele loved the outdoors and the beach. At 24, she was living a vibrant and active life until she was diagnosed with relapsed refractory acute myeloid leukemia.
In this video series, Michele shares her story of diagnosis, chemo and stem cell treatment, relapse, and the side effects she had to endure. Her continuing journey through AML is such a shining light of inspiration, especially for young cancer patients.
- Name: Michele G.
- Diagnosis (DX)
- Acute myeloid leukemia (relapsed/refractory)
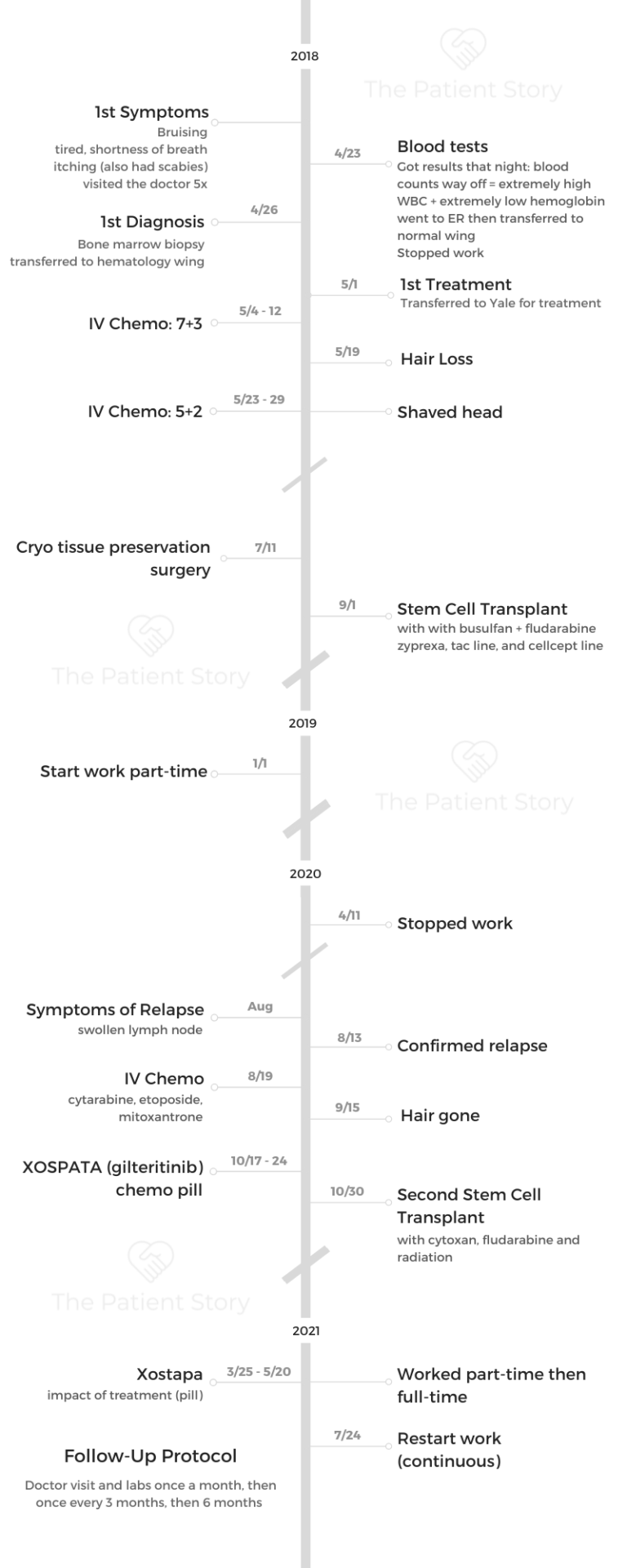
- 1st Diagnosis:
- Age at DX: 24 years old
- Symptoms:
- Bruising
- Tiredness, shortness of breath
- Itching
- Tests for DX:
- Blood tests
- Bone marrow biopsy
- Treatment
- 2 stem cell transplants
- IV Chemo
- Targeted therapy (Xospata)
- How I Got Diagnosed
- Going Through AML Treatment
- Video (Part 2)
- What made you change hospitals?
- How did you decide which treatment to take?
- What did you get for your chemo infusions?
- Describe the bone marrow biopsy
- Describe your chemotherapy and side effects
- Tips on dealing with a long hospital stay
- What helped reduce the side effects?
- What helped gain back some weight?
- The 1st stem cell transplant
- The medications taken post-transplant
- Describe the follow-up routine
- Managing anxiety before each bone marrow biopsy
- Relapse and Treatment
- Video (Part 3)
- Symptoms of the relapse
- Processing news of the relapse
- The benefits of meditation
- Describe your relapse treatment plan
- Differences between 1st and 2nd stem cell transplant
- More transplant side effects
- What was the radiation like?
- FDA Approval of Xospata (gilteritinib)
- Describe the Xospata and side effects
- Impact of taking a pill instead of getting an infusion
- Survivorship: Life After Diagnosis
- Video (Part 4)
- How to deal with the hair loss
- Deciding whether to stop or continue working
- The experience of being a young cancer patient
- The importance of fertility preservation
- The process of cryopreservation
- Perspectives learned from living with cancer
- The importance of self-advocacy
- Why I share my patient story
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
How I Got Diagnosed
Video (Part 1)
Michele tried to ignore the bruising, tiredness, and shortness of breath.
At 24, she was living an active and healthy lifestyle. Michele enjoyed playing sports and exploring the outdoors with friends, but the persistent bruises and itching prompted her to several doctor’s visits. Her labs eventually revealed she had acute myeloid leukemia (AML).
Here, Michele tells us how she faced and accepted her diagnosis.
About me
I’m from Connecticut. I enjoy just being outside. I love going to the beach, and also I love playing sports. I play basketball and soccer. I just like being active and healthy eating. I love to cook as well.
I recently got very into cooking tofu, which I know is very different. [It’s] something that doesn’t have a lot of flavors, but you can add flavor to it to make it delicious.
My AML symptoms
Throughout high school, even college, I never used to get sick at all. But a couple of months before my diagnosis, I started getting sick.
I had a lot of sore throats. I went to the doctor probably at least 5 times. They just would give me Claritin.


At the time, I’m just hanging out with friends, doing all these activities. I’m overworking myself. I didn’t really think anything of it. But when I look back, all the symptoms were there.
I had shortness of breath. Walking to my car, I’d be out of breath. I went to work one day, and I was there for an hour. I was exhausted, so I ended up going home and just sleeping that afternoon. Then I would get little bruises on my body. I thought I must have run into something, not a big deal, but I was itchy. Separate from the diagnosis, I ended up having scabies. But before I went to get my lab work done, I itched myself so much.
I was bruised all the way down my legs and on my back. That’s when I thought, ‘I need to go to the doctor.’
When I realized how serious this might be
It’s hard, of course, in retrospect. It’s easy to draw the lines and connect the dots afterwards. But at the moment, it’s so easy to explain away every symptom. I think so many of us experience that.
The itching on my legs and the bruising showing everywhere was the ultimate signal. I remember it was the day after my 24th birthday. I went to get my lab work done at Quest. They had it faxed to my doctor, and he said my counts are just completely off.
The white blood cell was 3 times the amount of a normal person, and my hemoglobin was 3 times below in the opposite. I think they don’t normally see the white cell go that high. That part was interesting.
I went to the emergency room that night. They gave me 2 bags of blood. They didn’t really know what was going on. I slept in the emergency room and then went up to a wing in the hospital to stay. They thought I had Lyme disease. They weren’t sure.
A couple of days later, I had a bone marrow biopsy. When the results came back, I got sent up to the hematology wing. Then I got transferred to another hospital to get treatment.

How I got through the “scanxiety”
When I was first diagnosed or when it was first happening, I thought this is minor because I never get sick. Like it’s not going to be a big deal.
When they mentioned Lyme disease, I thought maybe I got bit by a tick or whatnot. But when they did the bone marrow biopsy, I didn’t realize what even the test was for. My thought process is, “I just don’t know what’s going on, but I can’t imagine it’s bad.”
I still do remember him telling me I have leukemia. My mom was there. I didn’t even realize leukemia’s blood cancer. I didn’t know much about it, and it was hard.
The doctor actually treated my grandparents, too, but for a different form of cancer. It’s nice to have familiarity with him. Not that I was around that much, but he treated my loved ones as well.
I remember it as a little superficial. I thought I’m not going to have any hair. When I got moved from the normal wing to the hematology wing, it was just so much nicer.

I didn’t even realize then the impact of having cancer. I was told I had leukemia, but why is this also so much nicer? This probably isn’t a good thing. But my parents were there, and it was so nice to have them.
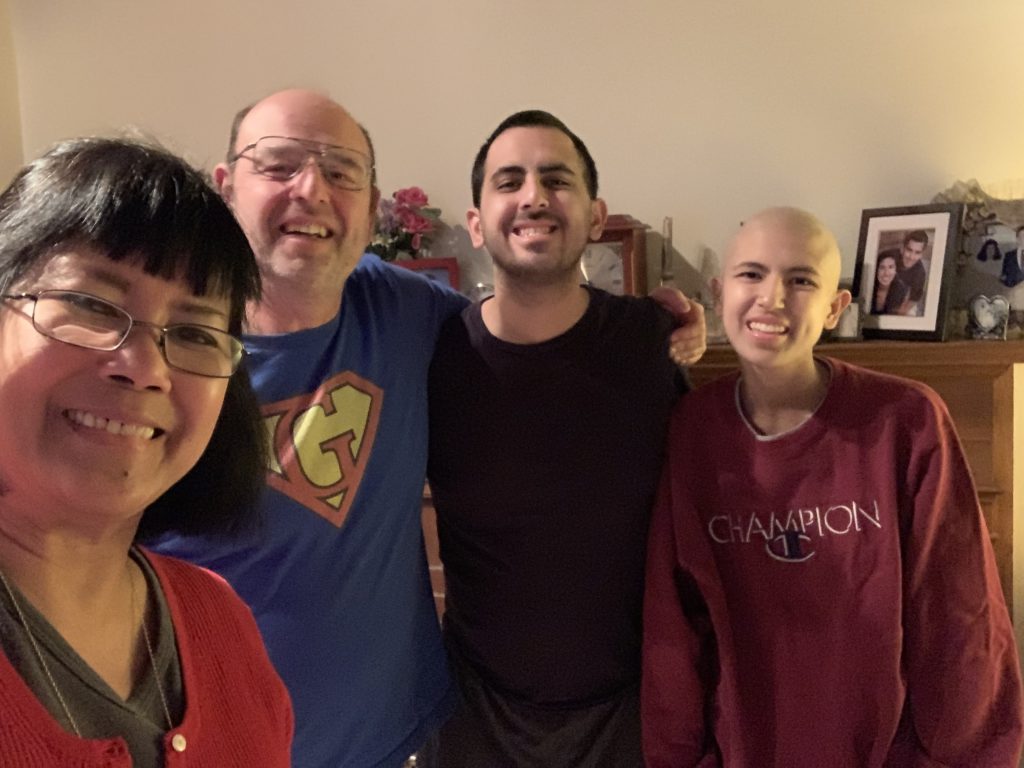
My mom wanted to sleep there, but I said no because she lives literally a half hour away. I don’t want her to sleep there. They came every day, which is super nice. My other family members came, too.
I also remember texting my friends. I think I was going to see them or something. I had doubts — should I tell them this?
A huge part of being sick for me is knowing the general reaction of people feeling bad, but I don’t want someone to feel bad for me.
I started to tell some of my friends, and they were super great about it.
When I was transferred to Yale to get better care, that’s when it became really hard. It’s far away from where I live, but my parents came to see me every day. Just the shock of it. I’m 24 years old, and I’ve never gotten sick. I can’t believe this is happening to me.
How my doctor broke the news
They were super supportive.
I remember there were residents or fellows around me, and then the doctor eased into it. She grabbed my hand and asked if I want to call my mom or anything. I said yes.
One of the residents around my age took my hand when I started crying and stayed with me. She was super sympathetic. We chatted about other subjects just to get my mind off things, too.
How can you tell someone something so hard? But his approach and having those people around me definitely made me feel comforted.
Recalling the moment of my diagnosis
I’m very much comfortable now with my diagnosis.
Thinking about it brings up the memories of what I had to go through or what I had to put my parents through. That’s the hardest part.

Back to telling new people, sometimes I have a tough time. That’s something I struggle with even today, just because I don’t want people to pity me.

Breaking the news to family and friends
Definitely in strides. It’s obviously a super heavy conversation to have.
My parents were the first ones to find out, and I had them tell my family. I was just so emotional even just to send the text that I was diagnosed. I only texted a handful of my friends. Others, I didn’t actually tell.
But they’d understand that I’m not responding back for days because I’m going through treatment, or I just can’t talk on the phone all the time because I was really tired.
I think taking it in strides and segmenting out my work friends, my family, and then having them tell each other so I don’t have to feel the need to tell everyone about my diagnosis.
Later on, as the weeks progressed, I felt more comfortable, and some came to visit me.
During the first week back, I texted my home friends who live around the area, and I told them it’s fine to tell everyone else. Some of them also came and visited me in the hospital.
It just made me happy. They were so supportive.
I do remember times when I would have 20 text messages on my phone. It almost felt like people feel the need to reach out to you even more, and it gets even more overwhelming.
It’s like a 2-sided stone. You have the benefits of feeling so much love, having everyone text me. But then again, I couldn’t respond at the moment.
I know they all care. It really does show you who really cares about you and who loves you. You are supported by a great family, set of friends, support system. It meant everything to me.

What is AML?
I didn’t even really know what type of cancer and leukemia. When they told me about it, they’re still doing tests.
There are different subtypes, different mutations. All that medical jargon, they went over and explained to me. They also talked about what could happen in the future. For example, fertility is a huge issue with chemo.
They talked about transplants, because not everyone who has AML gets a transplant. I also remembered them explaining maybe it was genetic for me.
I wanted more information, too. I thought it was extremely helpful just to understand.
None of my parents and grandparents have leukemia or blood cancer, but other cancers. The doctor described it as it’s almost like a car crash — you won’t know if it’s going to happen.
It was also helpful for your family to hear it right. I think one of the most emotional parts for me when I was getting diagnosed was seeing my dad get emotional wondering that very question: Was it because of the genes that my parents gave me?
Going Through AML Treatment
Video (Part 2)
Her life turned upside down, but Michele bravely faced AML treatments.
The IV chemo, stem cell transplant, and dozens of pills in her daily pillbox brought devastating side effects to Michele — physically, mentally and emotionally. However, she consistently and presently went through it all.
Michele tells us how AML treatment affected her.
What made you change hospitals?
It was the cryopreservation surgery. The hospital I got diagnosed with was a Catholic hospital, and they don’t do fertility preservation. I ended up going to Yale.
»MORE:Fertility preservation and cancer treatment
How did you decide which treatment to take?
As the thing about AML or any form of leukemia, as tests come up, the treatment differs.
What to expect next was definitely a question eating at me, because it was very uncertain.
The doctors would do rounds. During the first day I was hospitalized, I had 4 different people come in to greet me.
I got there at 7:00 p.m. I’d have 4 doctors in the next 2 hours, and then I went to bed. A lot of information was thrown at me, too.
That part, even though I do like knowing technicalities, was really a lot of information and definitely overwhelming.

I kept a notebook and would write everything down, any questions that I thought of during the day that I’d want to ask the doctor. My mom is in the medical field. Her boss, which is also a close family friend, would ask all the medical questions. It was a comfort for me to have that extra resource there.
I would ask even the nurses lots of questions. Since you see the same nurses, while you only see the doctor once a day unless something’s happening, it’s helpful to talk to them. The nurses were there for me the whole time, too, communication-wise — another line of support in general.
The hospital had a whiteboard. Since a big part of leukemia are blood counts, they would write my counts up there, too.
Definitely, there’s a lot of information and hard to organize, but having a nurse or being able to talk to someone you’re comfortable with — for me, it was my mom — helps.
That was like an affirmation that was I going through treatment.
What did you get for your chemo infusions?
I got a Hickman and a central line, as they would call it. I definitely had IVs in my arm before they put the line in. The hard part about this is I’m a tough stick, as they call it. You can probably still see a little bit of bruising or discoloration.
For treatment in general, it’s necessary to have it. They’re doing labs every day, almost round the clock, especially at first.
Until the Hickman is put in, you’re getting poked all the time, which takes up the veins as well.
That was probably one of the first procedures for major treatment event for me, aside from the bone marrow biopsy, which was a little scary, too.
Describe the bone marrow biopsy
I remember the first time because this was the scariest time especially.
At the hospital where I was originally diagnosed, they used something like a drill. That was the only time they ever used a drill. I remember the sound of it and my hands getting clammy. Honestly, it wasn’t that bad.
That time, I did have shooting pain down my leg, but all the other times no. Perhaps it’s the nervous reaction. Not from seeing the needle, but because the needle is huge, and they’re drilling a hole there.

The whole process is kind of nerve-wracking.
The residents were all there, too. I remember them being super supportive again, which made me feel nice.
Then when I got transferred to Yale, they had to do another bone marrow biopsy because it was a different hospital. It’s just been a week, and I had another one, so again, a nervous feeling. Now I’m very used to them.
I was trying so hard mentally to transport myself somewhere else. As it’s happening, I remember my then-fiancé asking me if I want a video or a photo. I said I don’t ever want to see what’s going on back there.
Describe your chemotherapy and side effects
For my first round of chemotherapy, it was 7+3 of cytarabine. It’s 7 days of 24-hour infusion. Then in the first 3 days, I have to take in another push drug.
Having a bag of chemo drugs carried around with me in the shower was just annoying. Then 2 weeks after that, they do another bone marrow.
That’s when they made the decision to do another round of chemo because it was greater than 5%.
I had 5+2 of the same drugs — 5 days, 24-hour infusion, and in the first 2 days are a push drug. Then they do another bone marrow maybe a week or 2 after the 5+2, and then it was under 5%. That whole time, I was down at Yale for 2 months.
It was definitely a long time. I didn’t get side effects until a week later because it just takes time for it to kick in.
The place was nice. They had a healing garden, which I loved to go to when I could manage. Some of my friends were able to take the train in, which is super nice of them. My parents came every day. I definitely had the support system while being down there.


I did make a friend, too. Most people with my diagnosis are white male, age 60+. Obviously, being biracial and being young and female doesn’t hit any of those categories. When I was down there about a month in, I met another girl who was just about 18. We would go on walks together. We’re going through the same treatment. She’s still a friend today
It was nice to go through something together and ask those kinds of questions that I didn’t know anyone else around my age asks. Like, why me?
It was a huge emotional impact on me, and having someone else around the same age group gave me a little more affirmation. It was nice to make a friend.
Tips on dealing with a long hospital stay
I would definitely go on to the wing itself. I would go on walks a lot. I’d do laps. I believe physical health does help mentally as well. The little walks help, too. It’s just nice to be outside and get some fresh air. They have little trees and a little waterfall in the garden.
Then I would wave if there are other people walking, or the nurses would talk to me.
I remember the royal wedding was happening when I was diagnosed, and one of my nurses said, “I’m only going to do this for a couple of minutes.” Then I said, “Stay and watch the royal wedding with me!” She stayed for a little.
I made really good friends with nurses. That definitely helps pass the time and helps emotionally as well.
I was in the hospital during COVID as well, so I did experience the difference between my first stay and second. There was a point when I was allowed no visitors at all. I would try to entertain myself, so I gained a lot of hobbies.
Before diagnosis, I knit a little, but after diagnosis, I knit a lot. I also watched lots of movies with great recommendations from friends. I still have a huge list today. I enjoy reading now, too. Puzzles were a huge one, too. Fun activities, too, just to keep my mind busy and have a little fun in it.
It’s really finding those little things that will make you happy.
»MORE: Mental and emotional support when leaving the hospital


What helped reduce the side effects?
Probably the worst ones were nausea. I can’t keep anything down. The chemo is just so intensive. There are medications that help alleviate it, like Zofran. The others are push drugs so that they react faster. But the nurses are great. You can just ring your call bell, and they’ll come.
Another worse side effect was feeling really tired. People are trying to visit, but I’m just so tired. My parents and friends would just then talk to each other.
Then the third one would be strength. The second time after my relapse and coming out of the hospital, I just couldn’t even walk. I was in bed all day.
I tried to be as active as possible, but my body mass decreased so much. I was not eating, and that’s a big one.
There are days when I’ve tried so hard to eat, but there are days I just couldn’t eat anything. I would try to take supplements. It’s crazy how little you can eat, and yet you’re throwing up. Even if you try to eat something, you just throw it up.
My parents would say, “Michele, just eat. Please, just another bite.”
All of that just weakened my body so much. Obviously, I love activities. I love running. I love being active. All that.
I can’t even walk. I needed a wheelchair, and it took a couple of weeks for me to even get up to walking up to the doctor’s office. It affected me mentally, too.
Throughout all my treatment, the hardest point was when I had MRSA a couple of times. Post-transplant, I had MRSA and C. diff.
I was home, and I just actually started working part-time.
I was just so excited to get to work, but after an hour, I couldn’t do anything. I went to bed.


I didn’t know what was wrong with me. Then I ended up calling the hospital a couple of days later, and I was at my lowest point in weight.
I lost a third of my body weight and was so weak.
Again, I needed to use a wheelchair up to the hospital. I spent another week in the hospital during that time. It’s nothing like I’ve ever seen.
What helped gain back some weight?
During my first transplant, the chemo was just so intensive. It took me almost a year to get back to regular eating.
I just couldn’t eat a lot of food, even a year post-transplant.
I eventually did see a dietician about it and talked about food. The Leukemia & Lymphoma Society has a lot of resources, and I talked to them. My work has a program called Consumer Medical, and they sent me cookbooks suggesting what’s good to eat when you’re experiencing certain symptoms.
In general, a transplant is wiping away your stem cells. You’re starting from scratch. The first 100 days are crucial.

I couldn’t eat fresh vegetables. I still haven’t eaten sushi. No raw meat. Because my immune system is just so weak, I can’t handle any bacteria that a normal person could. That also leaves me at a higher risk.
During the first 100 days, I can’t even leave the house. I had to be super sensitive and careful with food, but I did find the resources.
Currently, I do feel like my appetite has been good, relatively back to normal. I gained more weight, but obviously not up to what I was before. I think I’m in better shape now, and I’m comfortable with my body.
I did go through a lot of the ups and downs mentally being one way size and then losing that much weight.
I remember sitting on the chair. I was so bony it hurt to sit on a chair.
Even like a year or 2 after transplant, my thought process of my physical body is just so different from someone else’s because my body weight changed so drastically. It’s hard to describe that to someone, especially in a culture that’s so concerned with it.
There’s this stigma and perception of what a woman should look like.
For my situation, even if I only gained 5 pounds, that’s a lot. Having my body transform so much was a lot harder on me.
It was great to see the dietitian and reach out to other resources as well.
»MORE: Tips on food and drinks to help during chemotherapy
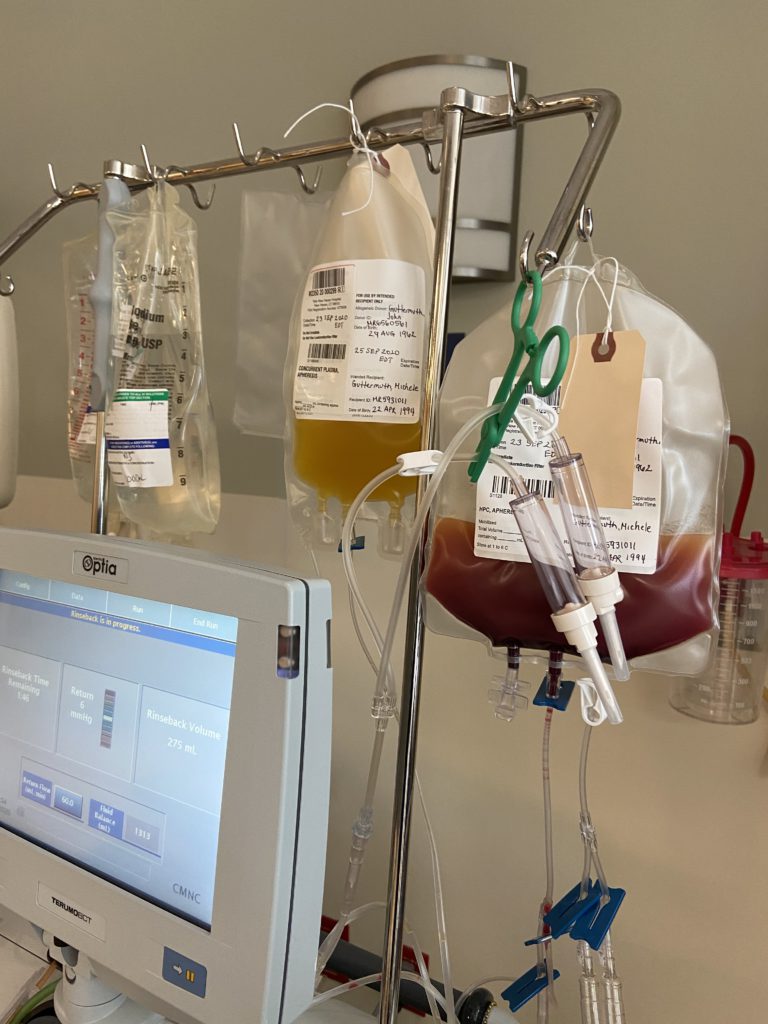
The 1st stem cell transplant
It was about 4 days of chemo. For me, they did tests beforehand.
There’s different variables with transplants. For me, being young, they did the most intensive chemo, and then a day of rest, a day or 2 of rest, and then the transplant.
Prior to this, my brother got swabbed. He actually ended up being a perfect match. He lived in Texas at the time, but my dad went out to visit him and discussed it. They took his stem cells out.
He had apheresis, and they froze his stem cells and then transported from Texas to Connecticut. The technology behind it is amazing.
My brother had that done in July 2018, but I didn’t get my transplant until September 7th. I was already in the hospital on August 30th, but they were waiting on my counts to recover and the most appropriate time for me to receive the transplant.
He came to visit, too, during my transplant. It was really nice to see him and have him there as well.
I was in the hospital for a month, so that’s probably approximate days of an average transplant. It does take a lot on the body, and my chemo is super intensive.

For a person who’s maybe 60, it could kill them. That’s how they make the chemo bag for your specific regimen. Chemo takes a little time, and that’s probably why I was in the hospital. I was just very sick again and started to lose a lot of weight. Same process. The first 100 days was just extremely tough on the body.
My immune system is so low. You’re almost like a newborn baby, and I had to get all my vaccinations again 1 year post-transplant. I was susceptible to all the diseases out there, and I was on 20 medications when I left.
I had a Hickman. They put in a PICC line, too — so much medication going through you.

The medications taken post-transplant
The major ones are TAC (tacrolimus) and CellCept, which are immunosuppressants.
When you get a new immune system, it has to acclimate with the rest of your body. In order for it to acclimate and not attack your organs, which is host-versus-graft disease, I have to take these meds so that doesn’t happen.
Prior to the transplant, I had Lupron injections for fertility and a lot of antiviral and antibiotics. During the transplant, I had a line of TAC going into me. After that, I had antiviral and antifungal medications. I was also on Zofran for vomiting.
My husband helped me keep track of them with Post-it notes to remind me. We bought those pillboxes, and I remember thinking, “Oh my gosh, I never thought I’d be young and using these pill boxes!”
One of the perks of the hospital is when you go to transplant, they have this kit for you, which included a pillbox. Mine’s big with 4 slots for each day because I’d have morning, noon, afternoon, and evening dosages and regimen.
They also had a calendar printout of all the medications. Post-transplant, they gave me all the medications, so I have them right away before I go home.
When you leave, a pharmacist will come and talk to you to explain everything. The pill chart was an explanation of what the drug is. You’ll have their number if you want to contact them, the doctor, or some stores.
I was still living with my parents at the time, so they were definitely a great resource to have. They would help me with medications, too, but I was very on top of things to get them done. I have my little chart that they gave me and then the pillbox. I would put the pills in all of them. It took a little organization as well.
A lot of meds, a lot of information. Feel free to ask the person you’re talking to if it’s okay to record them on your phone. It’s just nice to be able to reference something later, especially if you can’t write notes that fast. You can sort out the information after.
Describe the follow-up routine
After the transplant, the follow-up was 3 days a week. Then it went 2 days a week. I did have MRSA twice during that time period. I was hospitalized for a week, both times inpatient.
Then it went down to once a week and then twice a week. Then, in July of that year, I started going once a month.
By October 2018, I went slowly from 3 days a week to once a week, then to once every other week. By July, I started going once a month.
It’s still a lot. On day 30, I get another bone marrow biopsy. Day 100, another bone marrow biopsy. Day 180, another bone marrow biopsy. Then 1 year post-transplant, another bone marrow biopsy. Then I started getting vaccinations.
Managing anxiety before each bone marrow biopsy
It’s definitely nerve-wracking, but I also thought, “I got a stem cell transplant. There’s no way it’s going to come back.” I was trying to see the positive of it.
Just look at the good side of things rather than focusing on the negative, because the negative will give you anxiety. Some of the things I learned: A) be positive, and then B) keep your perspective.
Having those positive thoughts, even though you’re going through a scan, you’ll have a great support system as you’ve been through it. Just be positive.

You’re going through something so hard right now, but there is a light at the end of the tunnel. You will get through this.
Relapse and Treatment
Video (Part 3)
Learning that her acute myeloid leukemia had relapsed, Michele pressed on. She talks about her second stem cell transplant, round of chemo, radiation, and targeted chemo pill Xospata. Watch how Michele braved another shot at healing.
Symptoms of the relapse
Going through treatment, I became very in tune with my body, and I know when something is wrong.
I had a swollen lymph node on my neck. I couldn’t even see the jawline. Sometimes I get paranoid if I notice something different. I sought an appointment with my doctor, went to the hospital, and then they were keeping me longer than usual. I was so confused.
I remember sitting in a room while they did my labs, and I thought something was really wrong. I thought it was going to be a 30-minute appointment, but I ended up getting hospitalized. I called my parents immediately. They didn’t know what was wrong. They just saw that my counts were off.
I forgot exactly what they thought it was. I don’t know what kind of sickness they thought it was, but I was in the hospital for a couple of days. I remember it wasn’t my regular doctor who came up.
The doctor came up and said, “You’re going to get transferred to Yale.” I was like, “Wait, why?” He said I relapsed.

It hit hard emotionally, because I just didn’t think you could relapse after a transplant. I thought it was 99% effective. I don’t know where I was getting that statistic from, but I thought it was effective.
So it just hit hard.
I remember I didn’t even want to tell my friends, because I kept thinking, “This isn’t real. They didn’t do a bone marrow biopsy. How can they see it?” I guess [with] the lab work, they had scans where they could see it.
I know you’re not supposed to Google diagnoses, but that’s what I did. It gave me some affirmation for myself.
Processing news of the relapse
I didn’t believe it at all. I was in denial.

But then becoming more accustomed with it, I got sent back to Yale to my regular doctor to touch base and ask the tougher questions.
Obviously, I’m not the only one, but I learned about this genetic mutation that I had. That’s part of the reason why I relapsed. The other part is sometimes having a perfect match, but it can be too perfect.
I didn’t understand those concepts at first. Having those explained helped me understand more and cope with what was going on.
Having my supportive family and friends more accustomed to my condition, too, helped a lot.
The benefits of meditation
Meditation helped me emotionally censor myself. I had a spiritual connection with myself. It helped me reset for what is going on in my life and just keep it all out.
I did it in the hospital almost every day.

Describe your relapse treatment plan
It was more intensive chemo for the first round of my relapse. I was in the hospital for a month. Then I went home for a month and went back again to the hospital for a month for my transplant.
2 weeks before my transplant, I started the chemo pill and was on for a week. It’s also all of a sudden. They do the lab work, and then I’m ready for the transplant.
After the transplant, I was on pause for a little and just restarted a week or 2 ago.
Differences between 1st and 2nd stem cell transplant
The treatment plan for half matches are a little different. I had 4 days of chemo and then some radiation, not as intensive as if you’re having a tumor.
That part was definitely new for me, and you hear stuff about radiation. The regimen is a little different.
More transplant side effects
As for the side effects, I had the same symptoms I mentioned before. When I left the hospital, I was just so weak, and I couldn’t walk. The first time affected my stomach and appetite so much. I lost weight again, but not as much as the first time.
What was the radiation like?
I had full-body radiation because obviously blood flows throughout. For someone with a tumor, it would just be that area.
It sounds super scary, but pretty much all they did was measured my body, and then I went into this huge room. It looks like a dungeon, but it’s not scary at all.

I was just lying there while a light was shining on me. It’s really not that bad. Just the mental thought of it is so much worse than it actually is. It took about an hour, and then I flipped sides. There’s different grades, but I got the lighter dose, so it’s not as bad.
FDA Approval of Xospata (gilteritinib)
When I first was diagnosed, they were discussing that if I have FLT3, then we’ll have to go down this road. But the first time, I didn’t have it. Then after the transplant, in order for it to stay alive, it developed.
I was recovering from my transplant, and it takes a long time for the body to recover. They didn’t want to mix medications.
»MORE: Read more patient experiences with targeted therapy
Describe the Xospata and side effects
I was just tired, but I started work. I couldn’t tell if it was because of the transplant. I had 2 transplants, which obviously affected my body vastly. I was also tired from the pill, so they took a pause on it.
Now I just restarted again. I just upped the dose last week, but now I’m at a normal amount, and no crazy side effects yet.

They’re still doing my blood work. My creatinine was a little high, and that was the big concern.
I have an EKG once a week just to monitor the heart. I think a big part of it is the possibility of sending your heart racing, seizures, or possible fainting. There’s some nausea, but not as bad as when you were on the IV chemo.

Impact of taking a pill instead of getting an infusion
It’s better because it’s nice to be home, in your own bed, not getting woken up all the time.
Another huge part for me is with my parents having to travel to the hospital, which is so far away. Being home helps them manage their schedule and gives me peace of mind.
Being able to do it myself is so nice.
The research and technology with adaptations and how granular in detail they can get the medicine is just amazing and incredible.
Another big thing with MRSA is it’s 6 weeks of vancomycin through an IV. I was able to treat myself with an IV at home and not have to spend all the time going down to the hospital. They would send the medication straight to my house. I can fridge it, and I save a lot of time.
I noticed for my first and second treatment, they sent me a pole with a bag. With the second one, it’s almost like a ball I could keep it in my pocket. It was pressurized, and it makes it just so much easier for the patient.
Survivorship: Life After Diagnosis
Video (Part 4)
Her bright young mind couldn’t have comprehended her fate at first, but Michele chose to see the positive side of things.
With the love and support of family and friends, meditation, and enthusiasm to meet new friends, Michele now shares her story to give hope and inspiration to fellow young cancer patients.
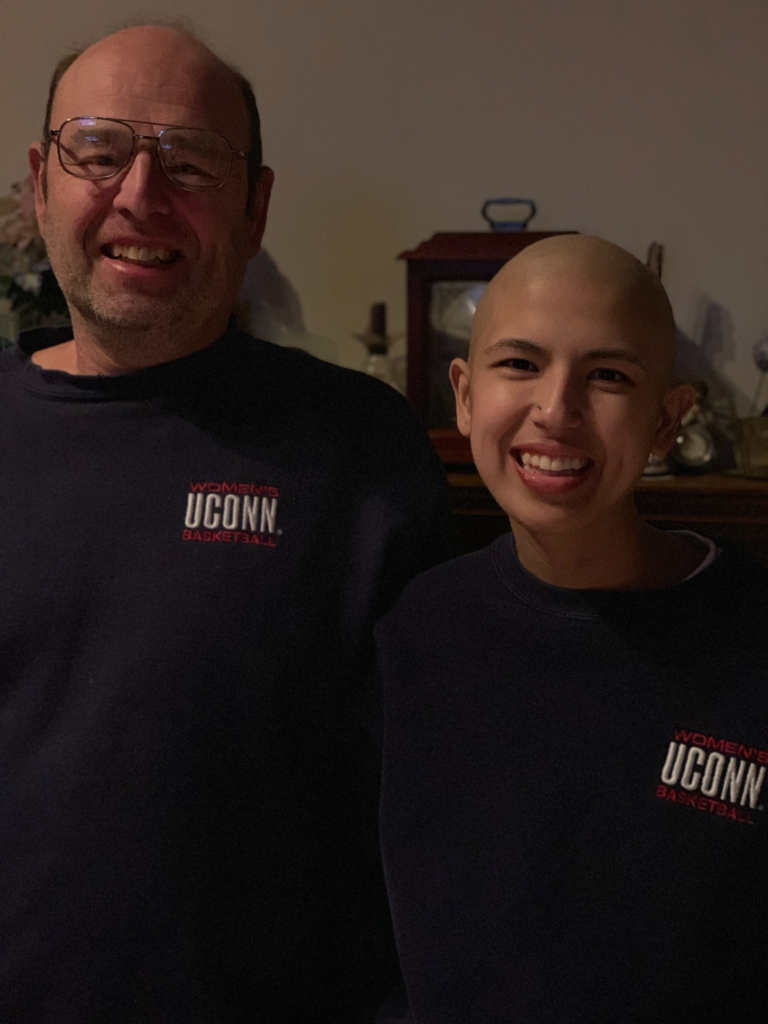
How to deal with the hair loss
I remember when I was diagnosed, I thought, “Oh my God, my hair!” That was one of my first reactions.
I used to have hair down to my shoulder, and I imagined I was going to lose it.
When it started falling out, it was so annoying. It was everywhere. I thought I should just shave it, so a lady came up when I was impatient and shaved my head.
The big part about it was emotionally. I thought I’m going to look like a cancer patient, and that part of it was hard to grasp. Obviously that comes with you, going through so much and then getting sick.

It does take an emotional and mental impact, because you do want to feel beautiful. Having that support system is just so key in helping with that. I also did look into wigs and had fun with it.

There is a little section at the hospital where I got to try on all the wigs and work with a hairdresser. I learned about the upkeep and everything. I wore that a lot through my first treatment.
Also, when people came to visit me, I’d just go bald or wear a hat. I’m very into hats, and I have a collection now. My aunt actually gave me another wig. When I relapsed, I got another wig.
New day, new hair.
It was bizarre. I didn’t wear any makeup because I didn’t want it to react with my skin. But as time goes on, you understand it more emotionally, and it’s fine. No one cares at all.
»MORE: Patients describe dealing with hair loss during cancer treatment
Deciding whether to stop or continue working
At first diagnosis and the transplant, I was at home for 100 days and not socializing.
The world was normal then. I really just want to get back to work without overpushing myself.
I went back to work part-time in January. My employer was great. They let me ease into it. I ended up having to go back to the hospital inpatient for a week, then took some more time, and then eventually was able to start full-time. They eased me into it, which is super nice.
»MORE: Patients talk about working during cancer treatment
The second time post-relapse — and also from having 2 transplants — I kind of steadied myself. I took a little longer before returning.
October 30th, 2020, was my transplant. Then I came back in April and then did a month part-time and then full-time.
The first time is so nice because you’re getting back to normal. But the second time took a while, also because of COVID. I couldn’t leave the house until I got vaccinated.
I was at home anyways, so I didn’t feel the rush to go back to normalcy.
I just wanted to feel normal.


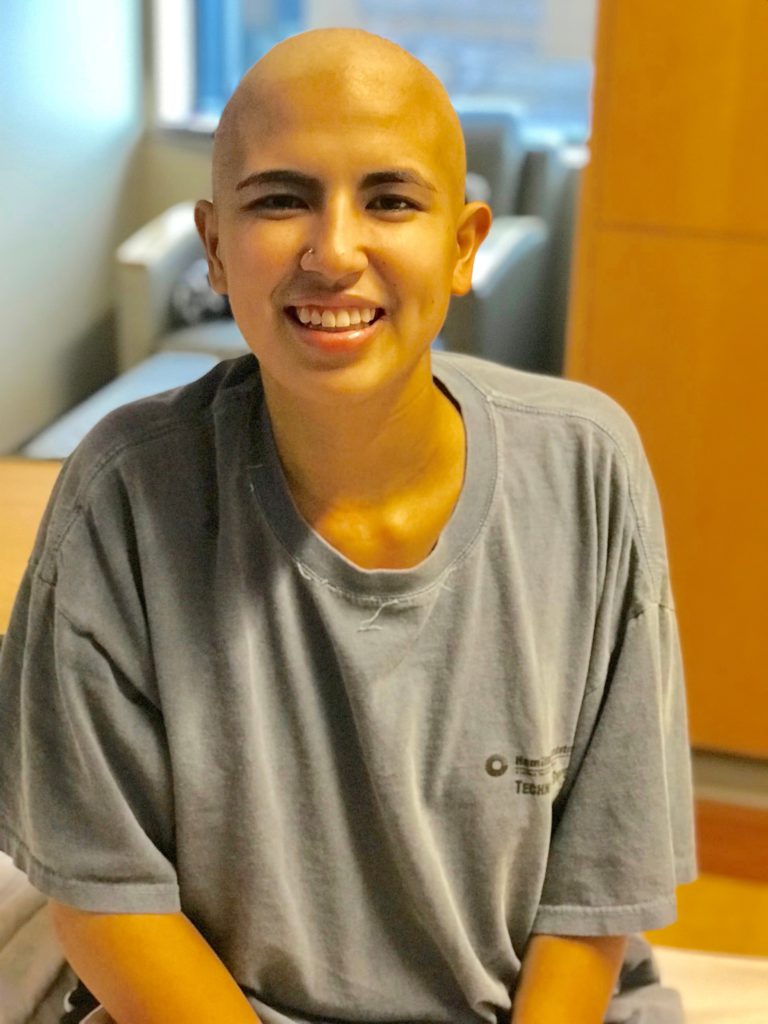
The experience of being a young cancer patient
Being young was probably one of the hardest points for me emotionally when I first was diagnosed. I thought it was just older people who get cancer. That’s naive and not true at all.
But I’m healthy. I’m young. I just don’t understand.
It was just a lack of understanding. I felt blindsided by the diagnosis, so I just wanted to find someone else I could relate to.
Meeting someone else in the hospital around my age was extremely nice. Having the same questions, the same diagnosis, and being both young was just comforting in general.
The Leukemia and Lymphoma Society has a Connection Program, where I can touch base with other people who are around my age group. I recently joined, and I’m excited to know more people around my age.
I wish I knew it during the time when I was going through treatment, but I’m glad to know it now. Just to give you that extra comfort.
The importance of fertility preservation
It came to me as a shock — realizing its impact on my fertility.
It was something they addressed right away. I switched hospitals to do it. It was too late to do preserving eggs, so the next-best option was preserving my tissues, which will produce the eggs.
The process of cryopreservation
The fertility doctors all came in to talk to me about it. It was nice to hear their knowledge of the concept and have the appointments. I came in for it after my first 2 rounds of chemo.
That’s my first time in anesthesia, but they knocked me out and then just grabbed some of my tissue.
I remember when I was getting wheeled into the surgery room, one of the anesthesiologists told me about her dad just having some type of leukemia, and he just found a donor. It takes 2 years if you got a random donor in the registry. She’s finding out who his donor is, and it gave me a positive light on that aspect.
The surgery part and just having that whole concept of fertility issues is definitely difficult to grasp, but understanding that there are other options out there is reassuring.
»MORE: Fertility preservation and cancer treatment
Perspectives learned from living with cancer
I definitely think it taught me a lot about perspective and understanding.
It’s a lot, especially at this age. I’m about to live on my own, get married, build my life. It was a very difficult time. There are still hardships. A good thing to have such a great support system. I’m truly loved.
I learned so much from it about myself, like how strong I am. My emotional understanding was enhanced, and I understood what my body needs physically and mentally. You learn a lot about yourself.


Give time. I’m a big advocate of meditation because it was something that did huge for me.
We all go about our busy schedules, but taking that time, having that perspective, not thinking about anything, and just relaxing makes you realize what is important in life. You are able to see the positivity.
It changes your mind and changes your understanding.
I think that as terrible as it was to go through, it changed my outlook on life. I realized how important each day is and how much love there is for each other.
You never know what someone else is going through, and having that understanding and empathy makes our society so much better.
The importance of self-advocacy
That’s a huge part.
My family’s in the medical field, so they obviously have an understanding, but their body isn’t going through it. They don’t understand what I went through exactly or when I know something is wrong.
I knew the second time around, I have it back and need to get an ultrasound. I was the one who suggested I need an ultrasound to my doctor. Advocating for yourself is extremely important.
You know what your body wants. All the medication that you’re taking interacts differently. The doctors have a certain regimen, a standard of treatment, but your body is different from someone else’s, and it will react differently. You know when you need certain medications or need extra help.
No question is too dumb to ask. When you need something, don’t be afraid to speak up.
»MORE: How to be a self-advocate as a patient

Why I share my patient story
When I was going through it, I would have loved to see someone’s vulnerability — that openness that I’m going through something, that someone else does, too, that relatable empathy that you have.
It just brings peace of mind to me, and I hope to bring that to someone else.
It’s something I sought out for and wish I had a little more. I feel like it’s only my due diligence or duty to help others who are going through the same experience.
It has so much impact on me emotionally, mentally, and physically to have someone else going through the experience. It helps me cope with what’s going on.
I want to share my experience as much as possible. Regardless of the diagnosis, cancer affects everyone. You probably have a family member, yourself, or anyone that has gone through this experience. It is terrible, but you learn the love, and you relate to people.

Inspired by Michele's story?
Share your story, too!
Acute Myeloid Leukemia Stories
Shelley G., Acute Myeloid Leukemia (AML) with NPM1 Mutation
Symptoms: Fatigue, rapid heartbeat, shortness of breath, low blood counts
Treatments: Chemotherapy, clinical trial, stem cell transplant
Joseph A., Acute Myeloid Leukemia (AML)
Symptoms: Suspicious leg fatigue while cycling, chest pains due to blood clot in lung
Treatments: Chemotherapy, clinical trial (targeted therapy, menin inhibitor), stem cell transplant
Mackenzie P., Acute Myeloid Leukemia (AML)
Symptoms: Shortness of breath, passing out, getting sick easily, bleeding and bruising quickly
Treatments: Chemotherapy (induction and maintenance chemotherapy), stem cell transplant, clinical trials
Grace M., Acute Myeloid Leukemia (AML)
Symptom: Headache that persisted for 1 week
Treatments: Chemotherapy, stem cell transplant