Mary Clare’s Relapsed Acute Myeloid Leukemia Story
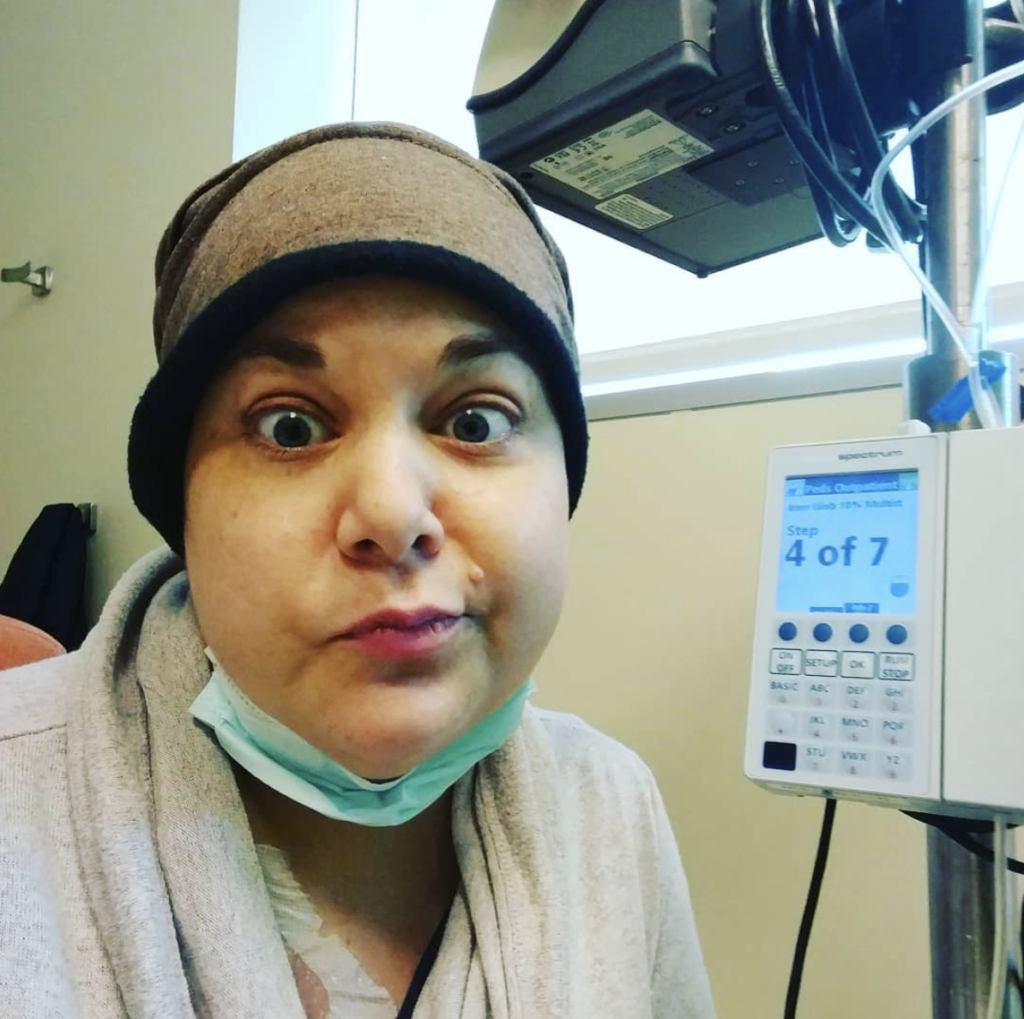
Mary Clare was diagnosed with acute myeloid leukemia (AML), the most common type of acute leukemia, at just 36 years old.
In her story, Mary Clare shares how she got through chemo, 2 bone marrow transplants, full body radiation, a clinical trial, and recovery. She also highlights the mental, emotional, and sexual impacts of cancer.

- Name: Mary Clare B.
- Diagnosis:
- Acute myeloid leukemia (AML)
- Age at Diagnosis: 36
- 1st Symptoms:
- Fatigue
- Headaches
- Upset stomach
- 1st Treatment:
- Induction chemotherapy
- Consolidation chemotherapy
- Bone marrow transplant
- 2nd Treatment:
- Azacitidine
- Venetoclax
- Chemotherapy
- Full body radiation (total marrow irradiation, or TMI)
- Bone marrow/stem cell transplant
I don’t think I’ve moved on. I think that I’ve learned how to manage the uncertainty. The side effects. The future.
Not knowing if things will come back and also just acknowledging that the support system that you think you had isn’t always there, your world gets pretty darn small sometimes.
But there’s a lot of beauty in that.
Mary Clare B.

- Symptoms & Seeking Answers
- How did you know something was wrong?
- What happened at urgent care?
- How long did it take to get the blood test results?
- When did you hear back from the doctor?
- How did you process the sudden news?
- How did you decide where to go for medical advice and treatment?
- Describe the first procedures at the hospital
- What were the first steps once you were in the hospital?
- Bone Marrow Biopsy & Diagnosis
- Induction Chemotherapy
- What were the treatment options?
- What was your chemotherapy treatment regimen?
- You had 3 days of chemo but stayed in the hospital for 6 weeks
- Describe your PICC line
- What were your chemo infusions like?
- Describe more of the chemo side effects and what helped with them
- What helped you calm down the chemo side effects?
- Describe the routine while you were inpatient after the chemo infusions
- White blood cell count recovery took longer for you
- What was next after 6 weeks in the hospital?
- How did your body react to the first chemo?
- Bone Marrow Match & Transplant
- Describe the bone marrow matching process
- What's “consolidation chemo”?
- Describe the consolidation chemotherapy regimen and side effects
- How many bone marrow transplant matches did you end up having?
- What was the transplant process?
- What was it like after the bone marrow transplant?
- How did your body react to the bone marrow transplant?
- Transplant Recovery
- How was the transplant overall?
- You had to advocate for yourself to go home from the hospital
- What should people know about that high-risk recovery period after the bone marrow transplant?
- Were you able to have any visitors outside of your husband, daughter, and mom?
- Where there any other steps you took to help protect yourself and weaker immune system?
- Any other tips on how to best isolate at home?
- You developed chronic graft-versus-host disease (GVHD)
- How did you determine it was graft-versus-host disease (GVHD)?
- What helped with the GVHD?
- Clinical Trial
- Resuming Life
- Relapse
- When did you find out the cancer was back?
- There was a very low level of disease
- How did they treat the relapse?
- How did your body respond to the azacitidine?
- What adjustments did you have to make at home and at work?
- How long were you on azacitidine overall?
- Describe the clinical trial for venetoclax
- How did your body respond to the venetoclax trial?
- How did you get off the drug?
- 2nd Bone Marrow Transplant
- Describe the preparation before your 2nd transplant
- They added radiation to the regimen
- Describe the radiation process
- How many times did you have to undergo radiation?
- Were there any side effects of the radiation?
- How soon after the radiation did you undergo the bone marrow transplant?
- What were the side effects of this second round of transplant and chemo?
- 2nd Recovery
- Mental, Emotional, and Sexual Impacts of Cancer
- How did you manage the flux of messages and visits from supporters?
- Any advice for people on what can help maintain energy while communicating with supporters?
- How did you deal with the mental struggles?
- How do you keep perspective?
- How did your cancer experience impact your personal relationships?
- Speaking of personal relationships, what were the sexual health impacts?
- What has helped uplift you most?
- How have you been able to move forward with life?
- Any guidance for people on how to handle life after cancer treatment?
- What’s your overarching message to those reading your story today?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms & Seeking Answers
How did you know something was wrong?
I was running programs for a college with lots and lots of high school students, who were coming to the college that summer to be part of arts programs. It was a hectic, crazy job. I had 350 students I was working with from all over the world. I was exhausted.
Normally, I respond to situations like that with all adrenaline all the time and then crash the week after the program is over. But I had felt poorly. Everything upset my stomach, and I was very fatigued and tired.

I knew something was up, and I thought it’s a cold [or] it’s allergies. I had gone to the medical practice on campus, and they said, “Oh, you just have a cold. Here’s some Flonase.” I didn’t think anything of that.
A couple weeks later, the program ended. I felt pretty crappy, and I started to have really bad headaches. I’m a migraine sufferer from my early 20s.
But it was nothing like migraines. It was these headaches that would wrap around the back of my head. Just the worst headache of my life, so I ended up going to the urgent care at the University of Chicago, which I had previously gone to.
What happened at urgent care?
As soon as I came in and talked about my symptoms, they were very concerned. First they wanted to do a spinal tap. That scared me, of course. [I was] thinking, “Oh, I just need better migraine medication or something.”
I knew something was wrong, but I had no idea that a blood test later that day would lead to me being admitted to the hospital that same night.
How long did it take to get the blood test results?
The urgent care is an offshoot of the main hospital of University of Chicago, so they have labs that are ready. I was able to go from my urgent care appointment across the hallway, get a blood sample taken, and then I came home.
I live about 10 minutes away, and they called maybe an hour later saying, “Something’s not right. We’re thinking about having you come back to do the blood again. But just keep your phone by your side. I’ll call you back.”
When did you hear back from the doctor?
Actually, that evening we were packing to go on a trip. [It] was going to be my first trip with just my husband and I. My daughter was little. I was making dinner and packing, and the phone rang again as we had sat down for dinner.
It was the doctor that I had seen at urgent care, a young doctor saying:
This is very serious. You need to come into the emergency room right now and pack a bag. You’re going to be staying here for more tests and more observation.
How did you process the sudden news?
We don’t have family nearby, so our first thought was, “How are we going to do this with my daughter?” [She] was 3 at the time. “How do we do this with a 3-year-old in tow?”
We just go to crisis mode. For us, the feelings don’t come till a little bit later. What are the practicalities of this? I think parenthood comes with that.
My daughter’s good friend lives 3 doors down, so we called them. They didn’t answer the phone, so we just packed a bag for Twila (daughter) and walked over there, trying to say, “Mom is not feeling well. We need to find out what’s going on.”
She immediately was like, “It’s my first sleepover! This is amazing.” She was just excited.

It was very odd. You’re putting on a face for your child.
My husband took her to the neighbors’ place and knocked on their door. They didn’t answer the phone because they’re in the middle of story time for their girls, but they welcomed her with open arms and said, “Whatever you need.”
It really made us be able to take our parent hats off and be able to absorb some of the situation. It felt really hollow. It felt like dread. It felt like something I’ve never felt before.
»MORE: Parents describe how they handled cancer with their kids
How did you decide where to go for medical advice and treatment?
My husband works for the University of Chicago, and my daughter went at the time to the laboratory schools, which is associated with the university. We would very much call ourselves a university family.
The majority of our friends work for the medical center or our academics, so we’re kind of in that world already. It’s just down the street. My husband walks to work, and I previously have worked there.
It felt like we weren’t going anywhere new or different; this is our neighborhood. It’s just a block from my husband’s office and a couple blocks from my daughter’s school.
It was a bit surreal in that regard, because it was just like we’re driving past our grocery store. I know where to park and all. Just very strange knowing that we were going there not knowing what that next piece would be.
We were totally clueless that I would be in the hospital for the next 6 weeks [and] that we would be dealing with this many years later as well.
We were pretty darn clueless, and we were hopeful, scared. I’m probably making really stupid jokes because that’s kind of how we deal with things.
Describe the first procedures at the hospital
What was surreal is that we had an appointment at the ER, which is not something you do. They knew we were coming. It almost felt like going to like a restaurant and saying, “Here’s my reservation. I have a reservation.” They had a room ready for us.
It didn’t take very long until 3 doctors, at least 2 of them oncologists, came in the room. They laid it out that based on my blood sample that they had taken earlier that day, my white count was really strange.
The rest of my blood results were out of whack. Their best understanding at that time was that I had leukemia of some kind, some sort of a blood disorder.
They did use the word “cancer” but said that they needed way more information. What they did know is that things move very, very rapidly with blood cancers and blood disorders. To be able to provide me the best care, I needed to check in to the hematology-oncology floor at the new hospital just a couple steps away.
It was a Friday night, so we actually had a weekend in the hospital where they checked in a little bit, but I didn’t really see the person who would become my team.
The 6 people that would come and really talk to me did it Monday, so it was very odd. I was like, “This seems so financially crazy to have me stay here for 2 days and just kind of check in on me, where I felt fine.” I didn’t feel awful. I felt a little sick but not terrible.
What were the first steps once you were in the hospital?
Monday, they hit the ground running at like 7 a.m. It was meeting with teams and learning what the plan of care would be.
Are we going to start immediately with chemo? We would do a bone marrow biopsy to get more information. All of those things went into place.
It was a head-spinning day, but we had that weekend to be able to kind of rally our team and support and to do some research on our own. We had actually [gone] into meeting with the oncology team pretty informed.
A good friend is an oncology pharmacist. She deals a lot with transplant patients, so we were pretty well informed.
Bone Marrow Biopsy & Diagnosis
Describe the bone marrow biopsy
I’ve probably had about 20 bone marrow biopsies at this point. The first one, I had no idea what I was in for.
They basically explained it to me, “We’re just going to take this tiny little sliver of your hip. It’s a very quick procedure. It’s done at the bedside. We don’t have to put you under or anything like that; we will numb the area.”
In my mind, I had thought of like when I had a mole removed or something like that in dermatology, that it would be something akin to that, but a little bit more. I think in a lot of ways, my doctors and my team have tried to not totally scare patients.
Not all details are shared before certain procedures. This particular one, [they said] you’re going to feel a pinch in a burn, there might be pressure, things like that.
What I realized pretty quickly is that it’s sort of like getting a root canal on your butt. That’s the best way that I could put it, because they do a little bit of work [and] have a bit of a drill.
I was pretty well drugged. Over the years of doing this, I now know my favorite cocktail of drugs to have before before a biopsy.
Was family in the room?
My husband was sitting there, also having no idea what was going to happen. My mom had flown in from Virginia, and so she was on the little patient couch at the end of my bed.
You’ve had about 20 bone marrow biopsies. What’s your advice on how to deal with them?
I think anyone who’s going undergoing a procedure where you’re either getting your port in or a PICC line — a bone marrow biopsy, in particular, it’s good to know how your body reacts to different medicines.
For example, if they give me Dilaudid, which is a very typical drug to be given that causes you to be mentally out of it, that for me was successful as far as no pain, but I would be vomiting for hours after.
I would feel way out of it and would just have to sleep for the rest of the day. I realized that was not the right drug for me, and I had to ask for something else.
I ended up with what they think is a lighter alternative, which is a heavier dose of Ativan mixed with Benadryl. I’m not mentally engaged with the pain. Certainly, I can feel things, but with Ativan you have a very limited memory from that experience. It does incur some memory loss, which in this particular case is great. I was totally down and okay with that.
Also, in previous outpatient settings, after using just the Ativan, I could sleep for a little bit. After the procedure on the table, maybe an hour after that. Then I’m a little out of it. I certainly can’t drive myself home.
I’m able to walk the block or 2 to the parking garage, have another cup of coffee at home, and restart my day. It doesn’t derail everything. It took a while to figure that out.
It also took a while to figure out that there were some members of the team that were seasoned and more experienced in doing difficult bone marrow biopsies.
I’ve learned that I’m one of those people that it is tricky. Some people have more forgiving bones, and I don’t. I learned the same thing goes with blood draws.
I’m a really tough stick, and so you need someone who has the combination of skill and confidence. If they don’t — if they have the skill but they don’t have the confidence, it’s not going to happen. Likewise, if you have the confidence but not the skill. Those are some things that I’ve learned over the years.
How long did it take to get the bone marrow biopsy results?
For the bone marrow biopsy, we received some news the next day. They had everything you would need on site at this particular hospital because it is a research institution, so they were able to get some of that staining back quickly.
They were able to get a deeper understanding of how many blast cells, but with the type of work that they’re doing, they also do a couple different other stains that take more time to develop. Then I would receive more information later in the week, if not the following.
That’s when they were able to tell me pretty much this is AML leukemia, based on what the cells looked like. They were able to tell me my percentage of blast cells, which really didn’t mean much to me at the time, but that it was aggressive.
There’s no stages for leukemia. There’s no Stage 1 and Stage 4. There’s nothing like that. It’s percentage of disease.
It’s not a cancer that is often found very low levels. It is in the 20+ percentage of these abnormal white cells that are overcrowding and hacking your body.
For me, learning that it was like 20 or 30% didn’t mean a lot. But knowing that you’re not supposed to have any, that it’s considerable, meant that they needed to move and act quickly. Once the body starts replicating the cells, it’s just going to continue and continue until it destroys your body.
How did you tell your daughter about your cancer diagnosis?
When I was first diagnosed, my daughter was 3 and was pretty clueless beyond, “Mom is sick.” She’s a smart young lady. She is inquisitive to the nth degree, so there was no keeping things from her.
I brought her to doctor’s appointments. When she was able to visit the hospital, we brought her. We didn’t shield her from much. We didn’t go into big, long details if something was going on. But if something was happening with my heart, I told her.
We had many medical supplies at home. My lines had to be cleaned. Infusions at home happened at some point, and she learned how to do all that stuff when she was 3 and 4. She’s probably a future doctor.
Over time, when I’ve had major mobility issues and issues with syncope and things like that, she is a caregiver. Her capacity to take care of other people is well beyond her years, and well beyond what anyone would expect from a child.

It breaks my heart to think that I’ve taken part of her childhood and innocence away from her.
But I don’t think we could have survived any other way.
She has very close relationships now with my mom, her grandma, and my husband’s mother (her other grandma) that would have never ever happened if cancer didn’t come into our world.
»MORE: Parents describe how they handled cancer with their kids
Did you consider a second opinion?
Luckily, I was at the University of Chicago. They have an adolescent and young adult clinic for blood disorders and specifically leukemia, so I was able to be with the foremost experts, not even knowing it.
I was starting to talk to people in my research and my husband’s research like, ‘I have the option of having one of the top experts, Dr. Wendy Stock, as my oncologist.’
It was an interesting process because she wasn’t rounding when I first came in, but she learned about my case through the weekly transplant meeting.
She came to my bedside and asked if she could be my main oncologist, which was just so cool. It was very patient-facing and very warm to have someone say, “Can I be your oncologist? Here’s my credentials, and this is why I’m interested in you.”
Induction Chemotherapy
What were the treatment options?
They had already presented some clinical trial options, mainly just different dosages of different chemo agents that they thought might be better for me, because I was in my 30s.
Typically people who get leukemia, if you look at the percentages, high amounts would be infants and very, very young children, as well as older adults over 70.
There’s a very, very small group of young adults, who would be classified between 18 and 40, that would develop this disease. It’s not unheard of, but it’s pretty rare.
What was your chemotherapy treatment regimen?
First off, it’s called induction chemotherapy. I believe it’s a 3-1. There are 3 days with a certain cocktail of drugs. I was only given very, very high doses of chemo over 2 weeks.
You had 3 days of chemo but stayed in the hospital for 6 weeks
The reason I was in the hospital for 6 weeks is because you cannot leave until your blood counts are at a level where if someone coughed in your vicinity, you wouldn’t get that. It would become pneumonia.
You need your immune system to be functional in the smallest amount possible. When you’re given this very, very heavy, high-dose chemo, it just destroys your immune system, as well as destroying the cancer.
That’s a major side effect, and they don’t want to release you back into the world, even if that is isolation in your home, until you’ve reached a certain standard with your blood counts. It took a while for mine to go back.
Describe your PICC line
I had a PICC line installed in my arm, which was a bedside procedure. [It was] somewhat uncomfortable, but not terribly.
I’ve had 2 PICC lines. That’s basically a line that goes directly into your heart from your arm. That would be a way for them to easily give you medications and drugs without having to start an IV each time.
It’s semi-permanent. You don’t have PICC lines for terribly long; 6 months is typical. I was hooked up with that.
What were your chemo infusions like?
Once a day, I would be given a drip bag of those chemo agents. That was typically a couple different bags hanging from an IV pole. The first couple days of that regimen, I was able to watch TV and be up and about.
They said walking the floor was okay, but I was not allowed to leave the hematology-oncology floor, go to the food court in the building, or anything like that. I was wearing my normal clothes. I was able to take a shower. I was able to do kind of my normal things the first few days.
After that, the side effects of chemo, where it really is starting to ravage your body, kind of took over. My blood counts dropped; red, plasma, and all those things were problematic. I started to be on that IV pole a lot because I was receiving platelets, red blood product, and I was receiving fluids as well.
As the weeks went on, they added potassium and magnesium because your body is really being depleted of a lot of the essential things that it needs to run.
Describe more of the chemo side effects and what helped with them
Main chemo side effects from the first induction round were really poor appetite, things started to not taste right, and just overall fatigue. Upset stomach was another thing, sometimes diarrhea, sometimes constipation back and forth with that.
Not only was I starting to feel poorly around the third day. No appetite. I did get a rash, which they think was from the red blood product. That happened once and never again. I was very uncomfortable.
I think initially it was the huge rash, head to toe, just itchy, and felt yucky. As soon as I presented with that, they had dermatology come and check me out.
When you do have a rash on the outside of your body, there’s something going on inside as well. You want to make sure that that can be looked at and dealt with quickly.
We realized at that point that you can get calamine lotion in a spray form. It was super helpful to have my mom, my husband, and some close friends who could run to CVS or the drugstore to be able to pick up little things you need.
I also packed a bag for one night. I had no clue that I would be needing my family to make sure I had clean socks and underwear and that I had the comfy kind of pajama-type clothes. That was really helpful. That first week or so, it was kind of like, ‘Well, what do you need?’ Setting myself up to be pretty self-sufficient.
What helped you calm down the chemo side effects?
Most everything was well controlled with medication. I was given any opportunity I wanted to be able to take anti-nausea medication, which was helpful.
I needed to figure out which ones again would be good as far as still letting me be somewhat conscious, because many of them will just knock you out and make you very, very tired.
You can sleep through all of this if you want to, but realizing that I was going to be there for a few weeks, I wanted to do something. I want to actually spend my time a little bit better, especially since family had flown in to be with me.
Figuring out ginger ale was very helpful. Ginger candies were helpful for an upset stomach. The main thing that has helped me over time has been heating pads.
In the hospital, a nurse can give you a little packet that they shake together and pop. It’s a nice hot, a little kind of a pillow that you can put on whatever is hurting you. That for me, especially while you’re waiting for other medications to kick in, is a lifesaver. It can also be very soothing if you’re trying to get to sleep.
Those were always things that I noticed. The nurse came and did her rounds. First thing in the morning, she’d load me up. She’d say, “Here you go, here’s 3. You’ll be good for the day.’
When I’m home, I use my heating pad that plugs into the wall. Those things were helpful.
I think still being active. Trying to get out of the room to walk around was helpful for digestion, for appetite, and for overall fatigue.
The fatigue is going to hit you. You’re going to take a nap, you’re going to go to bed early, you’re going to feel like watching a movie or TV or doing something quiet, and you’re probably not going to want to entertain a lot of guests.
Luckily, maybe once a day I would have some folks come over for maybe an hour, but the rest of the time I spent mainly alone.
Describe the routine while you were inpatient after the chemo infusions
I was just stuck at the hospital. I’m stuck in my same room. It became a typical routine that I would be woken up at 6 a.m., and they would do a blood draw, weigh me, and take my temperature, my blood pressure, and all that good stuff.
I could snooze a little bit after that. It may have even been like 4 in the morning. I’m not sure. It was crazy early. Depending upon the day of the week or the weekend, I may not see a doctor at all, but during the week, I would then see a doctor sometime between 9 a.m. and 1 p.m.
It was very vague when that team would be rotating through doing rounds. They would say, ‘Here’s your blood counts. Here’s what’s going on. Specifically, looking at the panels, you need potassium today or you need this today.’
Then asking me, “What are you feeling? What do you need as far as mitigating side effects and symptoms?” That just became the routine.
I watched the first 2 seasons of “Scandal” and talked to a lot of the nurses and the nurse assistants about all of that!
White blood cell count recovery took longer for you
After 2 weeks of chemo, I was still in the hospital for 4 more weeks because we were waiting for my blood counts to recover. It was unbelievably boring and stressful because I was a bit of an outlier.
Typically it takes a week or 2 for counts to come back, but my body really fought against that. I was not a candidate at that particular time, [because of ] the regimen that I was on, for something like Neulasta that would enable that to happen. It would cause more cancer cells to grow at that juncture, so I was just kind of stuck there.
What was next after 6 weeks in the hospital?
I was able to go home, be with my family, and rest my body a little bit. I was still going into the outpatient clinic at least once a week, sometimes more, depending upon side effects and symptoms. [I was] getting an understanding of what’s going on with my body.
How did your body react to the first chemo?
They realized after those 2 weeks that [my body] was responding to chemo and could put me in a temporary remission.
Bone Marrow Match & Transplant
Describe the bone marrow matching process
They began the process through the bone marrow biopsy and a million and one blood samples to find out what my biomarkers are, [as well as] what’s unique and special about my genome and my specific cancer to provide personalized care.
They would also look to see all the different special things about my bone marrow to be able to find a match in the registry. I don’t have any siblings, so I didn’t have any family to go to for that. It’s a very long and arduous process to find a match.
A good match takes a month sometimes, so they begin that process very early to see if that was going to be a possibility for me.
In a perfect world, if you had a donor lined up, you would have heavy-duty chemo and then immediately have a transplant.
That’s not how the world works. It takes a lot of time to get your donor in place, to make sure that you have a good match, and that all the legality is put together.

What’s “consolidation chemo”?
The initial chemo is to really test your body to see if you can get into remission. During that process, you’re waiting for that donor and that time to be set up for your insurance to approve everything.
Your body will start to probably make cancer cells again, and most patients that I’ve spoken with and that I know have all had something called consolidation chemo.
You may even have multiple rounds of consolidation chemo, and that is another couple days-stint of heavy-duty chemo agents that will keep your cancer down and your white cells at a more normal level.
It’s not as intense as induction, but it’s still a heavy-duty dose. For me, I went inpatient. By that point, my body was like, “Oh, okay, so I’m supposed to suppress everything, and then I’ll make some more cells.”
I didn’t have to spend 6 weeks in the hospital. I was very, very fearful of that. I only spent a week in the hospital for my consolidation.
Describe the consolidation chemotherapy regimen and side effects
It was 2 days, and side effects were a sort of mini version of the induction chemo side effects. The only big difference in side effects at that point is we had realized that I had become menopausal, so I was going through hot flashes. I was going through just feeling out of it and weird. My period had stopped.
I was also going through this really quick month of just drenching my pillow every night and being very unhappy. That was my very sped-up version of menopause. For women, it’s typically over the years.
Mine was over about a month, so it was intense.
Also, I had a lot of upset stomach. My skin was uncomfortable. I think I was having some dryness, and part of that is just being in a hospital environment and being hooked up to things. My skin was very fragile.
Nausea, upset stomach loss of appetite. Food tasted weird. I started eating just a lot of very plain food. Salt was helpful. Hot sauce was helpful if I could tolerate it.
How many bone marrow transplant matches did you end up having?
They had realized that I’m the whitest person alive and that there are many matches for me. They found out that I certainly had some matches that were potential in the system.
It was very vague at that point. They said there’s about 5 or 6 people that are a possibility worldwide, Germany being the biggest donor pool. Those are European folks. A lot of your bone marrow and your makeup has to do with your race.
For me, [I have] European origins on both sides of my family, pretty much English, Scottish, German. I was not a big mutt, so it was easier to match me, which is very unfortunate for many people who have much more varied lineage or come from other nations. I was able to be matched up.
At first, the doctors really wanted to consider and look very closely at each potential match. They were looking at things on a chromosomal level because much like a heart transplant or kidney transplant, the body may reject something foreign.
To mitigate that, to make sure that the chances of that are low, the matching factors — I believe there are 10 to 15 of these parts of your chromosomes that they’re looking at to see if they’re going to match with that donor. It’s called a match donor.
You can also get an unmatched donor, where they’ve got half of the chromosome. It’s much more risky, [and there are] way more complications after the fact. The closer the match you can get, the better outcome you’re looking at.
I found out later they were coming from Connecticut, but just because someone has registered themselves within the bone marrow registry doesn’t always mean that they will follow through with giving you their cells.
They have to narrow it down to the best matches and reach out to those individuals to see who is willing to move forward with a medical procedure to save someone else’s life.
What was the transplant process?
The beginning of November, I was brought back into the hospital for my transplant. I was given a day’s worth of heavy-duty chemo just to make sure everything was suppressed so that when the new bone marrow came into my body, it would be able to have space and room to replace mine.
There were a couple of intense but exciting days leading up to that transplant. It’s a risky process. Before the transplant, I needed to get a Hickman line installed, which is a central line that’s in your chest wall that is a better multiple line into the heart and circulatory system to be able to deliver drugs. It lasts longer than a PICC line.
They require a 3-1 Hickman for transplants so that you can get hooked up to a bunch of different stuff at the same time. That was my first process, going into Interventional Radiology to get that put in. Then I was brought up to my room and given heavy-duty chemo. The transplant happened on November 6.
It seems like any other blood donation. You’re getting a bag of plasma. It’s yellow.
You know how far it’s come from because if it has a preservative in it, it smells a little bit like chicken soup. You can smell down the hallway when someone’s getting a transplant if it’s from Germany (or comes from farther away) and had to be couriered over in a slower process.
Mine was fresh, so I didn’t have any of those smells. We knew this is good. The only thing I knew about my donor was that he was in his 20s and was young. That’s also a good factor. I didn’t know the name.
I didn’t know where [he was]. I didn’t know if I would even find out those details till later. You have to wait a number of years, so it seemed just kind of like a regular donation coming down the line.
We knew that these were magic. These were special stuff. We’re all excited, and it’s a birthday, too, so they sing ‘Happy Birthday’ to you because your immune system is brand new. It’s just been born.
I think my mom brought a balloon. We weren’t allowed to have fresh flowers or anything like that. I did not want any cake. It was tricky because for the transplant process, the cold and flu protocols were put into place by that point in the year, so children under 14 were not allowed to visit.
I was not allowed to see my daughter during that time, and I feared that I’d be in the hospital for 6 weeks or more based on previous experience. That was really hard. We’re doing FaceTime and all that kind of stuff. I missed out on Halloween that year, so they sent pictures. It was hard.

What was it like after the bone marrow transplant?
After you receive your stem cells and they’re going through your body, it’s really a waiting game to see how your body’s going to react. There’s many mitigating things that drugs can give you, steroids and things like that.
They begin this protocol the day before the transplant. Pills you’re taking, so you’ve got antivirals, antibacterials, drugs to prevent pneumonia, steroids to help your immune system. All these different things get put into place that also inform you that your body is heavily at risk, because you have a new immune system.
How did your body react to the bone marrow transplant?
The side effects were very similar to the chemo. More than anything else, that was the chemo that I was feeling side effects for more than the transplant.
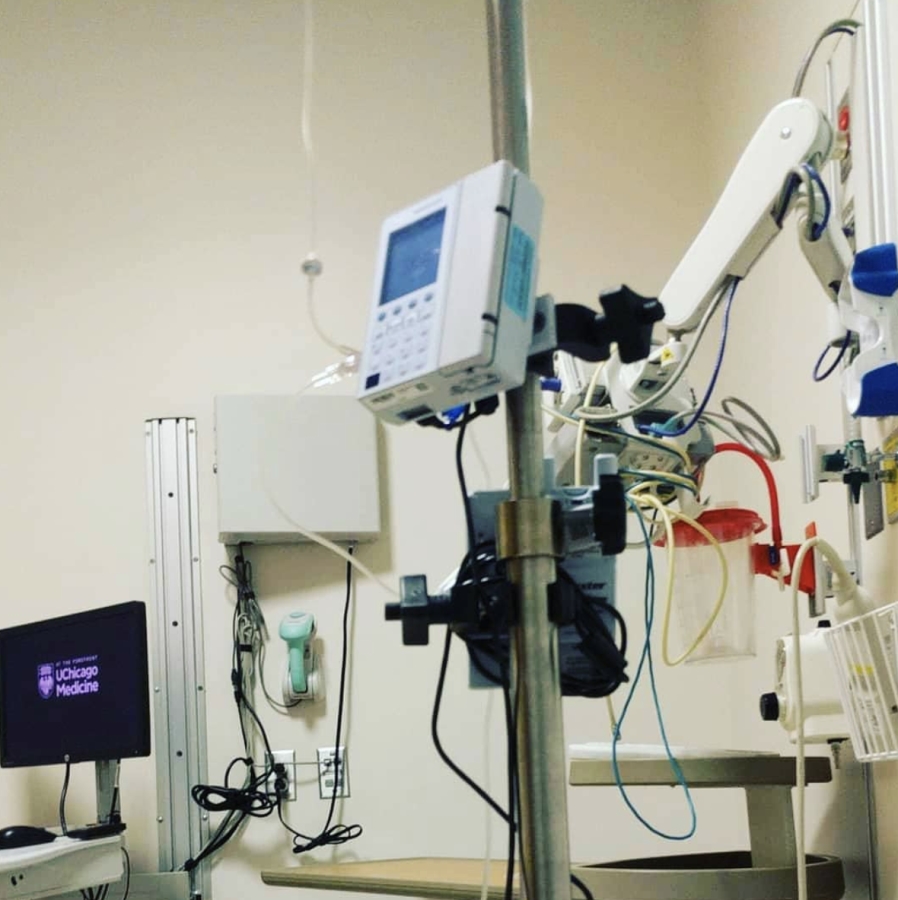
Very intense fatigue. The steroids also made me feel a little bit weird. I was on a pretty high dose of steroids. Lots of upset stomach. I did not want to eat. I did have mouth sores, which with high-dose chemo and many other types of chemo is common.
They did give me one type of chemo that is very much known for creating mouth sores, and I had mouth sores all the way down inside my throat. I couldn’t speak, and I had a very difficult time swallowing. It resolved itself.
After about a week, it got slowly better. It was unbelievably frustrating because the 3 things that doctors are constantly telling you to do after transplant is to move around, go for walks, and eat and drink water. They are measuring how much water and food intake and exercise I’m doing every single day.
I was not able at some points to do what they needed me to do, but I worked really hard at it.
Even if it was, “I can’t eat, but I certainly can get my husband to pick me up the highest calorie banana smoothie he can find with full fat ice cream in it.” I’ll have a couple sips. That’s better than nibbling on a cracker. It was also difficult because being vegetarian, there wasn’t a lot of food on the menu, so I ate a lot of peanut butter and jelly.
»MORE: Hear from a Bone Marrow Transplant specialist
Transplant Recovery
How was the transplant overall?
My transplant was very successful. I was able to go home after 3.5 weeks in hospital, which was amazing for everyone.
You had to advocate for yourself to go home from the hospital
A very scary thing was [with] the main doctor who was on call — not my oncologist, but the main transplant doctor I was working with. For those particular weeks, when it was time for me to go home and my cells had recovered enough for that to be safely done, she was not comfortable releasing me since I had a preschool-age child at home.
It took advocating for myself and working with my nurses to figure out what other doctor I could ask to see. I realized and did some of my work talking to the nurses, realizing that the doctor that I was working with was rather young, didn’t have children, and didn’t really understand that the whole reason I went through this process was to be a mom and to be with my family.
So I ended up meeting another doctor, who was wonderful. He has 5 children, so he got it. He understood, and we ended up making a deal.
We pulled my daughter out of school for the first 100 days after my transplant [because] the first 100 to 120 days are meant to be high risk.
Patients are in isolation at home or in the hospital. You can’t really go anywhere. You could wear your mask and gloves — very similar to this pandemic. Very strange.
A lot of that is because your immune system is being suppressed by immunosuppressant drugs so that you do not reject the new cells.
They can slowly wean you off of that if you are not having graft-versus-host acute symptoms and reactions. I was able to be weaned off of those pretty quickly in a number of months.
»MORE: Mental and emotional support when leaving the hospital

What should people know about that high-risk recovery period after the bone marrow transplant?
It’s also critical to have a caregiver during those 100 days. They would not allow me to have a transplant unless I had a 24-7 caregiver with me at my side monitoring me for any issues that may arise.
I also was not allowed to be further than 30 minutes away from my hospital.
My husband needed to take care of my daughter and needed to work, so we brought in my mom.
Were you able to have any visitors outside of your husband, daughter, and mom?
Yes. You just basically had to interrogate everyone like, “Do you have a cold? Does someone in your life have a cold?”
Where there any other steps you took to help protect yourself and weaker immune system?
I made my husband stop going on public transportation. There’s certain foods you’re not allowed to eat. You’re not allowed to eat fresh berries. You’re not allowed to touch soil. You’re not allowed to be around flowers. You’re not allowed to clean a litter box or pick up dog waste or anything like that. You’re not allowed to do the dishes.
There’s a lot you’re at risk for: viral, bacterial, all sorts of things. Fungal can actually kill you. It’s insane. When your immune system is that suppressed, you’re under some pretty strict protocols.
Any other tips on how to best isolate at home?
Figure out how you can connect with your community, whether that be a community of cancer patients, your community at church, friends, family — through the phone or through social media (if you’re comfortable with it), through email — to really make sure that you are making sure those relationships continue.
I think finding other people who are maybe 6 months or a year out from what you’ve been through is unbelievably helpful. You’re going to have a million questions. To be able to go to some of these communities online and ask those questions from informed people that speak in plain English not in “doctor-ese” is really comforting and really helpful.
You developed chronic graft-versus-host disease (GVHD)
I developed graft-versus-host disease a number of months after my transplant. This is typical. Oftentimes patients have some sort of acute graft-versus-host directly after transplant. It can impact any part of your body.
It’s truly your immune system saying, ‘Hey, there’s some old immune system here.’ It’s fighting it out, so it can fight it out in your kidneys, your skin, your muscles, your eyes, what have you.
I had some dry eye after my first transplant and was able to handle that with basic use of eyedrops. The main factor for me that was an issue was it really felt like I gained arthritis in my hands, and they were very sore. It was difficult to do knitting or crafting things that I regularly did, and that was due to graft-versus-host in that kind of muscle skeletal area.
How did you determine it was graft-versus-host disease (GVHD)?
I needed to see a number of different doctors to kind of eliminate all the possibilities that it could be before, because there’s no test for graft-versus-host.
It’s about observing over time and eliminating all the other things it could be.
What helped with the GVHD?
I was able to go on to Celebrex, and that was very helpful. Did physical therapy, but was not helpful. Didn’t do the job, but Celebrex was helpful.
I still get fatigued. I still have times when I need to massage my hands, put warm packs on there, or do different kinds of stretching.

»MORE: Explore more on GvHD and what to expect from a medical expert
Clinical Trial
How did you hear of clinical trials?
Being at a teaching hospital, I was often presented with opportunities to do clinical trials. Some of those were as simple as a 1-page questionnaire about my mental health.
One that was much more involved was the WT1 study, which was a vaccine, looking at a particular mutation that I had and trying to prevent relapse from cancer. It was an intense undertaking.
How was the main clinical trial you underwent?
The drugs were completely covered by the research study, so all I had to do was just show up on a staggered basis. First, 3 times a week for the first month, and then 2 times a week for the next month, and so on and so forth until it was every 3 weeks. I would receive an infusion. It was actually an injection, but it was very thick, so it was more like an infusion.
I would have to be at the hospital for 4 to 5 hours. They would not make the drug until they saw the whites of my eyes because it cost $10,000 per injection. But I did relapse. It was not a successful study.
Were there any side effects from that infusion?
It did not have many side effects for me beyond taking my time. I learned to make my clinic room into my office. I brought my laptop, and I would work from there on those days. It worked out for me.
It was a good transition emotionally and mentally away from very intensive getting blood counts every couple of days back into a life that isn’t totally structured around cancer.
Resuming Life
When did you decide to go back to work?
When I felt like it was time for me to go back into the office, I actually started at home. We did a trial period of a month where my daughter went back to school; I was healthy enough to have her bringing germs home. We tried that out to see how that was going to work.
I worked from my home office, which kind of worked and kind of didn’t. I just had the type of job that was difficult to work from home based on a lot of meetings, and the tech wasn’t in place. So I did return to the office.
»MORE: Read more on how others dealt with working after a cancer diagnosis
How did you feel when you physically went back to the office?
I will say that I had a lot of fatigue. I had a lot of brain fog, ended up going on more intensive anti-anxiety medication, and started a stimulant to help with the fatigue, which was helpful for a short amount of time.
I was able to transition back to the workforce, and it was very gradual. Every month or so, I would feel a little bit more like myself and a little bit more like myself. I would say after a year after transplant, I felt like my old self.
I was definitely a different person, mentally and physically. My get-up-and-go was back and my ability to focus on other things had changed, but I was able to do the things that were meaningful to me.
Relapse
When did you find out the cancer was back?
In August a couple years later, I had my yearly appointment with my oncology team. That’s a physical, as well as taking blood samples. They typically take 5 or 6 vials, and they’re testing for a whole host of different things and comparing it to your last visit.
I felt fine. I thought everything was great. I was moving on with my life, and things were going pretty well.
Unfortunately, 2 days later, I received the call that I needed to come in for a bone marrow biopsy because my blood samples too didn’t look good.
They weren’t sure, but they needed to get more information. I came in for a bone marrow biopsy just a couple days later and quickly received the results that a very low level, almost unheard of, of disease was found in my bone marrow and that the cancer was back.
There was a very low level of disease
It was strange because I was so used to the AML process with my experience and many survivors that I’ve talked to and their experiences. If you have AML, you’re immediately in the hospital, and you’re getting treatment.
I relapsed with I think 9% disease, which was a big complicating factor in a number of ways. That is unheard of. It doesn’t make any sense to give someone with that low-ish level of disease heavy-duty chemo and put them on the transplant train. There could be other things at play there.
I was just lucky that I had a scheduled appointment, so they found it very early. They were actually able to take some time and look at a number of different ways to treat this.
How did they treat the relapse?
I was treated outpatient for the first little more than a year of relapsing. We tried a number of different drugs. We tried a drug called azacitidine, which is often used for pre-blood cancers. MDS is that blood disorder.
How did your body respond to the azacitidine?
It was successful for me that it was able to keep me at that 9%. My body had very little side effects. I didn’t lose my hair or anything like that from this particular drug. It is a low-dose chemo.
What adjustments did you have to make at home and at work?
I did have to go in for those treatments, but I was able to live my life at home. I did know at that time that a second occurrence of leukemia does not have great odds. I immediately quit my job and went on disability.
The disability process takes 6 months or more, even if it’s fast-tracked, so I knew from my experience working with other survivors that I needed to do that and do that quickly.
How long were you on azacitidine overall?
I was on azacitidine for a little over 6 months, and then it stopped working. They were starting to see more development of disease.
Describe the clinical trial for venetoclax
They decided to try a clinical trial for venetoclax, which at that point in time was only approved for another type of cancer, CLL (chronic lymphocytic leukemia or small lymphocytic lymphoma), and it was in trial to be seen if it was an immunotherapy that was effective for AML.
»MORE: Learn more about what CLL is
That I received directly from the manufacturer. The manufacturer paid for it. It was unbelievably expensive. You would receive a pack of pills, kind of like a booklet. I took that at home, and there was a very specific way I had to take it.
I had to do weekly check-ins with the pharmaceutical company and weekly check-ins with my doctors.
How did your body respond to the venetoclax trial?
It didn’t really do anything. For my particular case, it didn’t have many side effects either. They really wanted to give it a good go because it had been successful with other patients.
They wanted me to take it for at least 4 months before they would abandon this treatment regimen. I took it for a while, and then we started going back down the transplant route.
How did you get off the drug?
It was once a day, but when it was time for me to get off of that particular pill, it had to be stepped down in a certain way.

2nd Bone Marrow Transplant
Describe the preparation before your 2nd transplant
Since I did have a low level of disease, my trajectory towards transplant the second time around was quite different. I did not have to do induction and consolidation.
That was compressed all together before my transplant. Once my donor had been picked, all of that paperwork was put together, and the schedule was put forward, we could move a little slower.
November, I checked back in into the hospital and began high-dose chemotherapy for the week before my transplant.
They added radiation to the regimen
They added full marrow radiation. It’s not quite full body radiation. I had 3 of those visits. That took a very long time. They tattooed parts of my chest and my stomach, and that’s where they aimed the radiation.
That is just like an extra thing. They wanted to do something different than they did the first time around, which was just standard protocol. They wanted to add some bigger guns to try and have my transplant be more successful long term.
Describe the radiation process
The radiation therapy was pretty hard mentally, having to be still, having to have casing over my face, this web fitted to my face. Having doctors move in and out of the room because of undergoing something really toxic was very scary.
I didn’t know how to prepare myself for it. I didn’t really know much or anything about that process. My previous treatments had been pills or infusions, and you have a little bit more control over your body, your surroundings, and how you distract yourself.
You are completely in the moment when you receive radiation. I think being unable to distract myself, even though they played good music and things like that, was difficult.
How many times did you have to undergo radiation?
Just 3. It was a couple hours each time, but there’s so much positioning and moving. I don’t know how much of that stuff was actually receiving the radiation, but it was hard. You had to go to a separate room for that.
I was transported from my inpatient room to the basement of a nearby building because they want to keep the radiation away from most people.
Were there any side effects of the radiation?
I did have major side effects from the radiation. My adrenal system failed. I actually lost consciousness the last time I did radiation. Trying to get on the table, I collapsed, and they called the cart and all that sort of stuff.
I did come back, and I didn’t injure myself. I had some bruises, but they did go through with radiation because I needed it after that, which is just bizarre. But the radiation has done some considerable damage to all parts of my body.
How soon after the radiation did you undergo the bone marrow transplant?
I believe I had my last dose of radiation in the morning and then had my transplant later that day. It was a really rough day. It wasn’t this “happy birthday” type thing because I had started to lose consciousness and had blood pressure issues.
I was up all night with tests. I was taken for CT scans, MRIs, and all sorts of neurological examinations to try and find out what was wrong. Everything was inconclusive. It was very difficult to try and figure out what was happening.
»MORE: Read other patient experiences with radiation therapy
What were the side effects of this second round of transplant and chemo?
I was losing consciousness a lot and was put on bed rest. At that point, all the side effects of the chemo kicked in. I had vomiting and diarrhea all the time and could not take care of myself.
I was really at the mercy of wonderful nurses, who took care of me and cleaned me up a million times a day.
It was a totally different experience because I really wasn’t really able to advocate for myself very well. I’m a medical marijuana user, and that had very much helped me the year before my second transplant mentally to deal with all the depression and anxiety.
I wanted to use that in the hospital during my second transplant. I didn’t smoke or anything; I just used edibles, but they really discouraged that. They didn’t want that to happen, and I understood.
I was given the synthetic version of marijuana, which is called Marinol. It’s a pill. I hallucinated for days on end, and it was terrifying. We realized that was what was going on, so they took me off of that. It was really, really hard.
2nd Recovery
How was this round of recovery?
I was in the hospital for 6 weeks. That’s long, but my family lost their minds when they did decide to let me go home because we live in a brownstone building with a big staircase.
I was collapsing constantly; I was this major, major fall risk and needed so much care. [I’m] someone who doesn’t have an immune system [and] is totally isolated.
At that point, my body stopped making magnesium and potassium, so I needed to be taken to the clinic every single day, sometimes twice a day, for hours at a time.
That was at least a little bit of a relief for my family to be like, “Okay, she can go and be with that team of nurses and be taken care of [to] give us a break and take care of [her] daughter while all of this is going on.”
We’re all on super high protocols at home. You come home, you sanitize, you leave your shoes outside, you were constantly washing clothes at high temperatures, and all that sort of stuff because I was very much at risk.
I physically was more vulnerable looking and acting than I ever had been. I really came home as a very different person. Then I started to have some cardiac issues that would come and go.
We think it’s due to one of the chemo agents that I had in 2014. There has to be a heart failure that has to be managed. It’s not a considerable amount of heart failure.

The other thing that’s really important after transplant is monitoring pulmonary, because it can go down very quickly.
Graft-versus-host disease of lungs is common. If it’s caught early, it can be dealt with. I was doing great pulmonary-wise during all my testing monthly, and then my pulmonary function just dropped with any exertion.
This is right when we were kind of figuring out how to repair my adrenal system. I was not having to use a walker all the time or a wheelchair. I was starting to make my own cortisol. Then my pulmonary function just tanked, and they put me on oxygen 24 hours a day.
What helped with your pulmonary recovery?
I worked with the most amazing pulmonary specialist, and she was able to to really work with me and figure out that this one particular anti-pneumonia drug that I was on called dapsone was just destroying my pulmonary function.
Literally, after struggling for months, my pulmonary function was completely normal.
How are you doing after the second transplant?
We’ve been able to manage a number of the aftereffects of my transplant. Some are ongoing. I’m one of the healthier people in the oncology office, but I have a new primary care physician, and I’m like the sickest person she’s ever seen.
At this point, heart, lungs, and sexual side effects are managed by treatments and therapies.
I go to the doctor more than the average person. I’m able to lead a pretty normal life. Fatigue is still a major, major factor, and I will have days where I just need to go back to bed. That’s becoming less, but it’s still there.
Once my adrenal system came back, many of my symptoms and the constant dizziness and verge of collapse resolved. Now when I have fatigue, I’m very dizzy and need to really remind myself so that I don’t lose consciousness.
How often do you have to go in for blood tests?
I’m on a monthly basis right now, though things are totally out the window. They have to closely monitor. I’m on every 3 months with the endocrinologist and a cardiologist.
What is life like now after treatment and transplants?
I do a lot of work on my mental health. I have a therapist. My daughter has a therapist. My husband has a therapist. We have family counseling. We’re all very upfront with each other about what we need.
I totally take antidepressants and anti-anxiety medications and for chronic pain. Medical marijuana has been a game changer and lifesaver for me. I’m a big advocate for that. My life has definitely taken a big step back [with] the financial hit of going from being a dual-wage earning, professional household to one income and some disability money.
Also, during the time, my daughter was diagnosed with profound dyslexia and needed to be in a very different educational environment. I mean, we’ll never be able to retire! I don’t know. I think we’re still kind of in denial about some of that.
What is your status now?
I’m in remission.
You could call me NED if you want to — no evidence of disease. All of those things are good.
Mental, Emotional, and Sexual Impacts of Cancer
How did you manage the flux of messages and visits from supporters?
It’s really tricky to figure out. I’m a pretty open book, so I shared on Facebook. I contacted my employer and let them know.
The director of my department at the college came and my assistant came, and that was very strange. In hindsight, I would not have permitted that. I think having people see you at your lowest moment is private. I learned a lot after I had my daughter. I did not need to have my best friend in the delivery room or my mother-in-law, but you live and you learn.
I did not have that in place. I did not have someone to filter all the people coming into my orbit at that point at all. I was kind of managing that myself.
And it was it was difficult. It was hard.
In some ways, it was like reliving the diagnosis all over again every time you had to tell someone what what you had, what cancer you have, and what’s happening. Also, the leukemia journey is quite different than breast cancer journey or the treatment protocols for colon cancer or anything like that. There’s much more inpatient.
It’s much more high risk. It’s very fast moving. The thought of even getting a second opinion… it’s just not possible. I think the majority of people I was talking to — unless they were someone who was already in the medical community — were just confused. They just were perplexed. That that was difficult, and I think it did make me kind of accept my circumstance faster than I would have if I would have kept everything private.
Any advice for people on what can help maintain energy while communicating with supporters?
I think setting up some sort of a website that is private, such as Caringbridge. There’s a number of other ones out there. Your social media, calendar, your email can be really helpful as far as scheduling goes. If you would like to, you can update and have a blog. I started with that process.
It got exhausting very quickly. Some people have their spouse or a family member updating that information about you. It’s truly up to you what you would like to share.
I think for many of those websites, there’s a way to schedule food delivery, set up if you need to raise some money, or if you need someone to offer to clean your house or walk your dog.
For us, it was really helpful because we wanted to create as much normalcy for my daughter as possible. We didn’t want her just hanging out at the hospital all the time. That’s just not realistic.
Even if she really didn’t know what was going on. [She] thought it was just this fun thing to go meet all these nurses who thought she was adorable and get all dressed up to go see mom. What we were trying to create was some normalcy for her.
We used Caringbridge to make playdates [and] to request food. Being busy professionals, we often had our groceries delivered through a service before cancer came into our world. [We were] letting my coworkers who live all over the place know that would be something that would be helpful beyond just delivering us food.
We’re a little complicated. My husband’s vegan and I’m vegetarian, so many people who don’t eat that way were kind of confused as to what do I bring them?
The grocery gift cards, which could be done through email, were just absolutely wonderful because we were also dealing with a pretty quick, significant loss of income. Feeding people is important.
How did you deal with the mental struggles?
The mental health side effects are significant as well. It changes perspectives. It changes your anxiety level and all sorts of things. It’s really important to shine a light on people who are still struggling, but making their life as positive as possible.
Even if you’re stuck in bed most days of the week, if you’ve got that one day where you make an amazing dish or spend really quality time with someone who’s important to you, that’s still a life. That’s still important. You still matter.
I think that’s very, very much an important thing to center in your world — that we don’t know what’s going to happen. That’s very hard, but we’re stronger than that. We can find a way to make a new life.
How do you keep perspective?
My story is beautiful and easy compared to a number of people I know who are in their 30s and 40s and are so permanently disabled [they] will never walk again. They’re losing their sight because of transplant complications. I’m fortunate that I already had a husband and a kid.
I’ve got a friend who’s trying to figure out how to date with all of this, and it’s hard.
How did your cancer experience impact your personal relationships?
When I was initially diagnosed and again the second time, a lot of friends fell away.

Friends that I had known for years and years and years, and for many reasons that I will never know. I think for some people, it’s just difficult to face cancer if they’ve lost someone or to face a friendship that is not just getting coffee and enjoying each other’s company. It becomes much more serious.
There’s still a lot of play in my world, a lot of fun, but it became smaller. It became my mom, my husband, my daughter, and a couple close friends. Sometimes those friends would shift and change month to month, because it is really exhausting and taxing. I think to have friendships that you can in some ways find an escape from cancer.
I have people in my life that I know I’m not going to sit down with and go through all the awful things that are going on with me when they say, “How are you?” I’m going to say, “Hey, let’s talk about this book we both just read or this movie,” or, “What are you cooking?” All of those kinds of things to compartmentalize things in a healthy way.
You can also realize that you are more than cancer and that this is just a huge mountain to climb. For me to be the advocate that I needed for myself and my family, cancer was really just the be-all end-all. [It was] everything that I was focused on. Everyone was focused on it, and it was hard to take myself out of that to be able to have a regular conversation.
It felt like I was living in some sort of alternate universe, and I couldn’t connect with anyone. It took time and patience to be able to figure out how to be authentically me. Angry about cancer, advocating for myself, still being hopeful, but also having friendships that were maybe a little more surface level, and that’s okay.
There are going to be people who leave your life, and it doesn’t make any sense to dwell on that. You can be sad. You can feel those feelings but move forward. I’ve met so many amazing cancer patients, survivors, doctors, and researchers that fill that void 10 times over.
Speaking of personal relationships, what were the sexual health impacts?
Having gone through menopause in my 30s rather early, I had all of the side effects of menopause that people think about, such as hot flashes and irritability. Down the line, I suffered from vaginismus, as well as a very dry tissue.
I was able to reach out through my regular gynecologist to a special group at the University of Chicago that works with women at every stage of the cancer process dealing with sexual side effects. You can also get graft-versus-host disease of the vulva or vagina. I did not have that. That was ruled out.
Primarily, the side effects that I was experiencing are very common for people who have gone through any sort of cancer treatment, which was very dry, very irritated tissue, and to be able to engage in a successful sex life with my husband.
I needed to go through some physical therapy, which I was able to do at home using dilators and trying lots of different lubricants. My cancer was not a hormonal cancer, so I was able to use hormonal creams. It was helpful and resolved things, but it was a multi-month process to slowly introduce moisture to my body to make sure that my body didn’t poorly react to being uncomfortable, in pain, and things like that.
It took time. You have to dedicate an hour of your day to working through that. Cancer often impacts intimacy in relationships. It can take work to get it back.
For women and men who go through cancer treatment, sexual health is a part of having to work at it again. I think the message there is sometimes it takes some work to refocus on that part, but it’s important.
I’m on a patient board, and I’ve helped them with a number of their materials and spoken at conferences. I’m very open about that sexual piece of side effects from cancer, particularly for people who are in marriages where you’re used to having regular sexual activity, you’re used to going on date nights. Cancer changes a lot of that — the fatigue and side effects from treatment.
For many people, they stop having sex. They stop engaging in anything sexual for years, months, depending upon the person. You have to kind of restart that relationship and those aspects of it.
You’re probably great with your partner as far as getting dinner on the table, hopefully paying the bills, and working together with childcare. But the thing that gets cut out of many people’s relationships is that. Intimacy is what brought you together in the first place, those connections, so you really do have to reeestablish them.
For myself and my husband, it was working with a great gynecologist, who was able to help us with the fiscal aspects. It was also working with a marriage counselor to be able to reestablish a lot of those things and to resolve some of the conflicts and issues that came up mentally for us both through treatment.

What has helped uplift you most?
For me, things that were just surprisingly helpful were these close relationships — that were sometimes fraught — with family that have really grown in new ways. My mom and my husband are now very good friends, and that just makes my heart sing.
My spiritual community and my church have been very important to me in that I was very active and involved before cancer. I worked with all the youth in my Unitarian church, but now I’m not able to do that. I’m able to support in different ways and had to learn how to be supported, which was hard but necessary.
The other things that are really helpful for me have been nature and finding ways to go outside. I was stuck for so long in hospitals and in my own home. I could just walk to the park or Lake Michigan here in Chicago. It’s just unbelievably important to me to be standing outside, even if it’s with a mask and a hat. Just feeling the sun is life changing, as well as creating and making things.
I make jewelry. I paint. I write. I share my story. I think those are ways that I feel like I’m still contributing to the world. I’m still able to be part of something and make something.
In the same way, music, reading, and audio books really, really have helped bring meaning to my life. My first transplant, I was so scatterbrained, so all over the place. I could just kind of watch junk food TV, and that was about it. That gets old fast.
Especially someone like myself, who loves books and loves literary fiction and poetry and things with a million footnotes, finding audio books and very wonderful narrators the second time around just fed my brain in a different way. That was really life-giving.
How have you been able to move forward with life?
I don’t think I’ve moved on. I think that I’ve learned how to manage the uncertainty. The side effects. The future. Not knowing if things will come back, and also just acknowledging that the support system that you think you had isn’t always there. Your world gets pretty darn small sometimes.
But there’s a lot of beauty in that.
Any guidance for people on how to handle life after cancer treatment?
Going through the cancer experience, for many of us, society expects for us to go through treatment, reach remission, and everything goes back to normal.
I don’t think that’s the case for anyone who’s had a cancer story or cancer journey.
Many of us have lifelong chronic conditions. Many of us, after years of getting back to normal, will have a setback, recurrence, new cancer, or a later effect.
It’s difficult for people to understand because it’s not communicated in the media, and it’s not always supported within the cancer nonprofits in those communities. People heavily focus on that time of intensive treatment, and then you’re supposed to be done. That’s really not how it works.
What’s your overarching message to those reading your story today?
The best piece of advice that I was ever given: I asked my doctor, “Should I stop drinking coffee now that I’m a cancer patient and all of this?”
He said, ‘Absolutely not. You should continue drinking coffee and doing your morning routine because you have a new job. Your job is being an advocate for yourself.’
That I have taken to heart time after time. It really structured my world and made me realize that I’m not a victim. I am advocating for myself, and I can make a difference in my own health and the health of others.
Inspired by Mary Clare's story?
Share your story, too!
Acute Myeloid Leukemia Stories
Russ D., Acute Myelomonocytic Leukemia (AMML), with NPM1 Mutation
Symptoms:Flu‑like symptoms, profound fatigue, blood pressure drop, shortness of breath
Treatments:Chemotherapy, clinical trial (menin inhibitor)
Shelley G., Acute Myeloid Leukemia (AML) with NPM1 Mutation
Symptoms: Fatigue, rapid heartbeat, shortness of breath, low blood counts
Treatments: Chemotherapy, clinical trial, stem cell transplant
Joseph A., Acute Myeloid Leukemia (AML)
Symptoms: Suspicious leg fatigue while cycling, chest pains due to blood clot in lung
Treatments: Chemotherapy, clinical trial (targeted therapy, menin inhibitor), stem cell transplant
Mackenzie P., Acute Myeloid Leukemia (AML)
Symptoms: Shortness of breath, passing out, getting sick easily, bleeding and bruising quickly
Treatments: Chemotherapy (induction and maintenance chemotherapy), stem cell transplant, clinical trials